
There are many different conditions that can cause lung problems and emphysema, including a variety of heritable diseases. One of these is Alpha-1 antitrypsin deficiency (also known as AAT deficiency or Alpha-1), a rare, incurable genetic disorder that most people have never heard of.
Alpha-1 is the result of a protein deficiency that can cause mild or severe damage to the lungs and liver. Many people with AAT deficiency experience asthma-like symptoms including breathlessness, wheezing, and coughing that can occur in childhood or later in life.
Because Alpha-1 is rare, most doctors don't routinely screen for the condition, and some people with AAT deficiency don't get diagnosed until they develop other liver problems or lung disease. This makes it a difficult disease to catch, especially since, for some people with Alpha-1, symptoms don't show up until late adulthood.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Only about 100,000 people in the United States have been diagnosed with severe AAT deficiency, and there are still many things that doctors and scientists don't understand about the disease. For instance, doctor's don't understand why some people with Alpha-1develop liver disease at a very young age, while many others go their entire lives without experiencing any liver problems.
If you or someone you know has been diagnosed with Alpha-1 antitrypsin deficiency, you probably have a lot of questions and worries. That's why, in this article, we're going to walk you through everything you need to know to better understand the disease, including symptoms, potential complications, and what kind of treatments are available to help people with AAT deficiency.
What is Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin deficiency is a rare, but potentially very serious, genetic disorder that mainly effects the lungs and liver. It occurs when a child gets defective AAT genes from their parents, which prevents their bodies from making enough of an important protein called the alpha-1 antitrypsin protein (AAT protein).
There are several different types of genetic mutations that can cause AAT deficiency, and some lead to more severe symptoms than others. Depending on their individual genes, a person with the disease can have different levels of AAT protein in their bodies, ranging from extremely low to only slightly lowered amounts.
Because of this, some cases of AAT deficiency are mild and don't cause many symptoms. Other cases can be very severe and lead to extensive lung damage, liver damage, and other complications.
People with severe AAT deficiency are prone to liver disease and cirrhosis as well as chronic lung infections, bronchitis, and emphysema. Because of this many people with the disease develop respiratory symptoms like wheezing and difficulty breathing as they get older.
Treatment for Alpha-1 antitrypsin deficiency depends on individual symptoms and the extent of damage to the liver and lungs. Most treatment plans focus on preventing organ damage by keeping the lungs and liver healthy, and avoiding irritants and toxinss that can damage them.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa')}}
How Alpha-1 Antitrypsin Deficiency Affects Your Body
Alpha-1 Antitrypsin Deficiency can take many different forms, and every individual case of the disease is unique. How exactly the disease effects the body depends on the type of genetic mutation that caused it as well as age, lifestyle, and exposure to environmental irritants like dust and smoke.
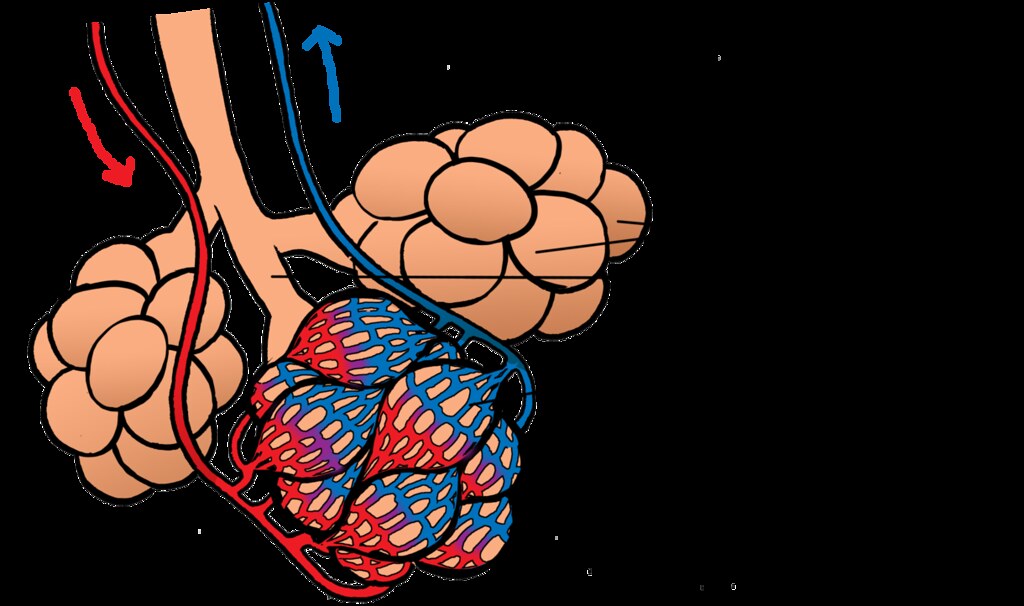
Problems caused by AAT deficiency are all related to the body making a dysfunctional version of the AAT protein. This protein is made primarily in the liver, and in healthy people it moves easily out of the liver and into the bloodstream, where it is carried to the lungs
.

People with Alpha-1 make an abnormal version of the AAT protein that gets stuck in the liver instead of moving into the blood. That means it can't make it into to the lungs to protect them from inflammation and irritation, leaving the lungs vulnerable to damage.
The symptoms of Alpha-1 and how severe they get over time varies widely from person to person. Generally, the less AAT protein a person has in their bloodstream, the more susceptible they are to lung damage and other symptoms.
A large number of people with AAT deficiency eventually experience some level of lung decline, usually between the ages of 20 and 50. Lung damage is accumulative, and how frequently the lungs get inflamed by infections and irritants like dust and smoke has a major effect on the severity of respiratory symptoms and complications.
Although slightly less common, Alpha-1 can also cause liver damage and scarring (cirrhosis). This can occur in both adults and newborn babies with AAT deficiency, although doctors don't understand exactly why it affects some but not others.
The following sections will give you a more detailed understanding of how AAT deficiency causes lung and liver disease in people with Alpha-1.
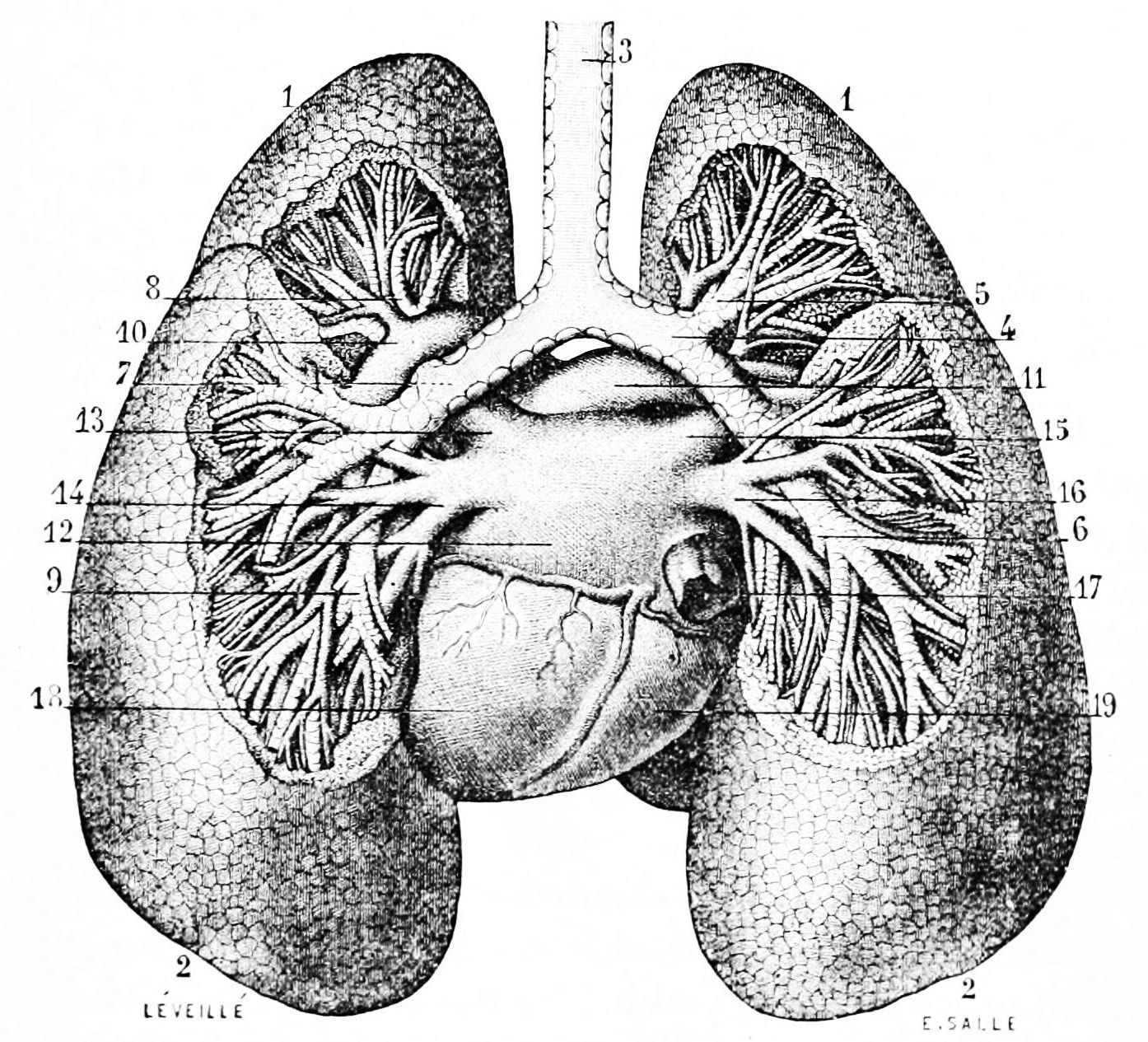
How AAT Deficiency Affects the Lungs
The AAT protein's purpose is to break down a powerful, caustic enzyme called neutrophil elastase. This enzyme gets into the lungs via white blood cells—immune system cells that circulate in every person's bloodstream ready to fight pathogens and infection when needed.
White blood cells release neutrophil elastase in the lungs whenever the lungs get inflamed by infections or irritants. This enzyme helps white blood cells dissolve bacteria and fight off disease, but it can also break down sensitive lung tissues if it's not tightly controlled.
In healthy people, neutrophil elastase doesn't cause any problems because the AAT protein breaks it down quickly before it can damage the lungs. Unfortunately, people with Alpha-1 antitrypsin deficiency don't have enough AAT protein in their lungs or bloodstream, so the powerful enzyme is left to wreak havoc in their lungs.
Leftover neutrophil elastase damages the tiny air sacs, called alveoli, that allow the lungs to absorb oxygen. Over the span of years, the lung tissue gets so damaged and scarred that it can't get enough oxygen into the bloodstream, causing lung disease and a variety of other complications as it worsens.
The best way someone with AAT deficiency can prevent this from happening is by taking special precautions to avoid lung infections and irritants like smoke. It is also important to treat any respiratory illnesses that you do get quickly and aggressively. Even minor lung illnesses like the cold or flu can recur again and again, causing chronic inflammation that, over time, can cause permanent damage to the lungs.
Most people with AAT deficiency experience some amount respiratory decline as they get older and their lungs accumulate damage. In people with severe AAT protein deficiency, this can eventually lead to chronic emphysema, shortness of breath, and other respiratory complications.
How AAT Deficiency Affects the Liver

Liver problems are much less common in people with Alpha-1, but when they do occur they can be serious and life-threatening. About five to ten percent of newborn babies with AAT deficiency are born with liver disease, but it's unknown why some babies and adults with Alpha-1 get liver damage while others don't.
Doctors and researchers only have a limited understanding of how AAT deficiency damages the liver and causes cirrhosis (permanent scarring). What they do know is that people with Alpha-1 get large build-ups AAT protein in their livers, which can make them prone to liver disease and dysfunction.
This happens because people with Alpha-1 make an abnormal version of the AAT protein that cannot exit the liver the same way that functional AAT protein does in healthy people. As a result, not enough AAT protein makes it into the bloodstream where it is needed to go to the lungs and protect them from inflammation.
Only about 15 to 20 percent of people with severe AAT deficiency ever experience symptoms of liver disease. For those that do, medications are available to help manage the symptoms and liver transplant surgery may be an option for people who develop life-threatening problems.
Causes of Alpha-1 Antitrypsin Deficiency

Alpha-1 Antitrypsin deficiency is caused by a defect in the gene that tells the body how to make the AAT protein. As a result of this mutated gene, people with the disease make a defective version of the protein that gets stuck in their liver instead of entering the bloodstream like it's supposed to.
This can cause liver problems and makes the lungs prone to inflammation. Over time, lung tissue can become damaged and scarred and lead to emphysema, trouble breathing, and low levels of oxygen in the blood.
In order to get AAT deficiency, you have to inherit two defective AAT protein genes from your parents. There are a couple different types of AAT gene mutations, and some cause a more severe protein deficiency than others.
Alpha-1 is inherited via a pattern known as autosomal codominance, in a way similar to how blood types are passed down through generations. The image below illustrates how this genetic inheritance pattern works.

Here are the three major types of AAT gene mutations:
-
The Z mutation: People with this mutation have extremely low levels of AAT protein in their blood. This is the most common mutation that causes Alpha-1, and it can lead to severe symptoms and disease in people who inherit two copies of the Z gene (ZZ).
-
The S mutation: People with this mutation have moderately low levels of AAT protein in their blood. This is a less common mutation, and usually causes less severe symptoms. People with two copies of the mutation (SS) usually do not have any symptoms at all.
- The M mutation: This is the normal, healthy version of the AAT gene. People with two copies (MM) of this gene type have normal levels of AAT protein in their blood and do not have Alpha-1. People with one normal copy and one mutated copy (MZ or MS) are considered carriers of Alpha-1.
You need to have two of these mutated genes in order to develop an AAT protein deficiency. However, it is possible to get the disease from any combination of the different AAT-deficient mutations.
For example, you could have one gene with the Z mutation and one with the S mutation and only develop a mild form of the disease, or you could have two Z genes (ZZ, the most severe form of the disease) instead. However, since they only have a very mild protein deficiency, people with two S genes (SS) usually don't develop any symptoms or complications at all.
If you only inherit one defective gene, and one normal (M) gene, then that makes you a carrier of Alpha-1. You won't experience any symptoms, but there is a chance you could give AAT deficiency to your children if you have them with someone who is also a carrier of Alpha-1.
Key Facts about Alpha-1 Antitrypsin Deficiency

Alpha-1 deficiency affects about 1 in every 2,500 people in the US. Even more Americans are carriers of the disease—an estimated 19 million people.
If the disease is caught and managed early, many people with Alpha-1 live just as long as people without the disease. With proper treatment and a healthy lifestyle, people with AAT deficiency can live long, active, and healthy lives.
People with the most severe AAT protein deficiencies (such as those with two copies of the Z gene mutation) are the ones that are most likely to develop serious, life-shortening diseases like liver damage and emphysema.
Because Alpha-1 is a relatively rare disease, it's not one that doctors routinely screen their patients for. Many people discover that they have Alpha-1 after they first develop breathing issues or show symptoms of liver decline.
Because the respiratory symptoms associated with AAT deficiency are so similar to other lung conditions, it's common for doctors to confuse the symptoms with asthma or smoking-induced emphysema. Fortunately, all it takes is a simple blood test to determine whether or not you have Alpha-1 deficiency.
Since so many people with Alpha-1 are misdiagnosed with other lung conditions first, medical professionals recommend that anyone diagnosed with a lung or liver disease get tested for AAT deficiency. Detecting the disease as early as possible is key for slowing or preventing further damage.
Unfortunately, researchers estimate that up to three percent of people living with COPD have undiagnosed Alpha-1 deficiency.
Alpha-1 Antitrypsin Deficiency Symptoms

The main symptoms of Alpha-1 include respiratory symptoms like coughing, shortness of breath, and frequent respiratory illnesses. Signs of liver disease, like yellow-tinted skin and eyes, are slightly less common but can be an important early indicator of AAT deficiency.
Every case of Alpha-1 is different, and how the disease affects you depends on how severe your AAT deficiency is and a variety of other factors. Some people with Alpha-1 are born with liver disease, while others develop liver damage later in life, or not at all.
Your individual lifestyle and how careful you are to avoid respiratory toxins and other irritants can play a major role in what symptoms you develop and how severe they become. If you have Alpha-1, you should have frequent visits with your doctor to check for signs of liver and lung damage so you can treat it as early as possible.
If you have AAT deficiency, it is especially important for you to protect your lungs from smoke, infections, and anything else that could cause damage or inflammation. You should also take care to protect your liver to avoid developing symptoms of liver dysfunction.
While some people with Alpha-1 develop organ damage early in life, many others don't notice any symptoms until they are much older. The first symptoms of AAT deficiency can appear as late as fifty or sixty years old.
Common Respiratory Symptoms for Alpha-1
- Shortness of breath and difficulty breathing, especially during physical activity
- Cough, often with phlegm
- Wheezing, especially during exertion
- Frequent respiratory illnesses and infections (e.g. recurring colds)
- Chronic allergies that last all year
Common Liver-Related Symptoms for Alpha-1
- Jaundice (yellowing of the skin and eyes) that can be present at birth or occur later in life
- Frequent itching
- Pale colored stools or blood in stools
- Dark urine
- Fatigue
- Swelling in the abdomen (ascites)
- Swollen, enlarged liver (hepatomegaly) or spleen
Panniculitis is another possible symptom of AAT deficiency. It is a very rare skin condition that causes raised, painful bumps (nodules) or ulcers on the skin.
Complications with Alpha-1 Antitrypsin Deficiency
Liver Disease

Low levels of AAT protein in the blood of people with Alpha-1 occurs because they make a version of the protein that won't leave the liver. As a result, it can't make it into the bloodstream where it's needed and instead builds up in the liver, leaving it prone to inflammation and disease.
Doctors and researchers aren't sure exactly how the buildup of AAT in the liver causes damage in some people with Alpha-1 but not others. However, they do know that, in rare cases, it can cause cirrhosis and serious damage that leads to liver disease over time.
Only a small number of people with Alpha-1 develop liver problems, but all people with AAT deficiency should take precautions to protect their liver from damage. Alcohol, viruses like Hepatitis A and B, and certain medications like acetaminophen can be especially dangerous for people with Alpha-1.
Emphysema
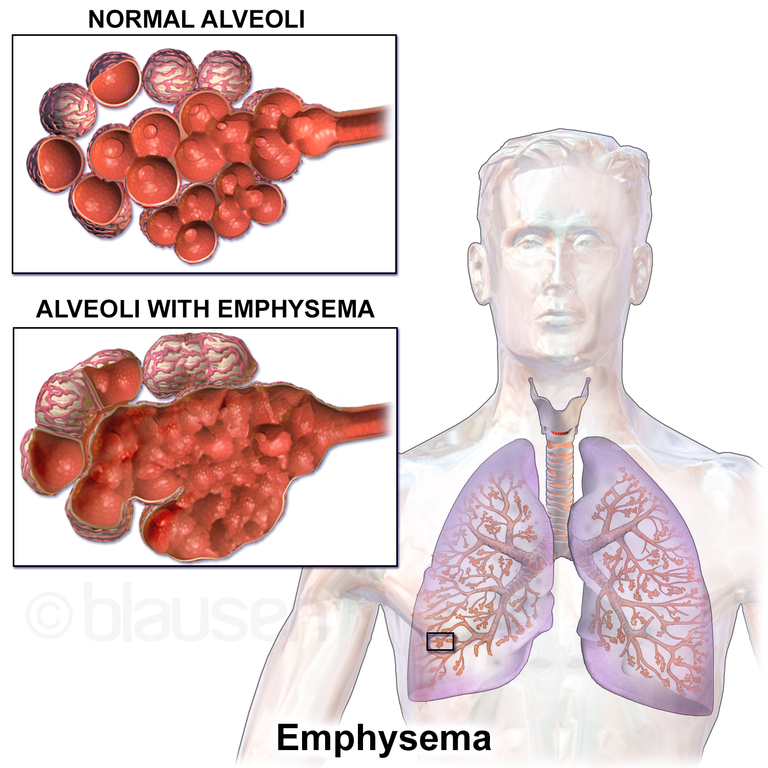
If you have Alpha-1, your lungs are prone to repeated inflammation and infection that can permanently damage delicate lung tissue over time. Because of this, many people with AAT deficiency experience some sort of lung and breathing issues as they get older, and some develop a more serious lung disease called emphysema.
Emphysema is a type of chronic obstructive pulmonary disease (COPD) that occurs when irritants, infections, or inflammation damages the tiny air sacs, or alveoli, in your lungs. This makes it difficult for your lungs to absorb oxygen and causes shortness of breath, wheezing, coughing, and other respiratory symptoms.
Damage to tissues in the lungs and small airways also makes it difficult to move air through the lungs. Unlike healthy, elastic lung tissue, damaged tissues lose their springiness and get stiff. This causes small airways to collapse, blocking air from flowing through and making it difficult to push all the air out of your lungs when you exhale.
Emphysema is an progressive lung disease with no known cure. That means there's no way to stop it from continuing to cause more and more lung damage over time, although medications and lifestyle changes can slow how quickly the disease worsens.
Exposure to toxins and other respiratory conditions can cause emphysema, but when emphysema is caused by AAT deficiency it is often referred to as Alpha-1 COPD. People with Alpha-1 tend to develop emphysema much earlier (by ten years or so) than “healthy” people who acquire it by smoking or exposure to other toxins.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Panniculitis

Panniculits is a rare skin condition that a small percentage of people with AAT deficiency develop. It happens when the layers of skin just under the surface get irritated and cause rash-like raised, red bumps (called nodules) on the skin.
Panniculitis often develops in patches on the thighs and buttocks and any part of the skin that sustains damage. It often only takes minor injury or abrasion to cause nodules to form, which can happen during vigorous physical activity.
The severity of symptoms varies from person to person, ranging from minor irritation to severe pain and discomfort. In the worst cases, panniculitis nodules can turn into more serious skin ulcers, known as necrotizing panniculitis.
Fortunately, panniculitis is extremely rare, even in people with Alpha-1, and can often be treated with medications like corticosteroids, antibiotics, and augmentation therapy (described later in the section on treatments for Alpha-1).
Risk Factors for Alpha-1 Antitrypsin Deficiency

Since Alpha-1 is a genetic disorder, you can only get the disease is if you inherit two of the defective AAT protein genes from your parents. Unfortunately, there's nothing you can do to change your genetics if you get the disease, but a healthy lifestyle and medical treatment can have a major effect on how severe symptoms get over time.
People with Alpha-1 who smoke or are exposed to workplace hazards like dust, pollen, mold, and chemical fumes, are much more likely to develop respiratory problems and emphysema that those who aren't. People who have asthma, a family history of emphysema, or get repeated lung illnesses are also more likely to experience complications with AAT deficiency.
Alpha-1 is most common in white people of European and Middle Eastern descent, where up to 1 in 32 people are carriers of the disease. It is much less common in people with Asian and African ancestry.
Treatment for Alpha-1 Antitrypsin Deficiency

Treatments and medications for Alpha-1 antitrypsin deficiency are mostly aimed at preventing progressive organ damage and managing uncomfortable symptoms. The key focus is prevention, because lung damage and liver cirrhosis caused by AAT deficiency is permanent.
People with Alpha-1 usually need frequent medical checkups, a strict healthy lifestyle, and medication to protect their liver and lung function from declining. There is also a special treatment available, known as augmentation therapy, that can treat the underlying protein deficiency in people who have Alpha-1.
Lifestyle Habits to Treat Alpha-1 Antitrypsin Deficiency
Living a healthy lifestyle is an important part of preventing organ damage in people with AAT deficiency. This includes healthy eating, regular exercise, and avoiding substances that are toxic to liver and lungs.
Healthy Diet & Nutrition
Eating healthy, wholesome foods is an important part of any healthy lifestyle, but it's especially important for people with AAT deficiency. A balanced diet ensures that your liver and lungs have all the nutrients they need to stay healthy and work as efficiently as possible.
A healthy diet and portion control will also help you maintain a healthy BMI and avoid health issues like diabetes and heart disease. If you develop liver damage as a result of AAT deficiency, your doctor might recommend a special diet or supplements to help your liver function better.
Vaccinations

There are several vaccinations that are especially vital for people with Alpha-1 deficiency. These include the hepatitis A and B vaccines, the pneumococcal vaccine, and yearly flu shots.
The pneumococcal vaccine helps prevent pneumonia, a serious lung condition that is even more serious for people prone to lung damage and disease. Yearly flu shots are also important to protect the lungs against the influenza virus.
Getting vaccinated against hepatitis A and B protects the liver from deadly viruses that can cause liver damage and cirrhosis. Since people with Alpha-1are particularly prone to liver damage, this is an important precaution to take against liver disease.
Avoid Lung Irritants and Alcohol

If you have Alpha-1, quitting smoking is by far the most important thing you can do to increase your lifespan and prevent lung damage. Even minor lung irritation from secondhand smoke, dust, or mold can cause serious damage over time.
AAT deficiency also makes your liver prone to getting damaged, which is why doctors recommend that people with Alpha-1 avoid drinking alcohol. Excessive alcohol use can cause cirrhosis even in people who don't have the disease.
Here are some common respiratory irritants you should take care to avoid:
- Smoke, including secondhand smoke, from any source (campfires, wood burning stoves, incense, cigarettes, etc.)
- Chemical fumes

