It's safe to say that most people don't look forward to doing chores, but this is especially true for people with COPD. Household tasks are unpleasant enough on their own, but they are much worse when you have to do them while struggling to breathe.
Having COPD means your lungs have to work harder all the time to supply enough oxygen for your body's needs. That means they have to work especially hard when you do physically demanding activities, such as many household chores.
If you're not careful, doing chores around the house can make you feel extremely breathless and fatigued. That's why many COPD patients dread doing housework or avoid doing it altogether.
Unfortunately, household chores are a fact of life and something that everyone has to deal with at some point or another. If you have COPD, it's particularly important to keep your home clean and maintain a healthy environment that promotes healthy living.
However, you shouldn't have to sink all of your energy into housework, especially when there's so many other things in life to do and enjoy. You also don't want to risk worsening your symptoms by over-exerting yourself when you clean.
Instead, you can use simple, practical strategies to make many of your household responsibilities easier to do. You can find a variety of new ways to approach daily chores that can reduce the effort and energy you have to expend.
By strategizing, simplifying, and learning to control your breathing, you can make any kind of housework more COPD-friendly. In this post, we're going to help you get started by showing you a multitude of useful tips and techniques you can use to complete housework with COPD.
In the next sections, we're going to give you general tips and advice for managing your symptoms while you do household chores. We'll also take a look at a variety of specific techniques you can use to simplify tasks and approach your chores in new, more efficient way.
We'll show you how to pace yourself as you clean and make your household responsibilities feel less overwhelming. We'll even give you specific, practical tips you can use right away to make tasks like cooking, doing laundry, and vacuuming easier to do.
In This Article:
- Techniques for Conserving Energy While You Do Household Chores
- General Cleaning Strategies for People With COPD
- Targeted Techniques For Completing A Variety of Chores With COPD
- Doing Laundry
- Dusting and Cleaning Surfaces
- Cleaning the Floors
- Doing Dishes
- Cooking
- Gardening and Yard Work
- Personal Tasks Like Grooming, Showering, and Getting Dressed
If you have COPD, then you have every reason to find ways that you can work smarter instead of harder. By minimizing the toll that household tasks take on your body and ability to breathe, you'll have more energy to invest in other things that matter in your life.
Practical Techniques for Saving Energy When You Do Household Chores
The main symptoms of COPD that get in the way of doing chores are breathlessness and fatigue. Even simple tasks like dusting or doing dishes can make you feel exhausted, especially if you have advanced COPD.
If you don't plan carefully and do too much at once, housework can sap up all the energy you have for the day. And if you have COPD, then you know that your energy is precious and limited, and you should conserve it as much as you can.
In the next sections we're going to share some useful tips for scheduling and pacing your household responsibilities in a way that reduces the energy you have to expend. You'll be surprised at how much of a difference some deliberate planning and organization can do for your energy as well as your peace of mind.
Pacing Yourself is Key
Many people with COPD struggle with reduced energy and endurance. This makes it difficult to stay active for long or do physically demanding chores.
That's why it's important to pace yourself and spread your household chores throughout the day. If you try to do too much at once, you'll end up tired and short of breath, or find that you don't have enough energy to finish your tasks.
Break Tasks Down Into Manageable Chunks

The first part of pacing yourself is figuring out how to split up household responsibilities into manageable chunks. That requires planning ahead so you you can fit everything into your schedule without letting chores pile up.
You can start by planning the most physically demanding chores for times when you know that you tend to have the most energy. Prioritize the tasks that are most important first, and get them out of the way before you end up too tired to follow through.
Your plan should be flexible, however, because you can't always know how you'll feel on any given day when it comes. It's an unfortunate, yet unavoidable, reality that there will be times when you feel too sick or run down to take care of chores.
If your list of chores for the day is too long, you might need to pare it down to avoid exerting yourself too much. After all, overexerting yourself today just means that you'll have even less energy tomorrow to take care of the things that need to be done.
If you don't feel well or have too much on your plate, don't be afraid to eliminate tasks on your list. Instead, delegate them to someone else or plan to do them a different day.
It helps to plan the most difficult tasks for days when you have fewer things to do or more time to spread the steps out throughout the day. It may also help to plan in a “sick day” or two so it's easier to take a day off when yo need u to.
You'll find that one of the best things about having a plan is that it makes managing daily life much less stressful and overwhelming. You'll spend less time worrying about how and when you'll get everything done and more time actually doing things.
Conserve Your Energy

The second part of pacing yourself is taking things slowly so you can keep your energy levels high. If you try to rush or work too quickly, you'll just make yourself fatigued and short of breath.
Move at whatever pace feels most comfortable to you and don't push yourself too hard. Remember that you're in it for the long haul; even if you are feeling good, there's no use in tiring yourself out all at once.
When you move at a slower pace, you can also more easily control your breathing and pay more attention to how your body feels. That allows you to better keep your COPD symptoms under control and recognize when you need take a break or sit down.
When you move slowly, it allows you to chose your movements more deliberately and avoid wasting energy unnecessarily. With some practice, you'll find that your endurance improves when you move at a slower, more steady pace.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Take Frequent Breaks

Finally, another vital part of pacing yourself is knowing when it's time to stop. Recognizing when you need to take a break or slow down will ensure that you have enough energy to make it through all the tasks on your list.
With COPD, it's often best to treat physically tiring tasks as a marathon, not a sprint. Plan on taking it slow, pausing for breaks, and giving yourself plenty of time to rest in-between tiring tasks.
You will know that it's time to slow down when you start to feel breathless, fatigued, or notice other COPD symptoms start to act up. When this happens, take as long as you need to sit down, rest, and get your breathing back under control.
You may also need to take a break from your chores and other responsibilities when you experience a symptom flare up or exacerbation. On days you don't feel well, don't be afraid to take the day off or ask for help from family and friends.
Schedule Tasks With Purpose

If you want to make your household chores more manageable you need to plan your course of attack. This allows you to identify the easiest and quickest way to get everything done.
Start by making a list of all the household tasks and chores you need to do for the day. Whether big or small, write them down so that you can consider them all together, side by side.
This will help you identify tasks that are best paired together and decide how to prioritize each responsibility. Then, you can put together a plan for how you will approach each task throughout the day.
For example, try to plan chores that you do in the same room or area back-to-back, that way you can get them done more efficiently. For example, if you need to clean the kitchen floor and wipe down the kitchen counters, plan to do both tasks in one go.
This allows you to get your supplies out and carry them to the kitchen just once, instead of twice. By pairing relevant tasks in this way, you'll do less moving about and running around from room to room.
You should also take a moment to think about your route through your home as you move from one task to another. This will allow you to identify opportunities to combine multiple small tasks into one.
One way to do this is to think about whether there are any items around that you should take with you whenever you head out of a room. For instance, if you are heading downstairs to clean the kitchen, you might bring some laundry along to throw into your washing machine on the way.
By taking a more calculated approach, you can eliminate a lot of unnecessary work and inefficiencies from your daily routine. You just have to plan ahead, be precise with your actions, and always be looking for ways to streamline different tasks.
Identify Simple Solutions for Tiring Tasks
If you want to reduce the amount of energy you expend doing housework, you have to get into the simplifying mindset. That means paying attention to how you do your chores and eliminating as many difficult steps as possible.
But first, you need to take a moment to really think about which tasks tend to give you the most trouble. After all, you need to be able to wrap your head around the problem if you want to come up with a solution.
When you're going about your day, you might not realize exactly what is wearing you down, only that you feel breathless and fatigued by the time you're done. That's why you need to take time to reflect, step by step, on what sorts of tasks and actions are sapping your energy the most.
Start out by thinking about what kinds of chores you tend to want to avoid and why. Do you avoid them only because you don't enjoy them, or is it because they make you feel tired, or make it difficult to breathe?
Write down a list any chores you identify that leave you feeling fatigued or cause your COPD symptoms to act up more than usual. Then, think about what specific movements or actions make you feel sore, short of breath, or put extra strain on your body.
For example, if you always feel tired after doing laundry, try to pinpoint exactly what it is about doing laundry that makes it difficult. Do you have trouble bending over repeatedly to handle clothes, or do you get breathless carrying armfuls of clothes up and down the stairs?
Often, you can find a way to eliminate the difficult steps or set the task up in a way that makes those steps easier. For instance, if you find stooping over to retrieve things out of lower cabinets tiring, then simply moving those items up to higher shelves is a great and easy-to-implement solution.

Even if the solution seems obvious, it's easy to miss if you're not looking for it. Once you take the time to analyze your methods and explicitly identify the problem, simple answers often makes themselves clear.
If you take the time to think it through, you'll be pleasantly surprised at how many simple solutions you can come up with. Sometimes, all it takes is some thought and organization to make tiring household responsibilities significantly more manageable.
Control Your Breathing
You can help yourself breathe easier while doing chores if you take care to control your breathing while you work. You can do this by practicing COPD breathing exercises like diaphragmic and pursed lips breathing.
We'll go into more detail on how breathing exercises can help you complete chores later on in this article when we talk about specific cleaning tasks and tips. In those sections, we'll show you a variety of ways you can incorporate breathing techniques as you go through the steps to complete different chores.
You can also learn more about controlling your breathing in our more detailed guide, Breathing Techniques for COPD.
Practical Strategies for Completing Household Chores with COPD
Living with COPD requires coming up with many creative solutions to things that the disease makes difficult to do. However, once you make the necessary adjustments, you'll find that you can handle much more than you could before.
When COPD makes your life more complicated, the answer is often simple. By finding ways to use less energy and simplify difficult activities, you can tackle all kinds of household tasks with much more ease.
General Cleaning Tips

In these next sections, we're going to go through a variety of common household chores and give you specific, actionable solutions you can use to make them easier to do. We'll cover everything from dusting and vacuuming to sanitizing surfaces, doing laundry, and more.
But first, let's go over some general techniques that make tackling just about any cleaning task simpler. These tips will help you avoid unnecessary physical exertion and eliminate a variety of minor and major inconveniences.
Use a Pocketed Apron, Tote, or Cart
 |
| Image by Plusea |
Pocketed aprons and rolling carts are indispensable tools that every person with COPD should own. They make all kinds of household tasks easier by allowing you to collect multiple items at once and carry them from place to place in your home more easily.
When you do chores, you can use your apron or cart to gather up all your cleaning supplies and transport them together. That way, you'll never have to take make more than one trip to your supply closet. They can also reduce the amount of bending and reaching you have to do by keeping all of your supplies within easy reach.
A pocketed apron allows you to carry a variety of cleaning tools right on your waist, that way you can keep your hands free while you work. However, it will also add extra weight to your body that you'll have to carry as you move around.
Using a rolling cart is often the best option for transporting multiple items without having to carry the weight yourself. However, carts are more pricey and sometimes less practical when you need to maneuver around stairs and narrow spaces.
If you live in a two story home, you could solve the stairs problem by getting a cart for each level in your house. You could also keep an over-the-shoulder bag or tote by the staircase to help you carry things up and down the stairs.
A handheld tote or tray can also be useful, although they can be heavy to lug around when loaded up. However, they are more useful than aprons for carrying items other than cleaning supplies when you do chores like organizing, picking up, and doing dishes.
Whichever tools you choose, you'll find that you can do tasks much quicker and easier when you don't have to make multiple trips from room to room. It saves time, reduces strain on your muscles, and reduces the total amount of walking you need to do.
Work in a Circle
You can also avoid unnecessary walking by making circular trips around the house. Compared to going back and forth from one room to another, it can significantly reduce the total distance you have to travel.
This is a particularly helpful method to use when you're picking up around the house and have a lot of various items to put away. As you go through each room, put away the items that belong there, and load up any items that belong elsewhere onto your cart. Then, simply deliver the items on your cart to the correct room when you pass it as you make your circle around the house.
Avoid Bending and Stooping
You should keep any items that you have to use often in the most convenient, easy-to-reach places. You shouldn't have to bend over or stoop down to reach tools and supplies you use every day.
For example, it's a good idea to store the cleaning supplies you use most often on shelves that are at waist level or higher. However, you shouldn't store them so high that you have to strain or climb up on a chair to reach them.
Place Stools Strategically Around Your Home
Sitting down while you work can help you conserve your energy and reduce shortness of breath. When you're doing household chores, tall stools are often the most practical seating choice.
High stools are easier to get up from because you can easily move from a seated to standing position without having to lift your body up far. You just have to slide off the edge and straighten yourself up, unlike pushing yourself up from a lower chair.
As you do your household chores, look for stationary tasks that are easy to do while sitting in one place. For example, chores like cooking, washing dishes, or folding laundry are often easy to do sitting down.
It's also nice to have a shorter stool on hand to help you do tasks that are low to the ground. It allows you to reach lower cabinets, shelves, and appliances like the dishwasher and dryer without having to bend over or stoop.

If you don't have any already, consider investing in a couple of stools to place in strategic places around the house. That way, you will always be able to find a seat nearby whenever you need it the most.
Some ideas for areas that could benefit from convenient seating include the kitchen, laundry room, bedroom, bathroom, and closet.
Specific Techniques for Completing Common Household Chores
While the tips we've discussed so far are great starting points for making chores less tiring in general, we still need to address how to do specific chores in a way that's easier with COPD. Luckily, we have a variety of targeted tips and techniques for tackling all kinds of common household tasks with ease.
In the next sections, we'll go into more detail on specific methods you can use to simplify everyday chores like cooking, yard work, and general cleaning tasks. No matter how severe your disease and symptoms, you can make household chores more manageable using some of the following practical tips and techniques.
Doing Laundry

Although most people don't think of it this way, laundry can be a physically demanding task. It usually requires repeated bending, lifting, and walking to haul clean and dirty laundry around the house.
Luckily, there are several ways to reduce the physical demands of washing and putting away your clothes. You can do this by getting better tools and by changing the way that you go about handling laundry days.
Sit Whenever Possible
First of all, consider sitting on a stool while you fold your clothes and when you move them between your washer and dryer. A short stool is often best, because it prevents you from having to stoop down to retrieve your clothes.
When folding or sorting out your laundry, you can also move to a table or counter where you can sit more comfortably. It also helps if you do all your folding at once, that way you don't have to make as many trips back and forth from the laundry room.
Find a Better Laundry Basket

Traditional hand-held laundry baskets are unwieldy and difficult to carry around. If you have limited mobility, balance, or get short of breath easily, it can be very tiring to haul laundry baskets by hand.
Instead, consider getting a wheeled laundry basket so you can roll it from place to place. This makes it easier to walk by taking the weight off your hands and making it significantly easier balance.
A rolling basket may not enough, however, if you have to frequently carry your basket up and down flights of stairs. In that case, consider getting a fabric laundry basket or bag you can sling over your shoulder whenever you need to carry clothes up and down the stairs.
Don't Haul Too Many Clothes at Once

Piles of clothes can get heavy, especially damp or wet clothes out of the washer. If you struggle with the weight, lighten the load by putting a limit on how much you carry at once.
Instead of trying to haul an entire load of laundry across the house, try loading up just one small stack in your basket at a time. It means making more trips, but you might end up less worn out than you'd be hauling heavy baskets around.
You can also reduce the extra work by transporting small stacks of laundry as you do other things around the house. Just remember to grab some clean clothes whenever you pass the laundry room in the direction of where you need to deliver the items.
The same works for dirty clothes too; just try to remember to take an armful with you anytime you leave a room that has dirty clothes. Once you get the hang of it, you'll never again have to make a special trip across the house just for laundry.
Invest in a Front-Loading Washer

Top-loading washers are standard in most homes, but they can be very difficult to use if you suffer fr
.png)
Oxygen therapy, pulmonary rehabilitation, and inhaled medication are the most common treatment options for COPD. They’re proven to significantly reduce respiratory symptoms like coughing, wheezing and shortness of breath, while simultaneously reducing the rate at which COPD progresses.
But if there’s one lesson you can learn about medical conditions, it’s that there’s no “one-size-fits-all” solution. Many patients suffering with COPD have overlapping conditions that may prevent them from experiencing relief using traditional treatment methods, or they might simply be dissatisfied with the results that they experience. At this point, it’s not out of the question to try a different approach like lung surgery.
Lung surgery, especially highly invasive lung surgery, often gets a bad rap in the medical community because it can be dangerous, costly, and time consuming. However, you should never be too quick to write them off, especially when it comes to treating a life-threatening condition like COPD. Millions of people around the world can attest to the effectiveness of surgery for COPD and it’s an area that’s seen some major advancements in recent years.
Whether you’re considering surgery for COPD or you’re just curious what your options are, you’ve come to the right place. In the following sections we’re going to take a look at each of the surgical procedures currently available for COPD, helping you to weigh their advantages, disadvantages, risks, and more.
Who Needs Surgery for COPD?

According to the National Heart, Lung, and Blood Institute, surgery is usually a last resort for someone suffering with COPD. While surgery is an option in all four stages of COPD, it’s most commonly advised only in stage four or “end-stage” COPD. Oftentimes, medical professionals are put in a difficult situation because the patient’s respiratory ailments need to be bad enough to warrant surgery but the patient also needs to be healthy enough for the procedure to go as planned.
Some considerations your doctor will make include:
- Your overall health and health history. Your doctor will want to ensure that you are strong enough to recover after the surgery and that you have a healthy body weight. If you have other conditions that may affect the surgery, you may not be approved for the procedure.
- Your ability and willingness to participate in pulmonary rehabilitation programs. These programs aren’t only great for teaching you how to breathe and exercise correctly, but they provide your doctor with important information about your progress.
- Your age. Surgery is not recommended for patients over the age of 75.
- You’re not a smoker. Smoking is known to cause a number of complications with surgery. It reduces blood flow, slowing the healing process after surgery and puts you at a greater risk of contracting pneumonia and other acute respiratory illnesses.
These are the general guidelines your doctor will use to determine if you’re right for surgery, however, there may be other requirements you have to meet. For example, your doctor may have to perform tests to locate the damaged area of the lung. If the damage is in the wrong area or it’s not localized, you may not benefit from surgery.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What Types of Lung Surgery Are There?
There are four main types of surgery used to treat COPD including bullectomy, lung volume reduction surgery (LVRS), endobronchial valves, and lung transplants. While each of these procedures is very different, they all have the same purpose: to allow the patient to breathe easier, reduce coughing and wheezing, and increase life expectancy and quality of life.

Lung Volume Reduction Surgery (LVRS)
Just like the name suggests, the goal of LVRS is to reduce the size of the lungs. While this may seem counterintuitive since you’re trying to make it easier to breathe, this procedure is used for COPD patients with a very specific type of ailment called hyperinflation where the lungs are in a perpetual state of overinflation. When this happens, it can be difficult to breathe because you won’t be able to fully expel air from the lungs.
How Emphysema Causes Hyperinflation
While hyperinflation can be caused by a number of lung conditions, it’s primarily caused by emphysema. About 3.5 million Americans have emphysema, a condition that causes damage to the alveoli (tiny air sacs) within the lungs. After years of exposure to cigarette smoke and other airborne chemicals, these air sacs begin to expand and become inflamed, impairing their ability to transfer oxygen and carbon dioxide to and from the blood.
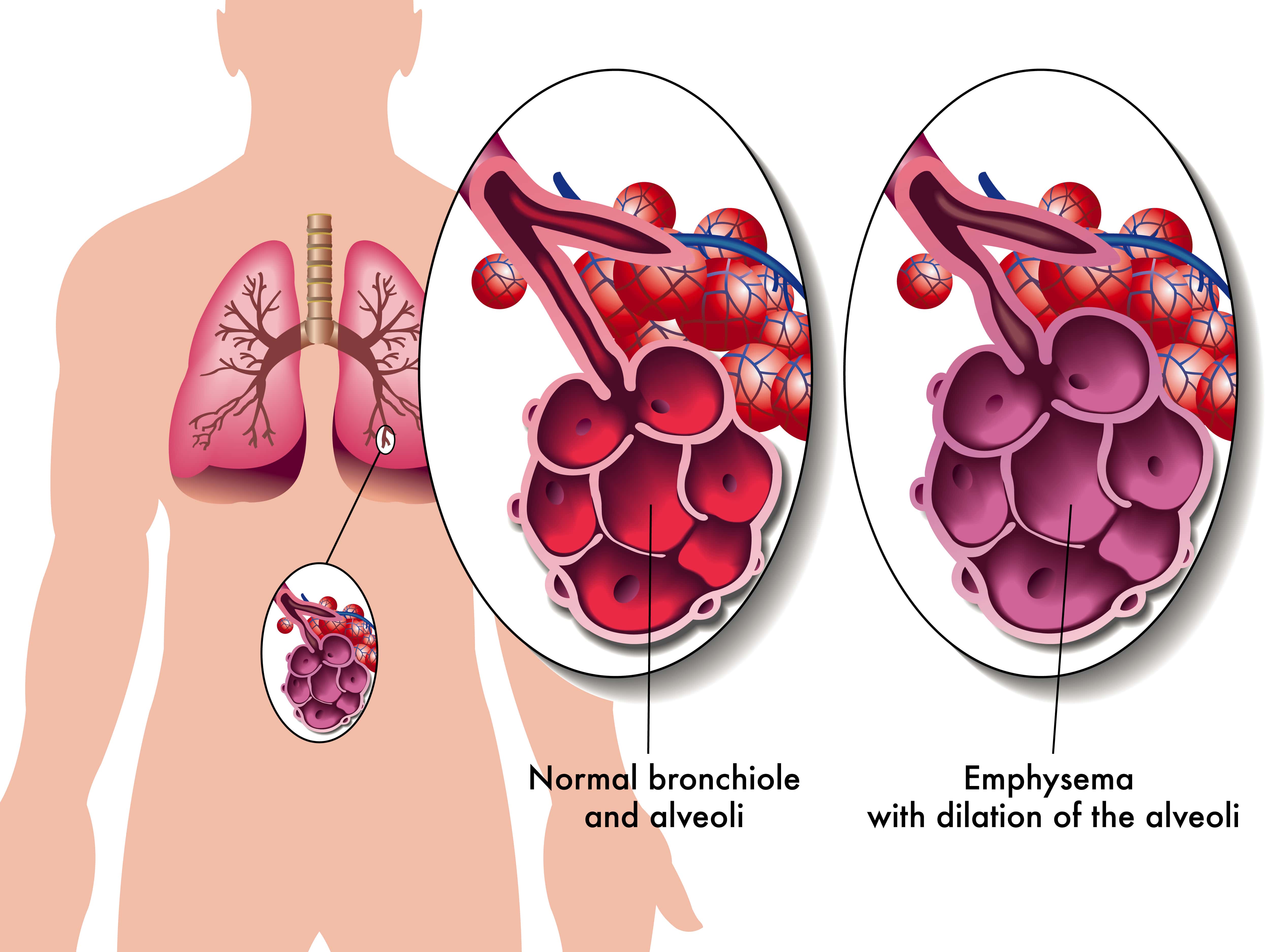
In a healthy person, the alveoli are elastic, allowing gasses to flow in and out of them easily. However, in an emphysema patient, these air sacs are baggy and air can get trapped in them, blocking healthy alveoli that surround it. This is known as “static” hyperinflation and can make it very painful to breathe and causing you to trap carbon dioxide within the lungs.
“Dynamic” hyperinflation is another type of overinflation of the lungs that can either work in tandem with or independently from static hyperinflation. Dynamic hyperinflation is caused by hyperpnea (the increased depth and rate of breathing) or exercise and results in an increase in end-expiratory lung volume (EELV).
Despite every emphysema patient having damaged alveoli, only about 1 - 2% of COPD patients qualify for LVRS. This procedure is typically only advised for patients with severe symptoms like if your FEV1 value (the amount of air you can expel in one second) is below 50%.
Your doctor will likely recommend LVRS if you have upper lobe predominant emphysema. This is a type of centrilobular emphysema that progresses upward, damaging both the upper lobes of the lungs and bronchioles (respiratory passageways).
How Lung Volume Reduction Surgery Works
While it may seem like the bigger the lungs are, the better they are for breathing, it’s not quite this simple. Think of the lungs like a giant sponge. When the lungs expand, they draw in air until they reach their max capacity. Oxygen and carbon dioxide are exchanged in the blood through the alveoli and then you can fully expel the carbon dioxide in the lungs.
Having bigger lungs wouldn’t help you unless you had more functioning alveoli to perform the exchange. So, if part of your lungs is severely damaged, it can actually be causing more harm than good. In the case of hyperinflation, the damaged part of the lungs is actually acting as dead weight that you have to deal with every time you breathe.

The goal of LVRS is to remove that section that’s causing problems and leave only the optimal, high-functioning parts of the lungs. This is typically about 30 percent of each lung, however, it depends on individual circumstances. There are two methods used to complete lung volume reduction surgery:
Sternotomy
This is the preliminary process in many types of heart and lung surgery. During this procedure, an incision is made down the center of the chest wall and the breastbone is separated. After the damaged tissue is removed and the lungs are resealed, the breastbone is put back into place to heal.
Thoracoscopy
Another less invasive method for completing lung volume reduction surgery is a thoracoscopy. During this procedure, several small incisions will be made between the ribs. The surgeon will use a videoscope to monitor what’s going on inside the chest. A stapler and grasper are used to remove the damaged tissue and reseal the lungs.
Bullectomy
A bullectomy is a type of lung surgery used to remove bullae from the lungs. A bulla is a small air bubble that is at least 1 cm in size, but it differs from other abscesses in the body in that it usually forms on the lungs due to something called bullous lung disease. However, occasionally, they can be found in otherwise healthy lungs.
Bullae usually grow over time and the bigger they get, the more they obstruct the function of the lungs. While in most patients bullae are harmless and dissipate with time, in severe cases, medical professionals may resort to a bullectomy to remove the pockets of air on the lungs.

Similar to hyperinflation, bullae affect the alveoli in the lungs. However, in this case, bullae result when the walls of the air sacs break down and form larger ones. These new air sacs don’t assist in transferring oxygen to the blood, and instead end up suppressing and weighing down on surrounding tissue.
Classification of Bullous Lung Disease
If you have COPD, there are two categories of bullous lung disease that you should know about: bullous emphysema and vanishing lung syndrome.
- Bullous emphysema is the classification of bullae that form in emphysematous lung parenchyma. This is characterized by the formation of multiple adjacent bullae which are the result of the progressive loss of alveolar attachments. 80 percent of patients with bullae have associated pulmonary emphysema.
- Vanishing lung syndrome got its name because on X-ray, it makes it look like the lungs are disappearing. This condition commonly affects young male smokers and is characterized by a large emphysematous bullae on the upper lobes of the lung. VLS is uncommon and usually requires a bullectomy for treatment.
When bullae form in normal lungs, they usually form on their own and are surrounded by healthy tissue. Although health experts are not quite sure what causes this type of bullae, it’s likely caused by some type of focal anatomic defect that causes progressive air trapping. Even with bullae, many patients still experience normal lung function.
How a Bullectomy Procedure Works
If the bullae found on your lungs are progressing quickly or they’re obstructing your breathing, you may qualify for a bullectomy. This procedure is much less intrusive than other types of lung surgery and can be completed using video assisted thoracoscopic surgery (VATS), also known as videoscopic surgery.
Endoscopic Lung Volume Reduction
While not technically “surgical,” valve therapy (endoscopic lung volume reduction) is often used as an alternative for lung volume reduction surgery. The basic premise of these valves is to prevent air from entering diseased areas of the lung while allowing air to exit freely. By doing so, the patient will be able to maintain an equilibrium with each breath and prevent hyperinflation of either lung.
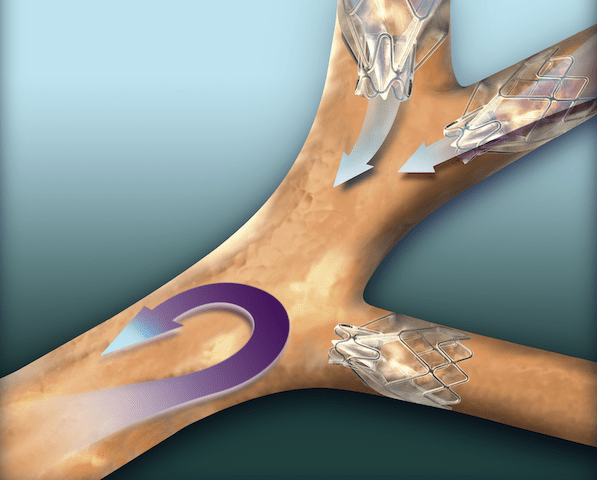
Zephyr valves, produced by PulmonX, are the most widely accepted and successful endobronchial valves on the market. And since the first successful implant in 2001, the company has developed a number of technologies to assess emphysema patients and provide better treatment.
Aside from being minimally invasive, one of the major benefits of endobronchial valves is that they can be repaired, removed, or adjusted as needed. Whereas lung volume reduction surgery is permanent, specialists are able to easily remove and repair endobronchial valves, move them around, or replace them entirely with a simple procedure.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}Lung Transplant Surgery

Last but certainly not least, we have lung transplant surgery. Despite being one of the most discussed surgery options for COPD, it’s far from being a common procedure. According to the 2015 report from The Registry of the International Society for Heart and Lung Transplantation, just over 17,000 patients had lung transplants for COPD between 1995 and 2014. This is a small fraction of people with COPD.
Because lung transplants are some of the most invasive and complicated procedures surgeons can perform, there is a long list of criteria that must be met before a patient will even be considered. Patients must be screened before the operation to ensure they don’t have any active infections or other health issues that could lead to complications.
When are lung transplants advised?
Permanently damaged lungs can significantly reduce someone’s quality of life. There are many treatment options like oxygen therapy and pulmonary rehabilitation which can increase your quality of life and help you live normally again. However, when all these other options fail and your doctor knows you won’t get better without surgery, he/she may recommend a lung transplant. Some of the most common reasons to have a lung transplant include:
- Cystic fibrosis
- Pulmonary hypertension (high blood pressure in lungs)
- Lung scarring (pulmonary fibrosis)
- Chronic obstructive pulmonary disease
Lung transplants are almost always a last resort option for treating these conditions. Your doctor may perform a number of tests to determine if other surgeries or medications are an option. Surgeries like lung volume reduction are far less invasive, costly, and time consuming, and they may provide you with the same or comparable benefits.
Risks of lung transplant surgery
Due to the intensiveness of lung transplant surgeries, there are many risks associated with them. Your doctor will be very precise and thorough when describing how to prepare for the procedure in order to reduce risks and leave as little room for error as possible. Before you even consider lung transplant surgery, it’s important to understand the risks involved.
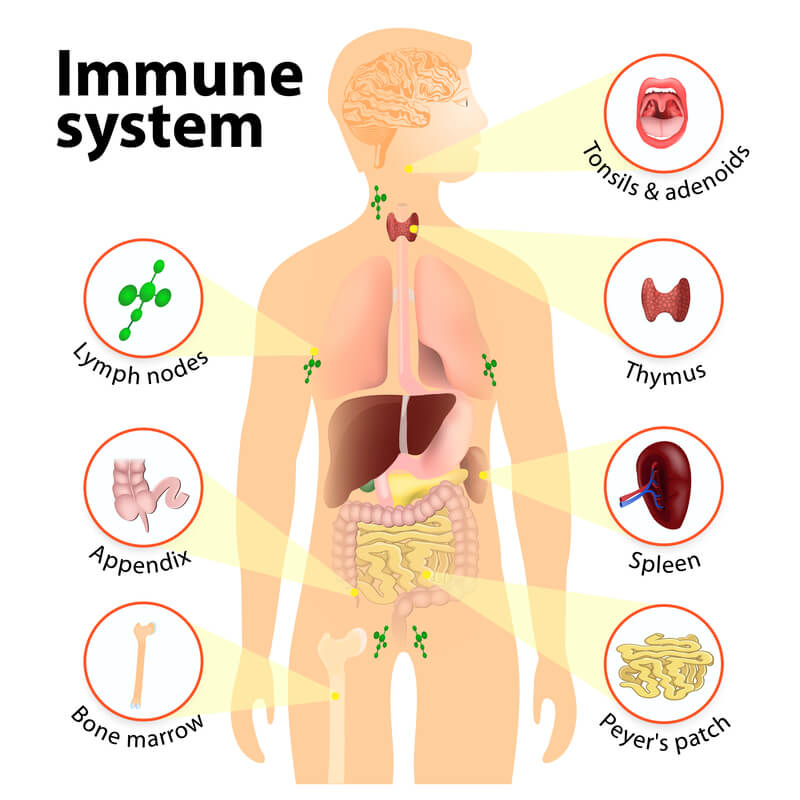
Lung Rejection

Your body is naturally equipped to fight infections and foreign substances using both your adaptive and innate immune system. While everyone’s immune system has its strengths and weaknesses, most tend to recognize the transplanted organ as a “foreign object.” When this happens, it can lead to organ failure. This is more likely to happen immediately after surgery and becomes less frequent as time goes on.
There are several different types of lung rejection that can happen after a lung transplant. Acute rejection is an immediate reaction to the new lung or lungs and is fairly common. As such, your doctor will be closely monitoring your progress after the surgery and you should ensure that you’re taking the immunosuppressive drugs that you’re given which will help your body accept the new lungs.
Another type of rejection is chronic lung allograft dysfunction (CLAD), or long-term lung rejection. This condition usually results in airflow restrictions or obstructions and can have symptoms ranging from mild to severe. One of the most common types of chronic lung rejection is bronchiolitis obliterans syndrome (BOS), a condition causing inflammation that affects the bronchioles, the smallest airways in the lungs.
Infection
Infection is another risk after lung transplant surgery. Your doctor will provide you with a plan that suppresses your immune system so that the lungs aren’t rejected, but this will also make you more likely to get sick. Contracting acute respiratory illness may also exacerbate any issues your body is having with accepting the new lungs, so it’s important to stay healthy.

Fortunately, lung transplants have become much safer within the past several decades. According to the U.S. Department of Health and Human Services, the one-year survival rate of a lung transplant patient was 45 percent in 1990. Since then, survival rates have risen to 83 percent, meaning transplants are a much more viable option than they were in the past.
How To Get Started
COPD is a debilitating respiratory condition that affects millions of people across the world. For some, COPD symptoms are not bad enough to warrant lung surgery, but for others, especially those in stage 4, surgery may be the only effective way of seeking relief. Whether you’re preparing for an upcoming surgery or surgery is something you may be considering in the near future, there are a few things you can do right now to prepare.
Speak With Your Doctor
Before you do anything else, it’s important to first consult with your primary care physician and pulmonologist. Many patients tend to rush into things only to be disappointed when they find out they don’t need or qualify for surgery. On the other hand, some people are terrified by the thought of surgery and try to avoid it meaning they could be missing out on a great opportunity to seek relief from their symptoms.

The more open and honest you can be about how you’re feeling and what symptoms you’re experiencing, the better your doctor will be able to align you with a treatment plan that works for you. Because surgery is so costly and time consuming, your doctor will likely try many other options before resorting to surgery.
Quit Smoking
Smoking is the primary cause of some of the world’s deadliest lung diseases including COPD and lung cancer — but the problems don’t end there. Smokers are also at a much higher risk of contracting type 2 diabetes, cataracts, strokes, heart disease, and complications during lung surgery.

According to the Truth Initiative, an organization dedicated to promoting tobacco-free living, smoking decreases blood flow and alters the immune system making it difficult for your body to heal properly. And because surgery is such a precise process, doctors will want to eliminate any potential risks they can before they begin. While some surgeons may operate on someone who has smoked recently, it’s in your best interest to stop as soon as possible.
Exercise

Pulmonary rehabilitation is an effective method of reducing shortness of breath, fatigue, and depression in COPD patients. And according to a study by the Journal of Thoracic Disease, preoperative pulmonary rehabilitation is also an important process increasing exercise tolerance before surgery. The study concludes that exercise capacity reduces both postoperative complication risk and the amount of time patients spend in the hospital after a surgery. Additionally, preoperative exercise increases muscle mass and reduces fatigue which can also help with the healing process post-surgery.
Eat Right
Your diet plays a crucial role in your body’s ability to manage and treat COPD symptoms like breathlessness, fatigue, and chest pain. Many COPD patients report feeling weighed down and weak when they don’t get the right nutrients in their body, and this is no different when it comes to preparing for a surgery.

.png)
Despite smoking being the cause of 80 percent of cases of chronic obstructive pulmonary disease (COPD), 38 percent of COPD patients report that they still smoke. These are staggering statistics and show the powerful addictive effects of nicotine and other harmful chemicals found in cigarettes.
Unfortunately, many people suffering with smoking addiction today are people who grew up in a time when smoking was hip, cheap, and socially acceptable. All the regulations that we now have on cigarette advertising and sales were nonexistent in the 50s and 60s and the awful side-effects of that era are still haunting us in the 21st century.
The good news is that youth smoking rates have dropped significantly, indicating a change in stigma towards cigarette smoking in newer generations. According to data by the U.S. Department of Health & Human Services (HHS), the percentage of 12th-graders who smoke cigarettes decreased dramatically from 25 percent in 1997 to just five percent in 2018.
While this decline is — at least in part — due to the increase in popularity of vaping and e-cigarettes, it’s also due to an increased awareness of the harmful effects of smoking. But while young people may be constantly exposed to information about smoking, older Americans may not be hearing the full story.
Whether you or a loved one has COPD, lung cancer, or any other respiratory condition, now is the time to quit. Smoking cessation will have a significant and immediate impact on your well-being, systemic health, and will make respiratory symptoms easier to manage while reducing the rate at which your disease progresses. In the following sections, we’ll outline all of the health benefits to smoking cessation, especially as it relates to current COPD patients.
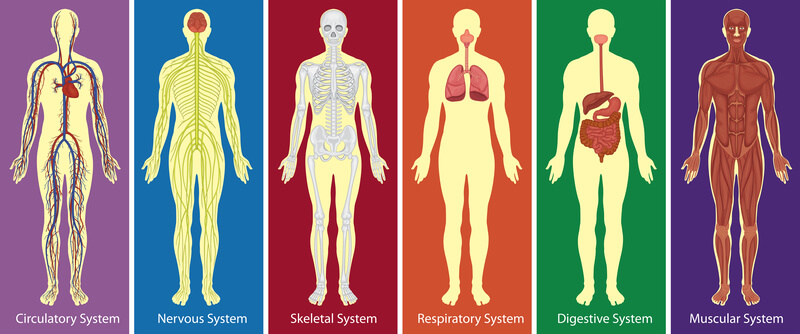
Improved Pulmonary Health
Out of all the parts of the body that are affected by smoking, the lungs are by far hit the hardest. Your lungs are one of five vital organs and they’re responsible for oxygenating your blood and removing carbon dioxide from the body through respiration. Because the respiratory system is made up of so many different components, smoking can have a number of effects like irritating the larynx or trachea, swelling and narrowing of the airways, and permanent damage to the alveoli.
When air enters the lungs through the bronchial tubes and enters one of the lobes, it passes to the alveoli where the exchange of oxygen and carbon dioxide takes place. Capillaries are blood vessels found in the wall of the alveoli that transport oxygen to the heart, and then throughout the body. Your pulmonary health includes anything that affects your airways, lobes, alveoli, bronchioles, and pulmonary arteries.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Reduced Inflammation
Inflammation is an immune response in the body. When there is an injury, infection, or toxins in a certain part of the body, chemicals are released from the white blood cells. This signals the body to send more blood to the affected area, causing it to become red, swollen, and warm. And while acute inflammation is a key process in our body’s immune response, chronic inflammation can cause serious medical issues if it’s not treated.
COPD is one of the primary diseases associated with chronic inflammation in the lungs. It results in permanent and irreversible damage to the airways and alveoli in the lungs. While the inflammation associated with COPD is not curable, many studies have shown that the inflammation resulting from smoking is curable.
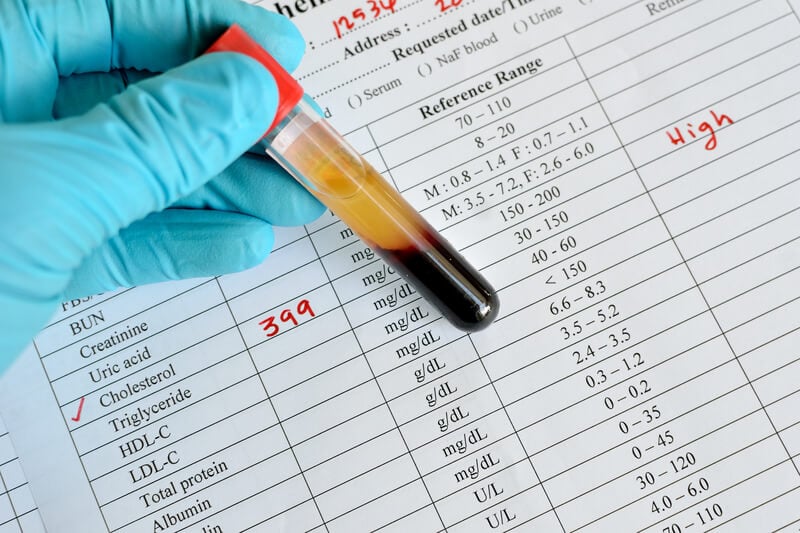
Smoking causes an increase in white blood cells and C-reactive protein (CRP) production. The CRP is a protein created in the liver and sent through your bloodstream in response to inflammation. In order to test for the presence of an autoimmune disease, doctors may perform a CRP test. While low levels of CRP are normal, high levels could be a sign of a bacterial infection, autoimmune disorder, or fungal infection.
According to a study published in the National Center for Biotechnology Information, CRP levels are elevated in smokers but there is no correlation between the amount of cigarettes smoked and CRP levels. What’s more, another study published in the same journal found that inflammatory responses returned to normal five years after a smoker quits. What this means is that even if you’re only smoking once a week, you will most likely have higher levels of CRP, and the only way to reduce it is through long-term smoking cessation.
While there’s still a lot of research that needs to be done on chronic inflammation and smoking, it’s clear that smoking has a direct and negative impact on the body’s natural immune response. While the lungs may never fully recover from this damage, the inflammation can be reduced with immediate smoking cessation.
Reduced Carcinogen Exposure
A carcinogen is anything that could potentially result in the process of carcinogenesis — the formation of cancer — in the body. Although it’s impossible to live your life without being exposed to some carcinogens, smoking is the greatest avoidable risk factor for carcinogen exposure.

In cigarette smoke, there are around 4,000 chemicals. 70 of these chemicals are carcinogenic and either cause, initiate, or promote the growth of cancer. Some of these chemicals include:
- Benzene
- Arsenic
- Aromatic amines
- Acetaldehyde
- Chromium
- Ethylene oxide
- Formaldehyde
Out of all of these carcinogens, perhaps the most studied is benzopyrene. Researchers have found that this chemical attaches itself to the DNA in cells layering the lungs. When benzopyrene enters the body, it’s processed by enzymes allowing it to be excreted through urine. Known as epoxides, these water-soluble forms of benzopyrene attach to DNA and mutate them.
Epoxides don’t just affect the lungs, however. Because they’re passing through other parts of the body, smokers are more likely to experience liver cancer, bladder cancer, and oral cancer as well. Although cells are able to combat some of the effects of the epoxides, some of them result in adducts, or attachments on DNA that are replicated, causing cancer.
The “Smoker’s Signature”
Bound by hydrogen bonds, a guanine base and cytosine base combine to create a base pair in DNA replication. However, when DNA is replicated with an adduct, it replaces the cytosine base with an adenine base. This results in something called a G-to-T transversion which can be seen as a sort of ‘typo’ in the world of genetics. And because G-to-T transversions have become so common among smokers, they’re often known as the ‘smoker’s signature.’
Unfortunately, benzopyrene isn’t just found in cigarette smoke; it’s produced with the combustion of other organic materials like coal tar and even grilled meats. Although smoking is the leading risk factor for lung cancer, everyone should make an effort to avoid inhaling airborne pollution, because there’s a good chance it has carcinogens in it.
Improved Cardiovascular Health

Smoking doesn’t just impact the lungs, it has a detrimental effect on the whole body including the heart. Smoking and being exposed to secondhand smoke can damage the blood vessels that transport blood throughout the body and when it affects your body’s ability to bring blood to or away from the heart, it can result in a heart attack, stroke, or death.
Reduced Risk of Heart Disease
Heart disease is the leading cause of death worldwide and about one fifth of all deaths by heart disease are caused by smoking. According to Hopkins Medicine, smoking contributes to a number of risk factors for heart disease including atherosclerosis, blood clots, and abnormal heart rhythms.
The chemicals found in cigarette smoke damage your blood cells and can alter the structure of blood vessels. Most often, this will result in a condition called atherosclerosis characterized by plaque buildup in the arteries. This plaque eventually hardens and forms a clot that can narrow or completely block your arteries.
If this plaque affects the coronary arteries, which carry blood to the heart, it’s known as coronary heart disease (CHD). This can result in a heart attack, heart failure, and even death if it’s left untreated. Other arterial diseases like peripheral artery disease (PAD) may result if the blood clot impairs an artery that carries blood to the head, limbs, or other organs throughout the body. Someone with PAD is at risk for a stroke and heart disease.
Lower Blood Pressure
It’s a well-known fact that smoking increases blood pressure (hypertension). This is the result of two primary functions: peripheral vascular resistance and cardiac output. In other words, your heart is pumping more, and there is increased resistance in the arteries. Studies have shown that both cardiac output and peripheral vascular resistance are acute symptoms of smoking, meaning when you stop smoking, these symptoms go away.

A study published in the American Heart Association journal examined smokers over a course of 24 hours. The researchers observed that both heart rate and blood pressure were significantly lower in periods of no smoking than in periods where the person was smoking. So, not only does smoking have long-term effects on your heart health, you’re also at a much higher risk of experiencing a heart attack or stroke while smoking a cigarette.
Improved HDL Cholesterol Levels
High-density lipoprotein cholesterol, also known as the ‘good’ cholesterol, plays an important role in your cardiovascular health. It’s responsible for gathering up other cholesterol and bringing it back to the liver to be broken down and removed from the body. However, when HDL-c levels are low, there isn’t enough to remove that cholesterol resulting in plaque buildup and eventually blood clots.
Studies have shown that smoking leads to lower levels of HDL-c and that cessation can bring cholesterol levels back to normal. Smoking interferes with several processes including HDL metabolism, subfractions, catabolism, biosynthesis and maturation, and intravascular remodeling of HDL. Smoking cessation will restore the protective functions of HDL and prevent it from becoming atherogenic.
Healing Damaged Heart Tissue
Smoking puts a significant amount of stress on the heart. Carbon monoxide in cigarette smoke enters the bloodstream and reduces oxygen levels in red blood cells. Once it reaches the organs throughout your body, they’ll have less oxygen to work with, and your heart will need to work harder to ensure your body gets the nutrients it needs.
The narrowing of the blood vessels due to nicotine and increased blood pressure and plaque buildup can also cause damage to the heart and reduce your exercise tolerance. However, the good news is that right when you stop smoking, your body will slowly begin to heal. Blood pressure will immediately drop, oxygen levels will increase, and there will be much less stress on your heart and arteries.
Improved Systemic Health
Your lungs and heart are the two most important things to consider when it comes to the effects of smoking on your body. However, cigarette smoke damages your whole body in some way or another and you may be surprised at all the negative effects it can have.
Lowered Risk of Type 2 Diabetes
With type 2 diabetes, your body has an impaired ability to metabolize glucose by either not producing enough insulin or altering the effects of insulin. And according to the Centers for Disease Control and Prevention, smokers are 30 to 40 percent more likely to develop type 2 diabetes than those who don’t smoke.
Type 2 diabetes can lead to many complications including damage to the kidneys, eyes, nerves, while also increasing your risk of stroke and heart attack. Smoking causes this disease through something called oxidative stress, an issue that arises when the chemicals in cigarette smoke mix with oxygen in the blood. Inflammation is thought to be another major cause of type 2 diabetes.
Improved Oral Health
Chewing tobacco isn’t the only thing that causes oral health issues; cigarette smoking is also a potential risk. What’s more, smokers are at a higher risk for periodontal disease, bone loss, and other common oral health issues that can lead to tooth loss at a younger age. Cigarette smoke can also stain your teeth and give you bad breath.

Gum disease is one of the most common oral health issues in the world and results from the growth of bacteria and plaque that develops on the teeth. Severe gum disease can result in gum recession and tooth loss. And because smoking impairs your body’s natural ability to fight off infection, it raises your risk for gum disease even if you brush and floss regularly.
Improved Eye Health
According to the New York Department of Health, smoking is a risk factor for eye diseases like age-related macular degeneration (AMD), cataracts, glaucoma, and diabetic retinopathy. There are a number of ways smoking affects the eyes. For example, the smoke can irritate your eyes and cause an allergic reaction similar to pollen or any other airborne pollution.

Another reason for eye health complications is artery occlusion or the sudden blockage of blood to the retina due to high blood pressure or diabetes. Smoking can also cause damage to the optic nerve resulting in vision loss or blindness and a reduced supply of antioxidants in the eye that can lead to cataracts.
Improved Bone Health
It’s natural for bones to change and evolve as we age. From childhood all the way through adulthood, our bones are developing. However, if bones start to weaken and become brittle, this is known as osteoporosis. In a healthy person, the production of bone matter is faster than the rate at which it is lost. In someone with osteoporosis, however, the bone cells begin to dissolve and bone loss is faster than bone growth.

According to WebMD, smoking generates a lot of free radicals in the body that causes overwhelming damage to the body. Hormones that keep your bones strong and healthy are set off balance and damaged blood vessels prevent your bones from getting the oxygen they need to grow. Osteoporosis is already common in old age so smoking will only cause it to take hold faster.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa')}}
Weight Regulation

Weight loss is extremely common among COPD patients. There are a number of reasons for this and we cover it in detail in our post How To Maintain A Healthy Weight With COPD. In short, increased lung volume, difficulty breathing, and anxiety caused by COPD along with atrophy (muscle loss) leads to a reduced appetite. When this is combined with the nicotine in cigarettes — an appetite suppressant — this can have catastrophic results. Being underweight can be just as unhealthy as being overweight, so smoking cessation is an important step towards maintaining a healthy weight.
Strengthened Immune System
We’ve already covered how smoking causes chronic inflammation, but what about how it affects your body’s ability to fight off infection? In short, smokers are much more susceptible to various types of chronic disease than non-smokers are. Tobacco compromises the antibacterial properties of leukocytes, a cell that circulates through the blood and fights foreign substances.
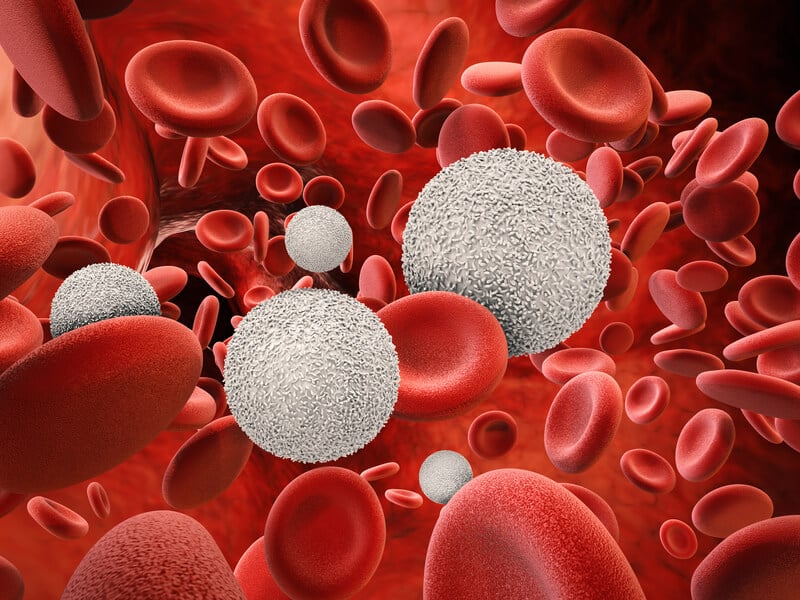
Reduced immune function is especially a concern for someone with COPD where any type of sickness can lead to an exacerbation or be the cause of a serious medical emergency. COPD already results in an increased risk of lower respiratory tract infections, so smoking will only make this worse.
Improved Mental Health
While there’s a seemingly endless list of negative health risks associated with smoking, it’s important to not forget the burden of smoking on your mental health as well. While many people think of cigarettes as something that will reduce stress and anxiety, recent studies have found that the opposite is true. And like any other drug, tobacco can alter your brain chemistry to increase irritability and lead to other mental health problems.
Reduced Stress and Anxiety
How many times have you heard someone say they need to “take a break” and go outside to smoke? Unfortunately, many smokers are tricked into believing smoking reducing anxiety, when in reality, it’s doing the opposite.
According to the University of East London, smokers normalize the experience of smoking while the periods between cigarettes are characterized by worsening moods and anxiety. As a result, many smokers believe cigarettes are alleviating these symptoms when it’s actually causing them.
Improved Self-Image

According to a pulmonologist at Bikram Hospital, Dr Vasunethra Kasargod, “smoking starts as a choice, but eventually becomes a compulsion.” While compulsions may feel nice at first, they eventually make you feel out of control of your own well-being and happiness. Over time, this will lead to a poor self-image and cause you to question your worth.
As an alternative, try embracing things that you can control and that feel constructive rather than destructive. While smoking can give you immediate satisfaction, you will experience a lot more long-term satisfaction the longer you go without a cigarette.
Better Relationships
Smoking can take a huge toll on your relationships. Whether you live with a friend, significant other, or family member, constantly going out for a smoke break or getting the smell of cigarette smoke around the house can be difficult to deal with. According to the Association for Psychological Science, people who have better relationships are happier and less stressed.

Another reason to quit smoking is because it shows that you’re serious about recovering. People will be more likely to help out if they see that you’re doing everything you can to help yourself, and the most basic way to help yourself is to avoid the habit that’s most likely to cause COPD.
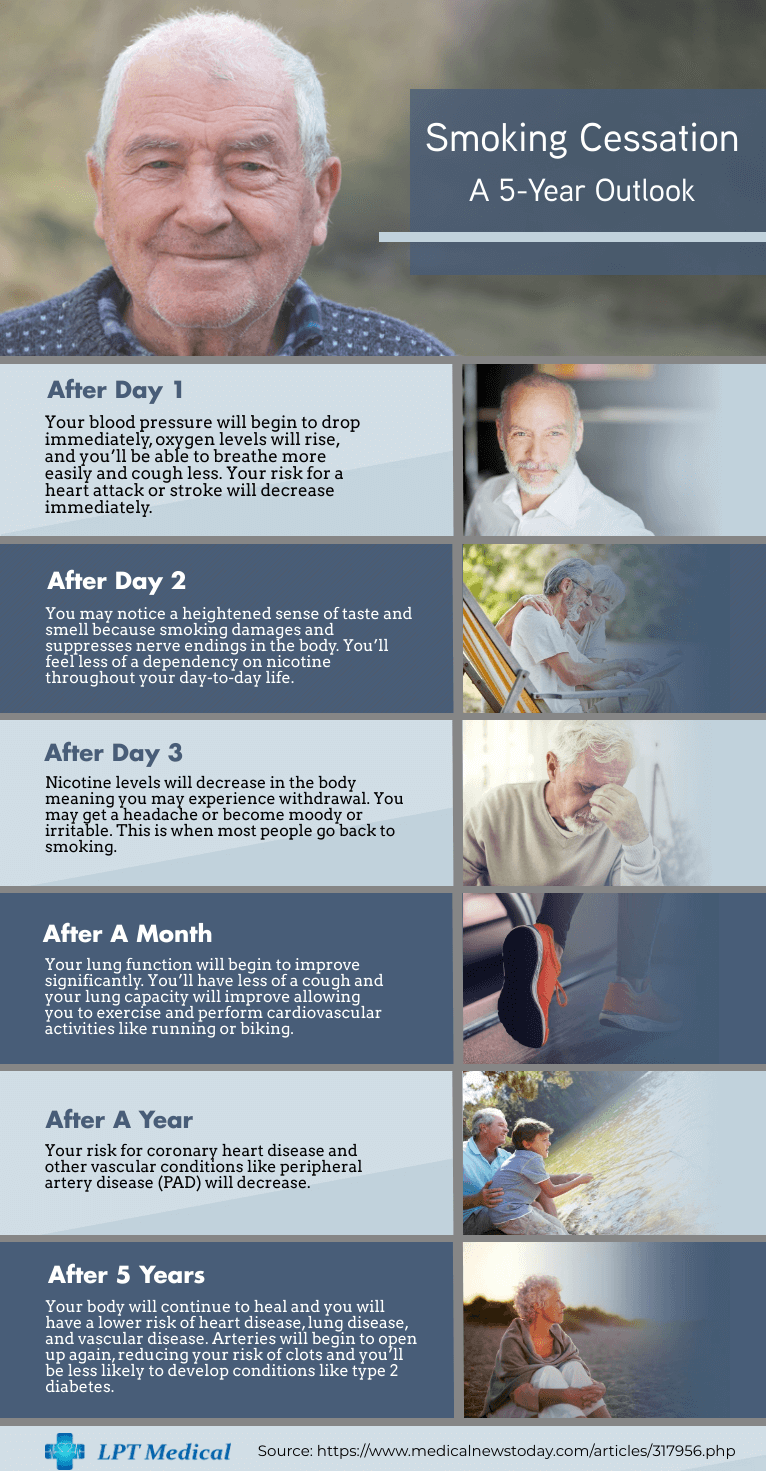
Smoking Cessation Timeline
If you’re more interested in the immediate effects of smoking cessation, you’ll be happy to know that there are plenty of them. There are a number of things that take place from the moment you put down your last cigarette to five and even ten years after the fact. Let’s take a look at the smoking cessation timeline.
Why Is It So Difficult To Kick The Habit?
Many people wonder what exactly causes cigarettes to be so addictive. We all know that nicotine is addictive, but can it really be addictive enough to keep us smoking even when we know it’s harmful to our health? The truth is, it’s not just nicotine that’s causing smoking addiction — cigarette companies have been altering their products for years to make them more addictive, less harsh for new smokers, and more deadly than ever before.

.png)
Chronic obstructive pulmonary disease (COPD) affects millions of people around the world. It’s a lung disease characterized by difficulty breathing, coughing, wheezing, chest pain, and more. While there is no cure for COPD, its symptoms can be reduced significantly by following a strict treatment plan designed by your doctor.
In our blog, we’ve discussed many topics about living with COPD such as shopping and cooking, completing household chores, and even living a more fulfilling life. But what about COPD patients who aren’t able to do these daily tasks without help? After all, COPD is a debilitating disease and for many people, doing the things they once could are simply no longer possible — this is where caregivers come in.
While you may think of a caregiver as someone hired by a home healthcare company, in reality, most caregivers are friends or family members who take time out of their busy day to help a loved one. Oftentimes, caregivers are people who are working full-time or part-time jobs, have kids, a spouse, or other commitments to attend to, so if you’re thinking of taking on the role of a caregiver, you need to be able to manage your time effectively.
Unfortunately, for this type of caregiver, there is no type of training to help prepare you for the task ahead. Being a caregiver means taking things one day at a time and adapting to the needs of your loved one as they age and their condition changes. At the same time, it’s important that you don’t forget the relationship you have with this person. In other words, just because you’re caring for someone doesn’t mean you can’t still be their son, daughter, grand kid, or friend.
In the following sections, we’re going to discuss the importance of caregiving for COPD patients, what you should know to get started, and some helpful tips to manage your time more effectively. It’s important to remember that you’re not alone in becoming a caregiver. According to the COPD Foundation, there are 65 million family caregivers nationwide who spend 20 hours a week on average caring for a loved one, so if you have any questions, consult online forums like AgingCare or speak with a pulmonary specialist.
Getting Started as a Caregiver for COPD
For many people looking to help a friend or loved one through caregiving, knowing where to get started can often be the hardest part. While you want to provide them with the best care you can, you still have your own life to manage, so finding the right balance should always be your first step.
Determine If You’re The Right Fit
One thing you should immediately ask yourself when presented with the prospect of caregiving for someone with COPD is, “Am I the right fit?” While you may be fully capable of taking on the challenge, that doesn’t necessarily mean your busy life will allow it.
Many people have children to raise, jobs to work, or other tasks to attend to, so the more honest you can be to yourself and your loved one about the feasibility of becoming a caregiver, the better. It’s best to find an alternative now rather than realizing three or four months in that you won’t be able to take care of them. Chances are, if it means sacrificing your relationships with friends, family members, or your job security, then finding another option is not out of the question.

Start by reaching out to home care providers in your area. While in-home care can be expensive, you need to consider all your options and remember that many health insurance companies, including Medicare, cover some form of home health services. Depending on your specific needs, it may be covered through either Part A or Part B of Medicare and includes care provided by a home health aide, therapy, and intermittent skilled nursing care.
It’s unlikely that you will get reimbursement from your health insurance if your loved one isn’t homebound, meaning they aren’t able to leave the home without extreme difficulty. Another thing to note is that you will need a signed home health certification from your doctor in order to be covered. If you’d like to learn more about this process, visit Medicare Interactive’s home health services page.
Allocating Your Time
Now that you’ve taken the time to consider hiring a home care provider, you need to start allocating time on your schedule. If you’ve hired a home care professional, you may only need to be there with them for a certain period of time each day. At this point, it’s just about finding this time in your schedule and making sure people are aware that you won’t be available during those times.

Staying organized will make all the difference in the world when you become a caregiver because it will ensure that you’re always prepared for whatever challenges you may face. If you’re organized, you’ll be able to more easily schedule doctors appointments, make yourself available for emergencies, and ensure your loved one is attended to when they need it.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Doing Your Research
Researching COPD is one of the most important steps when preparing to be a caregiver. Generally speaking, the more educated you are about the disease and its unique symptoms, the better prepared you will be to deal with emergencies associated with it. There are two forms of COPD, emphysema and chronic bronchitis.
.jpg)
Emphysema
In the lungs, there are tiny air sacs called alveoli. Oxygen passes through the alveoli walls and enters the bloodstream when you breath. However, in someone with emphysema, these tiny air sacs are damaged and they’re less efficient at transferring oxygen to the blood. This results in symptoms like low blood oxygen levels, shortness of breath, persistent cough, fatigue, and excessive mucus production.
Chronic Bronchitis
Although chronic bronchitis has similar symptoms to emphysema, it’s a condition that damages the bronchi, the tubes that carry oxygen into the lungs. While the main symptom of emphysema is shortness of breath, the main symptom of chronic bronchitis is a frequent cough, usually accompanied by mucus. Many COPD patients have varying degrees of both these conditions.
Stages of COPD
Aside from the types of COPD, you should also be aware of the stages of COPD. Unlike many other lung conditions, the stages of this disease progress slowly over many years. Although someone with mild COPD may experience very few symptoms, someone with severe COPD can experience symptoms that are much worse and can even be life threatening.

Stage One
In the first stage of COPD, symptoms are so mild that many cases go undiagnosed. According to lung.org, millions of people may be experiencing the early stages of COPD and not even know it. Symptoms include breathlessness, chronic cough, and fatigue.
Stage Two
In the second stage of COPD, breathlessness, persistent cough, and mucus becomes more pronounced. While symptoms may be debilitating, people often brush them off as a natural part of aging.
Stage Three
By stage three, most people have sought help and realized that they’re dealing with a serious respiratory condition. Stage three is characterized by more difficulty breathing, chronic cough, headaches, fatigue, and increased likelihood of exacerbations. Oxygen therapy is likely needed at this point.
Stage Four
The fourth and final stage of COPD is considered “severe.” Patients in this stage need to follow a strict diet, undergo oxygen therapy and pulmonary rehabilitation. The symptoms include significant difficulty breathing, cardiovascular issues, chest tightness, wheezing, and severe and often life-threatening exacerbations.
These are just a few of the things you should know about each stage of COPD. If you’re going to be a caregiver to someone with COPD, you’ll need to know exactly what stage they are in and what symptoms they are experiencing. If you’d like more details about each stage, please refer to our blog titled: The 4 Stages of COPD: What You Need to Know.
Speak With Their Doctor
Besides doing your own research on COPD, your loved one’s doctor or pulmonary doctor will be your best resource for any type of information regarding his/her disease. When you become a caregiver, you should expect to be the primary point of contact with their doctor because they may be unable to do so.

Before each doctor’s visit, it’s a good idea to sit down with your loved one and write up a list of questions to ask. It’s much easier to get all your questions answered during your visit than to have to keep calling him or her for information. However, if it’s your first time visiting with the doctor for COPD, you can find a great list of questions to ask in our blog, “16 Questions You Should Ask Your Doctor About COPD.”
Understanding The Unique Needs of a COPD Patient
Chronic obstructive pulmonary disease is unique in that it can’t be cured, but its symptoms can be significantly reduced with proper treatment. As a caregiver, you have the opportunity to have a significant impact on a patient’s life, not just by performing daily tasks, but by helping them maintain the treatment program set forth by their doctor. What’s more, there are a whole host of home remedies you can try to improve the quality of life of your loved one.
Symptoms and Exacerbations
Before being diagnosed with COPD, many people believe that their symptoms are a natural part of aging. Whether they have emphysema or chronic bronchitis, COPD symptoms are often confused with acute diseases like pneumonia or the common cold. However, when these symptoms last more than a couple weeks, it’s usually a sign that you’re dealing with something more serious. Caregivers need to learn to recognize the symptoms of COPD and COPD exacerbations so they can better treat them or prevent them altogether.
What is an exacerbation?
An exacerbation is a sudden flare up of lung symptoms. Typically, an exacerbation is triggered by either an external factor like air pollution or an internal factor like an infection or virus. So, as a caregiver, you need to make sure you’re doing everything you can to prevent your loved one from getting sick or being in an environment that could cause a COPD exacerbation. In end-stage COPD, exacerbations can be fatal, so they’re often referred to as a “stroke of the lungs.”

What can you do to prevent them?
As a caregiver, there’s a lot you can do to prevent exacerbations. First and foremost, you should understand the signs that an exacerbation is occurring. If you notice any of the following symptoms, you should visit your pulmonologist immediately.
- An increase in frequency or severity of cough
- Increased breathlessness when walking or at rest
- Pain or stiffness in the chest
- Lower blood oxygen levels than normal
- Headaches, lightheadedness, or difficulty sleeping
Avoid getting sick
Acute conditions like the common cold or the flu may be harmless to someone without COPD, but for someone with the disease, it can lead to severe complications and even be fatal. Sickness causes an inflammatory response in the body that can result in increased mucus production, congestion, and more coughing than usual all of which exacerbates COPD issues. If your loved one enjoys spending time with friends and family, take the time to ensure they aren’t near anyone who is sick and if they are, try to schedule their visit for another day.

Eating immune-boosting foods like oranges, yogurt, and ginger is one way to prevent sickness. Since respiration and metabolism are closely linked, maintaining a healthy diet not only prevents sickness, it also keeps a COPD patient feeling more alert, energetic, and ready to take on the day. As a caretaker, it’s a good idea to organize a diet routine for your loved one. However, be sure to speak to their doctor before getting started.
Improve indoor air quality
Many homes have an indoor air quality problem. According to the Environmental Protection Agency (EPA), Americans spend about 90 percent of their time inside where pollutants are concentrated up to five times as much as outdoors. When you’re taking care of someone with COPD, you need to be hyper aware of everything that’s affecting the quality of air inside their home. Try the following to boost indoor air quality.

- Avoid using air fresheners or any cleaning product with artificial fragrances
- Avoid using cleaning products with perchloroethylene, formaldehyde, 2-butoxyethanol, ammonia, sodium hydroxide, or chlorine.
- Vacuum and dust frequently
- Replace HVAC filters and prevent dragging in allergens from outdoors
It’s also important to ensure air quality is safe when you go out of the home. If you live in a busy area, avoid going outside during rush hour or any time air pollution will be at its worst. Seasonal allergies can also cause COPD exacerbations so be sure to avoid any parks or areas with a lot of pollen. There are a lot of trees that give off pollen, so check out a full list here. And if you’d like more information on improving indoor air quality read our blog about this subject.
Be prepared for an emergency
Beyond preventing sickness and improving indoor air quality, you should always be prepared for an emergency. First of all, you should locate the nearest emergency room and have a list of people to contact in case of an emergency such as their primary care physician and neighbors. While you may not always be able to make it to a loved one in an emergency, there should always be someone close by who can. Be sure to take this into consideration each time you plan a trip as well.
Oxygen Therapy
Many COPD patients are prescribed supplemental oxygen because it’s the most effective means of increasing blood oxygen levels and reducing COPD symptoms. Caregivers should be responsible for ensuring their oxygen tanks or oxygen concentrators are in working condition and that it’s comfortable for the patient.
Choosing an oxygen device
If your loved one is unable to choose an oxygen device on their own, you may need to help them out. It can be a tricky process narrowing down all your options so you should take your time and speak with an expert. Oxygen therapy devices include oxygen gas, liquid oxygen, and oxygen concentrators. Oxygen gas and liquid oxygen are stored in a tank while oxygen concentrators pull in ambient air and output a more pure, concentrated form of oxygen.

While there are pros and cons to each type of oxygen therapy, portable oxygen concentrators are the most state-of-the-art option. They’re lightweight (usually around 4 or 5 pounds), easy to maintain, and aren’t bulky like oxygen tanks. However, the oxygen device you choose will ultimately depend on the needs of your loved one and the recommendations made by his/her doctor.
Cleaning and maintenance
Once an oxygen device has been purchased, caretakers should clean and maintain the device. Oxygen tanks need to be refilled when they’re low on oxygen and portable oxygen concentrators have batteries that need to be recharged. Oxygen concentrators also have filters that should be cleaned often and replaced after 6 to 12 months of use. Nasal cannulas should also be cleaned regularly and replaced every couple months.
While most oxygen therapies are reliable, there’s always a chance you could encounter a faulty product. Once you’ve purchased a device, take the time to read the manual and get more acquainted with it so that you’re more equipped to deal with any problem you may encounter. Be sure to jot down the customer service number too so you have someone to contact if you’re away from home.
Ensuring it’s comfortable
Another aspect of oxygen therapy is how comfortable it is for the patient. Some people may have problems with the nasal cannulae, the tubing that runs from the device to the patient’s nose. There are several different types like curved prong cannulas, flared prong cannulas, and straight prong cannulas. While they all do the same thing, your loved one may find that one is more comfortable than another and that one may distribute oxygen better without becoming obstructed in the nasal passage.

Another comfort issue some people encounter with oxygen therapy is dryness in the nose. Since air is constantly being pumped out of the device, it can lead to rashes or irritated skin. This can be fixed by using an oxygen humidifier on your device. These are usually pretty lightweight, portable, and easy to maintain. Many CPAP and BiPAP machines come with humidifiers built into the device. For more information, read our blog titled How to Make Supplemental Oxygen More Comfortable.
Pulmonary Rehabilitation
Pulmonary rehabilitation is the process of improving lung function through simple exercises and techniques. This isn’t something you can do at home, however; you’ll need to see a pulmonary specialist for up to 12 weeks through a pulmonary rehabilitation program. These programs teach COPD patients how their lungs work, evaluate their lung health, and give you practical exercises for improving your lung function. Once this program is complete, the patient will be able to exercise at home more effectively.

As a caretaker, you should ensure that your loved one is always able to make it to their classes. Typically, they’re only two or three times a week, but it’s important that they make it to each session so that they get the most out of it. Once their classes are over, you can help them create an exercise schedule that will keep them on track.
Medication
Managing and administering medication is another important part of being a caretaker. Depending on the stage, severity, and other conditions your loved one may be coping with, there are a number of drugs your doctor may prescribe. You should follow these closely and ensure that you only administer the exact amount that the doctor orders. If you need to make any changes for any reason, be sure to consult a doctor first.
Corticosteroids
These drugs are typically administered to people with COPD or asthma and come in either oral or inhaled forms. Corticosteroids have a number of negative risks like high blood pressure, weight gain, and fluid retention, so it’s imperative that you take only the prescribed amount. Since oral corticosteroids affect the whole body, they’re more likely to have these negative side-effects.
Bronchodilators
This type of drug is important for anyone suffering with COPD, asthma, and allergic reactions. A bronchodilator relaxes muscles in the lung helping to clear mucus, reduce inflammation, and make it easier to breathe.
Other Medication
If your loved one suffers from another condition, your doctor may prescribe you other medication. Many drugs have negative symptoms when they’re used together so you’ll need to be careful and pay attention to what his/her doctor is telling you. If you have any questions or concerns about medications, it’s best to address them sooner rather than later.

Planning Doctor’s Visits
If you thought planning doctor’s visits and organizing medical paperwork was hard when you’re healthy, imagine doing it with a chronic condition like COPD. An easy way to keep track of all of this is to put together a calendar and filing cabinet just for COPD-related paperwork. When you schedule an appointment, mark it on your calendar. During your visit, take notes and store it in your filing cabinet so that you can refer back to it in the future.
Completing Daily Tasks
Another way to help a COPD patient is to complete daily tasks for them unrelated to their condition. Just like anyone else, someone with COPD still has things to get done around the house, errands to run, and people to get in touch with.
Grocery Shopping
Grocery shopping is no easy task for someone with COPD. Planning a trip to the store can take a lot of time and energy and leave someone feeling breathless and fatigued, especially in the later stages of COPD. As a caregiver, grocery shopping for them is a great way to help out and take a lot of weight off their shoulders. However, if you don’t have time or you’d rather spend it at home helping your loved one, many grocery stores have grocery delivery services that are surprisingly affordable.

Cleaning
We’ve already talked about using safe cleaning products without harmful chemicals, but you should also be helping with organizing and picking up around the house. Organizing their closet, cleaning their dishes, or vacuuming are some simple ways to make your loved one’s life easier and less stressful. Typically, homecare providers won’t clean up around the house so you may need to hire a maid or a friend to help out.
Cooking
Being around the stove or oven for extended p
.png)
Chronic obstructive pulmonary disease (COPD) is a lung condition that affects millions of people across the country. Advanced stages of COPD can lead to debilitating symptoms such as breathlessness, wheezing, and chest tightness. Since there is no cure for COPD, managing its symptoms is the best way to prevent it from progressing.
With that being said, it’s no surprise that many people afflicted with COPD also develop anxiety from their condition. In tandem with physical symptoms, knowing that the condition can’t be reversed can lead to severe anxiety and reduced quality of life. This is a common response and should be taken just as seriously as the disease itself.
In the following sections, we’re going to take a look at how exactly COPD can lead to anxiety, how anxiety can make COPD symptoms worse, and what you can do to prevent this negative feedback loop.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
How COPD Can Cause Anxiety
Much like how you feel hungry when you haven’t eaten all day or thirsty when you’re dehydrated, your body will exhibit symptoms when it’s low on oxygen. Short-term symptoms like the need to stop and rest more frequently while exercising are easy to notice, however, anxiety tends to be more of a long-term reaction that can be more difficult to detect.
It’s normal to experience anxiety to some extent throughout our daily lives and it can even be used to motivate us to make a change. For example, if you have dirty dishes piling up in your sink, you may experience enough anxiety to clean them and put them away, leaving you feeling relieved and accomplished.

On the other hand, chronic and severe anxiety, like what you may experience as a result of COPD, is not healthy and can even contribute to the physical symptoms you’re experiencing.
According to a study published by the Department of Health and Human Services (HHS), instances of anxiety and depression are “generally higher than those reported in other advanced chronic diseases,” and are much higher than the prevalence of anxiety in the general public, especially during later stages of the disease.
We’re going to take a look at just a few of the main reasons COPD leads to anxiety and what you can do about it.
Shallow Breathing
On average, a healthy person takes between 12 to 20 breaths per minute. If you take more breaths than this, it is known as tachypnea or hyperventilation. Although on the surface, this may not seem like a serious issue, for a COPD patient, it may be the root cause of their anxiety.
According to the Yearbook of Intensive Care and Emergency Medicine, patients with COPD demonstrate shallow and rapid breathing that often results in hypercapnia or carbon dioxide retention. This shallow breathing is usually the result of diminishing lung elasticity and general lung function and can result in breathlessness and increased blood pressure.
Whether it occurs as an isolated incident or chronically like in progressive lung disease, hypercapnia causes a stress response in the body that leads to anxiety. It’s your brain’s way of telling you that something’s wrong and your body isn’t getting the oxygen it needs.
COPD Exacerbations
A COPD exacerbation can result from anything that causes COPD symptoms to worsen. For example, inhaling an irritating substance like pollution or contracting an illness that leads to inflammation of the airways.
Exacerbations like these can lead to a sudden onset of anxiety commonly called panic attacks. If you’d like more information on treating and preventing COPD-induced panic attacks, our blog titled COPD and Panic Attacks: How to Manage Your Anxiety will be a great resource for you.
Aside from panic attacks, however, you might have anxiety about experiencing another exacerbation. For example, if you were outside when an exacerbation occurred, you may have a fear of going outside, especially in busy areas where you feel a lack of control. If this persists long enough, you could be missing out on a lot of the things you enjoy doing in your life.
Feelings of Guilt
One of the most common causes of anxiety in people with chronic respiratory conditions is a sense of guilt. Some patients may feel guilty about their increased dependency on loved ones or about an activity that they are no longer able to do with their condition.
Over time, feelings of guilt can lead to COPD patients not asking for the help they need or distancing themselves from friends and family in order to regain some independence.
The Breathlessness-Anxiety Cycle
When COPD and anxiety combine, they can create a cycle of negative feedback. Feelings of breathlessness may provoke panic, causing you to feel more anxious, thus making it harder to breathe. When you get caught up in this cycle, it may be difficult to distinguish the symptoms of anxiety with the symptoms of COPD.

If you believe you’ve found yourself in this breathlessness-anxiety cycle, it’s important that you speak with a doctor before making any decisions about your health. If you take medication for anxiety, it may exacerbate your COPD symptoms or vise versa. Your doctor will help you find the right balance and ensure that you aren’t making symptoms worse.
How To Reduce COPD-Induced Anxiety
Fortunately, there is ample research done on anxiety and many resources out there for you to go to if you’re experiencing COPD-related anxiety. But a good place to start would be to simply try to recognize the signs of anxiety and how they might be affecting your COPD symptoms.
If you notice that you’re stuck in a loop of negative thoughts surrounding your condition, you’re most likely experiencing anxiety and you should speak with a doctor immediately. However, in the meantime, try some of these tips to reduce anxiety, and ideally, improve COPD symptoms at the same time.
Pulmonary Rehabilitation
Pulmonary rehabilitation (PR) is the process of improving lung function and reducing the symptoms of chronic respiratory conditions through exercise and education. In pulmonary rehabilitation, you will learn more about how your lungs work and how to exercise effectively and safely.

By attending pulmonary rehabilitation, you will not only learn techniques for breathing more effectively, but you will be surrounded by a group of people who are facing similar challenges in their lives. This is a great opportunity to meet some new people and socialize which, in and of itself, may help you alleviate feelings of anxiety.
Breathing Exercises
Although it may seem silly to practice your breathing, it’s incredibly important and can help you live a happier and more fulfilling life, especially if you have a chronic respiratory condition like COPD.
Taking the time to understand how your breathing and posture affect your oxygen intake can be hugely beneficial. And as a result, you’ll be able to reduce symptoms of anxiety significantly. There are a lot of different breathing exercises you can try, however, for COPD patients, diaphragmatic breathing, deep breathing, and pursed lips breathing tend to be the most effective.

Diaphragmatic Breathing
The diaphragm is the muscle under the chest cavity that’s responsible for expanding the lungs, allowing air to flow in. Due to the reduced lung function in COPD patients, however, many people develop a rapid, shallow breath that doesn’t use the diaphragm muscle. Diaphragmatic breathing will help you concentrate on “breathing from the stomach” rather than breathing from the chest.
Deep Breathing
Once you’ve mastered diaphragmatic breathing, you may want to give deep breathing a try. Similar to diaphragmatic breathing, deep breathing requires you to take in a lot of air. However, with this exercise, you will breathe in slowly until your lungs are completely filled and then release it slowly. Ideally, you’ll want to be lying on your back to practice deep breathing exercises.
Pursed Lips Breathing
With this breathing technique, you will inhale slowly through your nose and release it slowly through pursed lips. The purpose of the pursed lips is to increase resistance in the airways, keeping them open while you breathe. Breathing in this way will help you calm down and reduce anxiety.
For more detailed information on breathing techniques, check out 6 Effective Breathing Techniques and Exercises for COPD.
Get More Sleep
One of the main causes of anxiety is a lack of sleep. When you don’t get enough sleep each night, your body is not physically, mentally, or psychologically equipped to make it through the day. And when you’re living life with COPD, you’re carrying additional emotional baggage that many people are not dealing with.
Sleep apnea is a condition affecting more than 18 million Americans. Although it’s not any more common among people with COPD, it can be a lot more dangerous for those that do. When someone has both COPD and sleep apnea it’s called “overlap syndrome” which increases your risk for chronic fatigue, high blood pressure, and hypercapnia.
Improve Your Diet
If you’ve already read our blog about 21 Healthy Foods You Should Eat if You Have COPD and 11 Foods You Should Avoid if You Have COPD, then you already have a pretty good idea of what food is good and bad for COPD. However, when it comes to anxiety, there are two in particular that you need to watch out for — sugar and caffeine.
Although sugar may make you feel great when you first consume it, your body will release extra insulin to absorb the glucose and once this happens, you’ll experience a sugar crash. After a sugar crash, you can expect to feel increased levels of anxiety, irritability, and fatigue.

Similarly with caffeine, you’ll get a quick boost of energy, but reduced levels of serotonin (the feel-good chemical) leading to a depressed mood. The bottom line here is that COPD symptoms are already hard enough to deal with and consuming copious amounts of sugar and caffeine will only make them more difficult in the long run.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Practice Positive Thinking
Sometimes, simply changing your mindset is a great way to reduce COPD-induced anxiety. Whenever you start a new medication, exercise routine, or anything else related to your COPD treatment plan, it pays to see things in a positive light and prevent negative thoughts wherever possible.
Although there is no way to cure COPD, if you follow your doctor’s recommendations and you take care of yourself, you’ll be surprised at all the things you can accomplish! Many people with COPD are able to live long and fulfilling lives just by making a few simple lifestyle changes.
If you’ve never tried it before, you may want to consider meditation or other techniques that help to quiet the mind and relieve tension in the body. These techniques often work hand-in-hand with breathing exercises because the more in tune you are with your body’s needs, the more your mind will be at ease.
Aside from meditation, maintaining a positive outlook on your situation can help you immensely in the long run. Instead of focusing on the negative aspects of your condition, try living in the moment and enjoying time spent with friends and family or doing your favorite hobbies.
Get Outside
In this day and age, humans spend the majority of their time indoors. There are a number of ways that this can have a toll on our mental health, especially when coping with a chronic condition like COPD.
In the past, before the invention of the electric light, humans spent more time outdoors. As a result, the human circadian rhythm was in sync with the natural light-dark cycle. However nowadays, we’re often exposed to light immediately before bed, after waking up, and all throughout the day which can disturb our sleep and increase anxiety.
The best way to combat this is to spend more time outside, especially in the morning or at night right before bed. Although many people work indoors throughout the day, the more you can mimic the natural day-night cycle of the earth, the better.

Another important part of this is staying consistent. Your body needs to get into a rhythm where it knows exactly what to expect each day. This will help you get more restful sleep and keep you feeling alert and positive each day you wake up.
Visit A Therapist
If you’ve tried all of the above solutions to anxiety but haven’t seen any success, you should never be afraid to speak with a therapist. Although it may seem like there is no solution to your anxiety, therapists are experienced with treating patients just like you.
Whether you’re experiencing general anxiety disorder or frequent panic attacks, a licensed mental health professional will help you identify and treat the underlying causes. More specifically, cognitive behavioral therapy (CBT) will help increase awareness of negative thinking patterns so that you’re more equipped to take on a challenging situation.

Additionally, your psychiatrist will help you determine if medication may be beneficial such as antidepressants and other anti-anxiety drugs. If you’re having trouble finding a psychiatrist that’s right for you, be sure to speak with your primary care physician.
Follow Your Treatment Plan
COPD is a progressive disease. What this means is that symptoms rarely get better on their own and they tend to get worse unless medical action is taken. Your doctor will set you up with a clear treatment plan for COPD, and it’s important to stick with it.
COPD treatment may involve a variety of things such as oxygen therapy, bronchodilators, or vaccines to prevent illnesses that make COPD worse. Additionally, your doctor may recommend pulmonary rehabilitation and lifestyle changes like a special diet to follow. Be sure to listen carefully, and if you ever have any questions, don’t hesitate to ask them. The more thoroughly you understand your condition, the better you will be able to manage it and the less anxiety you will experience.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
When it comes to COPD-induced anxiety, the sooner you take action, the better. It’s not uncommon for someone coping with a chronic disease to experience anxiety, depression, or panic attacks, and there is always something you can do to relieve these symptoms.

By following your treatment plan and making changes to your lifestyle, you’ll be able to experience more peace of mind and assurance throughout your daily life. When you live anxiety free, you’ll be able to enjoy the time you spend with loved ones and doing all of the activities you enjoy.
Additionally, finding ways to relieve anxiety could help reduce COPD symptoms like breathlessness, chest tightness, and exacerbations. Be sure to speak with your doctor immediately if you have any questions.
Did you know that living with COPD can make it more difficult to think, make decisions, and remember things? It's true; studies show that COPD can cause mild cognitive impairment, a condition that affects your memory and other mental functions.
Unfortunately, many people are unaware of, or underestimate, the effect that COPD can have on your brain. Because of this, many COPD patients experience mental decline without ever realizing that their disease could be the cause.
This is a shame, especially because COPD-related mild cognitive impairment is both treatable and preventable. But in order to avoid it or minimize its symptoms, you have to understand what it is and what is has to do with COPD.
That's why, in this post, we're going to explain how COPD causes mild cognitive decline and how to recognize it if you have it. We'll also explain what you can do to prevent COPD-related memory loss and how to treat it if it appears.
Many people with COPD have to deal with mild cognitive impairment at some point or another, and it's important to know what you can do about it and what to expect if it happens. That's why we've included a wealth of practical knowledge, helpful advice, and effective techniques in this guide to help you manage memory problems and other cognitive symptoms caused by COPD.
What Does Mild Cognitive Impairment Mean?
In general, mild cognitive impairment (MCI) is a condition that causes minor problems with memory, focus, problem-solving, and attention. It happens to many people as they age, but respiratory diseases like COPD can both trigger and accelerate the condition.
Many people who experience forgetfulness or worry their brain is not as “sharp” as it used to be are actually experiencing the symptoms of mild cognitive impairment. However, MCI is slightly worse than the normal changes to memory and cognition you'd expect to see with age alone.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Mild cognitive impairment happens when the brain's cognitive functions are slightly lower than they should be. It can result from both temporary problems (e.g. oxygen deprivation) and permanent changes (e.g. structural damage) that happen to the brain.
Mild cognitive impairment is very common, affecting about 10-20 percent of people over the age of 65 and about 36 percent of people with COPD. Fortunately, it is a treatable, and sometimes even reversible, condition that can improve with diet, exercise, and other lifestyle changes.
It's important to note that the symptoms of mild cognitive impairment are often very subtle. Some people notice these symptoms on their own, but many don't recognize the signs of MCI until a friend or family member points it out.
Here are some of the most common signs and symptoms of COPD-related memory loss and MCI:
- Forgetting things like events and appointments often
- Forgetting words or struggling to come up with the right vocabulary more often
- Losing or misplacing things more often
- Feeling overwhelmed when faced with problems, making decisions, or making plans
- Difficulty understanding instructions or doing activities that require multiple steps
- Struggling to focus on simple tasks like reading, watching a movie, or having a conversation
- Difficulty finding your way around familiar places or environments
- Increased impulsive behavior or poor judgment
Sometimes, mild cognitive impairment is split into two distinct categories: memory-related or “amnestic” MCI, and MCI that affects thinking skills like decision making and completing tasks with several steps. Some people with MCI experience just one or two symptoms, while others experience a wider rage of cognitive problems.
 |
| Image from www.amenclinics.com |
In the words of Charles Emery, a COPD researcher from Ohio State University, “COPD-related cognitive impairment usually isn't noticeable to the untrained eye, but it can be a serious problem.” That's why people with COPD should be more aware of their risk for cognitive impairment and more familiar with what it looks like in everyday life.
Even if you don't realize it's happening, mild cognitive impairment can make daily living more difficult and have rippling negative effects. Even minor memory problems, like misplacing bills or forgetting to turn off the stove, can cause serious problems in everyday life.
Minor cognitive impairment can also make it difficult to manage your disease and keep track of your medications and other treatments. For example, it could cause memory problems that lead you to use your medications incorrectly or skip doses accidentally, making you more vulnerable to life-threatening exacerbations, quicker disease progression, and other disease complications.
Experiencing difficulties with memory and concentration can also cause you to feel frustrated and stressed, even if you aren't aware that your symptoms are caused by MCI. This can lead to mental disorders like anxiety and depression, especially if the condition is left untreated for too long.
Luckily, COPD-related cognitive impairment can be treated and managed to minimize the symptoms and its effect on your quality of life. With healthy lifestyle changes and proper treatment, you may even be able to regain some or all of the cognitive ability you've lost, especially if you catch it early on.
Importantly, early treatment for mild cognitive impairment can prevent future cognitive decline and more serious conditions like dementia. Because it often results from low blood oxygen levels, recognizing mild cognitive impairment can also alert you to other problems that you need to address in order to better manage your COPD.
The Relationship Between COPD and Memory Loss

At first, it might seem strange that COPD, which is primarily a respiratory disease, could cause mental deficiencies and memory problems. However, a variety of studies have confirmed that there is a direct link between lung function and cognitive decline.
Research from the Mayo Clinic, for instance, found that having COPD can double your risk for mild cognitive impairment, including memory loss. The risk is even higher for people with more advanced COPD and people who use supplemental oxygen therapy.
Some people experience general cognitive impairment that affects many areas of cognition, while others only experience difficulties in one or two areas. Specific cognitive abilities that tend to be affected are memory, information processing, attention, concentration, executive function, and self-control.
However, research also shows that people with COPD—even advanced COPD—only show very slight cognitive decline. According to one study, people with severe COPD scored, on average, just one point less than people who didn't have the disease on a 35-point scale of cognitive ability.
But even though this amount of cognitive decline might seem trivial, it is not something you should ignore. Mild cognitive impairment is enough to affect everyday life and impair your ability to manage your COPD.
That's why it's important to look out for even minor symptoms, especially since cognitive impairment is much more treatable in the early stages. Recognizing the earliest signs of MCI and taking them seriously is a necessary step toward making the changes that can minimize your symptoms and prevent more serious cognitive issues in the future.
How COPD Causes Cognitive Impairment
To understand why COPD causes cognitive impairment, you have to realize that COPD is not just a simple breathing disorder. It is a disease that causes inflammation, strains your heart, and starves your body of oxygen.
One of the key links between COPD and MCI is low blood oxygen levels, known as hypoxemia, which gets worse in the later stages of the disease. This lack of oxygen affects every organ in your body, but it is especially harmful to your heart and brain.
The brain is particularly sensitive to the effects of hypoxemia because it needs so much oxygen; the brain uses up a large amount of energy and needs a continuous flow of oxgen-rich blood in order to function. Because of this, low blood oxygen levels are particularly bad for your brain, and they can lead to brain hypoxia and cognitive impairment.
As a result, memory and cognition problems are much more common in people with more advanced and severe COPD. As the the lungs lose more and more of their ability to function, blood oxygen levels drop lower and more often than they did before, increasing the risk for cognitive symptoms.
However, hypoxemia is not the only reason that people with COPD experience mild cognitive impairment. Researchers believe that a lack of physical activity could also be a cause.
After all, many studies have shown a strong link between regular exercise and better cognitive function. There are many reasons for this, but improved cardiovascular health and circulation seems to play a major role.

Unfortunately, inactivity is a huge problem among people with COPD because their breathing symptoms make exercise very difficult. However, this lack of physical activity worsens COPD symptoms and causes the disease to progress more quickly.
The result is that it becomes harder for your body to supply enough oxygen to your brain and the rest of your body. This can lead to a variety of complications including cognitive impairment and dementia.
COPD also significantly increases your risk for cardiovascular disease for many different reasons, including hypoxemia, lack of exercise, and other disease complications. Cardiovascular disease is a well-known cause of cognitive impairment, in part because it causes poor circulation and damages the blood vessels in your brain.
COPD also causes chronic inflammation, which is a major risk factor for both heart disease and cognitive decline. Researchers believe this happens in part because long-term inflammation causes harmful changes to the blood vessels and tissues in the brain.
Researchers also suspect that a history of smoking—which the vast majority of people with COPD have—can make you more prone to mild cognitive impairment. One study showed, for instance, that MCI is much more common among people who have smoked, are currently smoking, or who are exposed to secondhand smoke for at least one hour per week.
COPD and Dementia
Studies show that both COPD and mild cognitive impairment can significantly raise your risk for dementia. That's because the same conditions that cause COPD-related cognitive impairment can also cause long-term damage to your brain.
Dementia is a general, umbrella term that is used to describe a variety of different types of cognitive decline. It is much more severe than mild cognitive impairment, but it often starts with MCI that gets worse and progresses to dementia over time.
Here are some of the major signs and symptoms of dementia:
- Memory loss that significantly interferes with daily life
- Difficulty completing simple, familiar tasks
- Confusion about dates, places, and how much time has passed
- Difficulty making plans, solving problems, and keeping up with responsibilities
- Difficulties with language, including speaking, writing, keeping track of conversations, and coming up with words
- Frequently misplacing things and forgetting about major events
- Social withdrawal, including giving up on hobbies or work
One of the main ways that COPD leads to dementia is by depriving your brain of oxygen. If your blood oxygen levels stay too low for too long, it can cause permanent damage to the blood vessels and tissues in your brain.
Other COPD-related symptoms and complications can also cause dementia, including chronic inflammation and heart disease. Basically, most of the conditions that can cause mild cognitive impairment have the potential to also cause dementia if they are severe enough or happen frequently enough.
However, it's important to note that, even though mild cognitive impairment and memory loss can be early signs of dementia, they don't necessarily mean that you will develop the disease. For many people with the condition, MCI stays stable or even improves with time.
 |
| The appearance of a normal brain versus a brain with severe Alzheimer's Disease, a form of dementia. |
On the other hand, cognitive problems could be a sign that your COPD could cause, or is causing, serious damage to your brain. This is more likely to happen if your symptoms are severe or you suffer from frequent, severe hypoxemia.
If you have COPD and experience any symptoms of cognitive impairment, you need to be particularly diligent about managing your disease. By taking your medications, getting regular checkups, and living a healthy lifestyle, you can minimize your COPD symptoms and keep your blood oxygen levels high.
In many cases, it is possible to prevent COPD-related cognitive impairment and dementia with healthy living and proper COPD treatment. However, in order to do this, you might need to make some serious changes to your diet, your lifestyle, and how you manage your disease.
How to Prevent & Minimize Memory Loss Caused by COPD

If you have COPD, the best way to prevent memory loss and cognitive impairment is to keep your heart and lungs in the best shape possible. That means managing your COPD properly and building healthy habits that help you keep your body strong.
If you already have mild cognitive impairment, these same methods may even help you reverse your cognitive symptoms. At the very least, making healthy changes can prevent more severe cognitive issues and make a noticeable difference in your health and quality of life.
In the next sections, we'll show you a variety of simple things you can do in your daily life to boost your cognitive ability and prevent cognitive decline. The earlier you take action the healthier your brain will be as you continue to manage your COPD.
Exercise Your Body

Exercise is an irreplaceable tool for keeping your heart, lungs, and brain healthy, especially if you have COPD. It can improve your circulation, improve your ability to breathe, and help your body get more oxygen to your brain.
Studies show that physical fitness reduces cognitive decline caused by aging and even improves general cognitive ability. Other studies on people with COPD even suggest that exercise alone can improve at least some symptoms of cognitive impairment.
On the other hand, lack of physical activity weakens your heart and lungs, worsens breathing problems, and leads to a variety of other health complications. Inactivity is particularly hard on your cardiovascular system, leading to high blood pressure, heart disease, and worsened hypoxemia.
That's why it is so vitally important to get regular physical activity if you have COPD. That means getting at least 20-30 minutes of exercise, including light to moderate-intensity aerobic exercise (e.g. walking, swimming, or jogging), at least 3-4 times per week.
While this might seem daunting at first, don't let it scare or discourage you. You don't have to jump in all at once; you can start small and work at your own pace.
You can start with simple, low-impact activities like walking, stretching, and doing light aerobic exercises. Anything you can do to add more physical activity to your schedule will help, including hobbies like gardening.

You could also join a gym, try a sport, or take regular walks in a park you enjoy nearby. There are many different ways to exercise, and all you have to do is find a few activities that you can stick with and enjoy.
Building the habit can be difficult, but it is certainly worth the effort it takes. It can not only significantly reduce your risk for cognitive decline, but it can also strengthen your heart, reduce your symptoms, and delay the progression of your COPD.
To help you get started, we've put together several guides full of practical tips and tricks for exercising with COPD. Take a look at any of them by clicking the links below:
- Hobbies and activities that are well-suited for people with COPD
- Exercises you can do at home to improve your COPD
- How Pulmonary Rehabilitation can improve your ability to exercise with COPD
- Breathing techniques you can use to reduce shortness of breath when you exercise
Exercise Your Brain
Much like physical exercise helps keep your body strong, mental exercise can help you keep your brain and cognitive functions strong. That's why it's important to keep your brain active as you age, and especially if you suffer from COPD.
Research shows that one of the best ways to do this is by learning new things and doing activities that require mental focus. These kinds of activities strengthen important neural pathways in your brain and can even improve your mental function.
Activities that exercise your brain include things like reading, social activities, and creative endeavors like writing and painting. Other hobbies like playing chess or doing puzzles can also help keep your brain sharp.

Studies show that learning a new skill like playing an instrument or speaking a new language is particularly effective at preventing cognitive decline. You can also pick up new skills by taking a class at a local college or community center, or by joining an activity club.
In general, making an effort to use your brain in new ways and learn new things can help you preserve your memory and cognitive skills as you live with COPD. It can also reduce your chances for developing more serious forms of cognitive impairment, including dementia.
Maintain a Healthy Weight

Being underweight or overweight is bad for your brain and can increase your risk for cognitive issues, including memory problems and MCI. Unfortunately, many people with COPD struggle to


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













