If you have COPD, then you know that it can be dangerous when your symptoms suddenly get worse. That's why preventing flare-ups and exacerbations is one of the main goals of treatment for people with COPD.
A COPD exacerbation (also known as an acute exacerbation) happens when you get sick or your lungs get especially inflamed, making your symptoms much worse for an extended period of time. Even though they go away eventually, exacerbations can cause serious health complications and permanent damage to your lungs.
When you have COPD, your quality of life depends greatly on how much you prioritize your health and avoid habits and environments that put your lungs at risk. That means doing everything you can to keep your body strong and prevent acute exacerbations.
In this article we're going to help you do just that by explaining a variety of ways you can reduce your risk of experiencing a COPD exacerbation. We'll help you understand why exacerbations happen, how to recognize the warning signs.
Most importantly, we'll show you a variety of practical methods and techniques you can start using today to avoid flare-ups and exacerbations in the future. So if you're ready to improve your quality of life and take charge of your health today, continue reading for 15 practical ways you can reduce your risk for acute COPD exacerbations.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What is a COPD Exacerbation?
Most COPD patients are able to keep their symptoms under control most of the time, but flare-ups and exacerbations are always a threat. The frequency of exacerbations varies from patient to patient and depends on a variety of risk factors, including age, disease severity, and physical activity level.
On average, COPD patients experience at least one or two exacerbations every year. This does not include minor flare-ups, which might happen much more frequently in response to mild irritants.
Flare-ups Versus Exacerbations
A COPD flare-up is a temporary increase in symptoms that can happen when you breathe in respiratory irritants like dust, smoke, or dry air. Flare-ups are generally mild, short-lived, and treatable at home.
Exacerbations, on the other hand, last longer and are more serious than mild flare-ups. They usually happen as a result of a respiratory illness or infection that causes inflammation, excess mucus, and reduced lung function.
Exacerbations often require a trip to the doctor, although they can sometimes be treated at home. It's important to talk to your doctor about what you should do in the case of an exacerbation and how long you should wait to call your doctor when your symptoms start to get worse.
In general, it's safest to talk your doctor as early as possible if you think you might be experiencing an exacerbation. That's why it's very important to recognize the early symptoms and warning signs of an oncoming acute exacerbation.
Unlike flare-ups, exacerbations can have extended or even permanent effects. Sometimes, even once an exacerbation passes, the COPD symptoms don't improve all the way. Some patient's conditions don't ever get back to the baseline that they were at before the exacerbation, and they have to cope with a minor, yet permanent, increase in symptoms from that point on.
Exacerbations can be life-threatening at any stage of the disease, but they are particularly dangerous for people with advanced COPD. Flare-ups are common in all COPD patients, although sensitivity to respiratory irritants and the severity of the flare-up can range significantly depending on the patient's physical condition and disease stage.
How to Recognize an Exacerbation

Exacerbations are serious business, and recognizing the early symptoms could save your life. An exacerbation can be debilitating, life-threatening, and is are not something you should ever take lightly. Most researchers agree that preventing exacerbations is one of the most important things you can do to live longer and slow down the progression of COPD.
Some exacerbations are mild, but some are serious and require early and immediate treatment to prevent serious complications. Severe exacerbations can cause you to be hospitalized or even end in death.
That's why it's vital to pay attention to how you feel and be able to recognize the early warning signs of an acute exacerbation. You should always be monitoring your symptoms and looking for signs that indicate they're getting worse. Often, the only early warning sign of an exacerbation is a worsening of the symptoms you already have.
If your worsened symptoms don't start to get better soon, you should talk to your doctor right away and begin any additional medication
or therapies that your doctor recommends. The earlier you begin treating an acute COPD exacerbation, the better your chances of avoiding life-threatening symptoms and hospitalization.

If you ignore worsened symptoms, they're likely to continue getting worse. The longer you wait to seek help, the more you'll be at risk for serious complications and the less likely you'll be to make a full recovery.
Here are some of the early warning signs of a COPD exacerbation:
- Rapid, shallow breathing
- More difficulty catching your breath than usual
- More coughing or wheezing than usual
- A change in mucus color (yellow, green, or blood-tinged in color)
- Increased mucus in your lungs and airways
- Feeling unusually sleepy or fatigued
- Difficulty sleeping because your symptoms keep you up
- Having less energy than usual to do normal daily activities
- Breathlessness and fatigue at rest or after extremely light activities
- Confusion
If you think you're experiencing the early symptoms of an exacerbation, follow your COPD treatment plan and talk to your doctor as soon as possible. If your symptoms get significantly worse or you can't catch your breath, seek emergency medical care immediately.
There are certain symptoms that are a sign of serious oxygen deprivation and require immediate medical care. If you experience confusion, a severe headache, difficulty catching your breath at rest, a bluish tint to your skin, or have a sudden difficulty walking short distances, you should seek emergency medical attention immediately.
What Happens When You Have an Exacerbation?
When you have an exacerbation you'll experience increased symptoms and increased mucus production that makes it more difficult than usual to breathe. This happens because of inflammation that reduces your lung function and causes inflammation in your lungs and airways.
Mild exacerbations can sometimes be treated at home, although you should always talk to your doctor about when you should call him first. Your doctor might recommend a variety of medications to use in the short term to manage your symptoms until the exacerbation passes.
Here are some common medications used to treat exacerbations at home:
-
Bronchodilator Inhalers: Your doctor might recommend that you use your bronchodilator medication more often or prescribe you a different inhaled medication than you usually use. This will help open up your airways and make it easier to breathe.
-
Corticosteroid Medications: Inhaled or oral corticosteroids are common treatments for COPD exacerbations. They help reduce inflammation in your lungs, reduce swelling, and open up narrowed airways.
- Antibiotics: If a bacterial infection is the cause behind your exacerbation, your doctor might prescribe a course of antibiotics to treat it.
However, if an exacerbation gets worse, you might need to go see your doctor or be hospitalized if it gets severe. You should seek emergency medical care if you experience unusually severe symptoms, can't catch your breath, or show signs of low blood oxygen (like confusion, a severe headache, a bluish color to your skin, or extreme fatigue).
If admitted to a hospital, you will receive more intensive treatment that may include bronchodilators, systemic corticosteroids, supplemental oxygen, and breathing support. If your lungs aren't working well enough on their own, you may have to use a ventilator or a positive expiratory pressure (PEP) device to keep your airways open.

Without prompt medical treatment (and even with it), a serious exacerbation can be life-threatening. That's why preventing exacerbations is one of the most important things you can do to stay healthy and live longer with COPD.
What Causes COPD Exacerbations?
|
|
| Photo by Senior Airman Anthony Sanchelli |
There are many different COPD triggers, including dust, pollen, and cold air, that can cause your symptoms to get worse. However, these irritants usually only cause minor flare-ups, not full-blown exacerbations.
However, exposure to COPD triggers like respiratory irritants can significantly raise The majority of the time, exacerbations are caused by a respiratory illnesses or infection, not respiratory irritation alone.your risk of subsequent exacerbations.
According to research, respiratory illnesses cause 70 to 80 percent of exacerbations experienced by people with COPD. That's why it's so important to do whatever you can to avoid getting sick, including getting vaccinations, practicing good hygiene, and living a healthy lifestyle.
Here is a list of some of the most common causes of COPD exacerbations:
- Pneumonia
- The flu
- Seasonal allergens
- Smoke
- Air pollution
Unfortunately, in up to one-third of cases doctors are unable to determine the cause of a COPD exacerbation. It's important to make choices that limit your risk of having an exacerbation, but there's no way to reduce that risk to zero.
There are certain risk factors for exacerbations that you have little or no control over, like your age and the severity of your disease. Here are some common factors that put you a greater risk for exacerbations if you have COPD:
- A history of frequent exacerbations
- If you've had an exacerbation within the past year
- If you have more severe COPD symptoms (e.g. a severe daily cough or severe breathlessness every day)
- You have severely reduced lung function
- Low BMI
- Lack of exercise
- Old age

Taking care to avoid exacerbations is one of the most important things you can do to stay healthy, stay strong, and maintain your quality of life while living with COPD.. If you are ready to learn what you can do to protect your lungs and maintain your quality of life, continue reading to learn about fifteen different ways to avoid COPD flare-ups and exacerbations.
How to Prevent a COPD Exacerbation
Now that you understand the risk factors for exacerbations, why exacerbations happen, and how to recognize the early warning signs, it's time to learn how to prevent them. Even though you can't always avoid exacerbations, there are many different things you can do in your daily life that reduce your risk.
In these next sections, we're going to show you how you can avoid exacerbations by incorporating simple habits and techniques into your everyday life. We'll go in-depth into a variety of activities, useful techniques, and special precautions you can take to reduce your risk.
Don't put it off any longer; continue reading to learn about a variety of practical steps you can take today to reduce your risk of experiencing a COPD exacerbation.
Avoid Weather and Temperature Extremes
Hospitalizations for COPD-related exacerbations and complications go up significantly in extreme temperatures and weather. That's why you have to be particularly careful to protect yourself during the summer and winter months.
In general, it's a good idea to avoid going outdoors whenever it is extremely hot or cold outside. Both hot and warm air are hard on your lungs, make it difficult to breathe, and can make you more prone to flare-ups and exacerbations.
Avoiding Hot Weather

For some people with COPD, the summer heat brings relief and decreases their symptoms. But for those who are not so lucky, the hot air can make a variety of COPD symptoms worse.
When you spend time in the heat, it raises your body temperature, which makes your body have to work harder to cool you down. This is taxing on your lungs, which already need extra energy to function, and can make it much more difficult to breathe.
You are also more likely to get dehydrated and feel fatigued when you are out in the hot, humid air. Hot weather also tends to correspond with higher ozone pollution levels, which can irritate your lungs and make you even more prone to flare-ups and exacerbations.
Here are some tips for staying healthy and avoiding exacerbations in hot weather:
-
Always stay indoors when it is very hot or the air quality is low. Plan exercise and outdoor activities for milder days.
-
Plan activities during the early morning or early evening, when the temperatures are cooler. The hottest temperatures tend to occur between 11 am and 3 pm every day.
-
Drink lots of water during the summer, especially when you exercise or spend time outdoors. Always bring a bottle of water with you when you go out.
-
Keep your home cool and air-conditioned. If you don't have air conditioning, go to a public place that does have AC, like the library or mall, on very hot days.
-
If you feel overheated, try taking a cool bath or shower to cool down.
- Use a fan in your bedroom at night or any other rooms that tend to get hot and stuffy. You can also get a hand-held, battery-powered fan to bring with you whenever you go outdoors in the heat.
-
Drink a sports drink or salty food after sweating or spending time in the heat to replenish lost electrolytes.
-
If you are sensitive to allergens, always check your local pollen and allergen forecast. You can check it online at pollen.com.
- Bring your inhaler and any quick-relief medications with you whenever you go out in case your symptoms flare up.
Avoiding Cold Weather

Cold weather can also make COPD worse and put you at a much greater risk for exacerbations. In fact, one study showed that cold weather caused a significant increase in hospital admissions, with up to a 20% increase in hospitalizations for people with COPD. The main factors increasing the risk were lower temperatures, windchill, cold weather that lasted for more than a week.
Winter weather causes an increase in symptoms in part because cold air is denser, drier, and more difficult to breathe. Cold, dry air dries out your airways and nasal passages, causing inflammation that worsens symptoms and increases mucus production.
Together, these effects make it more difficult to breathe and increase your risk of getting an illness or infection. The effects are the worst at temperatures below freezing, but COPD hospitalizations increase at temperatures as high as 41 degrees Fahrenheit.
That's why it's so important to stay indoors and take extra precautions during the winter months. Here are some tips for avoiding cold weather and staying healthy during the winter:
-
Stay indoors on cold days and when the air quality is low. Don't exercise or do other physical activities outdoors; instead plan them for warmer days or save them for a warmer season.
-
Always dress warm for cold weather and use layers so you can add or remove them if your comfort level changes.
-
Always breathe through your nose, not your mouth. This allows the air to warm up and pick up moisture as it travels through your airways to your lungs.
-
Cover your mouth with a scarf or cold weather mask anytime you have to be out in the cold air. This traps the heat and moisture from your breath in order to warm and humidify the air you breathe.
- If you use supplemental oxygen, cover your oxygen tank and tubing when you go outdoors. You can string your tubing underneath your jacket or coat to keep it warm.
Humidity

Humidity is yet another weather condition that can have a significant effect on people with COPD. Most people do best when the humidity is around 40 percent, and a humidity range between 30 and 50 percent is recommended for people with respiratory conditions and diseases.
Both too little and too much humidity makes it difficult to breathe and can make your COPD symptoms worse. Dry air is harsh and irritating to your lungs, while extra-humid air is heavy and hard to inhale.
Humidity tends to be highest in warm weather, because warm air is able to hold more moisture. The air tends to be much drier during the winter, and the dense, cold air tends to make air pollution worse as well.
But humidity isn't just about the weather; even if the humidity is ideal outdoors, the humidity inside your house can still get high. Running a shower or bath and using appliances like your dishwasher or washing machine can raise the humidity in your home if you're not careful.
Humidity effects everyone differently, so pay attention to what humidity levels make your symptoms better or worse. To reduce your chances of flare-ups and exacerbations, you should avoid spending time outdoors any time the air is especially humid, especially dry, or polluted.

Here are some general tips for dealing with dry and humid weather:
-
Get a humidifier for your home and use it during the dry winter months. You can get one for your bedroom and any other space you tend to spend a lot of time in, or you can get a whole-house humidifier that hooks up to your home's main ventilation system.
-
When the humidity outdoors is very high, keep your windows and doors closed to keep the moist air out of your home.
-
Make sure any appliances that release moisture into the air, including your washing machine, clothes dryer, stove, and dishwasher well-ventilated.
-
Whenever you take a shower or bath be sure to open a window or turn on your bathroom fan to vent extra humidity.
- Use the vent fan on your stove when cooking steamy or smoky foods.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Attend Pulmonary Rehabilitation
Getting exercise and living an active life is another one of the best things you can do to keep your body healthy, strengthen your breathing muscles, and reduce your risk of COPD exacerbations. But in order to get enough exercise, you need to know how to manage your symptoms and control your breathing while you work out.
That's why many doctors recommend that COPD patents attend pulmonary rehabilitation, a special class designed specifically to help people with respiratory diseases live healthier, happier lives. Many people begin pulmonary rehabilitation after they have difficulty exercising and managing their disease on their own.
But pulmonary rehab is about more than just exercise; it's about learning how to manage all the different aspects of your life that are affected by COPD. You'll learn how to keep your lungs healthy, how to manage your symptoms, and how to handle the stress and emotional strain of living with a chronic disease.
Classes are usually run by medical specialists or social workers who have a wealth of knowledge and experience to share. Classes usually focus on these main areas:
- Exercise training classes
- Learning and practicing breathing techniques
- Diet and nutritional counseling
- Lung health and disease education
- Learning how to conserve energy for what's most important
- Mental health counseling and group support sessions
- Learning how to use oxygen and other medications to manage respiratory symptoms
Research shows that taking a pulmonary rehabilitation class increases exercise capacity and overall health in people with COPD. Multiple studies have also found that pulmonary rehab significantly reduces patients' risk of future exacerbations and hospital admissions, too.
Pulmonary rehabilitation is like a crash course on how to live the best possible life while managing your COPD. It's one of the best things you can do to jump-start your COPD treatment and learn how to integrate positive, healthy habits into your everyday life.
Find a Pulmonary Rehabilitation Class Near You

Pulmonary rehabilitation classes vary depending on where you live and what kind of help you need. Some programs are hosted as group classes at hospitals and clinics, some offer individual instruction, and some can even be done partially or fully at home.
If you have COPD, talk to your doctor about whether or not you could benefit from pulmonary rehabilitation. Your doctor can give you a referral and help you find a class in your local area that works for you.
Here are some resources to help you locate a pulmonary rehabilitation program near you:
Personal hygiene is one of those things that everyone knows is important, but few actually take seriously enough. For most people, hygiene is simply a routine part of life, not something they go out of their way to think about pay attention to.
But if you suffer from COPD, it's important to make good personal hygiene a top priority in your daily routine. Proper hygiene is your very first line of defense against illnesses and dangerous COPD exacerbations that can make your disease even worse.

LPT Medical's newest and most impressive portable oxygen concentrator, the ARYA P5 portable oxygen concentrator
However, practicing good personal hygiene takes more effort than most people think. Doing it right takes extra time out of the busy day, and it's very tempting to cut corners to save time.
That's why everyone should take the time to review the important components of good personal hygiene now and then. If you have COPD, then you have even more at stake, and you should take extra care to learn all the proper techniques.
In this post, we're going to show you what good personal hygiene looks like and how it can help you protect your lungs and manage your COPD. This guide will discuss a variety of important hygiene issues, both general and COPD-specific, and help you learn the skills you need implement good hygiene practices in your everyday life.
Why Hygiene is So Important for People with COPD
Most people understand the basics of good hygiene, but not everyone is great at practicing it consistently. Even so, imperfect hygiene is not usually a problem for most healthy adults.
However, good personal hygiene is much more important for people who suffer from COPD. The disease suppresses patients' immune systems, which makes them particularly vulnerable to disease-causing germs like viruses and bacteria.
Even worse, it can be very dangerous to get even a little bit sick if you have COPD. Respiratory illnesses, in particular, can wreak havoc on your lungs and immune system, making it much more difficult to breathe and control other COPD symptoms.
That's why practicing good hygiene is so vital; it protects you from the germs, bacteria, funguses, and respiratory irritants that cause you to get ill. You can't always control whether or not you get sick, but practicing good personal hygiene is one of the few effective things you can do to reduce your risk.
Even minor viruses like the common cold can worsen breathing problems significantly and permanently damage your lungs. Because of blockages and narrowing in your airways, COPD also makes it harder to flush viruses and bacteria out of your respiratory tract.
This significantly raises your risk for secondary lung infections like pneumonia if you get sick. COPD also makes it more difficult to recover from illnesses and infections.
In this way, COPD not only causes you to get sick more often, but also causes you to stay sick for a longer period of time. Unfortunately, one of the consequences of staying sick longer is an increased probability of minor illnesses causing serious infections and permanent damage to your lungs.
In the most serious cases, getting sick when you have COPD can lead to respiratory failure, hospitalization, and even death. That is why it is so important to practice impeccable hygiene if you suffer from COPD.
The Benefits of Good Hygiene

The main benefit of good hygiene is a significantly reduced chance of getting sick. That's because, when you practice good hygiene, you prevent a myriad of disease-causing pathogens like viruses, bacteria, and parasites from making it into your body.
Good personal hygiene is also good for those around you because it prevents you from spreading germs and sicknesses to other people. By practicing good hygiene, you can help protect other people with immune-suppressing diseases like COPD and prevent them from getting illnesses that could potentially threaten their lives.
Along with these physical benefits of good hygiene, there are social and psychological benefits as well. When you keep yourself clean, healthy, and groomed, you are likely to feel more confident and capable in other ways, as well.
Here are some of the main benefits of healthy hygiene habits:
- Improved overall health
- Reduced risk of disease and infections
- Reduced exposure to allergens and other respiratory irritants
- Reduced risk of COPD exacerbations
- Reduced risk of hospitalization
- Reduced risk of spreading germs and illnesses to others
- A cleaner, healthier living environment
- Improved confidence, self-image, and self-esteem
- Other people see you as more healthy, desirable, and attractive when you have good hygiene
What Does Good Personal Hygiene Look Like?

You probably already know the basics of good hygiene like bathing and washing your hands. But there's also a good chance you don't know, or have forgotten, the details of what good hygiene entails.
Still, knowing the basics works well enough for most people most of the time. At worst, most healthy adults will only get a mild illness every so often if they expose themselves to germs.
However, living with COPD means you can't cut any corners without putting your health in serious risk. That means you need to go out of your way to practice impeccable hygiene, even if you've gotten away with an average amount of effort so far in your life.
But to do that, you need to understand what good hygiene is and exactly what you have to do to practice it. Fortunately, practicing good hygiene is relatively easy to do and even simpler to learn.
The basics of good personal hygiene include:
- Knowing when to wash your hands
- Knowing how to wash your hands properly
- Knowing how to prevent yourself from spreading germs to others when you are sick
- Knowing how to avoid transferring germs to your body in public places
- Knowing how to practice good dental hygiene
- Knowing how to clean your body and your clothes to prevent germ buildup
How to Practice Good Hygiene to Improve Your COPD
In this guide, we're going to give you a refresher course on how to practice good personal hygiene. We'll also address a variety of personal hygiene issues and challenges that affect people with COPD specifically.
In these next sections, we will go through each important hygiene issue step by step so you can learn the proper techniques. We'll also give you tips for how to practice good hygiene every day and fit important hygiene practices into your daily routine.
Learning the tips and techniques we explain in this guide will help you ensure that you are doing everything you can to protect yourself from sickness and disease. That way, you can live your life more safely, more confidently, and with a reduced risk of serious COPD complications.
Wash Your Hands Often

Even though washing your hands might seem like obvious advice, it is so essential to personal hygiene that it's still important to review. It is the first step to practicing good hygiene and one of the most effective ways you can protect yourself from disease.
Unfortunately, most people are not as diligent about hand-washing as they should be, even knowing how important it is. Many people remember to wash their hands before eating or going to the bathroom, but get lazy or forget to do it in other situations.
Another problem is that most people don't take enough time to wash their hands thoroughly enough, which makes their hand-washing less effective. As a result, their hands may still harbor harmful bacteria even after washing up.
How to Wash Your Hands the Right Way

If all you do is rub your hands together with soap while giving them a quick rinse under the faucet, then you're not washing them well enough. In fact, if it takes you less than a full twenty to thirty seconds (count it!), then you probably need to correct your technique.
Here is a quick overview of proper hand-washing technique, as recommended by the CDC:
- Use clean, running water to rinse and wet your hands before applying soap.
- Rub the soap between your hands until it forms a lather.
- Scrub your hands for at least twenty seconds, getting your nails, wrists, and between your fingers.
- Rinse off all the soap under clean, running water.
- Dry your hands off on a clean towel.
To wash your hands properly, you need to make sure you scrub every part of your hands thoroughly with soap, including your fingers, fingernails, palms, wrists, between your fingers, and the backs of your hands. Any kind of regular, non-antibacterial soap will do the trick, including bar soap, liquid soap, and foaming soaps.
You may need to wash the skin above your wrists and further up your forearms after cleaning, washing dishes, or doing anything else that is likely to fling bacteria around. If your hands are especially dirty, you should also use a nail brush to scrub around and underneath your fingernails to remove excess dirt and grime.

Here are some more tips for more effective and hygienic hand washing:
- Avoid antibacterial soaps and hand sanitizers: Using antibacterial soaps and hand sanitizer is almost never necessary because regular soaps and sanitizers are effective. Additionally, anti-bacterial soaps are bad for the environment, and may even be bad for your health.
- Keep your hand towels clean and dry: If your hand towel stays moist for too long, it creates a perfect environment for mold and bacteria to grow. Let your hand towels dry thoroughly between uses and wash them regularly, especially if you notice a bad or musty smell.
- Don't re-contaminate your hands: After you get your hands all clean, you don't want to have to start over again. That's why you should be careful not re-contaminate them right away by touching a dirty faucet or door handle on your way out of the bathroom. When using a public bathroom, cover your hand with a tissue if necessary to avoid touching dirty public surfaces.
To see proper hand-washing technique in action, check out this video from the CDC.
When to Wash Your Hands

You probably already know that you should wash your hands before and after eating and after you use the bathroom. However, there are many other situations that call for thorough hand-washing, and some are less obvious than others.
In general, you should wash your hands after completing any activity that puts you in contact with germs. That includes anything that involves handling dirty items, touching public surfaces, or coming into contact with someone who is sick or injured.
Here is a more complete list of situations in which you should wash your hands:
- Before and after handling food
- Before and after eating
- Before and after treating a wound
- Before and after touching your face, especially your eyes, nose, and mouth
- Before and after caring for a sick person
- After sneezing, coughing, or blowing your nose
- After using the bathroom
- After changing a diaper or handling pet waste
- After touching a pet or other animal
- After touching another person
- After handling garbage or waste
- After touching a public item or surface (like a public pen or ATM)
- After smoking
Use Hand Sanitizer

Sometimes, you won't have access to a sink when you need to wash your hands. In case this happens, it's a good idea to keep hand sanitizer with you whenever you leave the house.
For the best protection, you should always use alcohol-based hand sanitizers instead of antibacterial ones. To be effective, your hand sanitizer should contain no less than 60 percent alcohol.
These hand sanitizers can kill the majority of bacteria and fungi on your hands as well as many viruses. The higher percentage of alcohol the sanitizer contains, the more effective it will be against all kinds of microbes.
However, hand sanitizer only works effectively if you use it right. If your hands are greasy or grimy when you apply hand sanitizer or you wipe the solution off too soon, then you won't get its full protection.
But even though it can be good in a pinch, hand sanitizer is not a good substitute for hand-washing in all cases. Using hand sanitizer is not nearly as effective as washing your hands, and you should only use it as a backup for times when hand-washing is not an option.
Here are some tips for using hand sanitizer correctly to protect yourself from illnesses and infections:
- Use hand sanitizer by pouring a dime-sized dollop into the palm of your hand and rubbing the solution thoroughly into your palms, fingers, and the backs of your hands.
- Make sure you don't have dirt, oils, or grime on your hands before applying hand sanitizer, otherwise it may not be effective.
- Once the solution has been absorbed into your skin, let your hands air dry. (Don't wipe your hands off; it should only take a few seconds for the solution to dry on its own.)
- Do not rely on hand sanitizer to clean harmful chemicals like pesticides off your hands.
Bathe Often for Healthy Skin and Lungs

No matter how careful you are to avoid germs, your body inevitably picks plenty of them up from your environment throughout the day. When you go outside, cook, clean, and sweat, you are exposed to all sorts of bacteria, fungi, and other harmful particles that stick to your hair, clothes, and skin.
<

Oxygen- It's as simple as inhaling and exhaling? Well for people with respiratory disease, not so much.
Oxygen is life, and without a sufficient amount to support life, it could be deadly. People with certain respiratory diseases that restrict airflow struggle everyday just to breathe. Not to mention the other stresses lack of oxygen places on one’s daily life.

That is why LPT Medical is dedicated to getting oxygen to the people who need it most. If you are looking to buy a supplemental oxygen device your first step is finishing reading this blog to learn about using oxygen as a first time oxygen user. The second step is getting in touch with an experienced oxygen specialist by calling 1+(800)-946-1201.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you are going to be wearing oxygen for the first time, you’ll likely remember the first day that you get your oxygen and supplies. It is normal to feel confused and overwhelmed.
Also, you’ll probably have a lot of questions. Even if you know about oxygen from spending time in hospitals or nursing homes you'll quickly realize there is a lot more to home oxygen therapy than what meets the eye.

The best thing you can do for yourself throughout your oxygen journey and your disease management process, is to continue learning more! Read on to learn more about what the oxygen experience can be like! You’ll also notice that oxygen affects everyone’s life differently, and there is no one right answer.
The more time you spend with your device, the more you will learn about what works for you and your lifestyle.
Your Oxygen Device Options Overview

We often write about the oxygen choice you have as an oxygen patient. You can find that information in these blogs listed below:
Optimizing the Cost and your Lifestyle Based on your Oxygen Device
Is Spending the Extra Cash on a High Quality Supplementary Oxygen Device Really Worth It?
Long Term Oxygen Therapy Devices That Make Life A Breeze
In these blogs, you will read about portable oxygen concentrators (POCs) and oxygen tanks.
The option between POCs and other oxygen devices will ultimately be determined by your oxygen intake. Your supplemental oxygen intake will be determined through a few respiratory tests that your doctor will conduct.
Once you have a flow rate prescribed by your doctor, you will either be able to get a POC, or if your oxygen flow rate is too high, you’ll need an oxygen tank.
If your flow rate is within the range where a POC will manage your oxygen levels, it is important to subsequently consider your lifestyle and travel plans. A POC will make your life objectively easier than if you opted for an oxygen tank.
There are several reasons POCs are a better option for many oxygen users. Firstly, they are battery powered. The Arya Portable Oxygen Concentrator battery can last for up to 16 hours! When you charge the device you simply plug it to a AC or DC power unit, and continue using it, as you would a cell phone.

The other big one, you can travel on airplanes with your POC! There is a lot you need to know about traveling with oxygen. You'll find that information in a few sections! For now, we will continue talking about the oxygen device options you have.
POCs are also notably small in stature and light-weight. Therefore, it is easy to go from place to place! The Caire Freestyle Comfort portable oxygen concentrator only weighs 5 pounds.

Confidence Going Out in Public with Oxygen
Spending time out of the house for the first time with you oxygen device and tubing can be intimidating. It can also be hard to deal with your loved ones and old friends seeing you with an oxygen device for the first time.
The best thing to remember in these situations, is that the oxygen is helping you become healthier. With the help of oxygen therapy you can get back some of your independence. In a way, you are helping them help you!

Independence is a great thing oxygen can give you back if you’ve lost that due to your condition. Oxygen therapy will eventually help you maintain more natural energy levels, and your ability to do things for yourself again!
You can also remember that, although the exact number is unknown, there are an estimated 1.5 million supplemental oxygen users in the U.S. So you are certainly not alone!

You can join Facebook groups or online forums to discuss with other oxygen patients about their experiences. This can ease the battle of feeling isolated.
Another helpful piece of advice is that you are using oxygen caused by a respiratory disease, and the oxygen is enabling you to do more. You wouldn’t be ashamed to wear glasses to help you see, or a hearing aid to help you hear, or if you have to wear a brace to help you walk. So don't be ashamed of your oxygen device that helps you breathe.
Sleeping with Oxygen
You might be questioning if you can sleep with a portable oxygen concentrator. You can, but it will be up to you and your doctor whether or not you need to. There are several notable benefits for using oxygen at night.
Sleeping with oxygen concentrator offers:
- A significant improvement in sleep
- A mood boost, by reducing anxiety and depression caused by insomnia
- More stamina, energy, and alertness during the day, as a result of a healthy sleep
- A significant decrease in the risk of developing health problems triggered by low oxygen levels
Now, even though wearing oxygen to bed has its benefits, it is not as simple as it sounds. You will have an adjustment period where you will need to learn how to wear oxygen while sleeping.

The biggest thing you do to make sure your oxygen device is working for you at night, is to breathe through your nose. Easier said than done! Most people breathe through their mouth, especially during sleep.
You should start by talking to your doctor about using an oxygen mask at night. It is typical that if you are using more than 6 liters per minute (lpm) or more of supplemental oxygen you can wear a closed oxygen mask at night or during the day to improve your breathing.
The use of an oxygen mask requires a prescription from your doctor. You could also try wearing a vent or OxyMask when using between 1 to 15 lpm — but again it is very important to check with you doctor first.
Here are some tips to help you adjust to wearing oxygen while you sleep:
- Make a goal of getting 30 minutes of exercise during the day.
Yes, exercising during the day will not only improve sleep quality but also sleep duration at night. As few as ten minutes of aerobic exercise, such as walking, cycling or taking a tai chi class, can dramatically improve your sleep quality. This works best when you are exercising on a regular basis.
- Avoid carbonated beverages late at night.
So the caffeine level in carbonated drinks is an issue for your sleep, carbonation is not helpful either. Carbonated beverages can produce gas that pushes on the diaphragm, making breathing more difficult. For that reason, it’s a good idea for people with respiratory disease and oxygen users to avoid carbonated beverages before bed.
- Establish a bedtime routine.
One of the best ways to get better sleep is to go to bed and wake up around the same time every day. Routine is key! When your body has a sleep cycle to rely on, it is the most natural way to achieve healthy sleep, even if you are sleeping with an oxygen concentrator during the night.
- Designate your sleeping spot.
Another big aspect of routine is doing similar or exactly the same thing every night before falling asleep. There are several helpful activities that can become routine before bedtime. Also it’s important that you designate your bed – and bedroom – for sleep. So avoid doing other things during the day in your bedroom such as watching TV or reading.
- Practice airway clearing techniques for airway clearance before bed.
Clearing your airways of mucus is something you can practice throughout the day to help you sleep better at night. These techniques can help you more naturally maintain oxygen levels throughout the day and night.
Traveling with Oxygen

Traveling is one of the most challenging obstacles to overcome when you first begin on oxygen.
Just getting in the car is hard, but getting on an airplane is actually impossible if you are using a gas or liquid tank.
You will need a portable oxygen concentrator that is FAA approved. These device can be found at LPTMedical.com or call 1+(800)-946-1201.
First of all, the Air Carrier Access Act does not require airlines to provide medical oxygen to any eligible respiratory patients during flights, so do not expect to be given oxygen on your flight. Very rarely will airlines provide supplemental medical oxygen on flights for their passengers, and if they do this oxygen service typically costs a fee.
.jpg)
There are some things you need to know and tasks you must accomplish before you travel by air with your POC. First of all, be aware that the FAA and the airline you are flying on may have different requirements and you must follow both the FAA and the airline’s regulations.
- The FAA regulations do not require that you tell your air carrier about your POC in advance, however almost every airline will have you notify them that you will be flying with oxygen at least 48 hours before your flight.
- If you are flying on Southwest and JetBlue, these airlines also also ask you to check in for your flight at least one hour before takeoff if you are traveling with oxygen.
- There are some instances when your airline will require a physician's statement
- There are some airlines that will require you to demonstrate how you respond to your POC's alarms before you board the aircraft.
Your best option is to get ahold of the airline you are flying with to learn about the regulations they are held to when it comes to passengers with oxygen concentrators on board.
Overview

We hope that this blog gives you some insight into what life is like with supplemental oxygen therapy.
As a first time oxygen user, education is key! Read up on your options, reach out to your doctor and health care team to learn more and more.
If you buy a POC from LPT Medical, you will work with the most experienced and helpful oxygen specialists who are always around to answer questions about your oxygen device.
Do you ever wonder what is exactly happening to your body? What do these diagnoses mean for you and life as you know it?
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If so, you need to read this blog that explains bronchiectasis in depth. Bronchiectasis is a condition where the bronchial tubes of your lungs are permanently damaged, widened, and thickened. This is an important illness that we at LPT Medical take very seriously. When it comes to oxygen therapy and supplemental oxygen devices, we are your go to company that supplies the most effective, quiet, high-tech oxygen machines.
Bronchiectasis causes damage to people’s air passages. Bronchiectasis often happens as a result of COPD. In these cases, many people will require a portable oxygen concentrator in order to get the right amount of oxygen.

The damages bronchiectasis causes in the lungs also causes bacteria and mucus to build up and compile in the lungs. This results in frequent infections and blockages of the airways. That being said, in conjunction with oxygen therapy, bronchiectasis patients must also be prepared with a proper treatment plan that can mitigate infections and exacerbated symptoms.
There is a lot more to this disease than what meets the eye. The sections in this blog will explain bronchiectasis and everything you need to know about what it means for you moving forward.
COPD and Bronchiectasis Overview
Bronchiectasis and chronic obstructive pulmonary disease (COPD) are two chronic conditions that involve damage to the lungs and they often happen together. In many cases, people with both of these conditions need pulse flow oxygen or a continuous oxygen device. The ARYA Portable Oxygen Concentrator is an example of a pulse flow device that people can use day or night. The Respironics SimplyGo is a continuous flow device that is very popular.

If you have other questions about portable oxygen concentrators, call LPT Medical at 1+(800)-946-1201.

The causes and treatments for each differ slightly. It is common for COPD to cause bronchiectasis.
It is important for you to know the differences and similarities between bronchiectasis and COPD and how each condition is treated.
There’s no cure for bronchiectasis or COPD, but both are treatable. With the proper treatment, you can lessen symptoms and slow the progression of the disease from getting worse. Bronchiectasis is objectively more mild, and with treatment, you can actually live a fairly normal life with less invasive symptoms and treatments than what one would go through with COPD.
.png)
With bronchiectasis, flare-ups must be treated quickly to maintain oxygen flow to the rest of your body and prevent further lung damage.
Because this blog is more focused on bronchiectasis, we are not going to dive deep into the similarities and differences between COPD and bronchiectasis. We did find a very useful Healthline article that explains this comparison more. You can find that by clicking here: Understanding the Similarities and Differences Between Bronchiectasis and COPD.
The rest of this blog is going to explain the bronchiectasis diagnosis, the symptoms of bronchiectasis, risks associated with developing bronchiectasis, tips for living with bronchiectasis, and lastly the treatment and outlook for people with bronchiectasis.
Bronchiectasis Diagnosis Process
A chest computed tomography also known commonly as a CT scan is the typical test for diagnosing bronchiectasis. X-rays are less accurate in diagnosing bronchiectasis.
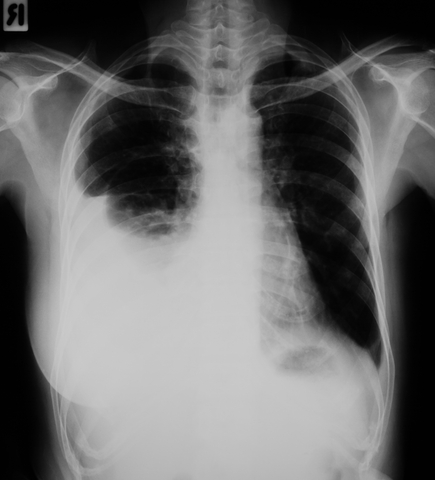
The CT scan is a painless test. It shows exact copies of your airways and other structures in your chest. A chest CT scan can show the extent and location of lung damage.
It is important during the diagnosis process, for your doctor to work with you to establish the cause of the bronchiectasis based on your history and physical exam findings. There are several causes that can cause or contribute to bronchiectasis.
Bronchiectasis is normally caused by your lungs becoming damaged and airways widening and becoming infected. This is why COPD often results in bronchiectasis. Sometimes, the cause of bronchiectasis is unknown.
You might be wondering— why is it important to know the cause of bronchiectasis? This is so that you and your healthcare team can effectively treat the underlying disorder to prevent the bronchiectasis from getting worse.

That being said, during your diagnosis process, you’ll want to know the underlying cause. Therefore, after your CT scan confirms you have bronchiectasis, you’ll then undergo laboratory and microbiologic testing and pulmonary function testing.
This evaluation will likely include:
- Complete blood count with differential
- Immunoglobulin levels (IgG, IgM, and IgA)
- Sputum culture to check for bacteria, mycobacteria, and fungi
- If your doctor suspects CF, they’ll order a sweat chloride test or genetic test.
Bronchiectasis Symptoms Explained
If you think you have bronchiectasis, you can monitor the sign and symptoms by researching what exactly bronchiectasis looks like. However, symptoms of bronchiectasis can take several months or even years to develop.

Some if the common symptoms include:
- chronic daily cough
- coughing up blood
- atypical sounds or wheezing in your chest with breathing
- shortness of breath
- chest pain
- coughing up large amounts of thick mucus every day
- weight loss
- fatigue
- change in the structure of your fingernails and toenails, known as clubbing
- frequent respiratory infections
If you’re experiencing any of these symptoms daily, you should contact a doctor. You can get a diagnosis and start treatment immediately to mitigate the progression and severity of the disease.
Risks and Developing Bronchiectasis
The risk of developing bronchiectasis increases as you get older. That being said, younger people can have it. Also, Women are more likely to have it than men, and women's experience with bronchiectasis also tends to be more severe.

Other health conditions that can put you at risk of having bronchiectasis include:
- Atypically functioning immune system
- Inflammatory bowel disease
- Autoimmune diseases like HIV
- COPD
- Allergic lung reaction to fungus
- Lung infections, such as whooping cough, pneumonia, or tuberculosis
Tips for Living with Bronchiectasis

Once you have bronchiectasis, there is no cure. This is a disease you will live with you the rest of your life. Therefore, you will need to learn how to live with the symptoms, treatments, and other conditions of the disease.
The bright side is that you CAN live with this disease. If you treat yourself properly, you can live a relatively normal life as you would without the disease!
Here are the basic tips you need to follow:
- Follow your bronchiectasis treatment plan.
- Take your medications as prescribed.
- Eat a healthy, well-balanced diet.
- Drink lots of water and other nonalcoholic beverages.
- Follow a gentle exercise routine.
- Practice good sleep hygiene.
- Get your annual flu shot.
- Get your COVID-19 vaccination and booster.
- Wash your hands.
- Avoid getting the common cold, flu, COVID and other illnesses.
- Perform breathing exercises and techniques.
- Maintain good posture.
- Relax and incorporate rest periods throughout your day.
- Do your more difficult tasks when your energy levels are highest.
Treatment for People with Bronchiectasis

So as we mentioned above in the first tip for living with bronchiectasis— You have to follow a strict treatment in order to live comfortably with bronchiectasis
Treating your bronchiectasis is important to help you manage the condition and daily life. Your main goal of treatment should be to keep infections manageable. So how do you do this?
Your treatment options for bronchiectasis include:
- Chest physiotherapy. Chest physiotherapy helps clear your lungs of mucus. This is a compression vest that gently pushes and releases your chest, creating the same effect as a cough. The purpose is to clear mucus from the walls of your bronchial tubes.
- Surgery. If there’s bleeding in your lung, or if the bronchiectasis is only in one part of your lung, you may need surgery to remove the affected area.

- Draining secretions. Another part of daily treatment involves draining the bronchial secretions, aided by gravity. A respiratory therapist can teach you techniques to aid in coughing up the excess mucus
- Treating underlying conditions. If conditions like immune disorders or COPD are causing your bronchiectasis, you will treat those conditions in order to mitigate bronchiectasis symptoms. Common treatments for COPD include oxygen therapy and pulmonary rehabilitation.
- Lifestyle changes. Things like exercise, eating a healthy diet, and drinking plenty of water may help improve the symptoms of bronchiectasis.
Outlook for People with Bronchiectasis
The outlook for people with bronchiectasis is dependent on the severity of the condition, how you treat the condition, and most importantly what is causing it.
Bronchiectasis affects 350,000 to 500,000 people in the U.S. Individuals with the non‐cystic fibrosis bronchiectasis overall have a positive outlook with treatment. That being said, severe bronchiectasis can be fatal.
Non‐cystic fibrosis bronchiectasis is a chronic lung condition in which the breathing tubes in the lungs, also known as airways or bronchi, become abnormally dilated and thickened over time. While there are many causes of bronchiectasis, damage to the airway by lung infection is the most common. These damaged airways can no longer effectively clear mucus and bacteria from the lungs.
Cystic fibrosis (CF) is a genetically inherited disorder that causes severe damage to the lungs, digestive system and other organs in the body. Cystic fibrosis affects approximately 30,000 children and adults in the United States and approximately 80,000 individuals worldwide.
Overview
One of the biggest and most important things when it comes to bronchiectasis is early diagnosis.
The earlier and faster you can begin treatment, the better it will be for managing the lung damage you already have and preventing it from getting worse.
Beyond early diagnosis, we hope that this article sheds light on bronchiectasis and how the disease will affect you and your daily life!
Please leave a comment or question if you enjoyed reading this blog, and share the link with friends, family, and followers to help others learn more about bronchiectasis.
COPD is a disease that affects your respiratory system. That being said, what you eat and how your stomach feels can greatly impact the way you breathe. Whether that's good or bad, is up to you!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you suffer from chronic obstructive pulmonary disease (COPD), you might find that eating specific foods and following certain diets can help manage your condition. You also might realize eating certains foods makes me feel worse, and can make your symptoms worse.
It is important that you eat food. COPD patients often lose a lot of weight throughout their diagnosis.
This article describes how diet affects COPD. We outline the best diet for COPD patients. And we include foods you should eat and foods you should avoid. We also provide an example meal plan you can follow, along with tips for cooking and eating.
How Diet Can Affect COPD
While COPD is a lung condition that limits your airflow making it hard to breathe, incorporating a healthy diet into your daily life can actually help you manage adverse health effects of COPD.
Research shows that a healthy and well-balanced diet can have the following beneficial health effects in people with COPD:
- reduces inflammation in your airways
- maintains and improves muscle strength in your body and lungs
- improves lung function in general
- Lowers metabolic and heart disease risk
The process of changing food to fuel in the body is called metabolism. Therefore, oxygen and food are the essentials materials metabolism. The energy and carbon dioxide created after eating and breathing are the finished products.
![]()
The right mix of nutrients in your diet can help you breathe easier.
Best Diet For COPD Patients

Your body is uniquely YOU! Therefore, there is not one single diet that all COPD patients must follow. Instead, you need to eat food that gives you fuel and energy, the food you eat should not make you feel bloated or full, and it should be a relatively healthy source of vitamins and minerals.
A healthy diet is essentially just the right mix of nutrients and a lot of variety. As a COPD patient you can cater your diet to help you breathe easier. Diet is a crucial aspect you need to discuss with your healthcare team. Together, you can comprise a meal plan, just for you.

It might be helpful to meet with a registered dietitian nutritionist (RDN). Their knowledge and expertise will help you get on track. You can also find an RDN who specializes in COPD by visiting the Academy of Nutrition and Dietetics or simply discuss this topic with your doctor.
Foods you Should Eat

While there is no strict diet COPD patients need to be on, there are general rules as to what foods will make you feel energized, light, and well-balanced
As a COPD patient you need food that are high in complex carbohydrates, fiber, protein, and Mono and polyunsaturated fats.

If you are like most people, all of those words don't mean much to you. And reading the small labels on foods is time-consuming and let's face it TOO SMALL TO READ!
Here is a what you need to know about foods you should eat:
Complex Carbohydrates
Complex carbohydrates contain long chains of sugar molecules. This is all scientific jargon, but it essentially means that complex carbohydrates are a great source of energy.

Here are some foods that contain complex carbohydrates:
- Fresh fruit and starchy vegetables
- Whole grains
- Whole grain bread and pasta
- Beans and lentils
Fiber Rich Foods

A person with COPD should eat foods high in fiber. you should be aiming to get around 20–30 grams of fiber each day. Here are some ideas of fibrous food you can start to incorporate into your daily diet:
- beans and lentils
- fruits and vegetables
- nuts and seeds
- whole grains, such as oats
- vegetables
Protein

Research shows that people with COPD have increased protein needs because protein rich foods help increase your muscle mass. This means that COPD patients do benefit even more from protein than individuals without COPD. Incorporating protein-rich foods during meals and snacks will improve your nutritional status and subsequently your quality of life.
Foods that are high in protein include:
- Meat and poultry
- Fish
- Eggs
- Nuts and seeds
- Tofu
- Cheese
- Milk
Mono and Polyunsaturated Fats
Basically, mono and polyunsaturated fats are good fats. These healthy fats can lower cholesterol, which is helpful for everyone, including individuals with COPD.

Some foods that contain these fats include:
- Olive oil and avocado oil
- Salmon
- Nuts and seeds
- Avocados
Foods you Should Avoid
If you have COPD, certain foods can make you feel worse.

The common symptoms associated with COPD include difficulty breathing, coughing, wheezing, and mucus production. All of these symptoms can be exacerbated or made worse depending on the food you eat everyday.
In addition to eliminating exposure to smoke and other air pollutants, there are certain foods that a person with COPD should avoid in order to minimize the symptoms. Here are some of the foods and ingredients you should avoid eating if you have COPD.
Simple Carbohydrates
Simple carbohydrates offer less nutrients than complex carbohydrates. Foods consisting of simple carbohydrates include:
- Table sugar
- Chocolate and candy
- Cakes and other sugary desserts
- Sugary drinks
- Processed foods
- White bread and pasta
Many high-fat foods are nutritious, and people can include them in a healthful diet. However, many highly processed foods are high-fat, and people with COPD should avoid or limit them to promote overall health.
High Fat Foods
People with COPD must avoid or limit the following high-fat foods:
- Fast food
- Bacon and other processed meats
- Fried foods
- Sugary pastries
- Margarine
- Ice cream
Example Meal Plan
As mentioned in the beginning of this blog, meal plans and your diet should be unique to you, your health, and your lifestyle. With that being said, people can consider the following meal plan as a guide and talk to you diatian or doctor about developing a meal plan that works best for you:
|
Breakfast |
oatmeal with strawberries, blueberries, and almond butter |
|
Snack |
Boiled egg and fresh sliced vegetables |
|
Lunch |
Grilled chicken breast with salad and new potatoes |
|
Snack |
Mixed nuts |
|
Dinner |
Grilled salmon with quinoa and zucchini |
|
Desert |
Greek yogurt with pumpkin seeds and berries |
Meal prepping tips

Preparing meals and cooking can be very challenging for COPD patients. First and foremost, you should always be using your portable oxygen concentrator even while cooking to ensure you are getting the oxygen you need to maintain your energy and oxygen levels.

Even with your oxygen therapy, COPD can make you feel low energy so you might not feel up to cooking. If this happens to you, you can consider trying the following methods:
- Quick meals: Find healthy recipes that take less than 30 minutes to prepare and cook. The less challenge and the less steps involved the better. Also, buy pre-cut vegetables to reduce meal preparation times further.
- Crock-Pot: Find healthy crock-pot recipes. You can throw the ingredients in, and simply leave all it there to cook over several hours with minimal effort.
- Leftovers: While cooking, you can try to make more than you need so that you have leftover food for your next meal or even the following days.
How to Eat More Regularly

If you have COPD, eating can be challenging. Not only is the process of cooking tiring, but the act of eating can be overwhelming for some. Some people with COPD may experience a lack of appetite due to breathing difficulties and general chest discomfort.
Here are some eating hints:
- Rest just before eating.
- Eat more food early in the morning
- Avoid foods that cause gas or bloating
- Eat 4 to 6 small meals a day
- limit liquids with meals; drink an hour after meals.
- Talk to your doctor about taking a nutritional supplement
-
If you are using oxygen therapy, continue to use your supplemental oxygen device, even while you eat.
Overview

We really hope this blog gives you some ideas for meals and snacks that can help you feel better and more energized throughout the day!
It is also our hope that you learned how consuming a balanced and nutritious diet may alleviate some of the breathing difficulties you experience with COPD. Eating healthy is also a crucial step towards preventing certain health complications in the future.
As person with COPD, you should try to eat plenty of protein, complex carbohydrates, and fiber-rich foods. Your snacks should add healthy sources of fat to your diet. Avoid foods high in fat like processed food and try to stay away from sugary drinks and food.
After reading this blog, if you are considering changing your diet or lifestyle, talk to your doctor for advice on how to do this safely and effectively!
Air Pollution, occupational dust, chemical fumes, cigarette smoking as well as second hand smoking can irritate the lungs. Long-term exposure to such lung irritants can lead to inflammation and the development of lung problems in some people.

One of the lung problems that you may acquire over time from the exposure is Chronic Obstructive Pulmonary Disease (COPD). It is a progressive disease that cannot be cured and makes breathing very difficult for people who have it. This is as a result of the narrowing of the airways caused by inflammation and blockage making it difficult for air to flow freely into and out of the lungs.
It is estimated that a whopping 65 million people around the world have COPD according to the World Health Organization. Many more are believed to have the disease without their knowledge.
Even though COPD cannot be cured, there are a good number of treatments and management techniques that are available such as corticosteroids, bronchodilators and pulmonary rehab among many others. Most of the people diagnosed with COPD can live a productive long life after diagnosis.

The most commonly prescribed drugs for COPD are inhaled corticosteroids, this is because steroids help reduce the inflammation in the lungs which is a chief contributor to the progression of COPD. When corticosteroids are paired with bronchodilator medication which helps to open up the airways, most patients experience relief from some of their worst symptoms.
An active area of research has been to find better ways to control the inflammation that underlies the development of COPD. It was reported by Medline Plus, a publication of the National Institutes of Medicine that antioxidants are man-made or natural substances that may prevent or delay some types of cell damage.
The body usually obtains antioxidants naturally from the food that you consume, some companies are however selling dietary supplements with the aim to increase what you derive from your diet.
In theory, if you are able to control or reverse the inflammation associated with COPD, the symptoms of this disease may be reduced and the functioning of the lungs could potentially become better. A study conducted in 2015 by the International Journal of Chronic Obstructive Pulmonary Disease explained that, “dietary antioxidants mainly vitamins C and E, are responsible for antioxidant defenses in the lungs.” A potential antioxidant effect with hydrogen has also been found by researchers.

A 2011 study in the journal Current Pharmaceutical Design found that, “hydrogen is the most abundant element in the universe constituting nearly 75 percent of the universe’s mass; however, hydrogen is absent on the Earth in its monoatomic form and is present in water and organic or inorganic compounds. Hydrogen gas, with the molecular formula H2, is a colorless, odorless, tasteless and highly combustible diatomic gas. The Earth’s atmosphere contains less than one part per million of hydrogen gas.”
It is not a new idea that hydrogen can reduce inflammation. A study done in 1975 in the journal Science first proposed its use as a cancer treatment, and ever since that time, a modicum of studies have applied the principles of hydrogen as an antioxidant to a scope of chronic diseases that are associated with inflammation, including emphysema and diabetes. Dr. Philip Diaz, a pulmonary specialist at The Ohio State University Wexner Medical Center in Columbus, Ohio said, “But there’s limited data even in animals.”
“There’s some literature and a theoretical concept that [hydrogen] might have an antioxidant effect depending on how it is delivered. But at this point it would be very premature” for patients to be receiving hydrogen as a component of their COPD treatment protocol, he says.
Despite the warning from Dr. Diaz and most other doctors that the evidence hydrogen can be used to treat COPD is not enough, some patients are using hydrogen peroxide as a so-called ‘natural’ treatment for COPD by experimenting on themselves.
A number of COPD discussion forums found online include threads about how individuals have tried to treat themselves by adding hydrogen peroxide into their nebulizers and through looking for hydrogen peroxide injections from alternative healers. However, by doing this they could face devastating consequences.

A “60 Minutes” report from CBS in 2005 investigated the use of intravenous hydrogen peroxide in the death of a woman that was undergoing treatment for multiple sclerosis and made a discovery that no reputable medical organization would recommend the use of this treatment for any disease and that its use may have led to the death of this woman.
“The National Multiple Sclerosis Society calls intravenous hydrogen peroxide ‘unproven’ and ‘potentially dangerous.’ The American Cancer Society warns ‘there is no evidence that it has value as a treatment for cancer or other diseases,’’’ the 60 minutes report noted. David Sampson, director of media relations for the American Cancer Society, says that the 2005 warning is “still accurate”. We’re not aware of any evidence that H2O2 [hydrogen peroxide] is useful as a treatment for cancer.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Some studies however suggest that there could still be some potential in the use of dissolved or inhaled hydrogen as a treatment for diseases that cause inflammation in the future. The interest in this possibility has also risen as a result of increasing incidences of COPD worldwide.
A study conducted in 2017 in the International Journal of Chronic Obstructive Pulmonary Disease investigated the role hydrogen plays in smoking-induced cases of COPD in rats. “It is still uncertain whether hydrogen has effects on COPD,” the authors wrote, “or whether different concentrations of hydrogen could have different effects on COPD.” They set out to examine these views and found that there was a connection between the administration of hydrogen and the progression of smoking-induced COPD in rats.
They noted that the rats that had been administered with hydrogen lost less weight than those that hadn’t been given any hydrogen. The rats that had been administered with hydrogen also experienced reduced inflammation in the lungs, improved lung function, positive changes to the lung structure and heart tissue and restoration of balance in enzymes that support cellular health. The study also suggested that the results were better when a higher dose of hydrogen was administered.
Although the results from this study seem to be promising, it is important to note that this was a single study and it was not conducted in humans. Before your doctor even begins to prescribe hydrogen as a therapy for COPD, it would need to be repeated many more times to help paint a clearer picture of its position in the treatment of COPD. Diaz says, “that animal observation hasn’t been translated to humans and people shouldn’t extrapolate that hydrogen testing in animals. It may not be the same in humans. Basically, there’s not a lot of good evidence in people that this would work.” According to him, a lot more testing would be required for any future use of hydrogen therapy.
Meanwhile, you should follow the orders that you doctor has given you and take the medicine prescribed to you as directed. Be sure to check with your doctor should you want to take up any other alternative treatments such as acupuncture or any other conventional approach.
A good way to provide your body with lots of inflammation-fighting antioxidants without the risk of uncertain therapy is through eating a diet that is rich in fresh vegetables and fruit. Dark leafy greens, berries and other brightly colored produce tend to be rich in antioxidants. You should go ahead and add these to your next meal for a safe and natural nutritional boost.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!
















