In order to maintain a healthy and well-balanced diet, it’s essential to consume a wide variety of nutrients. Most of these nutrients can be found in the food that we eat, but occasionally it’s advised that you take dietary supplements in order to boost your intake of certain vitamins and minerals.
While everyone needs the same nutrients, it’s usually a matter of what quantity you should consume them in. For example, babies need to consume a lot of vitamin D which helps regulate calcium and phosphate in the body. In turn, this aids in the development of strong bones, teeth, and muscles.
Similarly, a healthy adult may need to consume different quantities of nutrients than an adult with a chronic disease. COPD patients, in particular, are reported to have deficiencies in vitamin D and other nutrients with antioxidant capacity such as vitamins A, C, and E.
But getting the right nutrients isn’t as simple as it sounds. You’ll need to consult with your doctor and maybe even a dietitian who can examine your condition and compile a dietary plan that will work best for you.
In this post, we’ll take a look at some of the supplements that are most commonly used in COPD patients and we’ll provide you with all the information you need to know to start discussing supplements with your doctor. If you have any questions, don’t hesitate to leave them in the comment section so we can reach out to you.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The Good and the Bad of Dietary Supplements
According to a 2017 survey by the Council for Responsible Nutrition (CRN), 76 percent of U.S. adults use dietary supplements. And while supplements are widely available and easily accessible, they aren’t always used in a responsible way.
Unfortunately, just like drugs, dietary supplements have well-known and well-documented side-effects. Supplements contain active ingredients and if they aren’t used in moderation, they can have strong adverse effects on the body.

One of the greatest dangers of supplements is that they aren’t regulated the same way many drugs are. According to the American Cancer Society, both supplements and drugs are regulated by the United States Food and Drug Administration (FDA). However, drugs are often considered unsafe until proven safe, whereas supplements are considered safe until proven unsafe.
The reason this happens is that supplements are categorized as a “food product” making them immune to many of the tests that are required to bring drugs to store shelves. Drug manufacturers are required to put their products through a series of clinical trials that test their safety and efficacy. On the other hand, supplement manufacturers only need to prove that their products do not result in “a significant or unreasonable risk of illness or injury.”
Because supplements are “self-prescribed,” it’s a lot more difficult for health professionals to track their use. Rather than being able to prescribe each vitamin and mineral that their patient takes, doctors and nutritionists need to rely on their patients to do their own research and address any concerns they have before purchasing any type of dietary supplement.
Lastly, supplement manufacturers do not need to seek approval from the FDA in order to market their products. Supplement advertisements often tout anecdotal evidence rather than empirical evidence as proof that their supplements work. In other words, their evidence is based on an individual’s experience instead of proven facts and statistics.
Dietary Supplements and COPD
With all of this being said, the best advice for COPD patients interested in dietary supplements is to be cautious about what you read. While supplements don’t typically have side-effects as severe as drugs, they still contain powerful active ingredients that can make COPD more difficult to manage if you don’t know what you’re doing.

Another thing to note is that supplements are not a “cure-all” and they’re not intended to treat a specific disease or illness. They’re most commonly used to treat nutrient deficiencies in your body, and you won’t know what these deficiencies are unless you discuss your symptoms with your doctor.
COPD is a progressive and irreversible lung disease characterized by chronic inflammation and obstructed airflow. COPD varies widely in terms of severity and many patients will experience comorbidities such as sleep apnea, osteoporosis, cardiac disease, as well as mental health disorders like anxiety or depression.

As a result, it’s impossible for a pulmonologist to provide a “one-size-fits-all” treatment plan for a COPD patient. Each patient is considered a unique case, so even if something works for one COPD patient, it doesn’t necessarily mean it will work for all of them. Without further ado, let’s take a look at some of the most commonly recommended supplements for COPD.
Vitamins
Every day, your body works around the clock to produce skin, bone, and muscle. It sends nerve signals throughout the body and creates rich red blood cells that nurture every organ in the body. But without essential nutrients like vitamins, your body would not be able to do any of this.

Your body requires about 30 different types of vitamins, minerals, and dietary components. But the problem is, many of these components are not produced by the body naturally, so you need to get them from either the food you eat or dietary supplements.
Vitamin D
Vitamin D plays a number of important roles in the body. First and foremost, it promotes healthy calcium absorption. Calcium is a mineral that’s responsible for muscle function, hormonal secretion, nerve transmission, and vascular vasodilation and contraction. Vitamin D also plays an important role in the reduction of inflammation, immune function, and the modulation of cell growth.
.jpg)
Vitamin D deficiency is one of the most common side-effects associated with COPD. It’s estimated that about 25 percent of people with COPD have low levels of vitamin D. This occurs for two main reasons: COPD patients often don’t eat the recommended amount of meals each day because eating can be physically exhausting and lead to difficulty breathing.
Secondly, many COPD patients, especially those with stage 3 or stage 4 COPD, don’t get outside very much. Since a large portion of our vitamin D intake is absorbed from sunlight, respiratory patients are often deprived of this.
While COPD patients can take regular vitamin D supplements or vitamin D with calcium, vitamin D3 is a better alternative for many people. The reason for this is because vitamin D3 contains both sunlight and dietary-activated vitamins — both of which COPD patients lack.

Generally, vitamin D is believed to reduce the rate of lung decline for people with severe lung disease. Because vitamin D helps regulate inflammation, COPD patients may experience fewer exacerbations that are less severe. Regular vitamin D levels will also help prevent osteoporosis and other bone conditions that can make living with COPD even more difficult.
Too much vitamin D may result in vitamin D toxicity. This can cause too much calcium to build up in the blood (hypercalcemia), which can cause fatigue, weakness, and nausea. If hypercalcemia progresses, it can lead to the formation of calcium stones and pain in the bones and kidney.
Minerals
Like vitamins, minerals are one of the essential nutrients for your body. Minerals are naturally occurring inorganic materials that play a number of important roles like maintaining healthy brain function, muscle function, and heart function. There are two types of minerals: trace minerals and macrominerals.

Macrominerals include magnesium, phosphorus, sodium, potassium, chloride, sulfur, and calcium. Generally speaking, macrominerals are needed in much higher doses than trace minerals and they play a larger role in your body functions. Trace minerals, on the other hand, include fluoride, selenium, cobalt, zinc, iodine, copper, and iron.
Magnesium Sulfate
Magnesium sulfate (MS) is widely used as a treatment for asthma due to its bronchodilatory effects. What this means is that it can help widen the airways in the event of a severe asthma exacerbation. Unfortunately, MS has not been tested as widely when it comes to treating COPD, so its efficacy is still up for debate.

Several placebo-controlled trials have been conducted to test the benefits of magnesium sulfate in treating COPD. However, they have yielded mixed results and didn’t present enough evidence to indicate that COPD patients should adjust their treatment plan to accommodate for oral or nebulized magnesium sulfate supplements.
Zinc
Zinc is an essential trace element that plays an important role in immunity. While zinc can be found naturally in foods like whole grains, red meat, and poultry, it can also be taken in the form of dietary supplements. Zinc is an antioxidant, meaning it protects your cells against dangerous free radicals that are produced when your body breaks down food or you’re exposed to tobacco smoke.

An imbalance between antioxidant capacity and oxidative stress is believed to play a major role in the development of COPD, so zinc may have beneficial effects when it comes to regulating this. Since zinc plays such an important role in regulating the immune system, COPD patients with zinc deficiency will be at a higher risk of experiencing lung infections that can lead to exacerbations.
Omega-3 Fatty Acids
Omega-3 fatty acids are not one nutrient, but rather, a whole family of essential fatty acids. Since your body cannot produce these fatty acids on its own, you need to get them through your diet. Some examples of food that contain omega-3 include fish (salmon), flax seeds, chia seeds, and walnuts.
Omega-3 supplements are very popular nowadays and for good reason. It’s been proven to lower blood pressure, slow plaque development in the arteries, improve heart health, and even help you manage anxiety or depression. Omega-3 supplements, in particular, are great for people who don’t consume a lot of fish or other foods that contain omega-3.
One of the ways omega-3 helps COPD patients is by fighting inflammation. According to Richard Phipps, Ph.D. professor of Environmental Medicine and director of URSMD Lung Biology and Disease Program, “We never really knew why diets high in omega fatty acids seemed good, but now we know it’s because they provide the precursors for molecules that help shut down excessive inflammation.”
While many people take omega-3 supplements like fish oil without consulting their doctor, it’s recommended that COPD patients ask their pulmonologist first. There are three different types of omega-3s including alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA), all of which have different uses. What’s more, it’s important to consume the correct ratio of omega-3 to omega-6 fatty acids.
If you have a shellfish allergy, be aware that omega-3 supplements may contain trace amounts of shellfish. Be sure to address this with your doctor if you’re concerned about it.
NAC (N-Acetylcysteine)
N-acetylcysteine is an antioxidant that potentially has beneficial effects for people with COPD. While NAC has been shown to reduce cough and phlegm and thin mucus in some patients, it has shown little to no effect in others. More studies are needed to fully understand the pros and cons of using NAC to treat COPD.

From what we know so far, however, NAC seems very safe to use. What’s more, it can be taken either orally, or through a nebulizer which gives COPD patients plenty of options. NAC is typically prescribed in tandem with other treatment options rather than being used as a primary treatment for COPD.
Ginseng
Aside from vitamin D, ginseng is one of the most common supplements used for COPD. Ginseng is a root that’s found in many places around the world, but the most popular are American ginseng and Asian ginseng, the latter of which has been used in medicine for centuries.

While ginseng has many benefits for people with different conditions, for COPD patients, it has powerful antioxidants and anti-inflammatory properties. Another benefit of ginseng is that it’s an all-natural herbal supplement. So, unlike manmade vitamin and mineral supplements, it’s much easier for patients to verify that they are receiving a pure product without any additives.
Questions to Ask Your Doctor
Everyone needs to maintain a healthy balance of vitamins and minerals to be healthy. However, like drugs, taking too many dietary supplements can have adverse side-effects. Many people take a daily “multivitamin” which contains a variety of vitamins and minerals. And while these have some proven health benefits for some people, they don’t target specific nutrients that will benefit COPD patients.

If you want to do what’s best for your health, especially if you have COPD or another chronic illness, it’s best to consult your doctor. He/she will help you understand how dietary supplements fit into your overall COPD treatment regimen and give you an idea of what side-effects to expect. Ask your doctor the following questions to get you started:
- Are there any tests I can take to see if I have vitamin deficiencies?
- How will supplements affect my COPD diet?
- What are the benefits and risks of the supplements I’m taking?
- How can I ensure the supplements I’m using are safe?
- Are there any effective alternatives to the supplements I’m taking?
-
How will supplements affect my comorbidities such as sleep apnea, heart problems, or anxiety?
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Conclusion
Nutrition plays a fundamental role in our overall health. By getting our recommended daily value of vitamins and minerals, we provide our bodies with the raw materials they need to perform functions such as regulating blood production and blood flow, building strong healthy bones, and regulating metabolism. Dietary supplements are a great way to fine-tune our diet, but they can be equally destructive if they aren’t used correctly.
Similar to drugs, every dietary supplement has side-effects. If you’re someone with COPD or any other chronic illness, this could make your symptoms worse and even increase your chance of experiencing exacerbations. This is why it’s important to first discuss with your doctor so that he/she can recommend supplements that will work in tandem with your COPD treatment regimen, rather than working against it.
If you have COPD, then you've probably realized that treating the disease is not a simple process. In order to get it right, your doctor needs to have a very thorough understanding of your physical condition and the nature of your disease.
Because of this, people with COPD have to undergo a large number of medical tests and screenings over the course of COPD treatment. These tests, which include blood screenings, x-rays, spirometry measurements, and more, allow your doctor to tailor your treatment plan specifically to your needs.
Unfortunately, while these tests reveal valuable information about your health and your disease, many patients don't fully understand what their results mean. Even if you have a general idea of what the tests are for, chances are you still wouldn't know how to read and understand the results.
Fortunately, you don't have to be a doctor or a nurse to make some sense out of your medical test results. With a little practice and help, just about everyone is capable of grasping the important aspects of the different tests used to diagnose and monitor COPD.
In this post, we're going to teach you all about these tests—lung function tests, blood tests, chest scans, and more—and show you how to interpret the data in the results. We'll explain what each test is, how it works, and how to figure out what your results actually mean for you and your health.
This is a useful skill that can help you better understand what's going on when you visit your doctor and work with other members of your COPD treatment team. It can also give you the confidence to ask more questions and understand the nuances of treating and monitoring your disease.
Even though the medical jargon can seem complicated at first, it won't seem nearly as intimidating once it's broken down into layman's terms. Once you learn the basics, you'll find it much easier to navigate the medical vocabulary surrounding your disease and treatments.
In the following sections, we'll give you the information you need to start understanding your COPD test results on a deeper level than before. That way, you can take a more active role in your health and treating your COPD.
Getting Your Hands on Your COPD Test Results
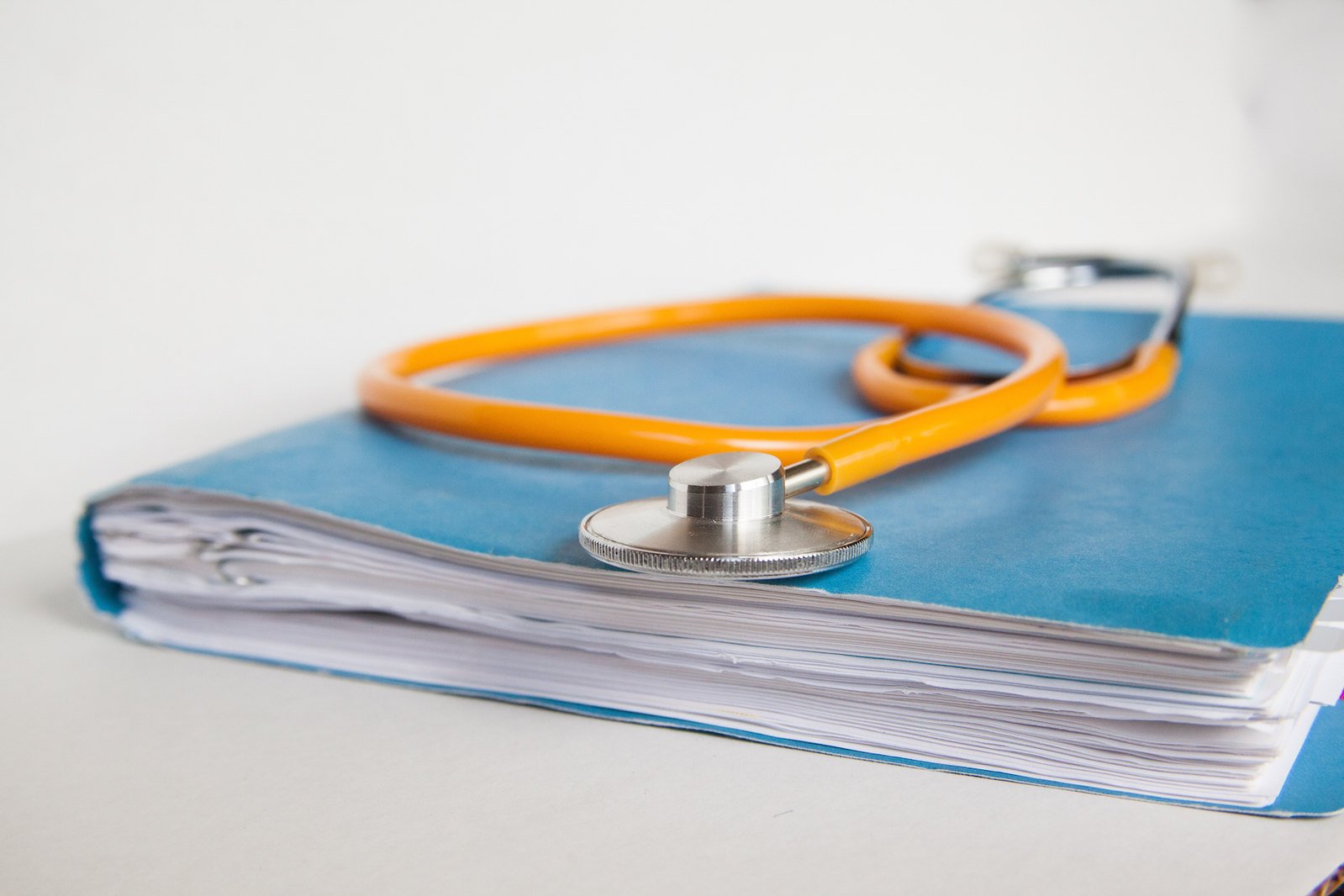
Image from Weiss & Paarz www.weisspaarz.com
If you want the opportunity to understand what your COPD tests mean, you need to make sure you have ready access to your results. In some cases, this is as simple as asking your doctor to give you a copy of all your records and reports.
Some healthcare providers, on the other hand, may require you to follow a specific request process in order to get your records. You may need to write a letter, fill out a form, or pay a small fee to cover the cost of making copies and mailing.
Whenever you take a new spirometry test or another type of health screening, make sure to let your doctor know that you'd like to look at the results yourself. Some test results take days or weeks to come
back, but if your doctor knows you're waiting to see them, he can make sure you get access to the records as soon as they're available.
Also keep in mind, that, if you live in the US, you are always entitled to see and review your medical records by law, except in a few rare cases (usually related to mental health records). It is a right under the US Health Insurance Portability Accountability Act (HIPAA), and it states that you must be able to access existing records within 60 days of requesting them.
If you cannot access your medical records or feel that your rights to review your records have been violated, you can file a complaint with the US Department of Health and Human Services. Just make sure you file your complaint with 180 days of your denied request.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Leverage Your Doctor's Experience: Always Listen to the Expert

Whenever possible, you should ask your doctor to go over your COPD test results with you personally, especially if you are unfamiliar with the test or how the data is organized. Even if you know the basics of what you're looking at, your doctor can help you understand the report much better than you could on your own.
You might ask your doctor to go through the report with you line-by-line to help guide you through the information. This gives him the chance to explain important concepts and details that can help you better interpret the results.
This also gives you an opportunity to ask questions and express any concerns you have about the results of your test. If there's anything you are unsure of, don't be afraid to ask your doctor to explain it more clearly.
Understanding Your Lung Function Test Results
There are several different types of lung function tests (also known as pulmonary function tests), and their purpose is to measure how well your lungs are working. They are quick, reliable, and simple to do, which is why they are widely used both to diagnose COPD and to monitor the disease long term.
Lung function tests can tell you whether or not your lungs are damaged and, if they are, give you a better idea of how much damage they have sustained. Doctors use the results to both diagnose COPD and to gauge the severity of the disease.
If you have COPD, then it's important to familiarize yourself with lung function tests—especially spirometry—and how they work. You will take them fairly often over the course of your treatment, likely as part of your regular COPD check-ups.
Taking these tests periodically allows your doctor to track any changes that happen in your lung function over time. This is important, because it allows your doctor to catch and treat problems, like infections, exacerbations, and lung function decline quickly when they occur.
The results of your lung function tests also help your doctor decide what kinds of medications and treatments you need. They also help your doctor determine how well your current treatments are working and evaluate the effectiveness of newly-prescribed medications.
Spirometry
Spirometry is the primary method doctors use to measure lung function and evaluate COPD. It's a relatively simple test that measures changes in your lung volume as you breathe.
By measuring these changes, spirometry can evaluate whether or not your airways are obstructed, and if they are, to what degree. Because of this, spirometry measurements are a reliable way to diagnose COPD and determine how severe the disease is.
Spirometry tests are simple, painless, and relatively quick to complete. If you have COPD, your doctor will probably ask you take a spirometry test at every appointment so that he can look for any changes in your results.
Taking a Spirometry Test
In order to take a spirometry test, you have to breathe out through a mouthpiece attached to a small machine called a spirometer. Your doctor will also put a clip on your nose to pinch your nostrils shut; this is simply to make sure that you only breathe through the mouthpiece during the test.
Then, your doctor will instruct you to take in a deep breath of air (not through the mouthpiece) before exhaling as forcefully and completely as you can into the spirometer's mouthpiece. You will need to do this at least a few times or until your doctor gets a good set of clean results.
The entire process should take less than fifteen minutes to complete. However, you may need to take the test two separate times: once without taking any medication, and once after you've used a bronchodilator inhaler, with a short pause in-between.
This is known as a bronchodilator reversibility test because it tells you how much the bronchodilator medication is able to improve your airway obstruction. This tells your doctor how well you respond to the medication and helps him determine the best course of treatment.
Spirometry Test Measurements

There are three main measurements that your doctor will measure in a typical spirometry test:
- FVC: Forced Vital Capacity
- FEV1: Forced Expiratory Volume (in one second)
- FEV1/FVC: this is a ratio comparing your forced expiratory volume (FEV) to your forced vital capacity (FVC)
Spirometry tests take other measurements as well, including forced expiratory flow (FEF), peak expiratory flow rate (PEFR), and maximal voluntary ventilation (MVV). However, we're not going to discuss these in any detail here because FVC, FEV1, and FEV1/FVC are usually the most important spirometry results to look at when it comes to diagnosing and monitoring COPD.
FVC: Your forced vital capacity (FVC) essentially tells you how much air you can push out of your lungs in one breath. More specifically, it is a measure of how much air (in volume) that you can exhale forcefully and quickly from your lungs after taking in as deep a breath as you can.
FEV1: Your FEV1 tells you how much air you can exhale from your lungs in exactly one second after taking a deep breath. Basically, FVC tells you the volume of air you push out during one full exhale, while FEV1 tells you the volume of air you can push out during the first second of that full exhale.
FEV1/FVC: When you divide your FEV1 by your FVC, you get another important number, which is simply referred to as your FEV1/FVC. This tells you what percentage of the air you exhaled from your lungs was pushed out during the first second of your exhale.
For example, an FEV1/FVC of 90% means that you pushed out 90% of the air during the first second of your exhale, and the remaining 10% of the air after that first second. If your FEV1/FVC percentage is too low, it is a sign that something is preventing you from pushing the air out of your lungs as quickly as you should.
If your FEV1 or FVC results are abnormal, this FEV1/FVC ratio helps your doctor determine whether or not the abnormality is caused by an obstruction (e.g. COPD) or a restrictive lung disease (in which FEV1 and FVC should change at a similar rate). If you have an FEV1/FVC of 80% or less, it is a strong sign that you have an obstructive lung disease.
Interpreting Spirometry Results
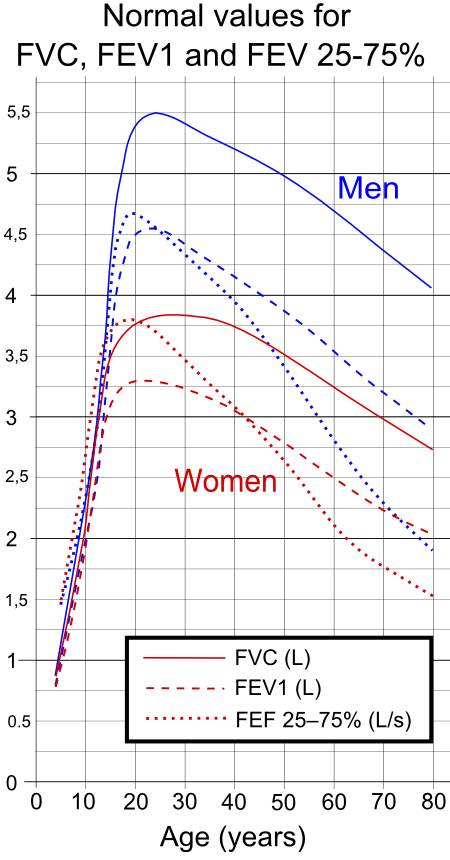
In order to make sense of your spirometry test results, you need to compare them against a standard table of healthy FEV1 and FEV1/FVC values. This will tell you how much your numbers differ from numbers collected from healthy adults of your age, weight, and height.
Then, in order to truly understand what these numbers mean, you will need to refer to another table, known as the GOLD spirometric criteria for COPD severity. This table presents four different ranges of FEV1 and FEV1/FEC results and tells you what it means if your numbers fall within that range.
The GOLD guidelines are the most commonly used and widely accepted criteria for diagnosing COPD. Finding out where your results fall within these four GOLD categories will tell you what stage of the disease you have and give you a better idea of how severe your COPD is.
Here's a quick look at the GOLD guidelines and what they can tell you about your health.
GOLD Spirometric Criteria for COPD Severity
- Stage I: Mild COPD
- FEV1/FEC less than 0.7
- FEV1 greater than or equal to 80%
- Stage II: Moderate COPD
- FEV1/FEC less than 0.7
- FEV1 between 50% and 80%
- Stage III: Severe COPD
- FEC1/FEC less than 0.7
- FEV1 between 30% and 50%
- Stage IV: Very Severe COPD
- FEV1/FEC less than 0.7
- FEV1 less than 30% or less than 50% plus chronic respiratory failure
While it's important to read and understand your spirometry test results yourself, remember that only your doctor has the training and expertise to accurately interpret the results. A licensed doctor is the only one qualified to diagnose COPD or make the call on what stage of the disease you have.
Lung Plethysmography

Lung plethysmography (pronounced ple-thiz-mah-graf-ey) is a test that measures your lung capacity, or how much air your lungs can hold at one time. It can also tell you how much air is left in your lungs after you exhale.
Your lung capacity is closely related to your general lung function, which is why plethysmography is often used to evaluate and monitor COPD. In particular, plethysmography helps your doctor determine whether or not your airways are obstructed, and how much they are obstructed, by measuring how you breathe.
This is especially useful for diagnosing unknown breathing problems, because it can confirm or rule out airway obstruction as a cause. This helps doctors determine whether someone has COPD or different type of breathing disorder.
Lung plethysmography also allows your doctor determine whether or not your lungs trap air and how severe the problem is. It does this by measuring exactly how much air is left in your lungs after you exhale.
This is important, because trapped air is a very common problem for people with COPD, and it can significantly worsen respiratory symptoms. Trapped air makes it difficult to breathe, worsens shortness of breath, and can actually stretch out your lung tissue (causing hyperinflation) over time.
Taking a Lung Plethysmography Test
 |
| Photo by Airman 1st Class Teresa Cleveland |
Taking a lung plethysmography test is simple and usually only takes about fifteen minutes to complete. All you have to do is sit in an enclosed, transparent chamber (about the size of a phone booth) and breathe in and out through a special mouthpiece attached to a spirometer machine.
During the test, your doctor will instruct you to breathe in specific ways so that the machine can measure a wide range of breathing patterns. You will alternate between normal breathing, fast breathing, shallow breathing, deep breathing, and any other breathing patterns your doctor wants to test.
If you normally use oxygen, you will most likely be instructed not to use it during the test. You may also stop the test and leave the chamber at any time if you feel too uncomfortable or claustrophobic, though this may require you start the test again from the beginning.
Interpreting Your Lung Plethysmography Results

Throughout the test, the machine attached to your mouthpiece carefully measures the airflow in and out of your lungs. The results provide your doctor with a few very important pieces of information about your lungs and how you breathe.
Specifically, there are three main things the test can tell you about your lungs:
- Total Lung Capacity (TLC): the amount of air in your lungs after you breathe in as deeply and fully as you can
- Functional Residual Volume (FRV): the amount of air that is left in your lungs after exhaling as fully and completely as you can
- Functional Residual Capacity (FRC): this is a measure that compares the amount of air left in your lungs after a normal exhale to the amount of air left in your lungs after you exhale as fully and completely as you can
To understand what these results mean, you will have to compare the numbers from your results to the numbers that are considered healthy for your age, sex, height, and weight. If your results are equal to the healthy standard, then that indicates that your results are normal. If your numbers are significantly higher or lower, however, that indicates abnormal lung function.
You can use the information in the following sections as a basic guide to help you understand how to interpret your plethysmography results when comparing them to the healthy standard:
Total Lung Capacity (TLC)
Increased TLC: If your total lung capacity is higher than normal, this can be a sign of a lung disease like emphysema. It means that your lungs can hold more air than the average person, which is often caused by obstructive lung diseases and especially lung hyperinflation.
Decreased TLC: It is a bad sign if your total lung capacity is lower than normal because it indicates that your lungs are not able to expand or fill up as much as they should. This is often caused by restrictive lung diseases like pulmonary fibrosis, which are different from obstructive lung diseases like COPD.
Functional Residual Volume (FRV)
Increased FRV: If your functional residual volume is higher than the healthy standard, it is a bad sign because it means that there is too much air left in your lungs even after you exhale completely. This is a sign that your lungs have lost elasticity and/or are hyper-inflated, which is common in people with COPD and especially emphysema.
Functional Residual Capacity (FRC)
Increased FRC: It is a bad sign if your FRC numbers are higher than the healthy standard because it indicates that air stays trapped in your lungs after you exhale. The higher the number, the more severe the problem is.
This indicates that you suffer from an obstructive lung condition, and is very common in people with COPD.
Decreased FRC: It is also a bad sign if your FRC numbers are lower than the healthy standard, because it means that your lungs are not filling up as much as they should. This indicates that the amount of available airspace in your lungs is reduced, which is often caused by narrowed airways and/or loss of elasticity in the lungs.
Decreased FRC is common in people with pulmonary fibrosis, sarcoidosis, obesity, and in people who have had lung reduction surgeries or strokes.
Lung Diffusion Tests
 |
| Image from Medical Graphics |
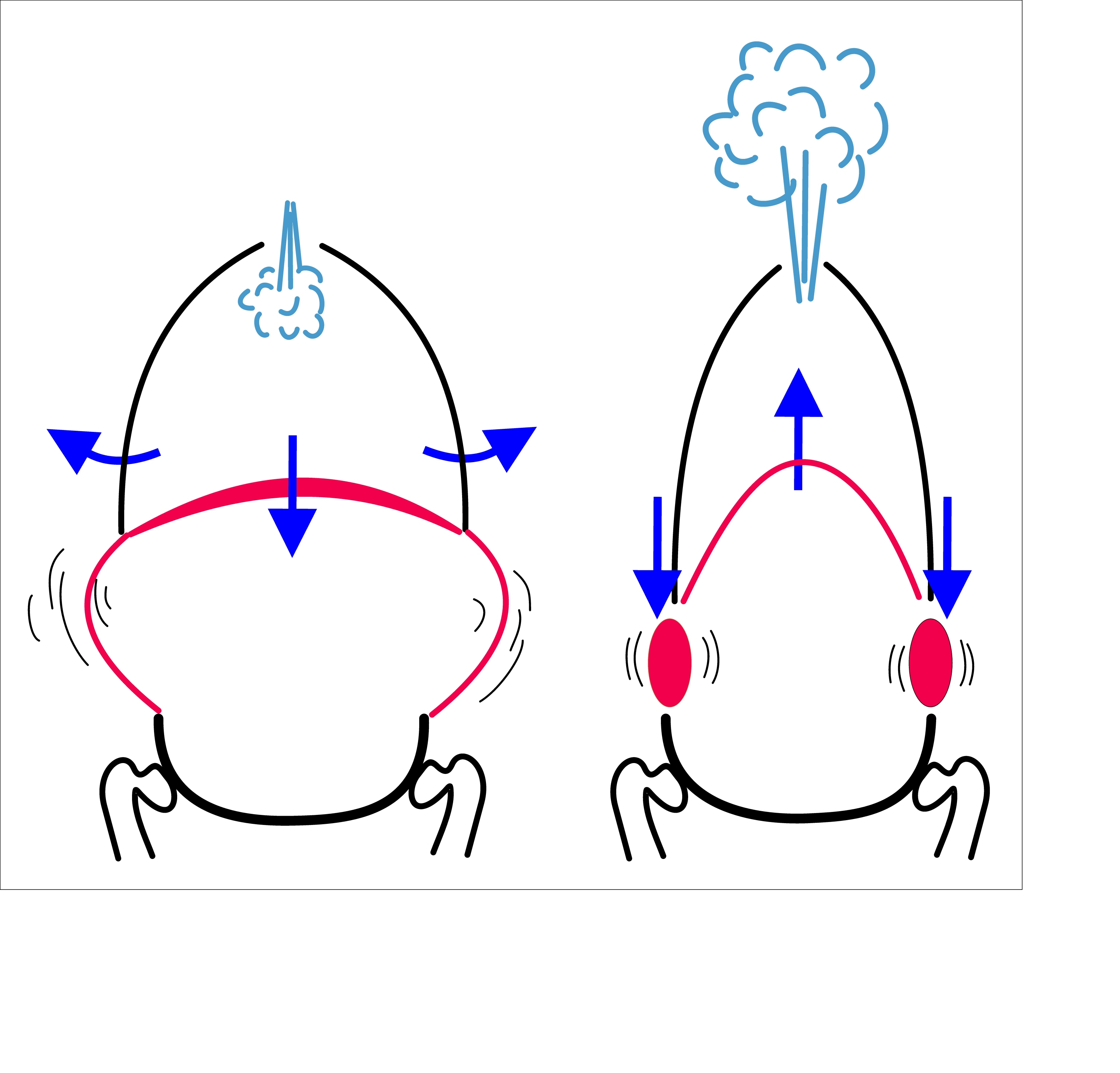
Whereas spirometry tests measure your lungs' overall strength, lung diffusion tests (also known as gas diffusion studies) specifically measure gas exchange, or how well your lungs can transfer gasses to and from your bloodstream. That is the lungs' primary purpose, after all: to absorb oxygen into your blood and remove carbon dioxide from it.
Your lungs do this via millions of tiny air sacs, called alveoli, which fill up with air when you breathe in. These alveoli are covered in tiny blood vessels with walls thin enough that gasses (oxygen and carbon dioxide) can passively move, or diffuse, in and out of the blood.
However, if these air sacs become damaged, then gasses cannot diffuse through them as easily, if at all. This type of lung damage is permanent and it is one of the defining characteristics of emphysema, one of the two main types of COPD.
In people with COPD, this lung damage continues to get worse and spread as the disease progresses. As more and more alveoli become damaged, less oxygen can diffuse into your bloodstream and less carbon dioxide can diffuse out.
That's why doctors perform diffusion tests on people with COPD and other lung disorders. By measuring how well gasses can diffuse through the alveoli in your lungs, diffusion tests help your doctor determine the nature and extent of any lung damage you have.
Taking a Lung Diffusion Test

Diffusion tests work like this: first, you breathe in a specially-formulated gas mixture through a mouthpiece and tube attached to a spirometer machine. This gas mixture is harmless and contains a specific amount of a “tracer gas,” usually carbon monoxide, which your lungs will process after you breathe it in.
Next, you hold your breath for about ten seconds in order to give the gas time to diffuse through your alveoli and get absorbed into your bloodstream. Then, you breathe out through the mouthpiece, which will deliver the exhaled air to the spirometer machine for analysis.
The machine then measures precisely how much carbon monoxide is in the air you exhaled. The more carbon monoxide left in the air, the less your lungs were able to absorb.
Essentially, healthier lungs will exhale less carbon monoxide, while damaged lungs will exhale more. The results of the test represent your lungs' diffu
If you have COPD, you're probably especially concerned about making healthy diet and lifestyle choices. You have to maintain your health carefully to prevent the disease from progressing, and that means eating nutritious foods and avoiding unhealthy and toxic substances.
As a result, many people are concerned about whether or not alcohol is dangerous for people who have COPD. Is it safe for COPD patients to drink alcohol, or can it make the disease even worse?
While alcohol isn't exactly healthy for anyone, the question of whether it's bad for your lungs or particularly dangerous for COPD isn't a simple question to answer. That's why, in this article, we're going to help you better understand the risks of alcohol and how it affects people with COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Risks of Alcohol Use
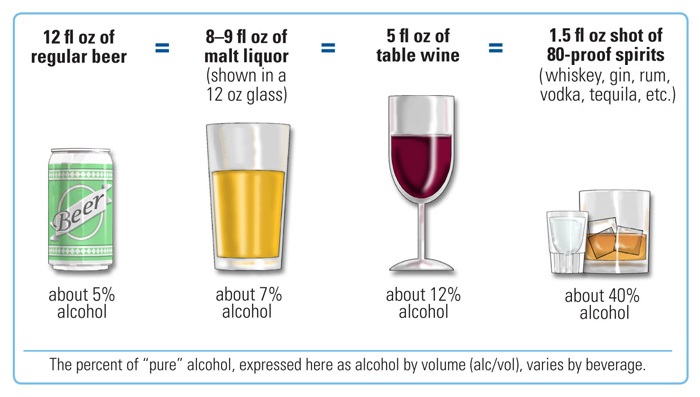
In general, light to moderate drinking isn't usually very bad for you, and most healthy adults who drink in moderation will suffer little to no long-term health problems. However, for people with chronic diseases like COPD, the mild toxic effects of alcohol may sometimes pose more of a risk.
Most of the short-term risks of alcohol concern the possibility of overdosing and the immediate effects of alcohol intoxication. These effects include impaired memory, balance, reflexes, and decision-making.
Alcohol is responsible for a large number of car accidents, falls, and other physical injuries that result from acute intoxication, which should be particularly concerning for people with limited physical strength and mobility. However, most of these effects disappear once the intoxication wears off.
Heavy alcohol consumption, however, can cause a variety of symptoms and health complications over the course of many years. You have a higher risk of experiencing these negative effects the more heavily you drink and the longer the period of time that you drink for.
Here are some common health complications for which long-term, heavy alcohol consumption increases your risk:
- Increased risk of certain cancers, including breast cancer, esophageal cancer, and pancreatic cancer
- Increased risk for respiratory infections
- Alcohol-related fatty liver disease
- Suppressed immune system
- Pancreatitis
- Nerve damage
- Ulcers
- High blood pressure
- Stroke
- Arrhythmia (irregular heartbeat)
- Heart disease
- Diabetes
Alcohol's Effect on the Body
Alcohol affects many different parts of your body in different direct and indirect ways. To understand how alcohol affects COPD, you first have to understand the general effects that alcohol has on your brain, heart, liver, kidneys, pancreas, and immune system.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa')}}
The Brain

The feeling of intoxication you get when you drink enough alcohol to get drunk comes mainly from alcohol's effects on the brain. But it also affects your brain in other ways; in the short term, alcohol affects the brain's ability to control your mood, your memory, and your impulse control.
Alcohol also impairs decision making, short-term memory, and can lead to anxiety and depression. In the long term, heavy alcohol use can cause permanent damage to the parts of the brain responsible for memory, motor skills, and emotional regulation.
The Heart

The short-term effects of alcohol on the heart are minimal. However, excessive, long-term alcohol consumption can cause serious damage to your heart and cardiovascular system.
Heavy alcohol use over many years can lead to high blood pressure, an irregular heartbeat, and elevated levels of fat in your blood. Over time, these cardiovascular changes can lead to much more serious health problems like diabetes and heart disease.
In the most severe cases, long-term, excessive alcohol consumption can even lead to stroke, cardiomyopathy, or sudden cardiac death.
The Liver

When you drink alcohol it is ultimately processed by the liver, which removes the alcohol from your blood and breaks it down into less toxic metabolites. However, these metabolites are also slightly toxic to the liver, and in large numbers can lead to problematic inflammation.
Small amounts of alcohol are not enough to cause any permanent damage to your liver, but when you drink too much at once, the liver gets overloaded with metabolites and becomes inflamed. Over time, this inflammation can lead to permanent scarring in the liver and fatty liver disease. In fact, alcohol is responsible for more than a third of cases of liver disease that end in death.
The Kidneys

Alcohol is a diuretic, meaning it causes you to urinate more frequently and get dehydrated more quickly. However, this also affects your kidneys' ability to regulate the amount of nutrients and electrolytes in your body.
Essentially, alcohol's diuretic effects causes nutrients and electrolytes to be lost when you urinate, leading to deficiencies in sodium, potassium, chloride ions, and other substances. This can lead to a variety of symptoms, including fatigue, nausea, irregular heartbeat, and gastrointestinal discomfort.
Over a long period of time, heavy alcohol use can cause permanent damage to the kidneys, including kidney enlargement and dysfunction in the balance of hormones that regulate kidney function.
The Pancreas
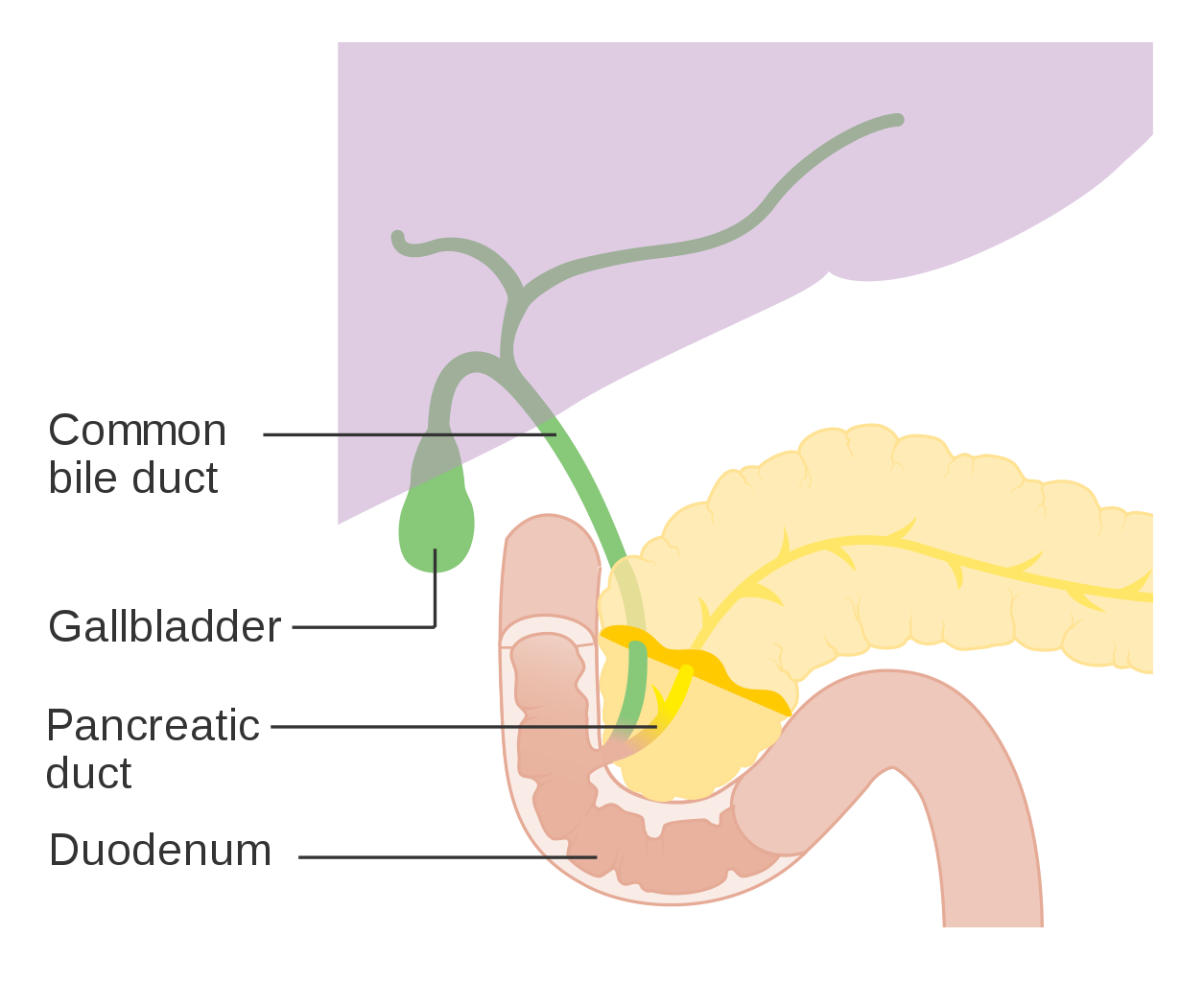
Excessive alcohol use can cause both short-term and long-term problems in your pancreas and interfere with your digestion. In the short term, it causes a build-up of digestive enzymes in the pancreas, which can lead to acute inflammation known as pancreatitis.
Pancreatitis causes a number of uncomfortable symptoms like nausea and diarrhea and can take weeks to recover from. If pancreatitis becomes chronic and is not treated properly, it can cause permanent damage to the organ and lead to diabetes or death.
Immune System

Drinking too much alcohol can significantly reduce your immune system's ability to stave off illnesses and infections. Even a single episode of heavy drinking can inhibit your body's ability to fight viruses and bacteria for up to 24 hours.
Studies even show that chronic, heavy drinkers are more prone to contracting contagious diseases like pneumonia, tuberculosis, and HIV. It also makes it harder to fight off any sicknesses you already have, meaning you might stay sick longer and experience worse symptoms.
This is of particular concern to people with COPD, who must be ever vigilant to avoid illnesses and infections. Even minor colds can lead to serious COPD exacerbations, and recovering from illnesses quickly is key for preventing further damage to the lungs.
Research on Alcohol and COPD

As you can see, heavy alcohol use can be detrimental to anyone, including people with COPD, for a variety of reasons. But is there anything that makes alcohol particularly dangerous for people who suffer from chronic respiratory diseases?
The answer is, “probably, yes,” but to what extent alcohol is dangerous for COPD patients is a difficult question to answer. There hasn't been much scientific research in this area which makes it difficult to discern how alcohol affects people with COPD specifically.
The body of research is not robust enough to form firm scientific conclusions and many of the studies that have been done on alcohol and COPD are poorly controlled and contradictory. Many also fail to separate the effects of drinking and smoking, which makes it impossible to tell whether or not negative health effects are the result of alcohol or tobacco consumption.
What research has been done focuses mainly on the effects of alcohol on lung function, dietary health, and medications. One thing that most researchers agree on is that heavy alcohol consumption can effect the lungs and can likely cause reduced lung function in people with chronic respiratory diseases.
In general, heavy alcohol use in the general public is associated with reduced lung function and airflow obstruction. However, this is difficult to study in populations of people with COPD, since COPD patients experience chronic airflow obstruction that makes it difficult to detect minor changes.
Some studies, however, have hinted at a link between heavy alcohol use and increased severity of COPD. For example, alcohol may be linked to increased coughing, wheezing, and breathlessness in patients with respiratory diseases who drink, and one study found that right-sided heart failure is more common in heavy drinkers who also have COPD.
Other studies show that alcohol can interfere or interact with certain medications used to treat COPD. Heavy drinking can also cause nutritional deficiencies and even make your lungs more prone to being damaged by smoking.
Clearly, people with COPD should be cautious about drinking alcohol. To help you better understand the risk, the following sections will explain in more detail how alcohol can affect your lungs, nutrition, and even interfere with COPD treatments.
Continue reading to learn more about the risks of alcohol use for COPD patients and how to reduce your risk if you suffer from the disease.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Alcohol Can Increase COPD Symptoms and Make You More Likely to Get Sick
|
|
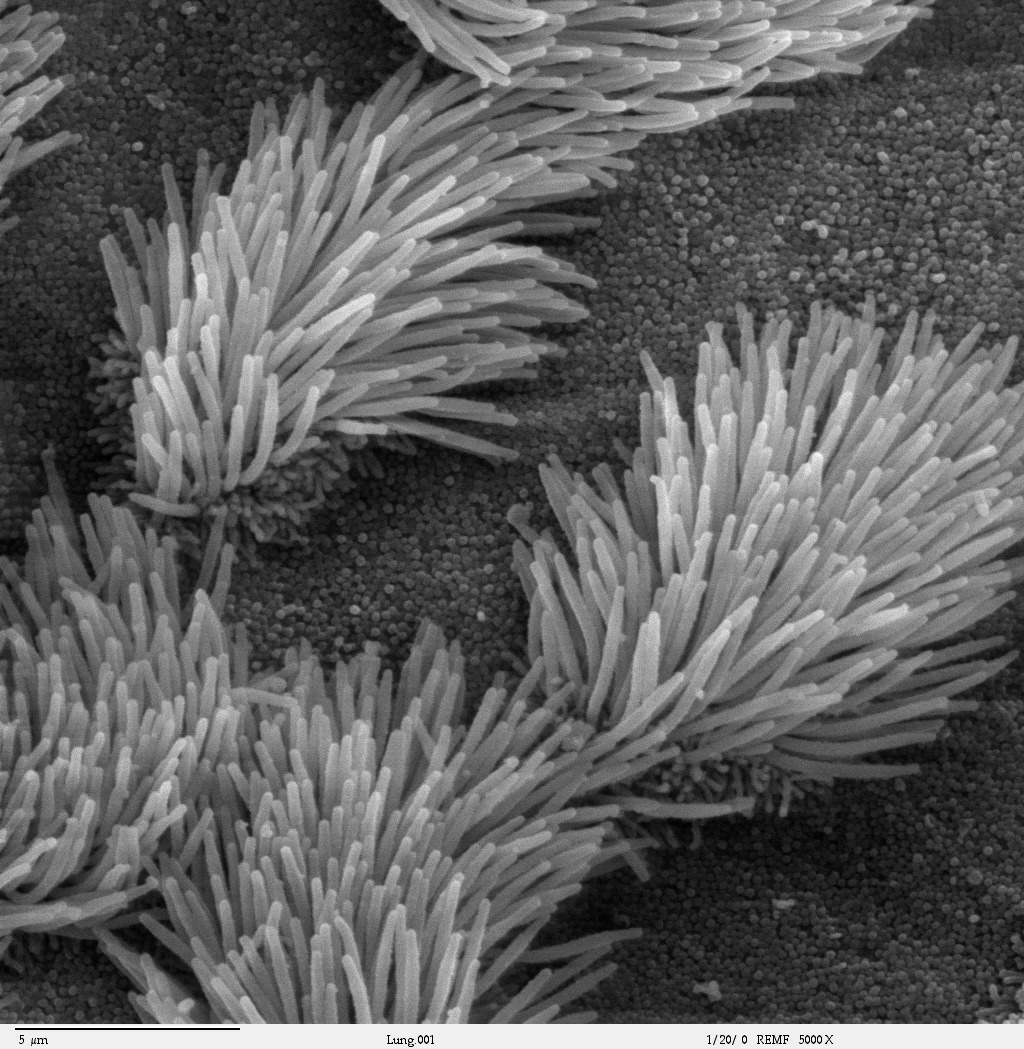
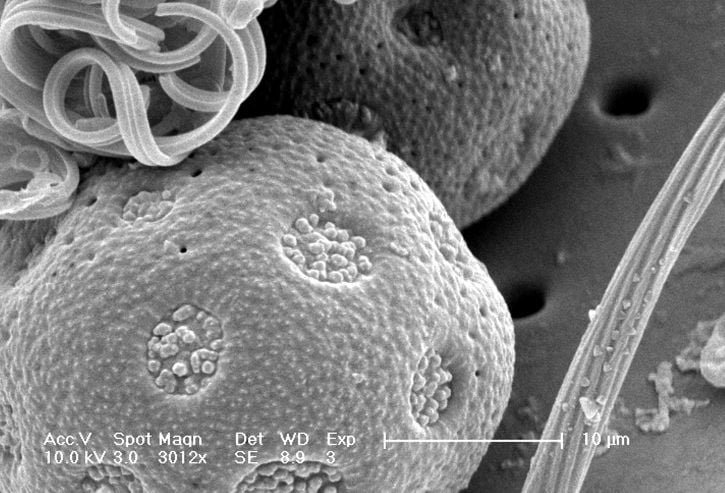
| Alcohol makes it more difficult for your cilia (pictured above) to clear mucus out of your lungs and airways. |
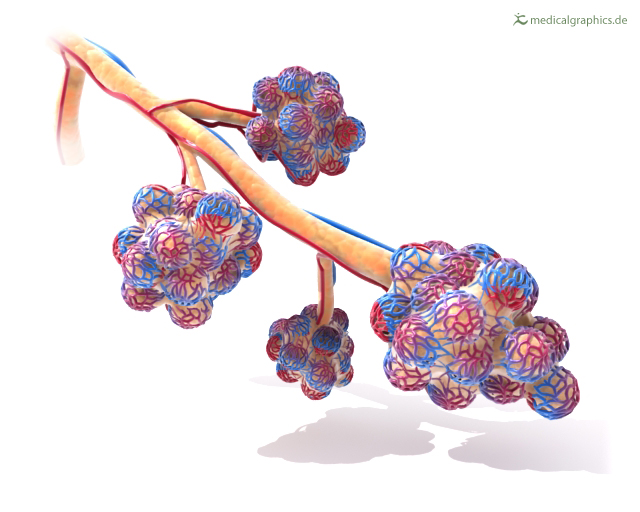
The main way that alcohol affects the lungs directly is by inhibiting their ability to move mucus up and out of the lungs. It does this in two main ways: by thickening your mucus and by suppressing the movement of cilia, which move mucus through your airways.
Thickened mucus happens as a result of dehydration, which happens more quickly when you drink alcohol. As a diuretic, alcohol flushes water out of your body, which in turn dries up your mucus, making it extra thick and sticky.
Alcohol also has a direct effect on the cilia in your airways, which work continually to keep too much mucus from building up in your lungs and airways. Cilia are finger-like protrusions that from a carpet lining the surface of your airways.
In order to get mucus up and out of your lungs, the cilia have beat back and forth to move the mucus in the right direction. Alcohol makes these cilia less responsive and less active, which makes them much less effective at doing their job.
All of this causes more severe COPD symptoms as a result of the thickened mucus building up to excess in your lungs. The mucus obstructs the flow of air through your airways, causing worsened coughing, wheezing, and and overall worsening of lung function.
This also makes you you more prone to contracting illnesses and infections. This happens because the thick mucus traps bacteria, providing an ideal, moist environment for them to live and multiply. It is also much harder for the cilia lining your airways to move that thick, sticky, bacteria-ridden mucus out of your lungs, significantly raising the risk of respiratory infections.
On a slightly different note, alcohol can also affect your lungs by making them more sensitive to cigarette smoke. It reduces the levels of an enzyme that helps protect your lungs from damage and inflammation caused by smoking.
How to Reduce Your Risk:
-
Drink plenty of water, especially when you drink alcohol. You should drink at least one glass of water for every alcoholic drink you consume.
-
Only drink in moderation. Heavy alcohol use is associated with worse dehydration and reduced cilia function.
- You should always avoid smoking, but especially when you drink. Studies show that smoking and drinking alcohol together is worse for your lungs than smoking alone.
Alcohol Can Interact and Interfere with Certain Medications Used to Treat COPD

You should always consider what medications you are taking before you choose to drink. Some medications used to treat COPD cause uncomfortable side effects or can be dangerous when combined with alcohol.
For instance, many antibiotics are known to not mix well with alcohol, causing uncomfortable side effects like dizziness, drowsiness, and stomach distress. Since doctors often prescribe antibiotics to COPD patients in order to treat lung infections and exacerbations, this is something you should keep in mind if you have COPD and choose to drink.
Certain antibiotics, including Bactrim, Flagyl, and Tindamax can have even more severe effects when mixed with alcohol. This can result in symptoms like nausea, vomiting, flushing, and a rapid heart rate.
Additionally, some corticosteroid medications used to treat lung inflammation in COPD patients can be dangerous if you mix them with alcohol. This is especially true if you are taking steroids long-term or if you drink heavily.
Alcohol and corticosteroids are both irritating to your stomach and digestive tract, and consuming both together increases your risk of stomach ulcers and indigestion. Additionally, both alcohol and corticosteroids can contribute to high blood sugar, osteoporosis, liver damage, and immune system suppression on their own, making it even more risky to take both at the same time.
Finally, drinking alcohol in combination with anti-anxiety and antidepressant medications can have severe, and even deadly effects. Consuming them together can cause you to become excessively sedated and cause dangerous spikes in blood pressure. In the most severe cases, mixing alcohol and antidepressants can slow your heart rate and breathing to dangerously low levels.
How to Reduce Your Risk:
-
Go over your complete list of medications with your doctor or pharmacist to make sure that none of them will interact with alcohol.
-
Make sure to check with your doctor about drug interactions and side-effects whenever you are prescribed a new medication.
-
If you take an antidepressant medication to treat anxiety or depression, you should abstain from drinking.
- Abstain or moderate your drinking carefully whenever you are prescribed a course of antibiotics or corticosteroids.
Alcohol Can Reduce Sleep Quality and Increase COPD Symptoms When You Sleep

Alcohol acts as a depressant, which means it relaxes your muscles and slows down many of your body's normal processes. During the daytime, this might just make you feel relaxed and a little drowsy, but at night it can severely hurt your quality of sleep.
Although many people use the relaxing effects of alcohol as a sleep aid, it's actually more likely to interfere with a good night's sleep. When you drink before bed, the alcohol disrupts your brain's normal sleep cycles. As a result, your sleep quality is lower and you have an increased risk of waking up and not being able to sleep in the morning.
Drinking alcohol at night can also affect your sleep in other ways—by affecting the muscles in your throat and worsening obstructive sleep apnea. And since sleep apnea is very common in people with COPD (known as overlap syndrome), this is a concern that affects a large number of patients.
Here's what happens: drinking alcohol at night can cause the muscles lining the airways in your throat to relax too much when you fall asleep, causing them to sag and obstruct your airways. This makes it more difficult to breathe and can reduce the amount of oxygen you get while you sleep.
This can trigger sleep apnea or worsen pre-existing sleep apnea symptoms, which can make it difficult for your body to get enough oxygen while you sleep. This can cause hypoxemia (low blood oxygen levels) which, over time, can lead to a variety of severe and life-threatening health complications in people with COPD.
Alcohol-related dehydration can also make it difficult to sleep, because it causes extra, thick mucus to build up in your airways. This mucus can obstruct your airways at night, causing you to cough and making it difficult to breathe while you sleep.
Many people with COPD already struggle with breathlessness, wheezing, and airway obstruction that makes it difficult to sleep at night. It's important to remember that alcohol will only make those symptoms worse.
Getting sufficient, good quality sleep is necessary for staying healthy and living a fulfilling life with COPD. Studies even show that poor sleep can increase your risk for COPD exacerbations, worsened COPD symptoms, and cause a wide variety of additional health problems like heart disease, diabetes, high blood pressure, and stroke.
However, as many as 70 percent of people with COPD struggle to sleep and get poor sleep on a regular basis. It's important to do everything you can to reduce your symptoms and get good quality rest, and that may include abstaining from alcohol at night.
How to Reduce Your Risk:
- Always drink in moderation. The more alcohol you drink, the stronger its depressant effects and the more likely it is to interfere with your sleep.
- Don't drink alcohol too close to bedtime.
Alcohol Can Cause Enzyme Deficiencies in People with COPD

Heavy alcohol use can suppress, inhibit, or deplete a variety of essential nutrients, electrolytes, and antioxidants that your body needs to stay healthy. The most notable for people with COPD, however, is an antioxidant known as glutathione, an antioxidant found in the lungs.
Glutathione helps protect your lungs from damage and inflammation caused by exposure to smoke, pollution, and other respiratory irritants. A deficiency in this antioxidant, which can happen if you drink heavily, can increase your risk for lung damage, exacerbations, and worsened COPD symptoms.
Heavy alcohol use can also cause deficiencies in important vitamins, especially vitamin B, vitamin A, vitamin B12, and folic acid. Additionally, alcohol contains a large number of calories, which can lead heavy drinkers to eat fewer nutritious foods or to become overweight.
How to Reduce Your Risk:
-
Always drink in moderation. Heavy alcohol consumption increases your risk for nutritional deficiencies and depletes glutathione in your lungs.
- If you drink, have your doctor test you for vitamin deficiencies. If you are deficient, you can increase your vitamin uptake by adjusting your diet or taking vitamin supplements.
So, Can You Drink Alcohol if You Have COPD?
|
|
| Photo by Sgt. Marc |
There's a lot of information available about how alcohol negatively affects your body and how drinking too much can affect your COPD. However, most of the available science focuses on the effects of heavy and excessive drinking. You might still be wondering, can I still drink in moderation if I have COPD?
As you might have guessed, the answer is not straightforward. You will need to talk to your doctor, who will take your unique medical history and physical condition into account, to know whether or not light or moderate drinking is safe for you.
If you do drink, you should take special care of yourself to minimize any negative effects that alcohol might have on your lungs or your COPD symptoms. Drink only in moderation, eat a healthy diet, and drink extra water to prevent thickened mucus and dehydration.
However, in most cases, drinking occasionally should be fine as long as you don't drink to excess and follow the guidelines recommended by the CDC. “Drinking alcohol [when you have COPD] isn't forbidden,” says pulmonary specialist Dr. Pichurko, “but if you drink, moderation is a must.”
As soon as the cold weather creeps in, it's inevitable that wood-burning stoves start firing up all across the country. For many people, burning wood is a long and cherished tradition, both for warmth and for recreation.
Unfortunately, most people don't realize how devastating wood smoke can be to their health. Research shows that it may even be twelve times more dangerous than cigarette smoke when breathed in similar quantities.
The truth is, burning wood in your home can increase your risk for a variety of serious health problems, including heart disease and COPD. It can also cause serious respiratory symptoms in healthy adults and especially in people with COPD.

Fortunately, wood smoke is not an issue for most people who only encounter it occasionally at bonfires and barbecues. However, there is still a large number of people—especially those who use wood furnaces to heat their homes—who get exposed to wood smoke much more frequently.
Unfortunately, those most at risk from wood smoke are those who already suffer from lung diseases like COPD. Even small amounts of wood smoke can cause serious breathing problems for people who suffer from asthma, COPD, and other respiratory problems.
That's why an important part of staying healthy with COPD is knowing how to recognize and avoid respiratory hazards, including wood smoke. That means avoiding all sources of pollution and especially keeping the air inside your home healthy and clean.
That's why, in this guide, we're going to tell you everything you need to know about wood smoke and COPD. We'll explain how wood smoke affects your lungs, how it can worsen COPD, and how to avoid exposing yourself to harmful quantities of wood smoke.
We'll also discuss how using a wood-burning stove for heat is a major source of indoor air pollution and extremely hazardous for people with COPD. To help you keep your lungs healthy, we'll show you a variety of things you can do to make your wood-burning appliances safer or replace them with less hazardous alternatives.
Why Wood Smoke is So Bad For You

Wood smoke and COPD have one main thing in common: they both cause irreparable damage to your lungs over time. Wood smoke is also a serious respiratory irritant that can exacerbate the symptoms of COPD and other respiratory diseases.
Wood smoke is dangerous for two main reasons: First, it releases dangerous amounts of tiny particles that get trapped in your lungs when you breathe them in. Second, it emits a variety of toxic gases that can damage your lungs and impair your ability to breathe.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
These toxic substances can trigger serious immediate symptoms as well as long-term heart and respiratory problems. That's why many health and advocacy organizations strongly warn against the practice of using wood to heat your home.
According to the Utah Physicians for a Healthy Environment, “wood smoke is uniquely toxic among all sources of urban air pollution.” This is in part because particle pollution from wood smoke is “extraordinarily small” and has the ability to causes prolonged damage to your body's cells.
Toxic Fumes from Wood Smoke

When wood burns (or combusts), it releases a wide variety of gases that are harmful to your lungs. These gases hurt your respiratory system mainly through inflammation, damage to delicate lung tissues, and by limiting your lungs' ability to absorb oxygen when you breathe.
Here's a quick snapshot of just a few of the many toxic fumes found in wood smoke:
- Nitrogen Oxides: can cause lung and airway irritation, shortness of breath, and an increased risk of lung infections, particularly for people with asthma or COPD
- Volatile Organic Compounds: can irritate the respiratory tract and some can even cause cancer
- Formaldehyde: can cause eye irritation, headaches, and can trigger respiratory symptoms like coughing and wheezing
- Hydrocarbons: cause lung inflammation, respiratory symptoms, and can cause lung diseases like asthma and COPD
- Benzene: can cause anemia, excessive bleeding, and suppress your immune system
- Sulfur Dioxide: causes eye irritation, respiratory inflammation, and bronchospasms, especially in people with COPD and other respiratory problems
- Dioxins: can cause cancer
- Carbon Monoxide: reduces your lungs' ability to absorb oxygen, straining your lungs and cardiovascular system; it can both cause and worsen respiratory symptoms and, in high enough levels, cause suffocation
- Acrolein: can irritate your eyes and respiratory tract
Ultra-fine Particles from Burning Wood
Wood smoke contains tons of microscopic particles, often called ultrafine particles, which experts consider to be the greatest health hazard caused by smoke. When you breathe in air contaminated by these tiny particles, they get trapped and stay deep inside your lungs.
The most dangerous ultrafine particles are known as PM2.5, which stands for particles that are smaller than 2.5 microns across. For reference, that's about half the size of a red blood cell or 30 times smaller than the width of a human hair.
Wood smoke produces a large number of PM2.5 particles, which are incredibly toxic to your lungs and cardiovascular system. These ultrafine particles can also irritate your eyes, your nose, and even your digestive system.
These tiny airborne particulates have been proven time and time again to be directly linked to a variety of serious respiratory and cardiovascular conditions. These include respiratory decline, asthma, heart disease, COPD, and chronic respiratory symptoms.
Fine particulates can even trigger heart attacks in people with existing cardiovascular disease, a health problem that is very common among COPD patients. Particle pollution is also linked to premature death in people suffering from heart disease and COPD.
You are more likely to develop health problems when the concentration of particulates in the air is high and you are exposed to them regularly over a long period of time. One common way that people get exposed to harmful levels of particle pollution long-term is by using wood-burning appliances to heat their homes.
Wood Smoke and COPD
Smoke from wood-burning stoves and fireplaces is both a cause of COPD and a major hazard for people who have COPD already. That's why it's so important for all people, and especially COPD patients, to be aware of the dangers of wood smoke.
Most importantly, you should never rely on a wood-burning stove to heat your home during the winter if you suffer from COPD. The indoor pollution it creates, even if it's only minor, is simply too much to risk for someone with a serious respiratory condition.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
COPD makes your lungs much more sensitive to the damaging effects of harmful particles and gases. That means it takes less smoke to inflame your lungs and trigger respiratory symptoms.
Even a tiny amount of smoke could make you feel breathless or bring on a serious coughing fit. Even if you don't experience any immediate effects, being around wood smoke can still harm your lungs.
Like any source of pollution, breathing in the toxic byproducts of burning wood too often could cause your COPD to progress even faster. It can speed up lung function decline and cause permanent worsening of existing COPD symptoms.
That's why using a wood-burning stove to heat your home throughout the winter is such a major risk. Even if you take the proper precautions, you could still get exposed to enough wood smoke pollution over time to experience negative health effects.
Having COPD means your lungs are already damaged and you only have a limited amount of lung function remaining. The risk of losing even more lung function is just not worth using a wood-burning stove for heat.
How Much Wood Smoke is Too Much?

Burning wood in the fireplace every once in awhile isn't likely to cause major problems for most people. However, burning wood in your home frequently over many years can seriously damage your lungs.
Most of the risk from wood-burning stoves and fireplaces comes from how it can damage your lungs and cardiovascular system over the long term. That's why heating your home with a wood-burning stove is so much more dangerous than using your fireplace once in awhile; wood-burning furnaces have to run 24/7 all winter long to keep your house warm.
That adds up to months and months of exposure to wood fumes and particulates for many hours every day. What's more, the pollution can remain in your home for days or weeks after you stop burning wood, affecting you long after the winter is over.
Ultrafine particles don't disappear on their own, and they are small enough to pass straight through the vast majority of air filters. As a result, they continue to circulate through the air in your home until they settle into a fine dust on your walls, furniture, and floors.
This toxic particulate matter is especially pesky to get rid of because it constantly cycles between settling and getting kicked back up into the air. It may take multiple deep cleans and airing out your house to to get rid of all the particle pollution left over from weeks or months of burning wood.
However, the dangers of wood smoke are still very much present even if you don't burn wood every day. Even short-term exposure can irritate your lungs, which can cause serious problems for people with COPD.
If you have COPD, asthma, or any other respiratory problems, then breathing in any amount of wood smoke can be harmful. It can cause serious immediate symptoms as well as long-term damage that can make your existing chronic symptoms even worse.
What About “Safe” Wood-burning Systems?

You might think that having a modern, efficient, professionally-installed wood stove is enough to keep you safe. Unfortunately, no matter what precautions you take, burning wood can still endanger your health.
While modern, EPA-approved wood-burning stoves are much safer than older appliances, no wood-burning appliance is completely safe. There is always a risk that smoke or particulate matter could make it into your home.
Even well-ventilated wood-burning furnaces can still leak a steady stream of pollutants that build up in the air indoors over time. You release even more harmful gases and particles into your home every time you open the furnace door.
It's nearly impossible to burn wood in a wood stove or fireplace without introducing wood smoke pollution into your home. A good rule of thumb is that if you can smell the fire at all, then you are inevitably also breathing in the toxic gases and ultra-fine particulates from the smoke.
No matter how you cut it, burning wood for heat is much riskier than using a modern gas or electric furnace. If you have COPD, asthma, or another respiratory condition, it's always best to assume that no wood-burning appliance is safe, especially for extended periods of use.
Other Wood-Burning Hazards
There are other costs to burning wood besides the negative effects on your health. Wood-burning stoves and fireplaces are actually a major cause of environmental pollution and cause more than fifteen thousand house fires every year.
Pollution Caused by Wood Burning

In addition to polluting the air indoors, home wood-burning also causes a surprising amount of outdoor air pollution. In fact, the World Health Organization estimates that outdoor pollution caused by residential wood burning caused approximately 9,200 deaths in the US in 2010.
In te San Francisco Bay area, nearly thirty percent of the particle pollution present during the winter comes from wood-burning in home fireplaces and stoves. Other studies show that burning wood creates even more pollution than burning oil, coal, or gas.
This is one of the major reasons why countries around the world discourage wood burning and urge people who do burn wood to use more modern, efficient stoves. Doing so could significantly reduce outdoor air pollution during the winter months and reduce the risk your wood stove poses to your fellow neighbors and citizens.
Fires Caused by Wood Burning

Every year in the US, about thirty people die and eighty people are injured in house fires caused by wood-burning stoves and fireplaces alone. Contrary to what most people believe, the vast majority of these deaths and injuries are the result of smoke inhalation rather than burns.
Uncontrolled fires release massive amounts of noxious fumes and fine particles that build up quickly inside a house. Just a couple minutes of breathing this smoke can cause smoke inhalation, respiratory failure, and permanent lung damage.
Smoke inhalation is life-threatening for healthy adults, but it's even more deadly for people with COPD and other lung diseases. Since their lungs already function poorly, COPD patients are much more vulnerable to suffocation and suffering from disabling breathing problems from the smoke.
That's why, if you burn wood in your home, it's important to consider the immediate risk of uncontrolled fires as well as the long-term costs to your health. Even if you escape from a house fire without getting hurt, the smoke you inhaled in the meantime could still cause serious, long-term damage to your lungs.
Alternatives to Burning Wood for Heat

If you use a wood-burning stove or furnace to keep your home warm, it may be time to consider upgrading to a better heating system. There are several other home heating options that are both cheaper and more efficient than burning wood for heat.
Despite what many people believe, heating your home with wood is not exactly budget-friendly. In fact, wood-burning stoves and furnaces are generally more expensive to run than other home heating options.
Even if you are hesitant to take on the initial cost and hassle of replacing your home heating system, remember that doing so may actually save you money in the long run. Even if you have to take a temporary hit to your budget, you can't place a value on the benefit of protecting yours and your family's health.
Here are some of the benefits of switching to a non-wood-burning heating system:
- Fewer emissions and outdoor pollution
- Significantly less indoor pollution
- Extremely simple to use and maintain
- More energy-efficient
- More effective at heating
- Often cheaper to run and maintain
- Eliminates the need to buy or store fuel
Here are some home heating options that don't burn wood:
- Central gas heating furnace
- Central electric heating furnace
- Boiler (radiant heating system)
- Solar Heater
- Heat Pump
How to Make Your Wood-Burning System Safer
Ideally, you should not use a wood-burning stove at all, especially if you have COPD. Just about any other heating option is better and safer for your lungs and overall health.
However, if you still choose to use a wood stove or furnace, there are many things you can do to reduce your risk. If you follow he best wood-burning practices, you can minimize the amount of harmful pollution your wood-burning stove emits into your home.
Get a Modern, EPA-Approved Appliance

There are many reasons to upgrade your old wood-burning stove to an EPA-certified model. Modern wood-burning stoves are much more efficient, environmentally-friendly, and significantly safer than older wood-burning appliances.
Unfortunately, the EPA estimates that 65% of wood stoves in the US are old and inefficient models. If your home uses one of these older stoves, then upgrading to a newer model could significantly reduce the risk it poses to yours and your family's health.
Here are some more benefits of using an EPA-certified wood-burning stove:
- They reduce pollution by 50-60 percent
- They use less fuel (about one-third less wood)
- They burn fuel more efficiently
- They circulate heat more efficiently (less heat loss)
Because of new EPA regulations introduced in 2015, nearly all wood-burning heating appliances now sold in the US must meet the EPA's requirements. These requirements are designed to reduce both indoor and outdoor pollution by ensuring that wood stoves emit no more than 4.5 grams of particulate matter per hour.
That means just about any wood stove that you buy from a US retailer should be EPA-certified and create relatively low amounts of pollution. However, even the safest wood-burning stove is still less safe and more polluting than non-wood-burning heating appliances.
If you use an older wood stove and you or anyone else in your household suffers from COPD, then upgrading your furnace should be a top priority. Home wood-burning is simply too hazardous for vulnerable lungs, especially if you don't use an appliance that meets modern safety standards.
Depending on where you live, you may even be eligible to participate in a wood stove change-out program. These programs may be able to help you cover some of the cost of installing a more efficient wood stove (or another type of heating system) if you otherwise couldn't afford to replace your old, inefficient stove.
To learn what options are out there, take a look at the EPA's complete list of certified wood stoves here. You can also contact your local air quality agency to see if there are any wood stove exchange programs in your area that can help you manage the cost.
Opt for a Pellet Stove

If you must use a fuel-burning appliance to heat your home, you should know that there are other options besides a typical wood-burning stove or furnace. One of these options is a pellet stove, which is generally cleaner and safer to use than a traditional wood-burning stove.
Pellet stoves are a special type of fuel-burning appliance that burn small manufactured pellets instead of firewood. These pellets are usually made up of compressed sawdust or wood chips, but some stoves can also burn pellets made of compacted paper, grass, corn, and other organic materials.
Of all of the different wood-burning appliances out there, pellet stoves are often considered the most clean and efficient option. They produce less smoke and are much easier to use and manage than traditional wood-burning stoves.
One thing that makes pellet stoves cleaner than wood-burning stoves is the type of fuel they use; pellets are reliably drier and more uniform in shape and size than firewood. Pellets are manufactured to contain just the right amount of moisture, and they tend to burn more evenly and completely in the stove.
It also takes much less effort to keep a fire going in a pellet stove. Most have auto-start ignitions and automated pellet feeding systems that make re-fueling the stove incredibly easy. In fact, most pellet stoves can keep themselves going for about 24 hours on a single hopper load.
Pellet stoves also get hotter because they use fans to circulate the air in the stove and ensure minimum heat loss. Unlike wood stoves, pellet stoves require electricity to power the hopper, ignition, and fans.
Pellet stoves generally cost about the same price as a typical wood-burning stove, but the fuel can b
They're in the air, in our homes, and in a wide variety of products we use every day—volatile organic compounds (VOCs) are everywhere. Unfortunately, exposure to too many VOCs can be bad for your health and particularly dangerous for your lungs.
VOCs are a major source of air pollution, and they can cause a variety of respiratory problems including lung irritation, lung tissue damage, and serious lung diseases. Certain VOCs can also worsen existing breathing disorders like asthma and COPD.
Fortunately, you can limit your exposure to harmful VOCs if you learn how to recognize and avoid them. That's why, in this post, we're going to tell you everything you need to know about volatile organic compounds and your lungs, including how to protect yourself from hazardous VOCs.
We'll explain what VOCs are, where they come from, and what the research says about how they affect your health. We'll also show you which volatile organic compounds are most harmful to your lungs and how you can minimize your exposure to them at home.
Being able to identify and avoid breathing harmful VOCs is a valuable skill to have, especially if you suffer from a lung condition like COPD or asthma. Even if you are a healthy adult, learning about VOCs can help you make better choices that keep your lungs safe, healthy, and strong.
What are Volatile Organic Compounds?
Volatile organic compounds, or VOCs, are essentially just carbon-based chemicals that can quickly evaporate into a gas or vapor. Previously, VOCs were known throughout the US as reactive organic gases (ROG's), a term you might still come across today.
Whether or not you've ever heard about volatile organic compounds before, you almost certainly encounter many of them every day. Some of these VOCs are completely harmless, but some are dangerous chemicals that can have serious effects on your health.
When makes volatile organic compounds unique is that they evaporate very quickly, and the vapors they release mix into the air the air we breathe. This is how most people get exposed to VOCs both inside and outside their homes: simply by breathing and inhaling them into their lungs.
It's important to understand that “volatile organic compound” is a very general term that encompasses a huge variety of both natural and man-made chemicals. In fact, most of the things we consider to be fragrances or scents actually come from VOCs.
All VOCs are different, each with unique toxicities and varying levels of health risk. Some can only harm you in large amounts, some are toxic in lesser amounts, and some pose little, if any, danger to your health at all.
However, many VOCs are harmful, which is why many are classified as carcinogens, air pollutants, and even explosion risks. Some of the most common and dangerous VOCs are lung irritants which can irritate your airways, damage your lungs, and cause a variety of other serious respiratory conditions.

Volatile organic compounds can affect a variety of different systems and organs in the body, and what levels of exposure are considered “safe” vary significantly between VOCs. But as scientists continue to study their effects, some VOCs are turning out to be even more hazardous than originally thought.
For example, some VOCs become even more potent pollutants when they react with other gases in the air, like nitrogen oxide, to form ozone. Researchers are just now beginning to understand how serious this problem is, and have found that everyday products and chemicals containing VOCs are starting to rival vehicle emissions as a primary source of air pollution.
VOC-catalyzed ozone is particularly harmful because it collects at ground level where we breathe, and it's responsible for variety of short-term and long-term health effects. VOCs also contribute to the formation of fine particles in the air, which is another hazardous type of air pollution.
Here are some examples of common volatile organic compounds you might have heard of before:
- Isopropyl alcohol: used in cleaners and disinfectants
- Acetone: found in nail polish remover and paint removers
- Formaldehyde: found in building materials and molded plastics
Where Do VOCs Come From

Many of the most harmful VOCs come from fuel and manufacturing emissions, including gasoline, diesel fuel, and industrial processes. Others come from chemicals used in commercial products and materials like treated lumber, cleaning chemicals, and paint.
Many pesky airborne irritants, the kinds that make your eyes water or tickle your nose, are actually volatile organic compounds. So are many of the fragrances and chemicals found in basic products that you might use in your home every day.
In fact, common household products containing VOCs, such as cleaning solutions, furniture, and cosmetic fragrances, are a major cause of indoor air pollution. These VOC's, along with those caused by industrial emissions, make their way outdoors where they contribute heavily to smog and and other forms of outdoor air pollution.

Wood smoke and tobacco smoke also contain hazardous levels of volatile organic compounds, which are partially responsible for the deadly health effects of smoking. Unfortunately, tens of millions of Americans regularly inhale VOC's from cigarettes, second-hand smoke, wood-burning stoves, and hazardous workplaces.
Here are some examples of some common products and processes that expose you to harmful VOCs.
Sources of VOCs In and Around Your Home
- Cleaning solutions & disinfectant sprays
- Air fresheners and other artificial fragrances
- Cooking fumes
- Cigarette smoke
- Wood-burning fireplaces
- Scented hair, body, and cosmetic products
- Burning oil or fuel indoors
- Fireplaces and wood-burning stoves
- Pesticides and moth repellent
- Dry-cleaned clothing
- Furniture
- Many glues and adhesives
- Permanent markers, art paints, and other hobby or crafting supplies
- Varnishes and finishes
- Building materials: e.g. paint, paint remover, caulk and sealants, carpet, and flooring (The amount of VOCs emitted by these products declines over time.)
Sources of VOCs Outdoors
- Automobile emissions
- Diesel emissions
- Power plant emissions
- Fuel extraction and processing
- Manufacturing plant emissions
- Emissions from other chemical and industrial processes

How Dangerous are VOCs?
Fortunately, most of the harmful volatile organic compounds only pose a serious danger in large doses or long-term exposures. If you have healthy lungs and only get exposed to small amounts of VOCs, then you are unlikely to experience any major health effects.
However, people with existing lung diseases are often much more sensitive to the effects VOCs. For these people, even low VOC concentrations in the air can trigger respiratory symptoms like coughing and shortness of breath.
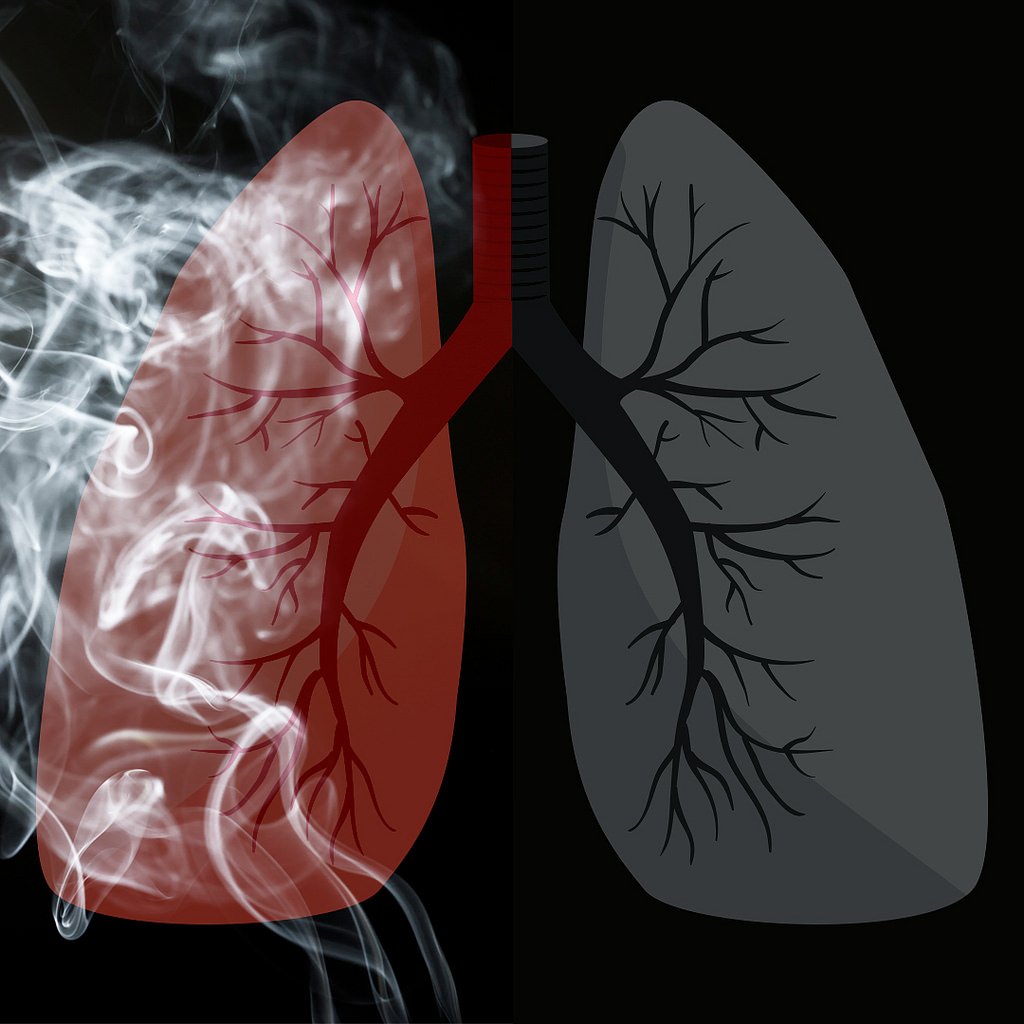
Still, even healthy people can experience short-term and long-term symptoms from low or moderate exposure to certain volatile organic compounds. Many people, for instance, get an itchy nose, watery eyes, or feel lightheaded when they use a noxious chemical like bleach.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Fumes from recently-painted walls can trigger symptoms for days, and new carpeting can emit high levels of VOC's (sometimes referred to as off-gassing) for weeks or months after installation. One study found that even just working in a newly-constructed building can expose you to enough VOC's to cause eye irritation and airway inflammation.
These symptoms are usually fairly mild and disappear on their own once you get away from the source of VOCs. You usually don't need medical treatment unless you've been exposed to unusually high concentrations or an especially toxic VOC.
Here are some of the most common short-term symptoms that VOCs can cause:
- Eye, nose, throat, and lung irritation
- Coughing and sneezing
- Shortness of breath
- Headaches
- Dizziness
- Minor skin irritation
- Worsened asthma and COPD symptoms
- Nausea or vomiting
Whether or not you realized it at the time, chances are almost certain that you've had minor reactions to VOCs before. For example, if you've ever used a cleaning product that made you sneeze, or felt your eyes stinging near a campfire or BBQ, then you've experienced the symptoms of mild VOC exposure.
This level of exposure is generally not dangerous on its own, especially if it only happens every once in awhile. However, if it happens regularly over the span of several years, it could cause long-term damage your lungs or lead to other health complications.
It's important to note that even a one-time exposure to extremely high levels of VOCs can result in much more serious and long-term symptoms. However, severe VOC exposures are relatively rare and happen most often to people in hazardous occupations that require them to work with or around dangerous VOCs.
Should I be Concerned About VOCs?
If you have a lung or breathing disorder like asthma or COPD, then you probably should be concerned about the amounts of VOCs you get exposed to day-to-day. People with lung conditions are much more vulnerable to the damaging effects of volatile organic compounds for a variety of reasons we'll cover in the next section below.
However, if you are a healthy adult, the answer is not so clear-cut. Researchers are still not sure what kind of impact low-level exposure to VOCs can have, in the long term, on your health.
Research suggests that all the VOCs you encounter as you go about daily life could have a cumulative effect, meaning that even mild exposure over a lifetime could lead to chronic disease. For example, several studies suggest that VOCs from regular activities like cooking and cleaning, if you do them frequently enough, could raise your risk for developing COPD later in life.
Because of this, experts generally recommend that you do your best to limit your exposure to VOCs outdoors and in your home. That could include using low-VOC products, keeping your house well-ventilated, and staying away from sources of second-hand smoke.
In general, exposure to VOC's is most likely to be dangerous if:
- You are exposed to moderate or high levels of harmful VOCs
- You are exposed to low levels of harmful VOCs for a long period of time
- You have asthma, COPD, or another respiratory disease
The most clear and severe cases of adverse effects tend to happen in people who are exposed to above average amounts of VOCs. Studies on a wide range of volatile organic compounds have found that overexposure can increase your risk for cancer, blood disorders, lung conditions, and other serious diseases.
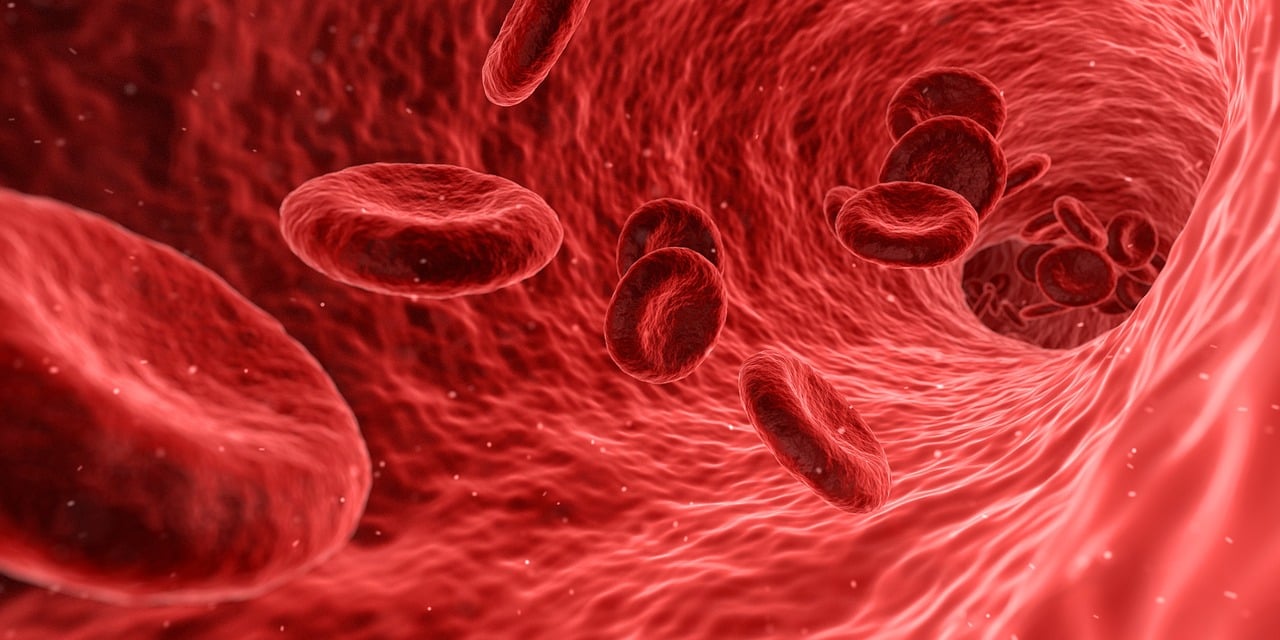
Here are some of the long-term health problems that VOCs can cause:
- Lung damage
- Kidney damage
- Liver damage
- Central nervous system damage
- Blood disorders
- Anemia
- Increased risk for cancers like leukemia (from very heavy or long-term exposures)
Volatile organic compounds are an unavoidable part of daily life, but there are still many things you can do to protect yourself from their harmful effects. For instancde, many hazardous VOCs come from man-made sources that you can avoid and keep out of your home.
How VOCs Affect People with COPD and Other Lung Diseases
Volatile organic compounds that affect your respiratory system tend to have particularly bad effects on people with existing lung diseases, especially asthma and COPD. Because of this, many experts advise people with these health conditions to take special measures to avoid VOCs as much as possible.
Asthma and COPD make your lungs extra sensitive to the quality of the air you breathe. Even temporary exposure to small amounts of respiratory irritants, such as dust, fragrances, and VOCs, can trigger coughing fits, shortness of breath, and other respiratory symptoms.
If you have severe COPD, exposure to VOCs can make your breathing symptoms worse for hours or even days. They can also make you more likely to experience a COPD exacerbation.
If you have high levels of VOCs in your home or workplace, it can make it more difficult to manage your disease in general. You might experience more frequent flare-ups, worse shortness of breath, and an increased risk for lung infections.
Keeping your symptoms under control is a vital part of keeping your lungs healthy, and anything that triggers them on a regular basis can accelerate irreversible lung damage. Because of this, being exposed to harmful VOCs indoors every day can permanently worsen your COPD.
Over the long term, this could have a significant impact on your overall health and quality of life. It can make it more difficult to breathe, more difficult to sleep, and make activities like walking and doing chores around the house more tiring.
Which VOCs Are Bad for Your Lungs?
Now that we've gone over the basics of volatile organic compounds and their risks, let's take a closer look at some specific VOCs that you may be exposed to every day. In this section, we'll introduce you to several of the most common VOCs that are dangerous to breathe so you can better recognize and avoid them in everyday life.
Formaldehyde

You've probably heard of this volatile organic compound before; formaldehyde is an exceptionally common gas that is dangerous to breathe except in very low concentrations.
This VOC originates from a variety of natural and man-made sources. In fact, your body produces a tiny amount of formaldehyde as part of its normal metabolic functions.
However, many commercial products like wood, soaps, and adhesives contain hazardous amounts of formaldehyde. When you use these products in your home, they can emit enough formaldehyde vapor to make the air unhealthy to breathe.
Even very low levels of formaldehyde can cause mild symptoms like eye, nose, and throat irritation. Sensitivity to formaldehyde varies widely from person to person; some (e.g. people with asthma) experience strong allergic reactions when exposed to even a small amount, while others are only bothered by high concentrations of formaldehyde in the air.
The best way to avoid formaldehyde is to replace formaldehyde-containing products with non-toxic alternatives and avoid bringing formaldehyde-treated furniture and wood into your home. If you must, you should air out your house thoroughly and avoid spending time indoors until the bulk of the formaldehyde has had time to dissipate.
Here are some more details about where formaldehyde comes from, what the symptoms of formaldehyde exposure look like, and how it affects your lungs.

Where Formaldehyde Comes From
- Dish soap
- Cosmetics
- Fabric softeners
- Disinfectants
- Permanent-press fabrics
- Leather treatment products
- Treated woods (e.g. plywood)
- Cigarette smoke
- Burning wood and fuel
- Insulation materials
- Carpets
- Other building materials
- Paints and varnishes
- Glues and adhesives
- Paper
Symptoms of Formaldehyde Exposure
- Nose and throat irritation
- Eye irritation
- Skin irritation
- Runny nose
- Difficulty breathing
- Headache
- Nausea
- Lung function decline
- Nose and throat cancers (rarely from long-term or heavy exposures)
How Formaldehyde Affects Your Lungs
Formaldehyde is toxic to the tissue that lines your respiratory tract in relatively low concentrations. According to the Agency for Toxic Substances and Disease Registry, it is not healthy to breathe air with formaldehyde concentrations above .003 ppm (parts per million).
Some of the most common symptoms of exposure to formaldehyde-contaminated air are eye irritation, nose irritation, and airway inflammation. It can cause serious damage to the delicate tissues in your lungs in high enough concentrations, and long-term exposure can cause chronic respiratory symptoms.
Studies show that workers who are overexposed to formaldehyde on the job experience significant lung function decline. Although it is uncommon, occupational exposure can lead to occupational asthma and rare nose and throat cancers.
Formaldehyde is particularly dangerous for people with existing lung diseases, for whom low levels of formaldehyde can trigger breathing difficulties. One study, for instance, found that formaldehyde released by typical laminate flooring was enough to cause severe respiratory symptoms and possibly even cancers in people with asthma and COPD.
Occupations that Put You at Risk of Formaldehydes Exposure
- Manufacturing plastics, resins, and foam insulation
- Hospital or medical work
- Dentistry
- Laboratory workers
- Construction work
- Textile and furniture workers
- Agricultural work (especially livestock farming)
- Morticians who work with embalming fluids
- Beautician work that exposes you to formaldehyde-containing dyes, cosmetics, and other body products
Benzene
Benzene is an abundant volatile organic compound found in many substances you encounter every day. Most people get exposed to benzene by breathing in gasoline fumes (e.g. while filling up your car) or air contaminated by emissions from cars and other fuel-burning devices.
However, certain common household products like paints, carpet, and glues also contain harmful levels of benzene. These products can heavily pollute the air in your home, especially when used for large projects like installing new carpet or painting your walls.
As the case is with many other VOCs, researchers have difficulty estimating exactly how much benzene is safe to breathe. Recent studies suggest that even low-level benzene exposure (e.g. living next to a gas station) can, over time, raise your risk for leukemia and other serious diseases.
For frequent, long-term exposure, benzene levels as low as 1ppm can be dangerous and result in serious blood disorders

If you have chronic obstructive pulmonary disease (COPD), you know that your lung health is directly linked to your systemic health. Just having COPD puts you at a higher risk for respiratory infection, heart disease, high blood pressure, and even mental health conditions like depression and anxiety. But did you know that there’s even a link between your oral health and COPD?
Chances are, you’ve been told from a young age that brushing your teeth will help you prevent cavities and have a nice smile. But this leaves out a lot of details about how your oral hygiene plays a bigger role in your overall health and wellbeing. According to a study funded by the COPD Foundation, people with severe COPD have poor oral hygiene and they also have poor oral health-related quality of life.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’ll discuss some of the reasons COPD patients tend to have poor oral health in comparison to the general population and we’ll also give you some tips for improving your oral health routine in order to live more comfortably with COPD. If you have any questions, please don’t hesitate to leave them in the comment section below so we can get back to you. Alternatively, you can reach out to your doctor for more information about this subject.
How Does COPD Affect Your Oral Health?
When someone is told that two seemingly unrelated organs in the body like the lungs and the teeth or gums are inextricably linked, they’re often surprised. However, the closer you look, the more you’ll realize that they’re related in a number of ways, whether it’s directly or indirectly. The body, as a whole, is a system, so it’s not surprising that something that affects one part will eventually have an effect on the whole.
The Effects of Smoking
The first reason that COPD patients are more likely to have dental health issues is that most COPD patients either currently smoke or were smokers in the past. According to the American Lung Association, around 85 to 90 percent of COPD cases are caused by cigarette smoking and around 38 percent of COPD patients report that they are still smokers. Over the decades, evidence has consistently shown that smoking is incredibly bad for your teeth and gums.

In your mouth, there is a constant battle going on between good bacteria which cleans your teeth and gums, and bad bacteria which leads to tooth decay and gum disease. Smoking negatively affects the quality of your saliva by destroying protective macromolecules, proteins, and enzymes. In other words, the immunological aspect of your saliva is severely hampered the more you smoke.
Smoking also affects your immune system as a whole meaning your body will be less equipped to deal with an infection in your gums or teeth. This study shows that cigarette smoking can have one of two effects on the body. It either exacerbates immune responses leading to chronic inflammation in the body or it attenuates the immune response. Either way, the immune system is less capable of doing its job and warding off infections before they become serious or even life-threatening.
Changes in Your Routine
There’s no doubt about it, being diagnosed with COPD can be life-changing. You might be pressured by your doctor or family to make sudden and drastic changes to your lifestyle, all of which can be daunting and feel like the weight of the world is on your shoulders. More often than not, this causes people to fall back on aspects of their daily routine that they’ve kept up on for many years like practicing good oral hygiene and even making it to the dentist regularly.

Considering the fact that COPD patients visit their doctor more frequently than the general population and many of them are working and maintaining their personal lives and relationships, it can be very difficult to find time to make it to the dentist. And the longer this goes on, the more likely it is that you could develop something like gum disease or periodontitis without even knowing.
COPD Medication
Believe it or not, the medication you take for COPD is another thing that could be causing a decline in your oral health. According to this patient education manual created by the American Thoracic Society, COPD medication can cause dry mouth, a condition where your salivary glands do not produce enough saliva. While this may seem rather harmless, it can actually be quite dangerous if it’s prolonged because saliva plays such a vital role in protecting your teeth and gums.

Inhaled bronchodilators (both short- and long-acting) can cause dry mouth. These medications are used to open up the airways to help you breathe easier and help them clear mucus. Also, inhaled anti-inflammatory medication (corticosteroids) like beclomethasone, budesonide, or fluticasone are known to cause dry mouth. Since these medications are a core part of your treatment plan, it’s best not to completely eliminate them, but to find a workaround for coping with dry mouth instead. This article will give you a good overview of how to deal with dry mouth.
Another potential issue caused by COPD medications is something called oral thrush. This is an infection that occurs in the mouth and throat due to a weakened immune system caused by inhaled medication. Typically, this condition is not serious, but it can cause discomfort while eating and you may need to take antifungal medication in order to get rid of it. Oral thrush is also known to cause or contribute to dry mouth.
How Does Your Oral Health Affect COPD?
Similar to how COPD affects your oral health, there’s also a mountain of evidence suggesting that your oral health can negatively affect your COPD. According to a study published in the Journal of Periodontology, periodontal disease may increase the risk of respiratory infection such as pneumonia in COPD patients. This is a condition that causes the alveoli (tiny air sacs in the lungs) to fill with fluid leading to a chronic cough and breathlessness.
It Can Alter Your Diet
Probably the most likely way that your oral health will affect your lung health is by altering your diet. If you’ve read our articles here at LPT Medical before, you likely know how important your diet is when it comes to reducing chronic pain while preventing breathlessness and fatigue. Most COPD patients should maintain a diet high in protein, healthy fats, and fiber, however, it depends on your individual circumstances.

As we get older, our dental health declines significantly. According to Boston Magazine, people between the ages of 35 and 44 years old have lost at least one tooth. And between the ages of 65 to 74, about 26 percent of people have lost all of their teeth. This is due to a number of causes such as tooth decay, gum disease, periodontal disease, and even traumatic injury. This can impact your diet because it may prevent you from eating certain foods.
-jpg.jpeg)
Unfortunately, foods that are easy to consume and provide us with a lot of energy also tend to be the worst for us. Things like fruit juice, soda, yogurt, and processed foods are convenient, but they’re also laden with sugar and additives that will exacerbate your respiratory symptoms and leave you feeling exhausted and unmotivated. Taking some extra time to cut or break your healthy foods up into smaller pieces may remedy this issue.
It Can Lead to Infections
Most dental infections occur in the tooth, gums, or supporting structures of the teeth. But did you know that dental infections can actually spread to other parts of the body if they aren’t treated? Most COPD patients have a weakened immune system meaning it will be more difficult for your body to fight it off. In certain cases, these infections can be severe and even life-threatening so it’s best to always seek help sooner rather than later. What’s more, dealing with dental issues can be extremely draining and it will take time and energy away from your COPD routine.

Preventing infections is absolutely imperative as a COPD patient. Lung infections are the most likely cause of flare-ups and exacerbations, and they’re also the most likely cause of someone being admitted to the hospital due to COPD. So, whenever you go to brush or floss your teeth, think of it as being beneficial for your full-body wellness rather than just your teeth and gums.
What Can be Done to Improve Your Oral Hygiene?
Brush More Frequently
Possibly the simplest way to improve your oral hygiene is to brush and floss more frequently. With the busy schedules that many people have nowadays, it can be hard to find the time to brush twice a day and floss, but it’s the best thing you can do for your oral health. People tend to skip flossing, but this is the only way to reach the bacteria between your teeth where it can cause the most harm. Be sure to brush your teeth at least twice a day and floss at least once a day.

Drink More Water
Proper hydration not only helps with organ function, but it can also help prevent cavities. When you think about all of the different foods you consume in a day, it’s not hard to see why this is so important. Water removes food from between your teeth, prevents dry mouth, and can dilute acids that stain and eat away at your teeth. Rather than drinking a bunch of water in the morning or right before bed, try drinking water throughout the day, especially during meals. This way, food particles don’t have the opportunity to latch onto your teeth and cause damage.
.jpg)
Schedule Regular Teeth Cleanings
While you can and should take your dental health into your own hands, it’s also important to see a dental specialist regularly. Even if you are careful with your brushing and flossing, any leftover plaque on your teeth when you go to bed at night will turn into something called tartar. This is basically a hardened version of plaque that can only be removed with special tools by your dentist. Another reason to schedule regular teeth cleanings is so that your dentist can make sure your teeth and gums are healthy and that you’re on the right track. Dental issues are almost always easier to fix when they’re detected early on.
Consider Dental Implants
It’s estimated that about 90 percent of people with no teeth use dentures. And while dentures can improve your smile, they don’t provide any benefits when it comes to eating. Dental implants, on the other hand, essentially provide you with a new pair of teeth that are just as effective as natural ones when it comes to chewing. In other words, you’ll be able to keep up with the dietary requirements that your doctor gave you to help you manage COPD. Dental implants can be used to replace just one missing tooth or a whole mouth of missing teeth.
.jpg)
The important thing to remember with dental implants is that your oral hygiene is still incredibly important. While implants can’t decay like your natural teeth can, you will still need to keep your gums healthy in order to prevent gum disease and periodontal disease. When you get dental implants, you will be provided with special cleaning tools and instructions on how to maintain your new teeth. Not everyone is a candidate for dental implants so you’ll need to schedule an appointment with a periodontist to see if they’re right for you.
Conclusion
There is a two-way road between your oral health and your lung health. Years of smoking and the development of COPD can contribute to problems like tooth decay and gum disease. On the other hand, maintaining a poor dental health regime can cause flare-ups in your respiratory symptoms. In other cases, poor dental health and poor respiratory health can contribute to comorbidities like heart disease, poor circulation, and more.
While you have a lot to worry about like making it to doctor’s appointments and pulmonary rehabilitation, it’s always important to make time for your oral health as well. The American Dental Association recommends brushing your teeth at least twice a day with fluoride toothpaste and you should go in for teeth cleanings every six months. And if you have any additional concerns about how COPD could affect your oral health, be sure to speak with your doctor immediately.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Lastly, if you’re a COPD patient looking for a better solution for your oxygen needs than a bulky oxygen tank, take some time to look through our portable oxygen concentrators here at LPT Medical. POCs are electronic oxygen delivery devices so you’ll never have to refill them. They’re also extremely travel-friendly and easy to use. We recommend the Inogen One G5 and Caire FreeStyle Comfort to most patients, but you can learn more about the specifications by reaching out to our respiratory specialists.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!