If you have COPD, then you've probably realized that treating the disease is not a simple process. In order to get it right, your doctor needs to have a very thorough understanding of your physical condition and the nature of your disease.
Because of this, people with COPD have to undergo a large number of medical tests and screenings over the course of COPD treatment. These tests, which include blood screenings, x-rays, spirometry measurements, and more, allow your doctor to tailor your treatment plan specifically to your needs.
Unfortunately, while these tests reveal valuable information about your health and your disease, many patients don't fully understand what their results mean. Even if you have a general idea of what the tests are for, chances are you still wouldn't know how to read and understand the results.
Fortunately, you don't have to be a doctor or a nurse to make some sense out of your medical test results. With a little practice and help, just about everyone is capable of grasping the important aspects of the different tests used to diagnose and monitor COPD.
In this post, we're going to teach you all about these tests—lung function tests, blood tests, chest scans, and more—and show you how to interpret the data in the results. We'll explain what each test is, how it works, and how to figure out what your results actually mean for you and your health.
This is a useful skill that can help you better understand what's going on when you visit your doctor and work with other members of your COPD treatment team. It can also give you the confidence to ask more questions and understand the nuances of treating and monitoring your disease.
Even though the medical jargon can seem complicated at first, it won't seem nearly as intimidating once it's broken down into layman's terms. Once you learn the basics, you'll find it much easier to navigate the medical vocabulary surrounding your disease and treatments.
In the following sections, we'll give you the information you need to start understanding your COPD test results on a deeper level than before. That way, you can take a more active role in your health and treating your COPD.
Getting Your Hands on Your COPD Test Results
Image from Weiss & Paarz www.weisspaarz.com
If you want the opportunity to understand what your COPD tests mean, you need to make sure you have ready access to your results. In some cases, this is as simple as asking your doctor to give you a copy of all your records and reports.
Some healthcare providers, on the other hand, may require you to follow a specific request process in order to get your records. You may need to write a letter, fill out a form, or pay a small fee to cover the cost of making copies and mailing.
Whenever you take a new spirometry test or another type of health screening, make sure to let your doctor know that you'd like to look at the results yourself. Some test results take days or weeks to come
back, but if your doctor knows you're waiting to see them, he can make sure you get access to the records as soon as they're available.
Also keep in mind, that, if you live in the US, you are always entitled to see and review your medical records by law, except in a few rare cases (usually related to mental health records). It is a right under the US Health Insurance Portability Accountability Act (HIPAA), and it states that you must be able to access existing records within 60 days of requesting them.
If you cannot access your medical records or feel that your rights to review your records have been violated, you can file a complaint with the US Department of Health and Human Services. Just make sure you file your complaint with 180 days of your denied request.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Leverage Your Doctor's Experience: Always Listen to the Expert

Whenever possible, you should ask your doctor to go over your COPD test results with you personally, especially if you are unfamiliar with the test or how the data is organized. Even if you know the basics of what you're looking at, your doctor can help you understand the report much better than you could on your own.
You might ask your doctor to go through the report with you line-by-line to help guide you through the information. This gives him the chance to explain important concepts and details that can help you better interpret the results.
This also gives you an opportunity to ask questions and express any concerns you have about the results of your test. If there's anything you are unsure of, don't be afraid to ask your doctor to explain it more clearly.
Understanding Your Lung Function Test Results
There are several different types of lung function tests (also known as pulmonary function tests), and their purpose is to measure how well your lungs are working. They are quick, reliable, and simple to do, which is why they are widely used both to diagnose COPD and to monitor the disease long term.
Lung function tests can tell you whether or not your lungs are damaged and, if they are, give you a better idea of how much damage they have sustained. Doctors use the results to both diagnose COPD and to gauge the severity of the disease.
If you have COPD, then it's important to familiarize yourself with lung function tests—especially spirometry—and how they work. You will take them fairly often over the course of your treatment, likely as part of your regular COPD check-ups.
Taking these tests periodically allows your doctor to track any changes that happen in your lung function over time. This is important, because it allows your doctor to catch and treat problems, like infections, exacerbations, and lung function decline quickly when they occur.
The results of your lung function tests also help your doctor decide what kinds of medications and treatments you need. They also help your doctor determine how well your current treatments are working and evaluate the effectiveness of newly-prescribed medications.
Spirometry
Spirometry is the primary method doctors use to measure lung function and evaluate COPD. It's a relatively simple test that measures changes in your lung volume as you breathe.
By measuring these changes, spirometry can evaluate whether or not your airways are obstructed, and if they are, to what degree. Because of this, spirometry measurements are a reliable way to diagnose COPD and determine how severe the disease is.
Spirometry tests are simple, painless, and relatively quick to complete. If you have COPD, your doctor will probably ask you take a spirometry test at every appointment so that he can look for any changes in your results.
Taking a Spirometry Test
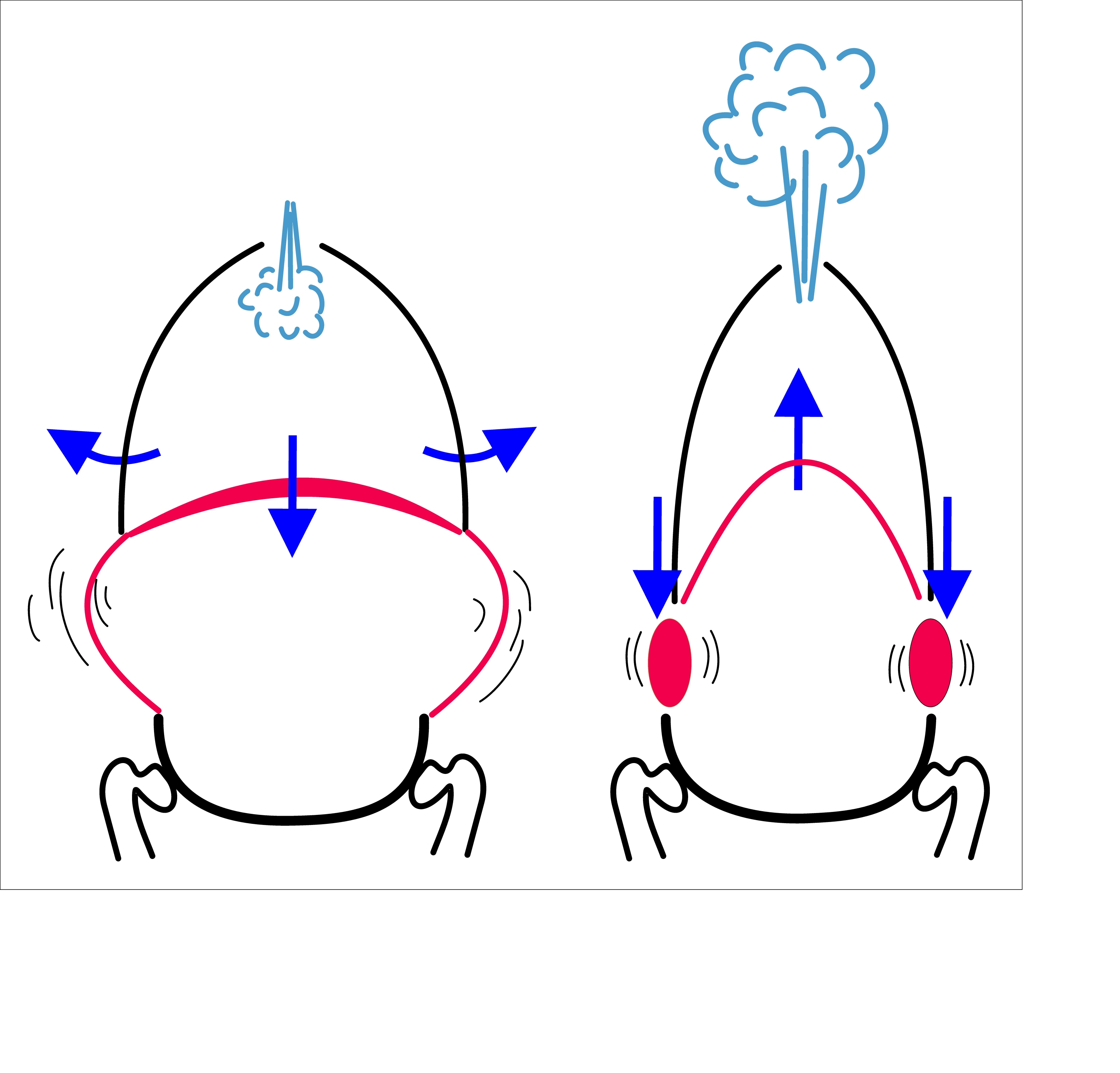
In order to take a spirometry test, you have to breathe out through a mouthpiece attached to a small machine called a spirometer. Your doctor will also put a clip on your nose to pinch your nostrils shut; this is simply to make sure that you only breathe through the mouthpiece during the test.
Then, your doctor will instruct you to take in a deep breath of air (not through the mouthpiece) before exhaling as forcefully and completely as you can into the spirometer's mouthpiece. You will need to do this at least a few times or until your doctor gets a good set of clean results.
The entire process should take less than fifteen minutes to complete. However, you may need to take the test two separate times: once without taking any medication, and once after you've used a bronchodilator inhaler, with a short pause in-between.
This is known as a bronchodilator reversibility test because it tells you how much the bronchodilator medication is able to improve your airway obstruction. This tells your doctor how well you respond to the medication and helps him determine the best course of treatment.
Spirometry Test Measurements

There are three main measurements that your doctor will measure in a typical spirometry test:
- FVC: Forced Vital Capacity
- FEV1: Forced Expiratory Volume (in one second)
- FEV1/FVC: this is a ratio comparing your forced expiratory volume (FEV) to your forced vital capacity (FVC)
Spirometry tests take other measurements as well, including forced expiratory flow (FEF), peak expiratory flow rate (PEFR), and maximal voluntary ventilation (MVV). However, we're not going to discuss these in any detail here because FVC, FEV1, and FEV1/FVC are usually the most important spirometry results to look at when it comes to diagnosing and monitoring COPD.
FVC: Your forced vital capacity (FVC) essentially tells you how much air you can push out of your lungs in one breath. More specifically, it is a measure of how much air (in volume) that you can exhale forcefully and quickly from your lungs after taking in as deep a breath as you can.
FEV1: Your FEV1 tells you how much air you can exhale from your lungs in exactly one second after taking a deep breath. Basically, FVC tells you the volume of air you push out during one full exhale, while FEV1 tells you the volume of air you can push out during the first second of that full exhale.
FEV1/FVC: When you divide your FEV1 by your FVC, you get another important number, which is simply referred to as your FEV1/FVC. This tells you what percentage of the air you exhaled from your lungs was pushed out during the first second of your exhale.
For example, an FEV1/FVC of 90% means that you pushed out 90% of the air during the first second of your exhale, and the remaining 10% of the air after that first second. If your FEV1/FVC percentage is too low, it is a sign that something is preventing you from pushing the air out of your lungs as quickly as you should.
If your FEV1 or FVC results are abnormal, this FEV1/FVC ratio helps your doctor determine whether or not the abnormality is caused by an obstruction (e.g. COPD) or a restrictive lung disease (in which FEV1 and FVC should change at a similar rate). If you have an FEV1/FVC of 80% or less, it is a strong sign that you have an obstructive lung disease.
Interpreting Spirometry Results
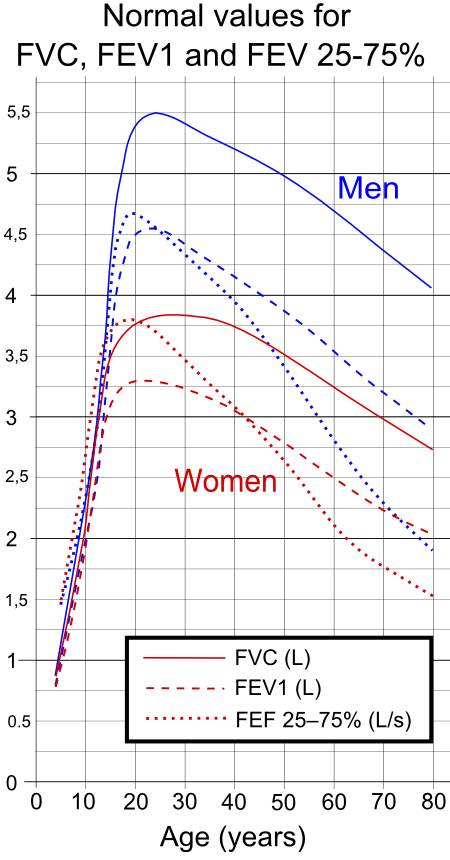
In order to make sense of your spirometry test results, you need to compare them against a standard table of healthy FEV1 and FEV1/FVC values. This will tell you how much your numbers differ from numbers collected from healthy adults of your age, weight, and height.
Then, in order to truly understand what these numbers mean, you will need to refer to another table, known as the GOLD spirometric criteria for COPD severity. This table presents four different ranges of FEV1 and FEV1/FEC results and tells you what it means if your numbers fall within that range.
The GOLD guidelines are the most commonly used and widely accepted criteria for diagnosing COPD. Finding out where your results fall within these four GOLD categories will tell you what stage of the disease you have and give you a better idea of how severe your COPD is.
Here's a quick look at the GOLD guidelines and what they can tell you about your health.
GOLD Spirometric Criteria for COPD Severity
- Stage I: Mild COPD
- FEV1/FEC less than 0.7
- FEV1 greater than or equal to 80%
- Stage II: Moderate COPD
- FEV1/FEC less than 0.7
- FEV1 between 50% and 80%
- Stage III: Severe COPD
- FEC1/FEC less than 0.7
- FEV1 between 30% and 50%
- Stage IV: Very Severe COPD
- FEV1/FEC less than 0.7
- FEV1 less than 30% or less than 50% plus chronic respiratory failure
While it's important to read and understand your spirometry test results yourself, remember that only your doctor has the training and expertise to accurately interpret the results. A licensed doctor is the only one qualified to diagnose COPD or make the call on what stage of the disease you have.
Lung Plethysmography

Lung plethysmography (pronounced ple-thiz-mah-graf-ey) is a test that measures your lung capacity, or how much air your lungs can hold at one time. It can also tell you how much air is left in your lungs after you exhale.
Your lung capacity is closely related to your general lung function, which is why plethysmography is often used to evaluate and monitor COPD. In particular, plethysmography helps your doctor determine whether or not your airways are obstructed, and how much they are obstructed, by measuring how you breathe.
This is especially useful for diagnosing unknown breathing problems, because it can confirm or rule out airway obstruction as a cause. This helps doctors determine whether someone has COPD or different type of breathing disorder.
Lung plethysmography also allows your doctor determine whether or not your lungs trap air and how severe the problem is. It does this by measuring exactly how much air is left in your lungs after you exhale.
This is important, because trapped air is a very common problem for people with COPD, and it can significantly worsen respiratory symptoms. Trapped air makes it difficult to breathe, worsens shortness of breath, and can actually stretch out your lung tissue (causing hyperinflation) over time.
Taking a Lung Plethysmography Test
 |
| Photo by Airman 1st Class Teresa Cleveland |
Taking a lung plethysmography test is simple and usually only takes about fifteen minutes to complete. All you have to do is sit in an enclosed, transparent chamber (about the size of a phone booth) and breathe in and out through a special mouthpiece attached to a spirometer machine.
During the test, your doctor will instruct you to breathe in specific ways so that the machine can measure a wide range of breathing patterns. You will alternate between normal breathing, fast breathing, shallow breathing, deep breathing, and any other breathing patterns your doctor wants to test.
If you normally use oxygen, you will most likely be instructed not to use it during the test. You may also stop the test and leave the chamber at any time if you feel too uncomfortable or claustrophobic, though this may require you start the test again from the beginning.
Interpreting Your Lung Plethysmography Results

Throughout the test, the machine attached to your mouthpiece carefully measures the airflow in and out of your lungs. The results provide your doctor with a few very important pieces of information about your lungs and how you breathe.
Specifically, there are three main things the test can tell you about your lungs:
- Total Lung Capacity (TLC): the amount of air in your lungs after you breathe in as deeply and fully as you can
- Functional Residual Volume (FRV): the amount of air that is left in your lungs after exhaling as fully and completely as you can
- Functional Residual Capacity (FRC): this is a measure that compares the amount of air left in your lungs after a normal exhale to the amount of air left in your lungs after you exhale as fully and completely as you can
To understand what these results mean, you will have to compare the numbers from your results to the numbers that are considered healthy for your age, sex, height, and weight. If your results are equal to the healthy standard, then that indicates that your results are normal. If your numbers are significantly higher or lower, however, that indicates abnormal lung function.
You can use the information in the following sections as a basic guide to help you understand how to interpret your plethysmography results when comparing them to the healthy standard:
Total Lung Capacity (TLC)
Increased TLC: If your total lung capacity is higher than normal, this can be a sign of a lung disease like emphysema. It means that your lungs can hold more air than the average person, which is often caused by obstructive lung diseases and especially lung hyperinflation.
Decreased TLC: It is a bad sign if your total lung capacity is lower than normal because it indicates that your lungs are not able to expand or fill up as much as they should. This is often caused by restrictive lung diseases like pulmonary fibrosis, which are different from obstructive lung diseases like COPD.
Functional Residual Volume (FRV)
Increased FRV: If your functional residual volume is higher than the healthy standard, it is a bad sign because it means that there is too much air left in your lungs even after you exhale completely. This is a sign that your lungs have lost elasticity and/or are hyper-inflated, which is common in people with COPD and especially emphysema.
Functional Residual Capacity (FRC)
Increased FRC: It is a bad sign if your FRC numbers are higher than the healthy standard because it indicates that air stays trapped in your lungs after you exhale. The higher the number, the more severe the problem is.
This indicates that you suffer from an obstructive lung condition, and is very common in people with COPD.
Decreased FRC: It is also a bad sign if your FRC numbers are lower than the healthy standard, because it means that your lungs are not filling up as much as they should. This indicates that the amount of available airspace in your lungs is reduced, which is often caused by narrowed airways and/or loss of elasticity in the lungs.
Decreased FRC is common in people with pulmonary fibrosis, sarcoidosis, obesity, and in people who have had lung reduction surgeries or strokes.
Lung Diffusion Tests
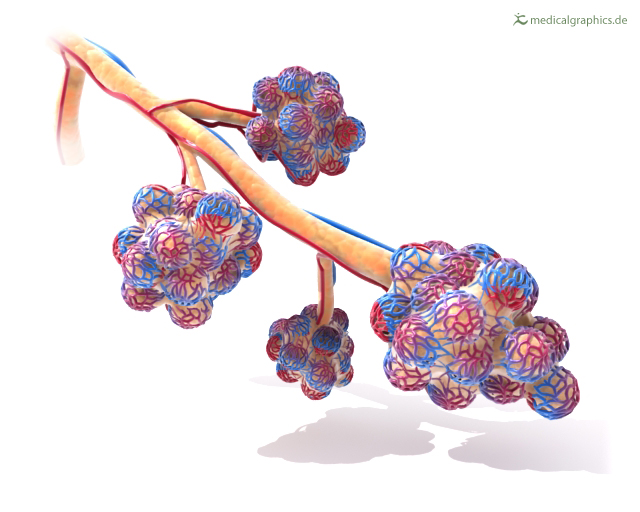 |
| Image from Medical Graphics |
Whereas spirometry tests measure your lungs' overall strength, lung diffusion tests (also known as gas diffusion studies) specifically measure gas exchange, or how well your lungs can transfer gasses to and from your bloodstream. That is the lungs' primary purpose, after all: to absorb oxygen into your blood and remove carbon dioxide from it.
Your lungs do this via millions of tiny air sacs, called alveoli, which fill up with air when you breathe in. These alveoli are covered in tiny blood vessels with walls thin enough that gasses (oxygen and carbon dioxide) can passively move, or diffuse, in and out of the blood.
However, if these air sacs become damaged, then gasses cannot diffuse through them as easily, if at all. This type of lung damage is permanent and it is one of the defining characteristics of emphysema, one of the two main types of COPD.
In people with COPD, this lung damage continues to get worse and spread as the disease progresses. As more and more alveoli become damaged, less oxygen can diffuse into your bloodstream and less carbon dioxide can diffuse out.
That's why doctors perform diffusion tests on people with COPD and other lung disorders. By measuring how well gasses can diffuse through the alveoli in your lungs, diffusion tests help your doctor determine the nature and extent of any lung damage you have.
Taking a Lung Diffusion Test

Diffusion tests work like this: first, you breathe in a specially-formulated gas mixture through a mouthpiece and tube attached to a spirometer machine. This gas mixture is harmless and contains a specific amount of a “tracer gas,” usually carbon monoxide, which your lungs will process after you breathe it in.
Next, you hold your breath for about ten seconds in order to give the gas time to diffuse through your alveoli and get absorbed into your bloodstream. Then, you breathe out through the mouthpiece, which will deliver the exhaled air to the spirometer machine for analysis.
The machine then measures precisely how much carbon monoxide is in the air you exhaled. The more carbon monoxide left in the air, the less your lungs were able to absorb.
Essentially, healthier lungs will exhale less carbon monoxide, while damaged lungs will exhale more. The results of the test represent your lungs' diffu

