In this day and age, everything seems to be getting smaller. Our phones are getting smaller, laptops are getting smaller, and even our cars are getting smaller. It feels great to invest in a product that’s both small and powerful because it allows us to have more freedom and control in the palm of our hands.
When it comes to investing in smaller and smaller products, however, it’s more important than ever that we’re aware of the potential problems of downsizing. For example, a small car may be able to zip around corners and save you a lot of money on gas, but is it able to provide you with the safety that you want and need?
This is no different when it comes to portable oxygen concentrators. Introduced in the early 2000s, these new medical oxygen devices offered an alternative to the clunky and dangerous oxygen tanks that came before them. Manufacturers wanted to push the limits of what was possible, so they’ve been making portable oxygen concentrators smaller and smaller ever since then — but this has often been at the expense of the consumer.
There’s a lot more that goes into a great portable oxygen concentrator than size; oxygen output, weight, reliability, battery life, and ease-of-use are also very important factors to consider. As such, if you want to find the best POC for you, it’s important to take all of these into consideration. Having a small portable oxygen unit is great, but only if it excels in other ways as well.
In this blog, we’ll take a look at two of the smallest portable oxygen concentrators on the market: the Inogen One G5 and the Respironics SimplyGo Mini to help you determine which one is right for you. If you have any questions, please leave them in the comment section below or address them with a respiratory specialist.
Respironics SimplyGo Mini Overview
Respironics is a world leader in respiratory and sleep products. Founded in 1976 by Gerald E. McGinnis, the company mainly focused on sleep apnea products like CPAP machines but later branched out to include bi-level technology in 1992 and eventually portable oxygen concentrators in the 2000s.
Respironics boasts two portable oxygen concentrators: the Respironics SimplyGo (continuous flow) and the Respironics SimplyGo Mini (pulse flow). Each unit has its pros and cons, but each one claims to be one of the lightest and most efficient POCs in its class while still offering the quality and reliability you’d expect from a Respironics product.

One unique aspect of this Philips oxygen concentrator is the touch screen display. Where most concentrators have physical buttons you can press, the SimplyGo Mini only has a “power” button and a “home” button. The rest of the unit’s functions are controlled by the touch screen. If you’ve never used a touch screen, however, don’t be intimidated. The SimplyGo mini has on-screen cues that will help you navigate its features quickly and effectively.
Inogen One G5 Overview
Inogen is widely considered to be the best portable oxygen concentrator manufacturer in the world. It was founded in the early 2000s with the conviction that technology in the medical oxygen field was not keeping up with the desires of COPD patients and that medical professions needed to try something new.
Inogen began work on their Inogen One G series of portable oxygen concentrators which aimed to provide oxygen patients with significantly more freedom than their oxygen tanks. Since then, we have seen five generations of Inogen oxygen machines along with other high quality products such as the Inogen at Home Oxygen Concentrator, as well as a host of accessories like backpacks, carrying cases, external battery chargers and more which help patients get the most out of their machines.
.png)
The Inogen One G5 portable oxygen concentrator is the latest POC by Inogen, offering an extended battery life and higher oxygen output than previous iterations. Having been released this past summer, it’s a relatively new unit, but that hasn’t stopped it from quickly becoming one of the most beloved POCs on the market, especially since it has such a reputable brand to back it up.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Oxygen Output
Oftentimes, one of the best places to start when comparing two oxygen concentrators is their oxygen output. After all, it’s very difficult to start examining other features of a medical oxygen device if it doesn’t provide you with the level of oxygen that you need.
Both the Inogen One G5 and the Respironics SimplyGo Mini are pulse flow units. What this means is that they have built-in technology that only delivers oxygen when you inhale. This enables manufacturers to make much smaller lightweight units, but they may not be ideal for patients with high-flow oxygen therapy needs.
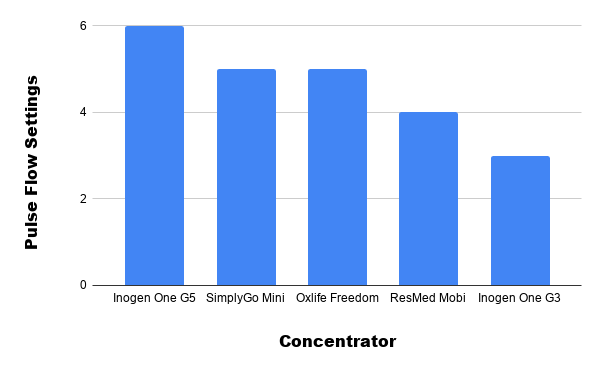
What’s more, the Respironics SimplyGo Mini Offers a flow setting of 5 while the Inogen One G5 offers a flow setting of 6, the highest option available for a pulse flow unit. No other pulse flow oxygen concentrator on the market can go up to a flow setting of 6. If you want to go any higher, you’ll need to switch over to continuous flow machines which are much heavier and bulkier.
This is not to say that the SimplyGo Mini is bad in terms of oxygen output. A setting of 5 is good when compared to most pulse flow oxygen concentrators. If you typically stay at a setting of 2 or 3 and your doctor tells you that a setting of 5 is enough, then the SimplyGo Mini may be a great option for you.
Battery Life
Another one of the most sought-after features of a portable oxygen concentrator is its battery life. A long battery life is what enables oxygen users to go where they want, when they want, and stay out for longer without having to get to a wall outlet to charge their device.
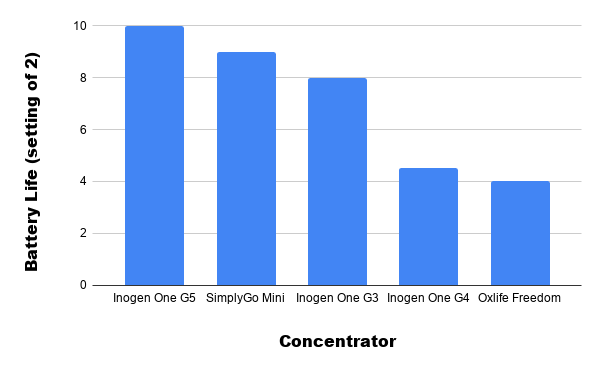
When someone brings up battery life in portable oxygen concentrators, they’re often compared to oxygen tanks. The average portable E cylinder will work for about 5 hours before it runs out of oxygen. An even smaller tank, the D cylinder, will go for about 3 hours before running out. Fortunately, both the G5 and the SimplyGo Mini offer much more freedom than that.

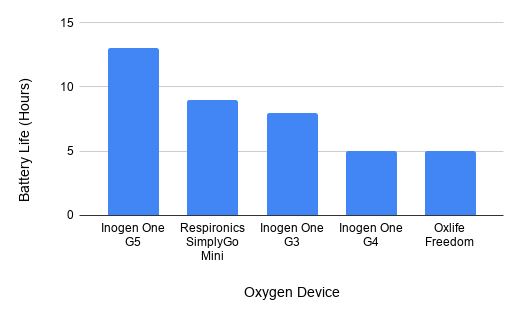
On a flow setting of one, the Inogen One G5 can attain an outstanding 13 hours of battery life on one charge using the double battery pack. The SimplyGo Mini is not far behind with a maximum battery life of 9 hours on a setting of two using the extended battery pack. Either way, this leaves you tons of breathing room (no pun intended) while you’re out and about to do as you please without having to go back home to charge your battery.
If 13 hours of battery life isn’t enough or you need to use a higher setting which drains more battery life, you can always carry an extra battery on you. The double battery only weighs a pound more than the single battery, so you won’t have any trouble carrying an extra one in your G5 backpack or carrying bag. Likewise, with the SimplyGo Mini, you’ll also have the option of carrying an extra battery or extended battery.
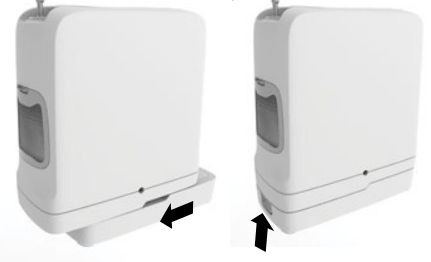
Ease-of-Use
The Inogen One G5 and SimplyGo Mini both have a lot to offer in terms of ease-of-use. Just so we’re clear on what this means, ease-of-use refers to how easily settings can be changed or adjustments can be made to your concentrator on the fly. It’s important to have an oxygen concentrator that’s easy to use so that you don’t waste time fiddling with it while you’re away from home.

Both these pulse flow portable oxygen concentrators have a simple interface. The screen and the controls are built into the top of the unit so you won’t have to lift the device up or strain yourself to make changes to it. The G5 display shows your remaining battery life, flow setting, audible alerts, and errors. The SimplyGo Mini, on the other hand, is almost entirely touch screen. You’ll be able to make pulse flow setting adjustments without ever using any buttons.
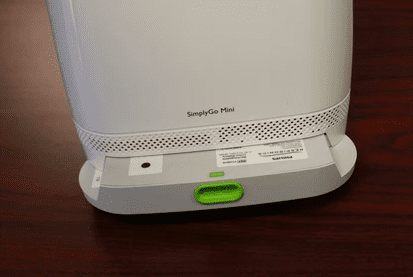
Another factor that contributes to ease-of-use is the battery pack. On both the Inogen One G5 and SimplyGo Mini, you’ll be happy to know that the batter can be slipped on and off easily by simply pulling the tab on the front of the case. The G5 battery will slide off the back of the unit and the SimplyGo Mini battery will slide sideways off the device.
If you decide to purchase a G5, you’ll need to remove your filters and wash them every couple of weeks to a month. Fortunately, this is really easy to do. Simply remove the intake vent filters from the front and back of the unit, clean it using a mild dish soap, and make sure it is thoroughly rinsed and dried before putting it back on the device. It’s imperative that you do not run the concentrator without the filters because it prevents air particles from damaging internal components and ensures that you’re always breathing clean air.
There are plenty of great accessories available for both devices as well that can contribute to how easy they are to use. For example, you can purchase either the G5 custom carrying case or G5 backpack which gives you ample ways to carry your Inogen G5. For the SimplyGo Mini, you may opt for accessories like the external battery charger or the carrying cart.

Size
Size can really be a deal breaker when you’re choosing an oxygen concentrator. If your device is too large, you’re going to have a lot of problems traveling with it especially if you need to get on a plane or a bus. While bulkier oxygen concentrators like the SeQual Equinox are approved by the Federal Aviation Administration (FAA) and most cruise lines, that doesn’t mean you’ll have a pleasant experience while you’re traveling with them.
On the other hand, pulse flow units like the Inogen One G5 and the SImplyGo Mini are small enough that you won’t have any problems traveling with them or finding a place to store them on a plane or bus. The Inogen One G5 is 8.15" H x 7.19" L x 3.26" W and the SimplyGo Mini is 9.4” H x 8.3” L x 3.6” W so the G5 is slightly smaller but not by a huge margin.

If you travel by air a lot, there’s no understating how convenient it is to have a small portable oxygen concentrator. The aisles on most airplanes are really narrow, so if your oxygen concentrator isn’t able to fit between them, you may have to pick it up or have someone else carry it for you. You’re supposed to put your belongings under a seat when you take off but if your concentrator is too bulky, you may have to hold it in your lap, which can be a safety hazard.
Let’s face it, we all have to go to the bathroom at least once when we’re on a flight. Airplane bathrooms are tiny enough as it is, but if you have an oxygen concentrator with you, it can feel nigh impossible. At less than a foot in width and height, however, the G5 and SimplyGo Mini won’t add any unnecessary bulk and you won’t have to worry about bumping other passengers on the way to the bathroom either.
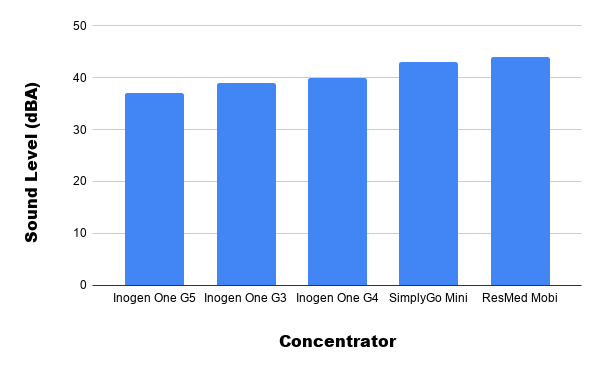
Sound Level
Noise is often a factor that many oxygen users are concerned about when purchasing a portable oxygen concentrator for the first time. They don’t want to disturb people or get kicked out of a library or wherever they’re going. While this is certainly an understandable concern, even the loudest portable oxygen concentrators are pretty quiet.
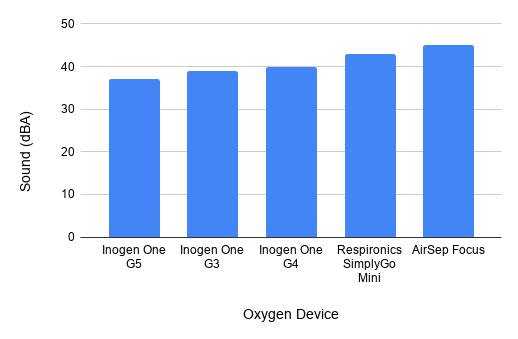
The Inogen One G5 is only 37 decibels (dBA) on a setting of 2 and the SImplyGo Mini is only 43 decibels on a setting of 2. That’s about the volume of a quiet whisper or gentle hum sound. Most people report getting used to the sound after a few times of using it and that it doesn’t disrupt other people when they’re around it. A difference of 6 decibels may sound like a lot, but when you hear the two devices side-by-side, you probably wouldn’t even know the difference.
The Ideal Candidate for the SimplyGo Mini
The SimplyGo Mini portable Oxygen Concentrator is one of the most popular units on the market and it’s backed by a company that’s been a leader in sleep and respiratory health for decades. Philips Respironics is known for producing medical oxygen equipment that’s durable, reliable, and powerful.
If you’re considering the Respironics SimplyGo Mini, it’s unlikely you’ll be let down. This medical oxygen device excels in nearly every aspect of its design like weight, size, battery life, and ease-of-use. The one thing to note, however, is that it goes up to a maximum flow setting of 5, as opposed to a flow setting of 6 like the Inogen One G5. So, you’ll need to speak with your pulmonologist beforehand to make sure this won’t be a problem.
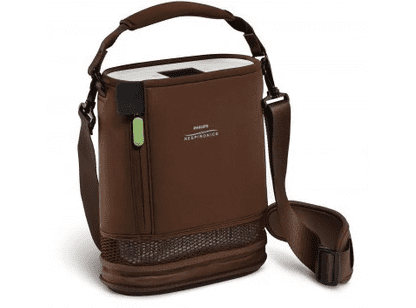
When compared to the G5, the SimplyGo Mini lacks in most areas. However, the differences are minimal in many cases, and depending on what your needs are, you may find that the SimplyGo fulfills your needs perfectly. Cost is another aspect to consider when purchasing a portable oxygen concentrator and there are so many deals going around that it’s impossible to say which unit will be cheaper at any given time.
The ideal Candidate for the Inogen One G5
Inogen is unlike Respironics in that it was created with the sole purpose of making medical oxygen more accessible and convenient for respiratory patients. Inogen broke barriers with their G1 oxygen concentrator back in the early 2000s and they continue to break barriers with their latest portable oxygen concentrator, the Inogen One G5.
The G5 broke records for the most external battery life of any POC as well as having the highest oxygen output of any pulse flow POC. This is a deal breaker for many oxygen patients because if they need a device with a flow setting of 6, they no longer need to switch over to a heavier, bulkier continuous flow unit. The added battery life affords oxygen patients the freedom to stay out of their house for longer and have more peace of mind while traveling.

All in all, the Inogen One G5 is the best portable oxygen concentrator for the greatest number of people. The G5 was released this past summer so it’s one of the newest POCs available, meaning replacement parts are widely available and technical support is in full force. However, it’s unlikely you’ll need either of these for some time because the G5 has had a very low failure rate right out the gate.
Conclusion
Ultimately, you can’t go wrong with either the Inogen One G5 or the Respironics SimplyGo Mini. Both oxygen machines are backed by reputable medical oxygen companies that have proven their commitment to customers for decades. Both units are fully supported with replacement parts and technical support so you won’t have to worry about your device breaking a year or two down the line.
While it’s great to have a preference in which POC you want, you should first consider your medical needs. Before purchasing a portable oxygen concentrator, speak with your doctor and pulmonologist to learn exactly what your oxygen needs are. This way you can invest in a unit that offers you plenty of breathing room in case your disease progresses or you experience an exacerbation.
.png)
The Inogen One G5 was released back in the summer of 2019 with praise from oxygen retailers and respiratory patients alike. Offering significant improvements in battery life and oxygen output over the Inogen One G3 and Inogen One G4, the G5 was more than capable of holding its own in a market that’s already saturated with plenty of reliable and efficient oxygen machines.
Possibly the most notable achievement of the Inogen One G5 is its battery life. As opposed to previous portable oxygen concentrators, the G5 afforded oxygen patients ample usage time with up to 13 hours of battery life on a flow setting of 1 and up to 3 hours on its highest setting (a setting of 6). This means that even patients with the highest oxygen demands can stay out and about for longer than ever before.
By excelling in all aspects of design like weight, size, battery life, cost, oxygen output, and reliability, the G5 set a new precedent for oxygen concentrator manufacturers. No longer would oxygen patients have to “settle” for below-average battery life or sacrifice their personal freedom and independence just to get the oxygen they need — the Inogen One G5 does it all.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
While you’ve probably already read a lot about the G5 itself, you may be wondering what accessories are available for it. G5 accessories are by no means necessary for you to experience the benefits of this oxygen machine, but they certainly help if you want to make the most of it. Read on as we take a look at 7 must-have accessories for your Inogen One G5 portable oxygen concentrator and be sure to leave a comment if you have any questions.
The Inogen One G5 Custom Carrying Case
The most fundamental Inogen One G5 accessory is the custom carrying case. This simple accessory provides G5 owners with the easiest and most effective way to carry their portable oxygen concentrator whether they’re simply taking a trip to the store or going on a long vacation around the world.

The custom carrying case is designed for the minimalist. Rather than offering tons of extra storage pockets, it has just enough room to carry small objects like a driver’s license, a grocery list, or your Inogen One G5 manual. But most importantly, it keeps your concentrator at your side as you go about your daily life. It also has the ability to carry a G5 with either the single or double battery attached.
Prevents Scratches and Dents
If you’re not already aware, the Inogen One G5 doesn’t have any place to clip a shoulder strap onto. As a result, you’ll need to have a case to carry it in like the G5 custom carrying case. Fortunately, this case provides ample protection so you’ll never have to worry about scratches, dents, or cracks.
Although the G5 is already a solid unit that resists damage with its hard outer shell, like any electronic device, it’s still susceptible to internal damage. The custom case is padded enough to prevent minor damage but thin enough that it won’t add a significant amount of bulk to the unit. You’ll be able to carry your oxygen unit wherever you please, even in busy or overcrowded areas, and still have the peace of mind knowing that your concentrator is safe.

Easy to Use
The G5 custom carrying case makes it incredibly easy to transport your POC. If you’re worried that you won’t be able to use your concentrator as easily, think again! When you slip the G5 into the carrying case, simply lift the flap on the top to access the control panel. There’s an open area in the back so that you can plug in an AC or DC power adapter. What’s more, to change batteries, all you need to do is unzip the bottom of the bag. Another reason the G5 carrying case is easy to use is that you can adjust the carrying strap to your liking. The strap has an adjustable pad on it so you’ll never feel uncomfortable while carrying your POC.
The Inogen One G5 Backpack
The G5 backpack is the opposite of the custom carrying case in many ways. While the custom carrying case opts for a minimalist approach, the backpack is designed for those who want to carry a lot of personal belongings with them. The obvious downside to this is that you’ll need to take the backpack off to check your battery life, oxygen purity status, and alerts, however, the control panel can be easily accessed without even having to remove it from the backpack. Note that the Inogen One G5 backpack can hold both G5s with single batteries and G5s with double batteries.

Perfect for Traveling
If you’re someone who loves to travel and explore the world, the G5 backpack has a lot to offer you. While it’s certainly important to travel light on long trips, you also need to make sure that what you do take is stored in the most efficient way possible. On the G5 backpack, you’ll find a large storage compartment for personal belongings and a pouch on the back of the bag allowing you to keep everything separate.
Your Inogen One G5 will fit snugly into the pouch meaning it won’t jostle around or fall out. The top of the POC is only partially covered, so you’ll still be able to check the screen, use the buttons, and plug in your cannula while it’s in the pouch. There is also a mesh material where the air intake is so that you ensure it’s always operating how it should be.

Comfortable to Wear
Let’s face it, if you’re traveling around the world and doing a lot of walking, the last thing you want is an uncomfortable backpack. Fortunately, the G5 backpack delivers in this category. Like the custom carrying case, the G5 backpack has adjustable shoulder straps to help you find the right fit. They’re also padded so they won’t dig into your shoulders.
Another reason the G5 backpack is so comfortable is that the G5 won’t hang down or move around as you walk. Naturally, the farther something protrudes out from a backpack, the more strain it will cause on your back. However, with this backpack, the G5 is held close to the main storage compartment so there won’t be any unnecessary strain on your back and shoulders.
The Inogen One G5 Single Battery
The single battery is the same one that comes with your Inogen One G5 portable oxygen concentrator. However, if you’re in need of more battery life on the go, an extra one may be just the thing you’re looking for. It’s called a “single battery” because it has just one cell in it. This cell has one anode and cathode which is separated by electrolyte, used to produce both a voltage and a current.
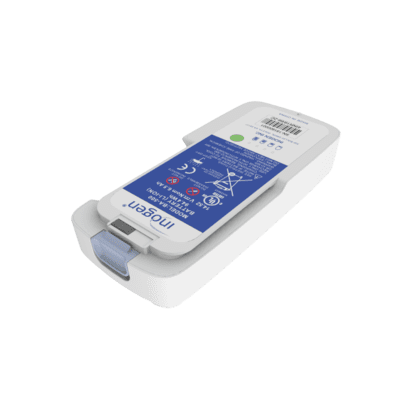
Lightweight Design
The Inogen One G5 is only 4.7 pounds with a single battery attached to it and a single battery by itself only weighs about 8 ounces. So even when you’re carrying an extra single battery with you, it will still weigh less than most portable oxygen concentrators on the market. Inogen has spent several decades refining the technology in their batteries allowing oxygen patients to have a longer battery life in a smaller and more lightweight battery. The single battery offers up to 6.5 hours of life on a flow setting of 1.
Easy to Replace
If you’re looking for extra batteries for your G5, chances are, you’re on the go often. If that’s the case, you’ll be happy to know that Inogen G5 batteries are extremely easy to remove and replace. Simply press the release tab that’s on the side of your G5. The battery will pop off of the unit and you can then put the new battery in its place. Make sure you push upwards so that it clicks into place and it’s secure while you’re going about your daily business.
The Inogen One G5 Double Battery
Some people get confused when they hear “G5 double battery” because they think it comes with two separate batteries, however, the word “double” is referring to the number of cells in its casing. In this case, the double battery provides twice as much battery life as the single battery. If you’re going on a long vacation or you’re planning on being away from home for a while, there’s no understating the importance of having a G5 double battery with you.

Ample Battery Life
The G5 double battery pack is equipped with up to 13 hours of battery life on a flow setting of 1. This is the longest external battery life of any portable oxygen concentrator on the market and offers an ample amount of freedom for you to be out and about as long as you please without having to replace your battery or find an outlet to charge your device.
If that’s not enough, you’ll be happy to know that the double battery isn’t a whole lot bigger than the single battery and it’s still very lightweight. The double battery weighs in at just 12 ounces, only 4 ounces more than the G5 single battery. In other words, you’re getting twice the battery life with a 50% increase in weight. This makes the double battery the most efficient battery option for the Inogen One G5.
Plenty of Options to Fit Your Lifestyle
The main takeaway when it comes to Inogen One G5 batteries is that they offer plenty of options to fit your lifestyle whether you’re super active and want to get out as much as possible, or you just need to get to the store once a week.

The Inogen One G5 comes with a single battery attached to it. This means you’ll get up to 6.5 hours of battery life right out of the box. If you want to extend that battery life, however, you can purchase either an extra single battery or an extra double battery. Two single batteries would provide you with up to 13 hours of battery life and a single and double battery would provide you with an astounding 19.5 hours of battery life! What’s more, you’d only be carrying 5.75 pounds of weight in total, that’s still less than other pulse flow portable oxygen concentrators like the Oxlife Freedom and the AirSep Freestyle 5.
The Inogen One G5 DC Power Cable
One thing we get very excited to tell oxygen patients about is the Inogen One G5 DC power supply. Why do we like this accessory so much? Because it adds to the many ways the G5 offers you freedom and independence throughout your daily life. Nobody wants to live in a world where they have to count down the hours of freedom they have the moment they live their home in the morning, it’s more reassuring to know that you’ll have access to oxygen wherever you go and the DC power supply offers this.

Perfect for Road Trips
We’ve already talked a lot about flying and taking a cruise with the Inogen One G5, but what about taking a road trip? The G5 DC charging cable allows you to charge your G5 in any vehicle with a cigarette outlet, so you’ll be able to keep your concentrator fully charged during your whole trip.
If you need to get out and do some sightseeing or to stretch your legs, you’ll have peace of mind knowing that you have a fully charged battery to work with. Once you get to the hotel or wherever you’re staying, you’ll be able to charge your G5 with the AC adapter as well via a wall outlet.
The Inogen One G5 External Battery Charger
One of the lesser-known and potentially underrated accessories for the Inogen One G5 is the external battery charger. Typically, in order to charge your G5 batteries, either through AC or DC power supply, you need to have the battery attached to your device. So, if you like to carry more than one battery on you, this accessory will enable you to charge two batteries at once.

Less Downtime
Life can be unpredictable sometimes. One minute, you could be sitting on the couch watching TV and the next you could be rushing out the door to meet with a friend or loved one. While we can’t always predict everything that we’ll do today, tomorrow, or next week, we can do our best to prepare for it.
By being able to charge two batteries at once, the G5 external battery charger will allow you to be prepared no matter what curveballs life throws at you. If you need to jump up and leave the house at a moment’s notice, you’ll have two full batteries to keep you going as opposed to just one.
Convenient and Easy to Use
The G5 external battery charger is very easy to use and can easily be packed with your extra batteries and charging cables when you’re away from home. Weighing in at just 0.85 pounds and about the size of a hockey puck, the external battery charger can easily be placed on a desk or table to charge and can be placed in your G5 backpack or a purse for safekeeping.
This accessory is very easy to use. Simply plug the AC adapter into the wall and into the external battery charger. Take either your G5 single battery or G5 double battery and plug it into the bottom of the external charger. You’ll see a light indicating that the battery is being charged. And once it’s fully charged, the “100%” symbol will illuminate to show you that your battery is fully charged. That’s it! Now you can simply detach the battery and use it on your G5. Remember to use the AC power cable you already own to charge another battery on the G5. That way, you’ll have no downtime.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Backup Oxygen Tubing/Cannulas
Last but certainly not least, it’s a good idea to have some extra cannulas lying around in case you need to replace them. Cannulas are the clear tubes that you attach to the G5 and place in your nose in order to inhale oxygen. Many people don’t know that cannulas come in many different shapes, sizes, and designs, so it’s important to find ones that work best for you and allow you to be comfortable throughout the day.
-min.jpg)
Cannula Quality
Quality is the most important factor to consider when choosing a nasal cannula or oxygen supply tubing. As you’re moving around and going about your day, low-quality oxygen tubing has a tendency to kink and can even tear if it’s bent out of shape enough. You should make it a habit to check your cannula and tubing regularly to ensure this doesn’t happen, but it’s best to just invest in high-quality nasal cannulas in the first place to avoid this situation.
Tubing Length
Another important thing to consider is the length of the oxygen tubing. Tubing is sold in a variety of lengths like 10 feet, 15 feet, and even longer. Ideally, you’ll want to use shorter tubing because longer tubing can be a tripping hazard and can affect the way oxygen is delivered. When you’re using a pulse flow unit like the Inogen One G5, the device needs to be able to recognize your breaths so it can deliver a precisely timed bolus of oxygen. Most specialists recommend a cannula shorter than 35 feet to ensure the oxygen is being delivered immediately upon inspiration.

Cannula Design
The design of the nasal cannula primarily affects its comfort. There are various types of cannula and depending on your preference, you may choose one over another. Below are the types of cannulas you can choose from.
- Curved prong cannulas
- Flared prong cannulas
-
Straight prong cannulas
You’ll also be able to choose between straight oxygen tubing and coiled oxygen tubing which is great if you want to limit the space your oxygen tubing takes up and it will also make it less of a hazard to you and others. If you need help making your oxygen tubing and cannula more comfortable, we wrote a great article about this a while back. You can find it here.
Conclusion
The Inogen One G5 is a fantastic portable oxygen concentrator. In the short amount of time that it’s been on the market, it’s rapidly become the most sought-after machine due to its reliability, long battery life, and high oxygen output. But we’d be remiss not to mention all the great G5 accessories that help you make the most out of your new device.
The seven accessories we listed above will offer you more freedom in the way that you use your G5 and ensure that you always have access to medical oxygen wherever you go. If you have any questions at all about the Inogen One G5 or G5 accessories, don’t hesitate to reach out to us or stay tuned to our blog for updates on the latest Inogen products.
.png)
If you’ve been tuning into our blog the last couple weeks, you probably read our post comparing the Inogen G5 and the Inogen G3. In this post, we showed you some of the key differences between the units that you may not have known such as their size, weight, and battery life.
While the G5 and G3 are widely considered to be the best portable oxygen concentrators on the market, they are far from your only options. There are a host of high-quality portable oxygen concentrators by Inogen, Philips Respironics, SeQual, and more that have broken boundaries in the oxygen therapy field.
So, in an effort to better inform buyers about their options, we make it a priority to give each portable oxygen concentrator its fair share of time and shine a spotlight on the unique features of each device. In this post, we’re going to compare the Inogen One G5 portable oxygen concentrator and the Inogen One G4 portable oxygen concentrator.
If you have any questions about what you read here, feel free to leave them in the comment section below or get in touch with one of our respiratory specialists. They will be able to walk you through your options and respond to any questions or concerns you may have about Inogen portable oxygen concentrators.
Inogen One G4 Overview
The Inogen One G4 was released in 2016 to the U.S. market. At this time, it produced more oxygen per pound than any other portable unit and was praised for allowing COPD patients around the world to regain their freedom and independence.
The Inogen One G4 adapted a new design over the G3 which opted for a more sleek and minimalist look. Instead of the sieve beds being visible on the outside of the unit like with the G3, they’re embedded in the front of the unit in one single column.

Another welcome addition to the G4 was its connectivity. The new Inogen Connect app allowed users to interact with their portable oxygen concentrator via their smartphone or tablet. This app allows people to see their battery life, column condition, and other information without ever having to look at their G4 control panel.
Inogen One G5 Overview
Releasing in the summer of 2019, the Inogen One G5 is the latest and greatest portable oxygen concentrator available from Inogen. Aside from a few minor changes, the look of the G5 remained mostly untouched from the Inogen One G4.
.png)
The most notable improvement with the G5 is that it doubled the oxygen output of the G4. This expanded pulse dose technology significantly and allowed more people to benefit from ultra-lightweight portable oxygen concentrators.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2')}}
Weight
For many people, weight is the single most important factor when it comes to portable oxygen concentrators. With a light portable oxygen concentrator, you’ll be able to go where you want and do what you please without being overburdened or becoming breathless after a few minutes of walking.
Both the Inogen One G5 and the Inogen One G4 are pulse flow concentrators. What this means is that oxygen is only delivered when the patient inhales as opposed to continuous flow where oxygen is put out persistently. Using this technology, oxygen concentrator manufacturers are able to make smaller devices that still provide you with a reliable source of oxygen.
One of the major selling points for the Inogen One G4 is that it’s the lightest Inogen concentrator ever produced. The only concentrator that has it beat in this category is the AirSep Focus which has less oxygen output and shorter battery life. The Inogen G4 weighs in at just 4 pounds with the single battery which is a half-pound lighter than the G5.
Oxygen Output
Oxygen output is probably the most objective aspect of oxygen concentrators; you’re either getting the oxygen you need to stay healthy, or you need a device that puts out more oxygen. If you need to be on a flow setting of 3 or higher, then the G5 will always be a better unit for you because the G4 only goes up to a setting of 3.
Conversely, if you are in the early stages of COPD and see no reason to have a device that goes up to a setting of 6, then the G3 may be perfect for you. Another thing to note about oxygen output is because the G4 is so light you may not need as much oxygen to feel normal. However, before adjusting your flow setting you need to first speak with your pulmonologist.
One thing you need to take into consideration when deciding between the G5 and G4 is whether or not you will be moving to a higher flow rating anytime in the future. If you already use a setting of 3 and your doctor predicts you may need to move up soon, it would be wise to invest in a unit that can go higher than that.
Size
Size is one factor that you may find important when purchasing a portable oxygen concentrator. Large portable oxygen concentrators and oxygen tanks are not only heavy, but they tend to have awkward shapes as well. For example, oxygen tanks are long and have nozzles on the end that tend to get caught on things like clothing. This makes it difficult to store it anywhere without worrying about it getting damaged.
The G4 and G5, on the other hand, are designed in a way that makes them very easy to carry and store. They’re more box-shaped than many portable oxygen concentrators on the market meaning they don’t take up any more space than they have to. There isn’t anything that protrudes from the device either so you won’t have to worry about it getting caught on anything.

In terms of the actual dimensions, the G4 and G5 are pretty similar, however, the G4 is the lighter of the two units. The G4 is 7.2” H x 5.91” L x 2.68” W and the G5 is 8.15" H x 7.19" L x 3.26" W. That’s not a huge difference, but if you’re looking for the smallest unit possible, the Inogen One G4 is a great machine to go with.
Sound Level
People often come to us and express the concern that their oxygen concentrator will be too loud and that they’re worried about taking it places because it may disturb people. Fortunately, most concentrators on the market are pretty quiet, even continuous flow units, and shouldn’t be a cause for concern.
The Inogen One G5 rings in at just 38 decibels while the G4 is just two higher than that at 40 decibels on a flow setting of two. Either way, that’s about the sound level of a whisper or a quiet conversation.
Another thing to take note of is the audible alert system that’s built into both the G4 and the G5. The audible alerts will notify you when your battery is low or if certain parts need replacement. If you are in a public area, you may want to disable this and re-enable it once you’re back home because the alerts may be louder than the actual concentrator.
Battery Life
Because portable oxygen concentrators cannot be plugged into the wall at all times like a home oxygen concentrator, they need a power source to draw from. The quality and longevity of your batteries are important because you don’t want to be out of the house without a way to power your portable oxygen concentrator.
Within the past couple of years, Inogen has put a lot of work into making their batteries more lightweight, efficient, and reliable. The Inogen One G5 double battery can go up to an astounding 13 hours on one charge with a flow setting of 1. That’s a steep incline from the G4’s maximum battery life of just 5 hours on a setting of 1.
FAA Approved
Part of regaining your freedom and independence means being able to fly on a plane again without hassle. Fortunately, you can rest easy knowing that both the Inogen One G5 and the Inogen One G4 are approved by the Federal Aviation Administration (FAA). What this means is that you’ll be able to bring your oxygen concentrator onto the plane as a carry-on item no matter where you are in the world. Due to the size and weight of the G4, you’ll have more options when it comes to storing your device while in flight.

Connectivity
One thing that’s unique to both the Inogen One G4 and Inogen One G5 is their connectivity. Whenever you purchase one of these devices, you will have access to a free smartphone application that connects to your portable oxygen concentrator. This app is called Inogen Connect.
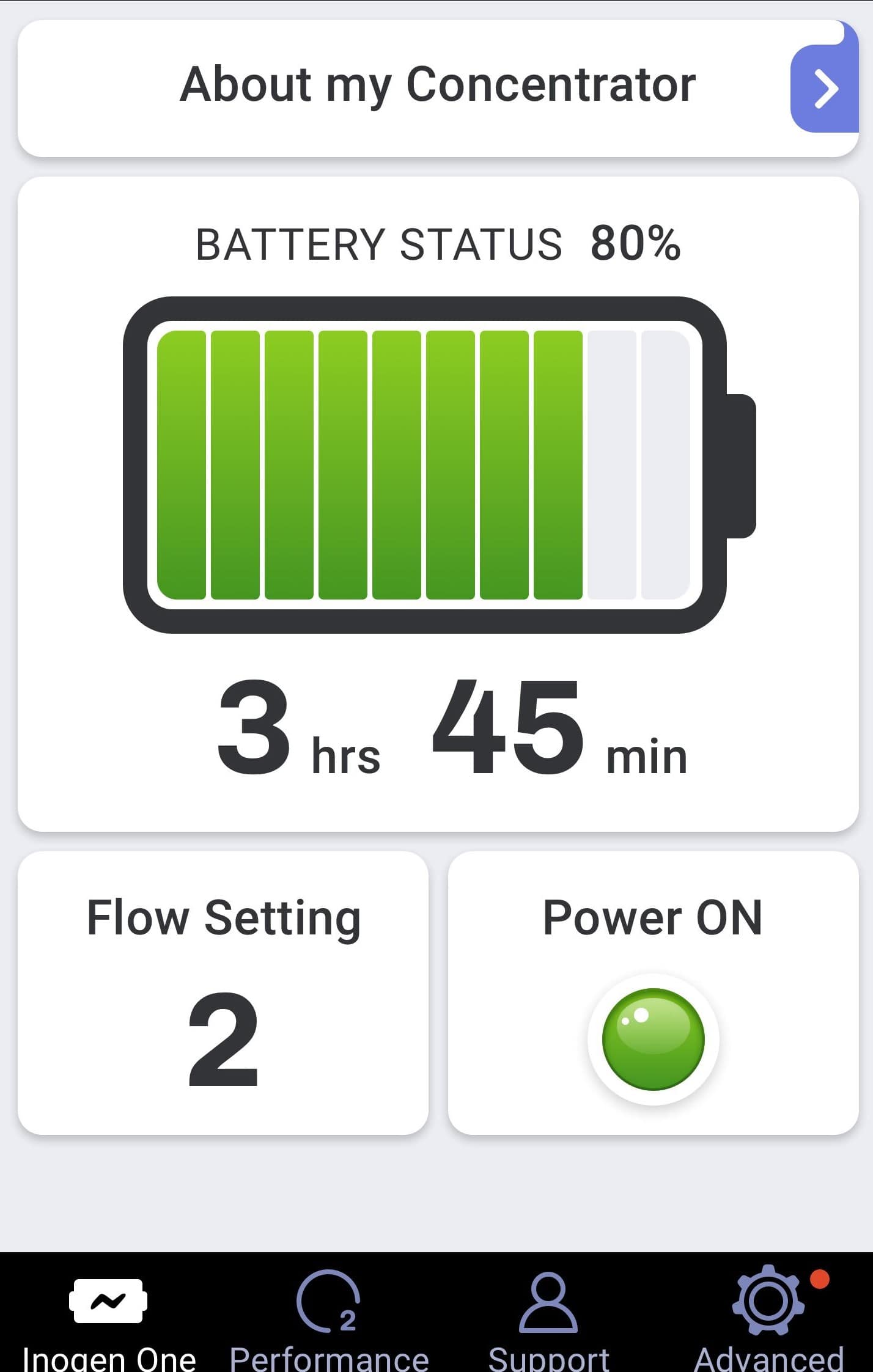
Using the Inogen Connect app, you will be able to get important updates about your POC without ever having to look at it. Below is some of the information you will see:
- Battery status
- Software updates
- cannula and filter maintenance updates
- Column life
- Troubleshooting tips, FAQS, and the user manual
-
Oxygen purity status
There’s no understating how convenient it is to have Inogen Connect. Unlike with other portable oxygen concentrators on the market, you’ll never have to take your user manual with you or remove the device from its carrying case to check its battery status or view other important information.
G4 and G5 Side-by-Side Comparison
|
|
|
|
|
Oxygen Settings |
Pulse Dose: 1 to 6 |
Pulse Dose: 1 to 3 |
|
Weight |
4.7 Pounds |
2.8 Pounds |
|
Battery Duration |
Up to 6.5 hours with single battery Up to 13 hours with double battery |
Up to 2.7 hours with single battery Up to 5 hours with double battery |
|
Battery Charge Time |
Up to 4.5 hours with single battery Up to 9 hours with double battery |
Up to 3 hours with single battery Up to 5 hours with double battery |
|
Maximum Oxygen Output |
1260 ml/min |
630 ml/min |
|
Noise level |
Around 38 decibels |
Around 40 decibels |
|
Dimensions |
Width: 7.19 inches Depth: 3.26 inches Height: 8.15 inches |
Width: 5.91 inches Depth: 2.68 inches Height: 7.2 inches |
Who Should Buy the Inogen One G4?
The Inogen One G4 is a fantastic portable oxygen machine that’s still the second lightest unit on the market, despite it being several years old. The best candidate for the Inogen One G4 is someone who wants a lightweight and small form factor concentrator that’s backed by a reputable and reliable brand like Inogen. However, be aware that it only goes up to a pulse flow setting of 3.
While the Inogen G4 is not the newest oxygen concentrator by Inogen, it remains a popular unit among COPD patients all over the world. Due to the high demand for the G4 Inogen still supports it by selling batteries, accessories, and replacement parts. Patients looking to buy a G4 will be happy to find that Inogen will support the device for years to come.
Who Should Buy the Inogen One G5?
The Inogen One G5 is the fifth generation of portable oxygen concentrators by Inogen. It’s the most advanced unit they offer with an impeccable battery life, lightweight design, and high oxygen output. The ideal candidate for the G5 is someone who wants the best battery life and highest oxygen output possible for a pulse flow unit.
Since the Inogen One G5 is the newest device by Inogen, you will always be able to find technical support if you need it. Most oxygen retailers sell this unit and many of them will repair it or send you replacement parts if you need it. Currently, the G5 offers the highest oxygen output of any pulse flow unit and the longest battery life.
Conclusion
As you can see, both the Inogen One G4 and the Inogen One G5 are viable portable oxygen concentrators. While the G5 is still the most advanced oxygen concentrator on the market, the G4 still has a lot to offer if you want an extremely small and lightweight unit. At the end of the day, it’s a matter of what your oxygen demands and preferences are.
Personally, we love the Inogen One G5 because it’s proficient or excels at everything it does including battery life, weight, size, oxygen output, and more. As such, we gave it the title, “the best portable oxygen concentrator of 2020.” If you’re still not sure which oxygen concentrator is right for you, be sure to get in touch with us and we’ll walk you through your options.
Living healthily and happily with COPD is all about developing healthy lifestyle habits and learning how to keep your symptoms under control. Because it is a chronic disease with no real cure, the only way to manage it is by keeping up with daily medication and carefully following treatment goals.
That's why all COPD patients should have a personalized COPD action plan to help them keep track of their medications and other treatment goals.
A COPD action plan is a comprehensive set of instruction on how to manage and treat your COPD. It's the most important tool you have for keeping your symptoms under control and preserving the health of your lungs and the rest of your body.
A typical action plan includes all the important parts of your COPD treatment, including your medication schedule, what to do when your symptoms act up, and your diet and exercise regimen. It also helps you remember what to do in an emergency and know when to see your doctor for a problem.
In this post, we're going to help you better understand what a COPD action plan is and how you can use it to better manage your disease. We'll show you what a good action plan looks like, how to make one with your doctor, and how to put your treatment plan into action.
Crafting your COPD Action Plan

Putting together your COPD action plan is an individualized process that you and your doctor will go through together. Every patient's action plan is unique and tailored to fit their personal needs.
A good COPD action plan will give you detailed treatment instructions and clear plan for what to do if your symptoms get worse. It should take your medical history, lifestyle, symptoms, and other life factors into account.
As you and your doctor work on your action plan, it's important to have a clear picture of both your current situation and your future goals. Here are some tips to help you and your doctor better understand your condition and get on the same page.
Track Your Symptoms
Helping you manage your COPD symptoms is the most important purpose of a good COPD action plan. But in order for it to be useful and accurate, you and your doctor need to have as much information as possible about all symptoms you experience and how they fluctuate over time.
The best way to get a better understanding of your symptoms is to record them daily with a journal or a symptom checklist. This will help you remember what symptoms you had and when you had them the next time you talk to your doctor, and to track patterns and changes over time.
You should try to make your notes as detailed as you can so that you and your doctor have as much information to work with as possible. Make sure you write down any and all ailments you experience, even ones that seem small or inconsequential.

The more information you have on your condition and symptoms, the more useful your action plan will be. However, it's worth writing down your symptoms even after you have an action plan in place. It will not only make it easier to notice changes in your condition as the disease progresses, but will also help you adjust your action plan as your symptoms change.
Here are some tips for what you should include in your daily symptom diary:
- Write a list of any and all physical and psychological symptoms you experience every day, especially breathing and respiratory problems. (e.g. breathlessness, fatigue, muscle weakness, coughing, anxiety, depression, etc.)
- Record and notable changes or improvements in your symptoms compared to recent days.
- Record any changes in the frequency or severity of your cough, and note any changes in the color and consistency of any mucus you cough up.
- Keep a detailed record of any breathing issues and when they get better or worse throughout the day. Record what kinds of activities cause you to feel short of breath and your general ease of breathing from day to day.
- Keep track of how much sleep you get (in general) and any sleeping difficulties you have, such as insomnia or waking up frequently during the night.
-
Write down the general time and situation in which your symptoms occurred. (e.g. all day long, in the morning, after eating lunch, after exercising, after going to bed, etc.)
- Include any special circumstances surrounding your symptoms. (e.g. you were outside in the heat, your allergies were acting up, you forgot to take your daily medication, etc.)
- Keep track of your overall mood and mental state from day to day. (e.g. you felt tired, you felt motivated, you felt anxious, etc.)
- Record any prescription or over the counter medications you took that day and approximately what time you took them.
- Keep track of any exercise or physical activities you do.
- Record any smoking, tobacco, or other drug use (including alcohol).
As you start your COPD symptom diary, it may help to have a complete list of COPD symptoms on hand to help you know what to look out for. You can also use a COPD symptom checklist, like this one here, to help you remember what's important to keep track of.
Think About Your Goals

In general, it is the goal of every COPD patient to breathe easier and reduce other respiratory symptoms. However, these larger goals are difficult to reach without first breaking them down into smaller goals that are easier to act on.
For example, if you smoke cigarettes, one of your goals could be to reduce the amount of cigarettes you smoke or stop smoking altogether. You could break this goal down into even smaller steps, too, such as going to a smoking cessation counselor or joining a quit smoking program.
You should also think about your lifestyle and any areas that you need to improve. For example, you may need to lose weight, eat more fruits and vegetables, or get more exercise to keep your body strong and prevent COPD complications.
Other goals might relate directly to your symptoms and helping you breathe comfortably throughout the day. Things like always taking your medications as directed, pacing yourself during exercise, and utilizing therapeutic breathing techniques can help you reach those goals.
Once you know what you are striving for, you and your doctor can put together a treatment plan that addresses all of these goals. The following list will give you an idea of some of the major treatment goals that you should consider as you craft your COPD action plan.
General COPD Treatment Goals:
- Quitting smoking
- Improving your ability to breathe
- Getting more exercise to strengthen your body and lungs
- Eating a healthier, COPD-friendly diet
- Reducing coughing, wheezing, and other respiratory symptoms
- Reducing the number of COPD flare-ups and exacerbations you have
- Reducing your risk of COPD complications (e.g. heart attacks and osteoporosis)
- Slowing your disease from progressing further
- Working with your doctor and other medical specialists to track your symptoms and achieve your treatment goals
Consult With Your Doctor

Once you've had time to track your symptoms and brainstorm your treatment goals, it's time to sit down with your doctor to put together a comprehensive COPD action plan. Your doctor may have a standard template, like this one, to fill out, or he might put together a custom document for you to take home.
Make sure you bring your symptom diary and any other information about your medical history that your doctor may need. Your doctor will also use lung function tests, including spirometry, to determine your treatment and medication needs.
It's important for your doctor to include you in his process and thoroughly explain every part of your action plan and how to use it. Take the time to look over your treatment plan carefully and don't be afraid to ask questions or ask for clarification.
While your COPD action plan helps your doctor coordinate your medications and treatment goals, your action plan's primary purpose is to be a resource for you. It is very important that you understand your plan in its entirety and how to use it to manage your disease on a daily basis.
Depending on your condition and situation, you may have a team of doctors and specialists working to help you stay healthy. In this case, you will need to coordinate your action plan with all of your caretakers to ensure your plan is as cohesive and comprehensive as possible.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The Three Zones of Your COPD Action Plan
It's important to understand that your COPD action plan is actually split up into three distinct plans of action. From here on out, we will refer to these three plans as the green zone, yellow zone, and red zone action plans, as this is the typical way to organize them.
These three zones make up the core of your COPD action plan and tell you what to do in different situations. They tell you how manage your COPD when your symptoms are normal (green), worse (yellow), and severe (red), and how to know which zone's action plan to use.
This scheme is very useful for helping you recognize when you experience a flare-up or you need to call your doctor or seek emergency medical attention. It also helps you remember how to stay healthy and what to do when your symptoms get worse.
Think of each zone as representing a specific plan of action depending on how you feel on a particular day. It is composed of two main parts: your symptoms and the actions you should take.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The first part is a description of the symptoms and the duration of symptoms that correspond to that particular zone. This is meant to help you recognize when your symptoms fit the requirements for that zone's action plan, so you can always tell when to take the actions for that zone.
The second part is a list of actions you should take whenever you experience the symptoms that correspond to that zone. It may include things like what medication to use, how much exercise you should do, breathing techniques, mental health strategies, and other instructions for keeping yourself healthy.
For example, the green zone would include your normal, baseline symptoms and strategies for managing them on a regular basis. It would also include a list of actions to take on a regular day when your symptoms are at a typical level.
The Yellow zone should include a description of what it looks like when your symptoms flare up, and what to do to manage them and keep them from getting even worse. You would refer to the actions and strategies in this zone when you experience a minor flare up or exacerbation.
The red zone gives you instructions on what you should do when your symptoms get more severe. It will help you recognize at what point you should seek medical attention and what to do in an emergency.
The symptoms and actions that go in each zone will depend on your medical history, lung function, and your personal COPD symptoms. Since it is based on your baseline symptoms, which may be more or less severe, your green zone action plan may differ significantly from other patients, and will change as your disease progresses.
Here is an overview of the different action plan zones and when you should use them:
- Green Zone: “I am doing well today.” Use this plan when your symptoms are at a normal, baseline level, and you feel well enough to continue your usual exercise and activities.
- Yellow Zone: “I am not feeling well today or I am experience a COPD flare-up.” Use this plan when your symptoms are worse than normal, you are having difficulty breathing during your usual activities, or you notice a change in your mucus, your sleep quality, your appetite, or the frequency with which you have to use your quick-relief medications.
- Red Zone: “I need urgent medical care.” Use this plan if your symptoms become very severe, to the point that you feel shortness of breath at rest and are unable to do any physical activity. Breathing difficulties that severely interfere with sleep, fever or shaking chills, feeling confused, coughing up blood, or having chest pains are other signs that you need emergency medical care and need to follow your red zone plan.
To see an example of what an actual COPD action plan looks like, you can check out this sample plan from the American Lung Association.
Daily Treatment Goals and Instructions (Green Zone)
Your daily symptom management and treatment goals—the green zone—is one of the most important aspects of your COPD treatment plan. It contains all the medications and actions you should take on a typical-symptom day to stay healthy and keep your symptoms under control.
When your symptoms are at your usual baseline level, you should follow the actions in this plan. If you keep your COPD well-managed and minimize flare-ups, you should be able to use your green zone plan on most days.
It's a good idea to review this part of your plan regularly, even though you use it often, just to jog your memory and review your goals, medications, and treatments. It will help you stay motivated, keep on track, and remind you of any habits or treatment methods you may have gotten lazy about doing.
Your Plan for Managing Flare-ups and Exacerbations (Yellow Zone)
Generally, any noticeable increase in COPD symptoms should direct you to use your yellow zone action plan, including feeling low on energy, experiencing more difficulty breathing, worsened coughing, or changes in your sleep quality and appetite. You should also look for changes in the color and consistency of your mucus and how frequently you have to use your quick relief medications.
When your symptoms flare-up or your breathing problems get worse, your yellow zone plan will tell you exactly what you need to do to keep your symptoms under control. It should include your usual maintenance medication along with instructions on how to use your quick-relief medications effectively.
Your yellow zone action play will likely include other treatments for reducing your symptoms, such as breathing techniques and mucus clearance techniques, which we will discuss more in the following sections. It may also include stricter guidelines for using supplemental oxygen and protecting your lungs from inflammatory environments and irritants.
Your doctor may instruct you to start taking a course of antibiotics or corticosteroid medications when your symptoms get worse as part of your yellow zone action plan. You may also need to call your doctor if your symptoms don't get better within a day or two.
Your Plan For Emergencies (Red Zone)
The purpose of your red zone action plan is to remind you of what to do in an emergency. You should follow this plan when your symptoms become so severe that you have difficulty breathing at rest.
Extreme shortness of breath, severe fatigue that interferes with daily living, or being unable to do light physical activity is a sign that you need to seek immediate medical attention. Other signs include chest pain, coughing up blood, fever, chills, confusion, and symptoms that are so severe that you are unable to sleep at night.
If you experience any of these symptoms, follow your red zone action plan and call 911, or have someone else drive you to the emergency room as quickly as possible. You may also need to take a medication or adjust your oxygen prescription to help you cope until you get to the hospital.
The Components of a Good COPD Action Plan
A good COPD action plan contains everything you need to know about managing your disease on a daily basis and when your symptoms flare up. It should tell you what medications to take every day, what medications to take when your symptoms get worse, and all the actions and habits you need to do on a regular basis to keep your lungs healthy and your symptoms under control.
Many action plans also include information about your diet, exercise, and lifestyle goals related to your COPD. In these next sections, we'll explain all the different components that your COPD action plan may include as part of your green and/or yellow zone plans.
Your Medications

Your COPD action plan should include all of the prescription and over-the-counter medications that you need to treat your COPD. It should tell you what medication to take when your symptoms are at baseline, what medication to use as-needed (and when to use it), as well as the correct dosage and the frequency that you should take it.
Your maintenance medications help you breathe easier on a daily basis and are the cornerstone of daily COPD treatment. However, you have to take them every single day as directed by your doctor in order for them to be as effective as they can be.
On the other hand, not keeping up with your daily maintenance medications can make your symptoms worse and cause your COPD to progress faster. By keeping your symptoms minimized on a daily basis, your maintenance medicine is very important for staving off flare-ups, exacerbations, heart problems, and other serious COPD complications.
Your doctor may also prescribe quick-relief or rescue medications—in addition to your maintenance medicine—to use as part of your yellow zone action plan on days when you experience worsened COPD symptoms. These medications help reduce sudden, uncontrolled symptoms and help you breathe easier when your symptoms flare up.
Your doctor may also give you a course of steroid medication or antibiotics to use when you notice your symptoms getting out of hand. Most of the time, you will be instructed to take them if your symptoms stay worse for more than a day or two or when you notice the signs of an oncoming exacerbation.
Whenever you start a course of antibiotics, it's very important that you continue to take the entire course, even after you start to feel better. As long as you use them correctly and as directed by your doctor, antibiotics and steroid medications can help you avoid serious exacerbations and recover from flare-ups more quickly.
Your COPD action plan should also include information about any vaccines you need, including pneumonia and influenza vaccines. Most adults need another dose of the pneumonia vaccine after the age of 65, and all COPD patients should get their yearly flu shot to stave off exacerbations and infections.
Whatever medications your doctor recommends should be included in your action plan along with enough detail to help you use them reliably and consistently. If you have any questions about your medications or how to use them, talk to your doctor and ask him to clarify the instructions in your plan.
Breathing Exercises

Breathing exercises like pursed lips breathing and diaphragmatic breathing are a vital part of daily COPD management for patients who struggle with shortness of breath. These breathing techniques help you control your breaths and even strengthen the muscles in your chest that you use to breathe.
Practicing breathing techniques every day can help you keep your breathing steady and under control when you exercise and do other active, daily tasks. They can also help you manage minor symptom flare-ups and get through bouts of coughing more easily.
If you deal with breathlessness and coughing often, your doctor may recommend breathing exercises as part of your everyday COPD management plan. They may also be helpful to practice when your symptoms get worse as part of your yellow zone action plan, too.
Managing Airway Congestion
Excess mucus is a common symptom that many COPD patients have to manage. If you don't take care to stay hydrated and clear the mucus out of your lungs, it can make symptoms like coughing and breathlessness worse.
If you let mucus build up in your airways, it narrows the passages that air can flow through and makes it more difficult to breathe. Mucus buildup can also trap bacteria, viruses, and irritating particles that can inflame your airways or cause infections in your lungs.
Because of this, keeping your airways clear of mucus is often an important part of managing COPD. To address this, your treatment plan may include mucus clearance techniques to use when you get excess phlegm.
The goal of mucus clearance techniques is to dislodge stuck mucus from the walls of your airways and cough it up and out of your lungs. Often a two-pronged approach of proper hydration and huff coughing can help you keep congestion under control.
Staying hydrated thins out your mucus, while coughing moves the mucus up through your airways so you can cough it up through your mouth. Your doctor may also recommend a variety of other mucus clearance techniques and aids, such as chest percussion, positional drainage, or using a special high frequency chest wall oscillation vest, as part of your COPD action plan.
Quitting Smoking
If you are a smoker, then quitting should be your number one priority and included as part of your COPD action plan. Quitting smoking will help prevent further damage to your lungs, reduce flare-ups, and preserve the lung function that you still have left.
To help you quit, you may want to include a quit smoking program or therapy as part of your COPD management plan. If you are unable to quit, reducing the number of cigarettes you smoke or seeing a smoking cessation therapist can help put you on the right track to ending your addiction.
If you want help quitting smoking, check out this article, “Where to Get Help When You Decide to Quit Smoking,” from the National Cancer Institute. You can also get more information about smoking cessation and quit smoking resources from the CDC, the American Lung Association, smokefree.gov, and many other places online.
Other Healthy Lifestyle Goals
Everyone experiences bloating every now and then, often the result of a big meal or a minor stomach illness. However, bloating tends to be a frequent problem for people with COPD for different reasons, and it's a problem that is frequently underestimated.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2')}}
Bloating tends to be particularly uncomfortable for COPD patients because it can make it much more difficult to breathe. Common COPD symptoms like chest soreness and coughing can also feel much worse when your belly is bloated and tight.
What many patients don't realize is that their COPD bloating symptoms could be directly or indirectly caused by their disease. In some cases, treating underlying COPD symptoms can relieve and prevent bloating or at least make it much more tolerable.
In this article we're going to help you better understand the connection between COPD and abdominal bloating and what you can do about it. We'll explain how and why COPD bloating happens, how to reduce bloating, and how to better manage your symptoms and feel more comfortable when bloating unexpectedly strikes.
The Connection Between COPD and Abdominal Bloating

Bloating is a symptom that many people with COPD deal with on a regular basis, and it can make it more difficult to cope with the disease. However, despite how common bloating is among COPD patients, many doctors and patients don't realize that the two conditions could be related.
Sometimes bloating is a direct result of COPD symptoms or medications, and sometimes it's a result of COPD-related lifestyle changes and complications. For example, COPD often makes it difficult to stay active and eat a healthy diet, both of which increase your risk for bloating.
It also works in the opposite direction; being bloated can make COPD symptoms like breathlessness worse. Bloating causes swelling in your stomach and intestines, which causes them to push up on your lungs and diaphragm.
Many COPD patients also have enlarged lungs which require extra room to expand. This combined with the extra pressure that bloating puts on your lungs can make it especially difficult to breathe.
Having a bloated stomach can also make your breathlessness worse when you eat, especially if your lungs are enlarged. Many COPD patients struggle to breathe when they eat because their lungs have less room to expand when their stomach is full.
What is Bloating?

Bloating is usually described as a feeling of tightness, pressure, or stretching in the abdomen. It is often caused by gas trapped in your stomach or intestines, and it can even cause your stomach to visibly swell up.
Bloating is usually caused by problems with digestion, such as when food moves too slowly through your digestive system; this creates more opportunities for it to be fermented into gas. It can also be caused by food allergies, illnesses, and digestive disorders like irritable bowel syndrome.
However, bloating can be caused by many other things, including medications, stress, inactivity, and swallowing air. Just about anything that can have an effect on your digestive system has the potential to cause bloating.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The most common reason that otherwise healthy adults experience bloating is a poor diet. Eating too many fried and fatty foods, eating too much, and not eating a balanced diet can all lead to bloating.
Bloating can also refer to water bloating, which happens when your body retains extra water, causing your limbs and abdomen to swell slightly. This kind of bloating can be just as uncomfortable as bloating caused by gas and causes many of the same symptoms.
While bloating isn't a serious symptom on its own, chronic bloating could be a sign of a more serious underlying condition. For people with COPD, frequent bloating is a problem because it can make other COPD symptoms much more difficult to manage.
How COPD Causes Bloating

There are a number of reasons why COPD patients are more prone to getting bloated. In these next sections we'll take a closer look at some of the most common reasons that people with COPD suffer from bloating.
Shortness of Breath
COPD makes it difficult to breathe and causes frequent episodes of shortness of breath. When this happens, it can cause you to gasp, wheeze, or hyperventilate, which can sometimes lead to bloating.
When you struggle to breathe, you tend to take quicker and shorter breaths. This makes it easier to swallow extra air into your stomach along with the breaths you inhale.
This air gets trapped in your stomach, causing it to expand and feel bloated. That, in turn, can put extra pressure on your lungs and make your breathlessness even worse.
Hyper-inflated Lungs

COPD causes many people—especially those with emphysema—to develop enlarged lungs over time. This happens because damaged lungs tend to trap air when you breathe, which prevents your lungs from deflating completely when you exhale.
Over time your lungs continue to trap more and more air, which causes them to stretch out to accommodate the extra pressure. This is known as lung hyper-inflation (also known as expanded lungs or “long lungs”), and it causes your lungs to become larger, less elastic, and take up more space in your chest.
Hyper-inflated lungs press down and put extra pressure on your diaphragm, stomach, and intestines, which can make it more difficult to breathe and eat. This can cause side-effects like poor diet and worsened shortness of breath, both of which can cause bloating.
What's more, having hyper-inflated lungs makes even minor bloating more noticeable and potentially extremely uncomfortable. This is one of the major reasons that bloating is such a problem for so many people with COPD.
Lack of Exercise

Many people underestimate how important exercise is to keep your digestive system running smoothly. Exercise stimulates your digestive tract and is a very effective way to get your metabolism going.
Unfortunately, COPD often makes sufferers feel breathless and fatigued, which makes it difficult to exercise and stay active. This causes many people with COPD to avoid physical activity and lead more sedentary lives, which can lead to bloating.
When you don't get enough exercise, your intestines have a harder time contracting and moving food through. This slows down your entire digestive system and makes your stomach empty more slowly.
The longer food sits in your stomach and intestines, the more likely it is to create gases that make you feel bloated. It can also lead to indigestion, which can make bloating even worse.
On the other hand, when you exercise, it gets the muscles lining your digestive tract moving and helps your stomach empty faster. It also helps move gas through your intestines, making it less likely to build up and cause discomfort or bloating.
Diet

Many people with COPD struggle with uncomfortable feelings of bloating and breathlessness when they eat. This is partially because COPD patients are particularly sensitive to the pressure of a full stomach, which can push up on their lungs and make it more difficult to breathe.
It is much worse for patients with hyper-inflated lungs, who need even more space for their lungs to expand. In fact, some COPD patients experience such severe shortness of breath when they eat that it significantly disrupts their diet.
Some patients have so much trouble eating that they eventually give up on wholesome meals and healthy eating habits altogether. In the worst cases, some patients with advanced COPD experience such severe symptoms when they eat that they end up losing weight or even developing nutritional deficiencies.
Bloating can also trigger a cycle of worse and worse bloating, as it triggers worsened COPD symptoms like breathlessness which can cause you to swallow more air. You are especially prone to swallowing air and becoming bloated if you struggle to breathe while you eat, which is more likely if you are already bloated.
Many people with COPD are older adults who are particularly sensitive to certain foods that are known to cause bloating. Because of this and the other reasons mentioned, mealtimes can be tricky situations for COPD patients to navigate, especially those who suffer from bloating.
How to Reduce Bloating if You Have COPD
Eat Smaller Meals

Hyper-inflated lungs and breathing problems caused by COPD can make it difficult to eat without feeling bloated. The simplest and quickest way to solve this problem is by eating smaller portions at mealtimes to make sure you never get too full.
Instead of eating the traditional three large meals a deal, try eating five or six smaller meals and spacing them out throughout the day. That way, your stomach is never too full at any given time and you're less likely to feel bloated and breathless when you eat.
Whenever you cook meals or go out to restaurants, try to choose smaller portions and don't rush through your food. Take as much time as you need to eat, stop when you start to feel full, and don't be afraid to save leftovers for later.
If you have trouble eating enough at mealtimes without feeling bloated, make up the extra calories by eating healthy snacks throughout the day. It's important to make sure you get enough to eat in order to prevent malnutrition and other complications like osteoporosis.
Some COPD patients also benefit from using supplemental oxygen when they eat, which helps with shortness of breath and may prevent bloating. It can also help to sip water (but not too much) and take breaks when needed during your meals.
Here are some extra tips for breaking up your meals into smaller mini-meals and snacks:
- Try to fill your meals and snacks with healthy, whole foods including fruits, vegetables, healthy fats, lean protein, and whole grains.
- Avoid empty calories like simple carbs, sugar and soda that will just fill you up without providing healthy nutrients.
- Try to eat the most nutritious foods on your plate first, before you start to feel full.
- If you have trouble getting enough calories throughout the day, try eating some healthy, calorie-dense foods like nuts and dairy. These will provide your body with lots of calories and nutrients without taking up too much room in your stomach.
Eat More Slowly

When you scarf down your food too quickly it's easy to swallow extra air along with your food without realizing it. This can cause your stomach to feel bloated, which can make it more difficult to breathe.
Then, if you are struggling to breathe as you eat, you are even more likely to swallow air. This can create a vicious feedback loop where eating makes you feel bloated, being bloated makes you feel short of breath, and being short of breath causes you to become even more bloated.
The solution to this is to eat more slowly, which reduces the amount of air you swallow as you eat and helps prevent you from getting too full. Pacing yourself also gives you the chance to practice breathing exercises while you eat and pay closer attention to how your body and stomach feel.
Another benefit to eating more slowly is that it allows you to chew your food up more before you swallow. This speeds up digestion by giving the food more time to break down in your mouth, reducing the risk of bloating.
Get More Exercise

As we mentioned earlier, exercise helps kick-start your digestive system, which helps prevent uncomfortable gas from building up in your stomach. As a result, physical activity can be a powerful tool for reducing bloating and keeping your digestive tract running efficiently.
Exercise increases blood flow to your stomach and intestines, which helps stimulate the muscles that contract your intestines and move food through. This helps your stomach empty faster, which moves gas-creating foods into your small intestine, where they are less likely to cause discomfort.
Exercise also strengthens your abdominal muscles, which helps move gas more quickly through your intestines. This prevents gas from building up in your gut and reduces bloating and discomfort.
As you can see, exercise can be both a treatment for bloating and used as a preventative measure against bloat. If you experience COPD bloating often, then increasing the amount of exercise you get could make a significant difference in how gassy you feel.
Research shows that even a small amount of moderate exercise every week can substantially improve bloating symptoms. Just thirty minutes of physical activity three times a week was be able to significantly reduce bloating in people with irritable bowel syndrome, a common stomach disorder that makes sufferers especially prone to bloating.
If you live a sedentary lifestyle or often have long periods of inactivity, talk to your doctor about putting together a new exercise plan to help you increase your physical activity. Then, it's up to you to build the exercise habits that will help you be healthier and less bloated.
Even if you have limited mobility or exercise seems like a daunting task, there are many different kinds of aerobic and strength training exercises that are tailored for people with breathing disorders and chronic diseases. You can start by taking walks, exercising at home, or taking part in a pulmonary rehabilitation class.
Get Moving After Meals

Since we know that slow digestion contributes to bloating, and exercise speeds up digestion, then it follows that getting some exercise after you eat can help prevent bloating. This is supported by studies that show mild exercise after a meal can aid in digestion.
If you tend to feel bloated after you eat, then try to plan in some time for light exercise after you finish your meal. For example, you could take a short walk around the block or do some stretching exercises to get your digestive juices flowing.
However, you should save more serious physical activities for at least a couple hours after you eat. Heavy exercise reduces blood flow to your stomach and intestines, showing down your digestion, and could end up making you feel sick or nauseous after you eat.
Watch Your Posture
How you position your body during and after eating can have a significant affect on your digestion and how bloated you feel. The best thing to do is sit up straight while you eat and avoid lying down after meals.
Lying down and reclining your body makes it difficult to pass gas and encourages gas to build up in your stomach and intestines. Lying down also puts pressure on your lungs, which can make it even more difficult to breathe when you're bloated.
One study found that simply keeping your body upright can significantly reduce the amount of gas that gets trapped in your intestines. Because of this, keeping an upright posture, especially during and after meals, can reduce bloating and make it easier for you to breathe.
Avoid Foods That Cause Bloating

There are a variety of different foods that are known to cause bloating, although they don't affect everyone the same. Some people may be extremely sensitive to bloat-inducing foods while others have no problems at all.
Some foods cause bloating because they are difficult to digest or provide fuel for gas-producing bacteria in your intestines. Other types of foods, like fatty foods, cause bloating because they take extra time for your body to digest.
Let's take a closer look at some of the most common foods you should avoid that cause bloating.
Fatty Foods

Fatty foods, especially greasy and deep-fried foods, are a major cause of bloating. That's because foods that are high in fat take longer to digest and move through your system.
If you tend get bloated after meals, try to eliminate some of the most fatty foods from your diet. Reducing your intake of greasy foods and fried fast foods is especially important.
Instead, try to eat smaller portions of fat as part of a balanced meal along with fruits and veggies, lean protein, and complex carbohydrates. You might find that reducing the amount of fat you eat makes a big difference in how bloated and uncomfortable you feel.
Salty Foods

Salt causes your body to retain water, which can cause you to feel bloated. While this kind of bloating is different from bloating caused by gas, it can be just as uncomfortable and make it difficult to breathe.
According to the US Department of Health and Human Services guidelines, older adults should limit their salt intake to 1,500 mg or less every day. That translates to about ¾ teaspoon of pure salt.
Unfortunately, it's nearly impossible to stay under 1,500 mg of salt unless you go out of your way to avoid it. That means limiting processed foods, salty restaurant foods, and home-cooked meals that include a lot of salt.
Salt hides in all sorts of unexpected places, which is why the best way to limit how much salt you eat is to cook low-sodium meals yourself. Nearly all processed foods, including processed snacks, processed meats, processed cheese, canned foods, cereals, and boxed meals, contain unhealthy amounts of salt.
You should also check the nutrition labels on all the foods you buy and choose versions that are lower in sodium whenever possible. When you eat out at a restaurant you can check their menu online ahead of time to look for lower sodium options, or ask your server to recommend items that are low in salt.
Carbonated Beverages
Carbonated beverages are bubbly and fizzy because they are infused with carbon gas. This gas escapes from the liquid over time, which is why carbonated drinks get “flat” after they've been left open too long.
When you drink something that's carbonated like soda or sparkling water, the gas escapes from the liquid while it's in your stomach and intestines. This gas gets trapped in your abdomen, resulting in uncomfortable bloating and gassy symptoms.
If you tend to struggle with bloating, you should try to avoid soda and all other types of carbonated drinks. To make the adjustment easier, you can replace them with other flavored beverages, such as tea, coffee, or water infused with fruit.
Sugar Substitutes

Foods labeled “sugar-free” usually use sugar substitutes, known as sugar alcohols, as a replacement for normal sugar. Sugar alcohols work because they taste sweet but aren't processed by your body the same as other sugars; this makes sugar alcohols low in calories and usually reduces the effect they have on blood sugar.
However, the downside of sugar alcohols is that they aren't very digestible, which causes many people to experience stomach distress and bloating when they eat them. In fact, health experts say you shouldn't eat more than a couple servings per day of artificially-sweetened foods.
You can recognize the most common sugar alcohols on nutrition labels with the names xylitol, sorbitol, and erythritol. They are most often found in sugar-free foods like candies and desserts and also in sugar-free gum.
Here is a list of all the sugar alcohols you may find in foods:
- Xylitol
- Sorbitol
- Erythritol
- Maltitol
- Isomalt
- Manitol
- Lactitol
- Hydrogenated starch hydrolysates
Beans and Cruciferous Vegetables
Beans, legumes, and vegetables from the cruciferous family are all known to cause gas and bloating. This happens because they contain a lot of fiber along with certain types of carbohydrates that many people's bodies have a difficult time digesting.
If you tend to get bloated after eating
Exercise is absolutely vital for healthy living, especially if you have COPD or another respiratory disease. But when you're hooked up to your oxygen tank or concentrator, it can make working out and doing other physical activities a little bit more tricky.
Fortunately, exercising with oxygen isn't too difficult if you know how to do it right. In fact, the extra oxygen you get should make it easier to exercise by improving your endurance and making it easier to breathe.
In this article, we're going to give you a variety of tips and techniques to help you better manage exercise while you're using supplemental oxygen. That way, you can continue living an active, healthy life without letting your disease or your oxygen therapy get in the way.
How Oxygen Helps You Exercise

Many patients with COPD and other breathing disorders use supplemental oxygen when they exercise, including those who use oxygen 24/7 to manage their disease. If you have mild COPD, your doctor might prescribe you oxygen specifically to use when you work out or do other activities that make you feel short of breath.
When you exercise, your body's oxygen needs go up as your muscles work hard to move your body. This forces your lungs to work harder, too, by taking more frequent breaths.
This is why physical activity can make you feel so short of breath when you have COPD. Because your lungs don't work as efficiently, they have trouble absorbing enough oxygen to keep up with your body's needs.
As a result, your blood oxygen levels can fall, causing you to feel short of breath. It can also trigger other COPD symptoms like coughing, wheezing, and fatigue.
That's where oxygen comes in: it allows your lungs to absorb more oxygen with every breath you take. This keeps your blood oxygen saturation at a healthy level, and it can be particularly helpful during exercise.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
By helping your lungs work more efficiently, supplemental oxygen makes it much easier to exercise and do other activities that put extra strain on your lungs. It can also reduce your respiratory symptoms and make it easier to breathe.
Overall, oxygen therapy allows you to do more physical activity for longer periods of time without feeling as breathless or fatigued. It also helps keep your heart healthy by reducing the strain that is caused when your blood oxygen levels fall too low.
Now that you understand why using your supplemental oxygen is so important, let's take a look at how to use it when you exercise. In the following sections, we'll give you a variety of practical tips and techniques you can use right away to work out more easily on oxygen.
How to Exercise with Oxygen

Getting used to moving around and working out on oxygen isn't exactly easy. Oxygen equipment can be bulky, unwieldy, and difficult to handle, especially during physical activity.
However, the limitations you face because of your oxygen will be different depending on what kind of oxygen supply you use. For example, using a portable oxygen concentrator gives you significantly more mobility than oxygen tanks and full-sized oxygen concentrators.
Luckily, there are many ways to work around the challenges of exercising with all your oxygen equipment in tow. In these next sections, we're going to show you a variety of techniques for working around your equipment and exercising safely and effectively on oxygen.
By learning how to manage your symptoms, your equipment, and find oxygen-friendly exercises, you'll find that you can do all kinds of physical activities while hooked up to your oxygen machine. We'll show you how to make oxygen therapy more comfortable and so you can reap the greatest possible benefits from your oxygen when you work out.
Take heart in the fact that there are many solutions for making oxygen therapy more comfortable and convenient, no matter what kind of physical activity you enjoy. Even though it may take some adjustments, you can make exercise happen, whether you use oxygen just occasionally or 24 hours a day.
Use a Portable Oxygen Concentrator

When you use an oxygen tank or full-sized concentrator, you have to deal with long extension tubes that connect you to the device, which may be several feet away or even in a different room. However, a portable oxygen concentrator is small enough to carry on your person, eliminating the hassle and danger of getting tripped up by long tubes.
Many portable concentrators only weigh a few pounds and are easy to wear on your back or sling over your shoulder. Because you're not tethered to a heavy oxygen machine, this gives you much more freedom and flexibility to move around.
Using a portable oxygen concentrator allows you to go on walks, do aerobic exercises, and all kinds of other activities without hauling or maneuvering around bulky equipment. It also makes it easier to go to the gym when you don't have to wheel a heavy oxygen tank around.

While portable oxygen concentrators can be pricey, they give you much more freedom to live every day to the fullest. Using a portable concentrator can significantly improve your quality of life and make it much easier to stay active while using oxygen.
While you can sometimes rent a portable oxygen concentrator from your oxygen supplier, you will likely need to finance at least some of the cost on your own. Luckily, there are many options for financial assistance and affordable monthly financing with low payments. Depending on your situation, you may even be able to get Medicare or your private insurance provider to cover some of the cost.
Investing in a portable oxygen concentrator if you can is well worth it; they are light, maneuverable, and can make exercising on oxygen much simpler. However, if that is not an option for you, then you can still do many kinds of exercises while using larger oxygen tanks and concentrators.
Double-Check Your Equipment Before Your Workout

When you are exerting yourself during exercise, it's especially important to make sure that your oxygen source is working properly. Otherwise, you risk getting too little oxygen, which makes it much more difficult to exercise.
Because exercise puts extra strain on your lungs, you are at a higher risk of your blood oxygen levels dropping when you work out, which is bad for your heart and lungs. Low blood oxygen makes it more difficult to breathe, makes you feel fatigued, and cause other dangerous symptoms.
To ensure you get enough oxygen, double check your nasal cannula, oxygen mask, and tubing to make sure they are properly attached to your oxygen source. If you are using an oxygen tank, check your pressure gauge to ensure that there is enough oxygen left to last you through your whole workout.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
If you are using a portable oxygen concentrator, then you should always make sure that it is fully charged before you start to work out. It's also a good idea to keep an extra charged battery nearby in case the first one runs out of charge.
You may also want to bring an extra nasal cannula with you just in case you need to switch it out. You can carry all the supplies you need in your portable oxygen concentrator carrying case or in a separate bag or backpack, if needed.
Secure Your Tubing

When you're moving around a lot during exercise, the tubing that connects you to your oxygen machine can be a huge pain to manage. However, it is much easier to keep the tubing out of the way if you fasten it down securely before you work out.
First, you will need to secure the tube that connects your oxygen mask or nasal cannula to the extension tubing. The simplest way to do this is with a clip, which you can use to hook the tube to your shirt or waistband.
You can do this with a large safety pin (being extremely careful not to pierce the tube) or, preferably, with a special tubing clip. Some patients find that clipping their tubing to the back of their shirt is the most effective technique for keeping it out of the way.
You can also thread your tubing underneath your shirt, which can help keep it away from your arms as you exercise. Don't be afraid to keep experimenting with different arrangements until you find a system that works for you.
Next, you will need to secure the long extension tubing that connects your nasal cannula to your oxygen source. Otherwise, you risk tripping over the tube as you move around the room during your workout.
To do this, think about the arrangement of the space you will be exercising in and how much room you need to move around. Try to string your extension tubing off to side or otherwise out of the way of the main space.
To keep your tubing off the ground, string it over a hook positioned several feet off the ground. This will keep the tube away from your feet and reduce your risk for trips and falls.

It's very important to take the time to arrange your equipment and tubing so it won't trip you up as you exercise. Otherwise, you risk damaging your equipment or causing serious injury to yourself if you fall.
If you use a portable oxygen concentrator, then you can avoid this problem altogether by wearing your oxygen source on your body. That way, you can move around freely without any long lengths of tubing to get in the way.
Another thing that can help is to use swivel connectors to connect your nasal cannula to your extension tubing and your extension tubing to your oxygen source. This makes it easier to adjust the position of your tubing and gives you a more flexible range of motion.
Use Cushions to Reduce Irritation
The tubing that contacts your face and loops over your ears can cause irritation over time as it touches your skin and moves around. Exercise can make this skin irritation worse by jostling your oxygen mask, nasal cannula, and tubing around even more.
If you don't use them already, you should consider getting ear cushions to protect your ears from the tubing as you work out. These little pieces of foam absorb the impact of tugging and rubbing and can significantly reduce ear pain caused by oxygen therapy.

You can also get cushions to go right under your nose to prevent chaffing from your nasal cannula. You can also get soft, fabric covers to wrap any other sections of tubing that tend to rub against your skin.
You can find practical solutions to remedy other oxygen therapy side-effects, too, including mouth and nasal dryness, skin irritation, and chronic ear pain. You will be surprised at how much more bearable oxygen therapy becomes once you've implemented some simple measures of comfort.
To learn more about how to make using oxygen more comfortable, check out our previous post here. This guide will introduce you to a variety of special equipment, practical techniques, and DIY fixes that can make you much more comfortable on oxygen.
Clear Your Airways
COPD often causes excess mucus to clog up your lungs and airways, which makes it more difficult to breathe. Nasal secretions can also affect your oxygen therapy by clogging and dirtying your nasal cannula and tubing.
To address both of these problems, you can take some time to clear excess mucus out of your airways before you work out. You can do this with simple techniques like huff coughing or postural drainage, which help move mucus up and out of your respiratory tract.
You can also use tools like a lung flute, which creates vibrations when you blow through it to help dislodge sticky mucus from the walls of your lungs and airways. High-frequency chest wall oscillation works in a similar way, but with a vibrating vest you wear over your chest.
Back and chest percussion is another way to dislodge extra mucus so you can cough it out of your lungs. To do this, you will need a partner to firmly, repeatedly tap on specific places on your back and chest.
While these techniques may not get rid of the mucus completely, they can get rid of a enough of it to make it easier to breathe. By clearing out space in your airways, it allows more air to flow through, and can reduce unwanted coughing when you're trying to work out.
You should also make sure to drink plenty of water every day to keep your mucus thin, which makes it much easier to clear out of your lungs and airways. And, because oxygen therapy can dry out your mouth and throat, staying hydrated can reduce these side-effects and make oxygen more comfortable to use.

You will also need to drink extra water when you exercise, especially if you sweat a lot or work out in warm temperatures. Keeping a water bottle with you when you do physical activities will help you stay hydrated and also combat dryness from your oxygen therapy.
For more tips on how to clear your airways, check out our comprehensive guide on mucus clearance techniques here. The guide covers all the most effective techniques for getting rid of excess mucus in more detail, including more detail on the methods we touched on here.
Find Exercises for Small Spaces

If you are hooked up to a large oxygen tank when you exercise, then you will have some limitations on how much you can move around. Even portable oxygen tanks and concentrators are sometimes too heavy for patients to lug around during fast-paced activities.
That's why it helps to find exercises that you can do while keeping your portable oxygen concentrator or oxygen tank on the ground nearby. These include exercises that allow you to stay stationary or only move within a small area so you can work out without having to move your tank or carry your portable oxygen concentrator around.
Some examples of activities that allow you to stay in one spot include jogging in place, using a stair step machine, or riding a stationary bicycle. Chair exercises are another great idea because you can sit in one spot with your oxygen source nearby and conserve energy while you build muscle tone.
Resistance bands and free weights are also great tools for building muscle while standing in place. If you have a gym membership, you can also use a variety of exercise machines that can help you maintain your balance and learn proper form.
All of these exercises are easier to do on oxygen because they keep you easily within the reach of your oxygen tubing. This allows you to set down your oxygen tank or concentrator nearby and more or less forget about it until it's time to move again.
Slower-paced activities like walking are also easier on oxygen, because they allow you to carry or wheel your oxygen tank or portable concentrator behind you as you go. You can also try yoga or tai chi, which are exercises made up of slow, fluid movements that are less likely to be hindered by your oxygen equipment.

Including these kinds of stationary and slow-paced exercises in your workout will free you from having to worry about re-arranging your tubing or lugging around your oxygen source while you're trying to focus on exercise. You'll find that working out is much more comfortable when your routine isn't constantly interrupted by having to move your equipment around.
Eat a Healthy Diet
Eating a well-balanced diet that's low in carbs is important for your lungs and can make it easier to exercise. As we've discussed on this blog before, eating too many carbohydrates is hard on your lungs, and can actually make it more difficult to breathe.
By eating a healthy diet, you ensure that your lungs have all the vitamins and nutrients they need to work as effectively as they can. By limiting how many carbs you eat, you can help your lungs work more efficiently, which can reduce how breathless you feel when you work out.

Healthy eating habits work in concert with your oxygen therapy to keep your blood oxygen levels up while you exercise. It can also help you stay more active, more healthy, and make a noticeable difference in your COPD symptoms.
Take Breaks When You Need To

Even if you use oxygen properly when you exercise, you might still struggle with breathlessness throughout your workout. If this happens, don't be afraid to slow down or take a break before continuing to exercise.
As long as you stick to a healthy exercise routine, it's okay to take it at your own pace. While you should try to do as much as you can, it's important not to push your body past its limits.
Talk to Your Doctor

As always, you should talk to your doctor before making any major changes to your activity level or workout routine. While most COPD patients are encouraged to stay as active as they can manage, some patients may have special conditions or limitations to consider.
Your doctor can tell you what kinds of activities are safe and if there are any kinds of exercises you should or should not do. Never hesitate to call or schedule an appointment with your doctor any time you have questions or concerns about your exercise routine or the symptoms you experience when you work out.
Other Tips for Exercising with COPD
Many people struggle to exercise because of their COPD symptoms, even when they use supplemental oxygen. Luckily, there are therapies and medications that can help you exercise more effectively while keeping your COPD symptoms under control.
For example, you can ask your doctor to refer you to a pulmonary rehabilitation class, which is a special program designed to help people with breathing disorders like COPD. Pulmonary rehabilitation teaches you how to better manage your symptoms and stay active through exercise classes and hands-on instruction.
Another thing you can do is practice breathing exercises, which can help you improve your breathing technique. By teaching you how to control your breath and push trapped air out of your lungs, breathing exercises can make it easier to breathe and easier to exercise without feeling short of breath.

It's also very important to always take your medication on time every day according to your COPD treatment plan. Some doctors also recommend using your bronchodilator medication before you exercise to make it easier to breathe.
Physical activity is important for your heart, your lungs, and your overall quality of life, which is why it's vital to stay active, even if you have to start small. If you struggle to exercise for any reason, talk to your doctor about what you can do to improve your symptoms and work out within your limitations.
For more tips on how to exercise with COPD, you might want to take a look at our article on Pulmonary Rehabilitation or our guide to Exercising at Home with COPD.
Conclusion
While oxygen can make exercise a little more complicated, there's no reason to let it get in the way of living an active life. If you remember the tips and tricks in this article, you should have no problem working out and staying active while using oxygen.
Whenever you get frustrated or discouraged, remember that your oxygen is your lifeline, and it can allow you to do more as you manage your COPD. Many people are able to live much healthier and active lives with oxygen, and you should think of it as an asset, not a hindrance.
Using oxygen is an adjustment at first, but it gets easier with time. It may take a little practice and patience, but soon you'll find that oxygen makes you even more capable of living the life you desire.
Whatever you do, don't give up on exercise and allow yourself to fall into a sedentary pattern. Take action and take charge of your health instead of letting COPD define and limit what you can do.
Remember that you are not alone in your struggles, and many oxygen patients are managing the same problems that you are every day. Remember that many of them successfully manage these problems and live active, fulfilling lives.
As long as you remain confident in your ability to manage your own health you can handle any challenges that come your way. If you stay motivated, stay active, and follow your COPD treatment plan, you'll be able to manage your COPD and keep your body strong.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!















