Oxygen to be harnessed and used to treat respiratory patients is a relatively new form of medication, but it has been proven to increase the quality of life and even add years to people's lives with severe respiratory illnesses. As with any new treatment or medication, the tools and methods are evolving, becoming more advanced and efficient. The history of oxygen as a drug moves in an exponential trend towards the safest and most efficient devices that LPT Medical carries today.
As a modern day medical equipment company based in Denver, CO and other locations including Boca Raton, FL., we are humbled by the history of oxygen therapy products in particular. We want to appreciate all the pioneers and innovators who came before us, the ones who paved the way into a new-age of technology for people struggling with respiratory diseases.
Without their ingenuity we would not be here today, able to offer our customers these top of the line products like the Inogen One G5 and the Caire Freestyle Comfort. Oxygen has come a long way, and the methods in which oxygen is prescribed and the devices used to administer oxygen have both progressed into the safest and most effective products.
There was a moment in time where to pursue oxygen as a therapeutic resource for patients with chronic lung disease was cause for concern. In the 20th century of the risks of experiencing oxygen toxicity due to the administration of oxygen therapy was relatively high. Oxygen toxicity is a form of lung damage that occurs when you breathe in too much supplemental oxygen. It’s also called oxygen poisoning, and it happens to divers, people who use too much of their medical oxygen supply, or those who use supplemental oxygen and do not have low enough blood-oxygen levels.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you are using portable oxygen for long-term oxygen therapy purposes, your healthcare team will test you while you are doing normal activities or exercise and at rest to determine that your oxygen is at the correct setting. Talk with your doctor about how to use oxygen safely and correctly if you are unsure.

Similarly to any new medication or treatment, time and research was put into the application of oxygen as a drug, and overtime and with the accessibility of ambulatory oxygen devices, the long-term effects of continuous oxygen were able to be established and meet certain safety and efficiency requirements that we have today.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Today, there are three popular ways to get your oxygen outside of the hospital:
.
- Liquid oxygen tanks
- Compressed gas cylinders
- Portable oxygen concentrators
With a portable oxygen concentrator (POC) you will be able to carry this small, battery-powered device around with you, use it at home all day and night, and even take it with you on an airplane.

Your POC will come with a carrying case that you can throw around your shoulder if your device is light-weight enough to carry. You can also get a portable oxygen concentrator backpack that will carry your POC and other belongings. Other POCs come with wheels or a cart if they are 10 pounds or more like the Respironics SimplyGo and the Solar Eclipse 5. Both of these devices are continuous and pulse dose capable, offer high oxygen outputs, and they are still very portable.

POCs run on batteries, so a device with a larger battery will last longer, and you will never have to get the device “refilled” instead you will plug in the device or the battery to an external charger or an AC or DC outlet, and you can use the device while the batteries charges.
A liquid oxygen system has a refillable oxygen reservoir that is stationary inside your home and other smaller refillable portable tanks that you can take with you when you leave your home. The tanks are very cold, so you have to be careful when you handle them. Your delivery company will refill your tank about every 2 weeks, and you will refill your own portable tanks when you need to with the large reservoir in your home.

A compressed gas system can also be used at your home. It includes a stationary oxygen concentrator with a long tube. When you go out, you carry a portable tank. Your supplier can deliver the portable tanks to you refilled, or you can refill it on your own from your concentrator. When you go out with your portable tank, you’ll use an oxygen conserving device that supplies small, pulsed doses to help your portable tank last longer.
Based on this information, it might be evident that the portable oxygen concentrator is the newest and most efficient form of oxygen therapy that has been developed so far. Because the device takes air from the surrounding area, you will never have to rely on an oxygen supply company to come to your home and refill your oxygen, instead you just have to recharge the batteries as you would with your cell phone or other electronics.

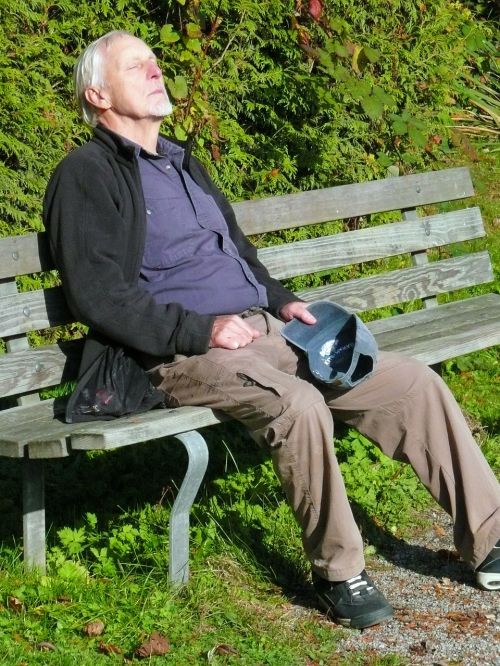
These devices are designed to be portable, so you can maintain a healthy and active lifestyle, even if you use your oxygen all day long. The pulse dose machines are typically under 6 pounds, making them easy to carry with you without getting worn out from the added weight.
The continuous flow devices range from 10-18 pounds, however these are still more portable and less restrictive than any other device like a tank or canister. The carts are durable, and the wheels are lightweight and large enough to make it through any kind of terrain. They also all fit underneath the seat in front of you when you fly, because one of the most freeing aspects of these devices is that you can fly on airplanes with them!
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Before a portable oxygen concentrator, oxygen was still readily available to people with respiratory disease.
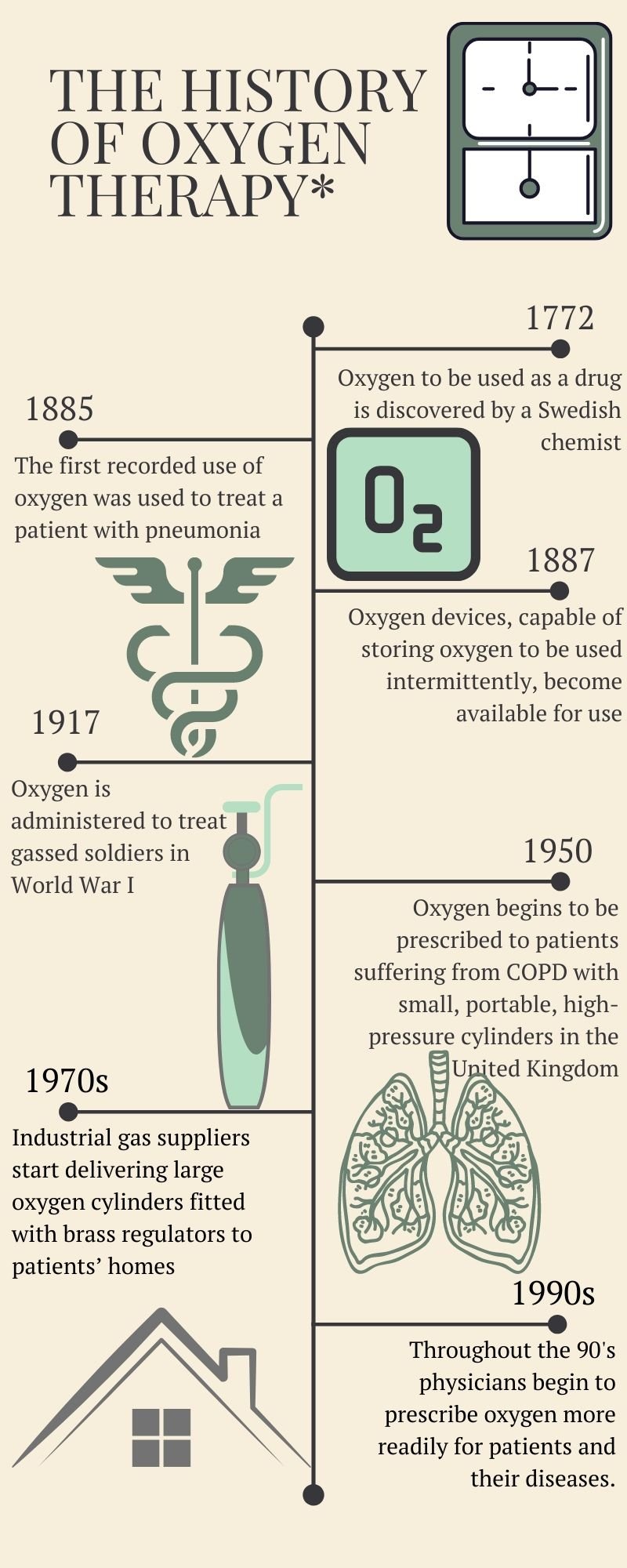
Here is the overall history of oxygen therapy:
We did it! We made it through another year!
Despite all the ups and downs of 2019, it’s time to wipe the slate clean and start over with a new year and a new decade.
And if you’re like many people, you’ve probably taken the time to brainstorm New Year’s resolutions, write them down, and even plan for how you’re going to accomplish them.
When they work as intended, resolutions can be a great way to make positive lifestyle changes and break bad habits that burdened us in the previous year.
Unfortunately, resolutions don’t always work as planned… According to a study done by the Journal of Clinical Psychology, about half of adults make New Year’s resolutions, but only about 10 percent pursue them longer than a few months.
It’s not hard to see why many people fall short of achieving their resolutions. Over time, we lose sight of what we’re trying to accomplish, and we may become overburdened by things like work, health, or other aspirations.
If you have COPD, you know that following through with your New Year’s resolutions can be challenging. Being able to accomplish your goals means having a strict COPD treatment plan that allows you to feel better and focus on things that are important to you.
In this post, we’ll discuss the importance of managing COPD symptoms if you want to follow through with your New Year’s resolutions, and how the Inogen One G5 is the perfect oxygen machine to help you do it.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Health Should Always Be a Priority
Despite what resolutions you wrote down for the year 2020, there’s nothing more important than your health and well-being. While it may seem selfish to constantly focus on your own health, even the most generous people had to help themselves before they could help others.

As a COPD patient, the disease you deal with on a daily basis impairs one of the fundamental functions of your body — breathing. It’s difficult to describe what it feels like to suffer from a chronic respiratory ailment, but many patients describe it as “suffocating while being surrounded by breathable air.”
With that being said, you have every right to focus on your own health before anything else. While it can be easy to get ahead of yourself and start planning for all the things you want to accomplish in the new year, it’s best to start with your own health, ensuring that all your basic needs are met first.
COPD is a Distraction
Another reason to focus on treating COPD is that it can be a huge distraction when you’re trying to accomplish your goals. Think of it this way:
The shortest distance between two points is a straight line. Similarly, the fastest way to accomplish a goal is to address it directly. If you have obstacles standing in your way such as COPD symptoms, you’re going to have a hard time achieving your goals.

COPD is a condition that can occupy your thoughts and affect your emotions. It’s not uncommon for people to feel anxiety or fear about their health which can be a significant distraction when it comes to setting and achieving your goals.
The Inogen One G5 is Designed for Freedom
Oxygen has been used for medical purposes for hundreds of years. However, during most of this time, medical oxygen devices were bulky, heavy, and difficult to use. This wasn’t ideal for most oxygen therapy patients because it caused them to be immobile and home-bound for much of their life.
In the early 2000s, portable oxygen concentrators became the oxygen therapy device of choice because they’re much smaller, lighter, and can be used virtually anywhere. One of the latest and most popular portable oxygen concentrators is the Inogen One G5. This oxygenator offers a long battery life, lightweight design, and a high enough oxygen output to support most oxygen patients.
.png)
COPD is a debilitating disease in many ways, but that doesn’t mean you shouldn’t have the freedom to live a normal life. The Inogen One G5 was specifically designed to keep people with COPD moving without having to worry about their health. The following are just a few of the ways the Inogen 1 G5 will eliminate barriers that prevent you from achieving your goals.
Getting More Restful Sleep
Throughout your whole life, you’ve probably had people nag you about the importance of a good night’s sleep. This can be annoying, but it couldn’t be more true! Most experts recommend 7 to 9 hours of sleep each night depending on your age. But if you’re a COPD patient, you may struggle to even get the bare minimum amount of sleep.
-jpg.jpeg)
Hypoxemia (low blood oxygen levels) are just as likely to occur when you’re asleep as when you’re awake. As a result, many oxygen patients need to be able to sleep with their oxygen therapy device. Otherwise, they may not experience the benefits of a full night’s sleep.
COPD often coexists with sleeping disorders like obstructive sleep apnea (OSA) in something called overlap syndrome. What this means is that the patient has both lung inflammation due to COPD and their airways collapse at night due to sleep apnea. In this case, it’s imperative that they have both their CPAP or BiPAP machine and their oxygen therapy device on at night.
The Inogen One G5 is compatible with CPAP and BiPAP machines meaning you’ll be able to feed oxygen directly into your CPAP mask as you sleep. It won’t interfere with the effects of the sleep apnea device and you’ll be able to experience a restful night’s sleep every night.

The Inogen One G5, like other Inogen 1 portable oxygen concentrators, is designed for 24/7 use. So, you won’t have to worry about running your device all throughout the day or turning it off once you get in bed.
According to healthfinder.gov, a full night’s sleep will boost your immune system, help you manage your weight, reduce stress, and improve your mood. All of these things are important if you want to follow through with your New Year’s resolutions.
See More and Do More
If your New Year’s resolutions involve anything physical or fitness related, you’re going to need an oxygen concentrator that matches this new lifestyle. Maybe you decided that you want to be able to walk a mile or you want to visit every state in the country. These are great resolutions to pursue, but they aren’t achievable unless you’re prepared.
The Inogen One G5 is equipped with everything you could possibly need to travel the world with your oxygen machine. It weighs in at just 4.7 pounds, making it one of the lightest oxygenators on the market. What’s more, it offers up to 13 hours of battery life on a flow setting of 1 (its lowest flow setting). This is more than enough battery to stay out all day without any problems.
The G5 is also very compact making it very easy to carry and store. Unlike oxygen tanks, the Inogen G5 oxygenator has no compressed oxygen inside it. All of the oxygen that is sent out the nasal cannula is drawn from ambient air. This means manufacturers are able to make the device very small. And with G5 accessories like the custom carrying case and the G5 backpack, you’ll have plenty of options to fit your lifestyle.

The Inogen One G5 is approved by the Federal Aviation Administration (FAA), a government organization that’s in charge of regulating safety policies for all major commercial airlines in the United States. All Inogen 1 portable oxygen concentrators are FAA-approved which means you’ll be able to carry your G5 with you on the plane. But it’s recommended that you speak with the airline a few days in advance in case you need to fill out any additional paperwork before your flight.
The Inogen One G5 is great for all other forms of transportation as well. If you enjoy taking cruises, you’ll be happy to know that the G5 will offer you the freedom to explore the ship and go on excursions without worrying about your medical oxygen. Cruise ships have electric outlets, so once you’re done enjoying your day, you can go into your cabin and charge and use your G5 all night while you sleep.

Last but certainly not least, the Inogen G5 is great for road trips and public transportation. The great thing about this day and age is that we have no shortage of options when it comes to getting around. You can take the bus, take a taxi or Uber, take the subway, or drive yourself depending on where you’re going and what your goals are. Fortunately, you can rest assured that the G5 will provide you with a reliable source of oxygen the whole time.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
With the Inogen One G5 car charging cable (DC power supply), you’ll be able to charge your portable oxygen concentrator no matter where you are. If you’re taking a road trip across the country, you can keep your G5 fully charged so that once it comes time to get out and explore, you’ll have ample battery life to keep you going.

If you’re traveling by bus, subway, or a similar form of public transportation, you need a portable oxygenator that’s small enough to take into crowded areas. The G5 is very compact at just 8.15" H x 7.19" L x 3.26" W which is almost small enough to fit in a purse or handbag. We recommend purchasing an official Inogen carrying case, however, because they’re specifically designed for the G5 by accommodating for the air intake vents on the side of the device.
Ultimately, when you have the freedom to go where you please and do anything, it’s going to be way easier to follow through with your New Year’s resolutions, especially if they involve traveling. Most oxygen patients who transition from oxygen tanks or continuous flow portable oxygen concentrators to pulse flow oxygen concentrators are amazed at what they’ve been missing out on.
Relying Less On Loved Ones
It can be really frustrating getting into a situation where you rely on friends or family members for support. But what many people don’t realize is that even if you suffer from a progressive disease like COPD, you can take steps to reduce your reliance on loved ones. This all starts with ensuring that you have the oxygen you need to stay healthy.
The Inogen One G5 has the highest oxygen output of any pulse flow POC on the market. It goes up to a setting of 6 which is the equivalent of 1260 ml/min of 90% (+6%/-3%) oxygen. This is enough oxygen for the vast majority of oxygen patients. What’s more, due to Intelligent Delivery Technology, oxygen is delivered at a precise moment during inspiration, ensuring that the device runs as efficiently as possible, day and night.
Another reason you’ll rely less on your loved ones is because the G5 doesn’t need to be refilled. Oxygen tanks and portable oxygen tanks can only hold a limited amount of oxygen, so once they run out, you either need to have a backup tank, or you need to refill it with oxygen. There are special home oxygen concentrators which can refill your tank, but many people have to visit oxygen refill stations. On the other hand, the G5 doesn’t hold oxygen. It pulls in ambient air and removes the nitrogen meaning it has an infinite supply of oxygen as long as it has battery life.

It’s not a bad thing to rely on friends and family for support. But if you notice you’re losing more and more of your freedom because you need someone by your side all day and night, you should take steps to improve your self-reliance. Not only does self-reliance allow you to live life on your own terms, but it will give you the confidence you need to follow through with your New Year’s resolutions.
Improving Peace of Mind
As a COPD patient, you know what it’s like to have a bad day. Exacerbations can occur seemingly anywhere or at any time and you never know when the next fit of breathlessness or coughing will happen. If you have an unreliable source of oxygen, this will only amplify your issues and give you one more reason to feel anxious or worried.

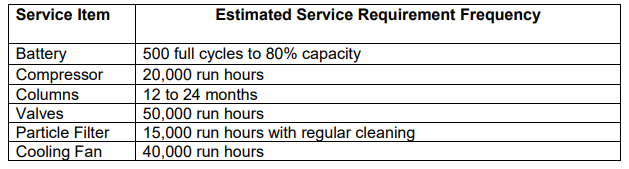
Without a doubt, Inogen produces the most reliable oxygen concentrators in the industry. Ever since its inception in the early 2000s, Inogen has produced some of the most durable medical oxygen units and they’ve only gotten better with each successive generation. The compressor in the G5 is set to last 20,000 hours and other components such as the filters can last years without being replaced. As long as you take several precautions when using your Inogen One G5, you’ll be happy to know that your unit can run 24/7 without problems.
Peace of mind is very important when it comes to achieving your New Year’s resolutions. It’s very difficult to accomplish goals if you’re feeling anxious or concerned about not receiving the oxygen you need throughout the day. You may feel unmotivated to even get out of bed in the morning because it’s better to play it safe than to risk experiencing an exacerbation.
Reducing Financial Insecurity
Financial well-being is another major concern for many COPD patients. You probably already spend a lot of money out-of-pocket on things like medication, doctor’s visits, and pulmonary rehabilitation, so adding another cost to the mix can be devastating for many respiratory patients.
You’ve probably heard Medicare or private health insurance companies refer to portable oxygen concentrators as “luxury items.” Fortunately, this couldn’t be farther from the truth. Calling them luxury items is their way of justifying their lack of coverage for these units. They’ll have you believe that portable oxygen concentrators are not necessary and that oxygen tanks are all you need.

While the upfront cost of concentrators is more than that of oxygen tanks and liquid oxygen tanks, in the long run, you will be saving a lot because you’ll never have the need to refill your unit or purchase additional tanks as “backups.” Another reason oxygen tanks are more expensive is because they usually don’t come with warranties to protect you if something breaks.
-min.png)
Financial well-being plays an important role in your ability to keep New Year’s resolutions. If you’re caught up in trying to pay the bills, you’re not going to have the time or attention to allocate towards your goals and aspirations. What’s more, if your goals require you to spend a substantial sum of money, you may not be willing to expend it. Alternatively, you’ll need to save the money to fall back on if you’re faced with more expenses.
Conclusion
At the end of the day, many respiratory patients rely on their oxygen machines. It’s the most fundamental way of treating symptoms like breathlessness, chest pain, coughing, wheezing, and more. And without a reliable medical oxygen device, COPD and cystic fibrosis patients are housebound without the freedom to live life on their own terms.
For the large majority of oxygen users, the Inogen One G5 is the best portable oxygen concentrator to both meet their needs and allow them to set and achieve goals without relying on friends or loved ones. If you’d like to learn more about what the Inogen One G5 has to offer, check out this guide. And be sure to stay tuned to our blog for the latest news on portable oxygen concentrators, home oxygen concentrators, and much more.
-png.png)
If you were to honestly ask yourself: What stops me from exercising? And your answer is that your COPD makes it too hard for you to breath, this article is for you!
If you have COPD, symptoms like difficulty breathing and muscle fatigue are most likely the main reasons you avoid from working out or beginning an exercise program in the first place. This is unfortunate because the best way to improve exercise tolerance and decrease breathlessness in COPD is to be active.
If you do not already know this, doing something active everyday is one of the best ways to treat COPD, and reduce your experience with symptoms while also slowing down the progression of your COPD, thereby adding years to your life.
If you're finding it difficult to exercise with COPD, try accomplishing some of these methods in this article to help improve your endurance and boost your energy levels, improving your well-being overall.
Talk to Your Doctor

Before getting into a new workout regime, speak with your doctor about exercise and your COPD.
It is important to review your health status and go over the specifics of your medications with your doctor. After this, your doctor may also suggest you take an exercise tolerance test (ETT). This test will measure your endurance and your overall ability to exercise.
Based on the results of your ETT your doctor should be able to help you organize an exercise program. This personalized exercise program will depend on your abilities, lung capacity, and COPD severity.
You exercise program should include a variety of stretching, strength training, and cardiovascular exercises, along with some light interval training.
A exercise program that will enhance your tolerance for physical activity

Remember the whole idea of beginning an exercise program is to build up the endurance you need to live a healthier and longer life with COPD. This means that you should start small, and do not try exercises that cause you to feel overwhelmed or exhausted.
In no time, you will begin to notice your capabilities are growing, but this will not happen overnight. Be patient and kind to yourself in the first few weeks, and your body will thank you for it!
Breathing exercises
You should practice certain breathing exercises, before performing any exercise program. Using breathing techniques while you exercise is a great way to help increase your lung capacity to be able to handle the added activity.
Breathing exercise can also be done while you are not doing any kind of exercise, because they help increase the capacity of your lungs which will also help reduce the symptoms associated with COPD.
Breathing exercise done regularly, can help make physical actives easier and more comfortable.
Breathing exercise include:
- pursed lip breathing
- coordinated breathing
- deep breathing
- huff cough
- diaphragmatic breathing
While you are exercising, always breathe slowly to save your breath. Inhale through your nose by keeping your mouth closed. This will warm up, filter, and moisturize the air you breathe in. Exhale your breath through pursed lips.
By breathing out slowly and gently through pursed lips you will develop more complete lung actions, strengthening your lungs and improving the quality of each breath you take.
Also remember, exercise will not harm your lungs, even when you experience shortness of breath during an activity, this means that your body needs more oxygen. If you slow down your breathing and concentrate on exhaling through pursed lips, you will restore oxygen to your system more rapidly, thereby makes the activity more comfortable.
Stretching and Flexibility

Stretching exercises are movements, postures, and poses that extend your muscles and ligaments. That being said, it is very important to “warm up” before you stretch. If your muscles are cold and tight, you may pull or tear muscles by stretching them out.
Think of your muscles as rubber bands, when the rubber is warm the band can continue to stretch further without tearing. If you freeze the rubber band and continue to stretch it out, it will tear or rip in half very easily.
If you consistently practice yoga and other stretching exercises where you are slowly lengthening your muscles, it will increase your range of motion and flexibility. It is a good rule of thumb to stretch before and after any cardiovascular exercises to prep your muscles for activity, thereby preventing the risk of injury, and after, to cool down and prevent muscle strain, and soreness.
Strength-Training Workouts

Strength training exercises are done by repeatedly contracting or tightening your muscles until they become tired. This can be done using weights or doing body weight exercises. With COPD, it is good to focus on doing upper-body strengthening exercises, as they are especially helpful in improving the strength of your respiratory muscles.
Also by focusing your exercise program on strength training exercises this will result in less shortness of breath, and a great substitute rather than trying to do more cardio workouts. You are likely less able to tolerate much cardio with your COPD.
Aerobic Workouts

Cardiovascular or aerobic exercises include walking, jogging, cycling, rowing, dancing, and water aerobics, all of which utilize large muscle groups to strengthen your heart and lungs. This work will improve your body’s ability to use oxygen.
These exercise will be difficult at first, especially with your COPD, however research shows that getting regular cardiovascular exercise can improve your breathing and decrease your heart rate and blood pressure.
Interval Training

During interval training, you repeat sequences of high-intensity exercise scattered with light exercise and some periods of rest.
For example, you may walk for 30 seconds, rest for 1 minute, then walk again for 1 minute, and rest for 2 minutes, and repeat the cycle for a total of 10 minutes. This training will allows you to catch your breath after more vigorous exercise.
Interval training in COPD patients is often used as part of a pulmonary rehabilitation program.
How often should you exercise if you have COPD?
The duration and the amount of exercise you need is completely dependent on your skill set. If you were always an athlete and have a higher tolerance for exercise already, you will need to exercise more frequently than someone who has never been interested in physical work outs before.
In order improve your tolerance for exercise you have to understand what you base level of physical activity is to begin with.
The frequency of your exercise program is how often you complete all of the exercises listed about. On average, to achieve maximum benefits, you should gradually work up to an exercise session lasting 20 to 30 minutes, at least 3 to 4 times a week. By exercising every other day you will be able to keep a regular exercise schedule, and by giving yourself a rest day in between, you will not get burnt out.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
How can oxygen therapy help to improve exercise tolerance?
If your health care professional has told you to use supplemental oxygen while doing activities, you should also use oxygen with exercise. Your usual oxygen flow rate (the number you set on your oxygen machine) may not be enough for you during exercise.
If you are preparing for an exercise program, speak to your doctor about the supplement oxygen requirements you have, and how to adjust you oxygen intake when you are exercising to match the recommended dose of oxygen you need for exercise.
If you do not already have a portable oxygen concentrator (POC), these little light-weight yet powerful machines are perfect for preforming any kind of physical activity.
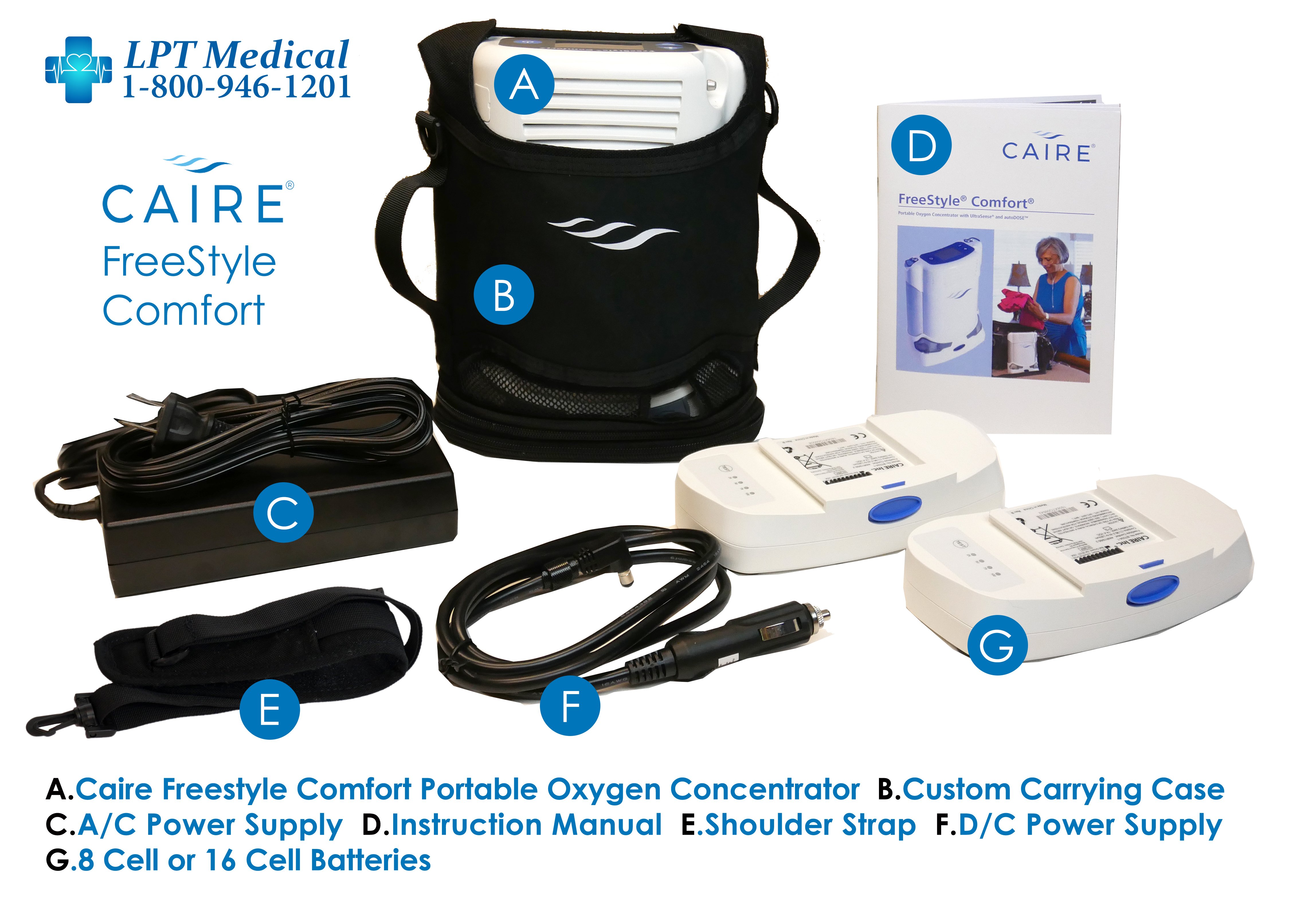
For example the Caire Freestyle Comfort Portable Oxygen Concentrator only weighs 5 pounds and can operate at a pulse flow setting from 1 to 6. If your favorite form or physical activity is walking, having a POC that can join you will only incentivize you to walk further and more often!

The Caire Freestyle has a concave side to fit around your hip when you are carrying it across your shoulder. The carrying case is open at the top, making it easy to adjust the controls and pulse flow settings at anytime.
On the lowest flow setting with the 16-cell battery, you’ll experience an astounding 16 hours of battery life! That’s 3 more hours than top-of-its-class portable oxygen concentrators like the Inogen One G5. What this means is that you’ll be able to stay out walking or exercising and about for longer without having to come back home to recharge your unit.
Speaking of the Inogen One G5, this unit is also great for exercise and physical activity. The G5 is 4.7 pounds and can be set at a pulse flow of 1-6, making it one of the most powerful but also the lightest POC on the market.

So as your breathing rate and requirements change depending on if you are laying in bed or exercising, the Inogen One G5 has the ability to satisfy your oxygen demands.
The One G5 also has extended longer-lasting battery life compared to other Inogen models, allowing you to be mobile and stay mobile for longer periods of time.
There are so many other options when it comes to selecting the best portable oxygen concentrator for your exercise requirements, as well as your daily life. In order to ensure you purchase the right unit for your lifestyle, first speak with your doctor.
Your doctor will inform you how much oxygen you need per minute (LPM or Lp/min), and the correct dose (pulse or continuous flow) of oxygen your lungs require to function properly. Your doctor will also write a prescription for supplemental oxygen which is required if you are purchasing a POC or home oxygen concentrator from a licensed distributor.
LPT Medical offers products from the most reputable manufacturers in the industry including but not limited to Inogen, Philips Respironics, Drive Medical, and more. These are the companies that are pushing the boundaries of what’s possible for patients suffering with a debilitating respiratory condition. And by offering these brands, we ensure that more people around the country have access to the most state-of-the-art oxygen therapy equipment in the world.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Stay motivated and continue to exercise
Exercise itself cannot cure or reverse COPD, but it can change the way you feel, breathe, and function.
Begin your exercise routine slowly by starting with easier exercises. Even if you think you want to push yourself and your limits, take it slow. Your muscles need to adjust to working like that!
The exercises you do should begin to get more challenging, and over time, you can walk faster for longer periods of time. Increase the amount of weight you use for strengthening exercises. And breathe better over-all. When you’ve reached the point that you’re feeling better and breathing better, keep this up every week at least three times a week.
If you are in the market for a POC, LPT medical is always here to help you find the best unit that will fit into your lifestyle and hopefully get you started or progressing further with your exercise program. To speak with a respiratory specialist call us at 1-800-946-1201.
.png)
Chronic obstructive pulmonary disease (COPD) is one of the most substantial health burdens in the world. According to the Centers for Disease Control and Prevention, “chronic lower respiratory disease” (primarily COPD) is fourth on the list of leading causes of death worldwide, behind heart disease, cancer, and unintentional accidents. And despite the fact that fewer people are smoking than ever before, experts are expecting the number of COPD cases to rise within the next 50 years.
While the vast majority of COPD cases are caused by cigarette smoking, many people are surprised to find that COPD is a diverse group of diseases that have a multitude of different causes. One of the other major causes of COPD is alpha-1 antitrypsin deficiency. This is a genetic condition that inhibits proteins that are responsible for protecting the lungs from inflammation and long-term damage. Other factors such as air pollution, irritants, and chemicals can contribute to the onset of COPD. However, these are more commonly associated with interstitial lung disease (ILD).
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
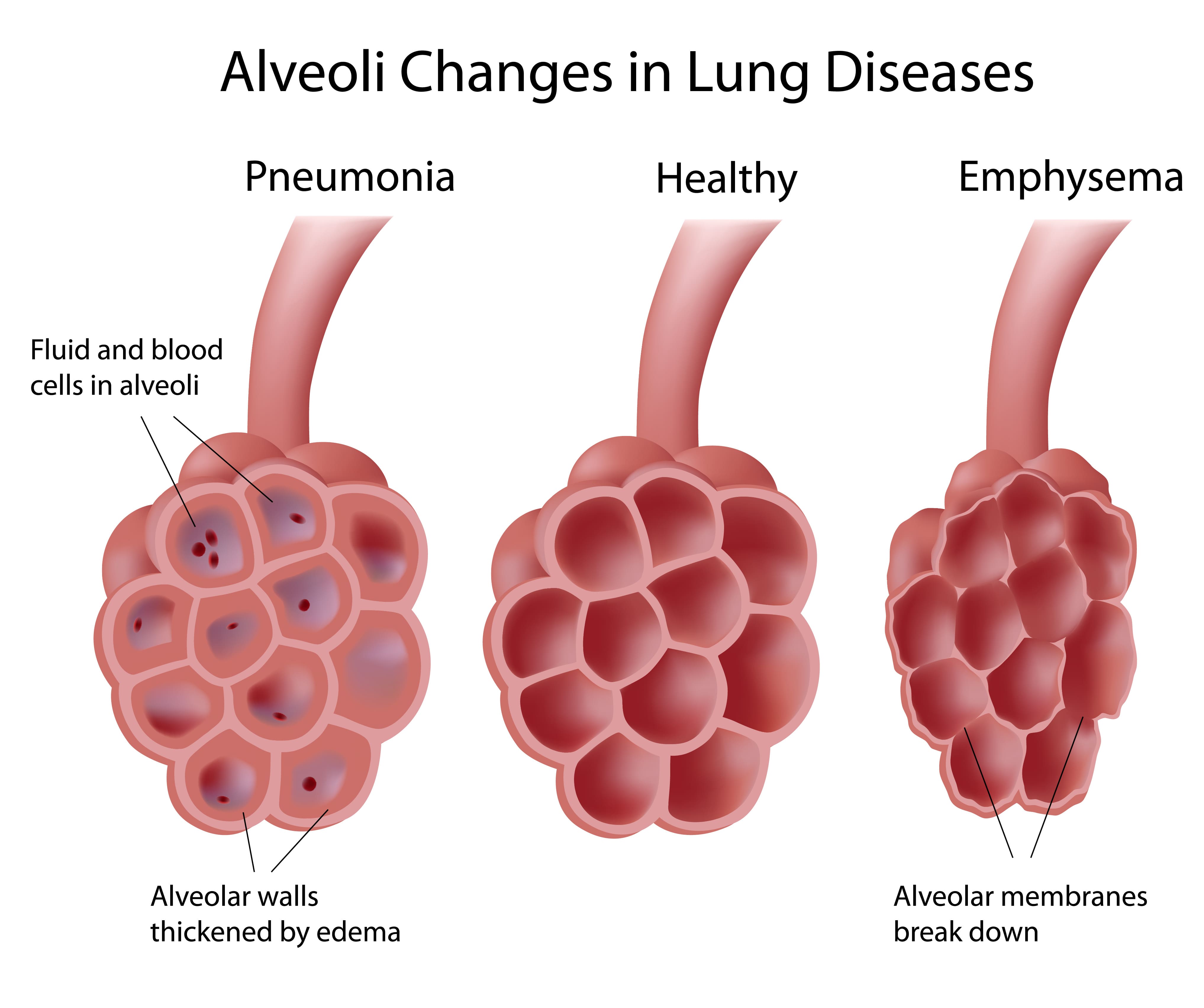
COPD is divided into two different types: chronic bronchitis and emphysema. Bronchitis affects the airways and emphysema affects the lungs. Many COPD patients have both of these diseases simultaneously but it is possible for someone to contract one without the other. And while many people think of emphysema as one disease, it’s actually divided into three different morphological categories. Depending on which one you have, you may require different treatments to manage your symptoms effectively.
In the following sections, we will provide you with an overview of emphysema as well as the three different subtypes. If you have any questions, don’t hesitate to reach out to us by leaving a comment or contacting us by phone or email.
What is Emphysema?
Emphysema is a condition that’s caused by the deterioration of lung function due to the loss of lung elasticity and the deterioration of the alveolar walls. The alveoli are tiny air sacs located at the end of the bronchioles, the small airways that lead into the lungs. There are around 300 to 500 million alveoli in the lungs, and they’re microscopic, so they’re extremely sensitive to foreign substances like cigarette smoke, chemicals, and air pollution.
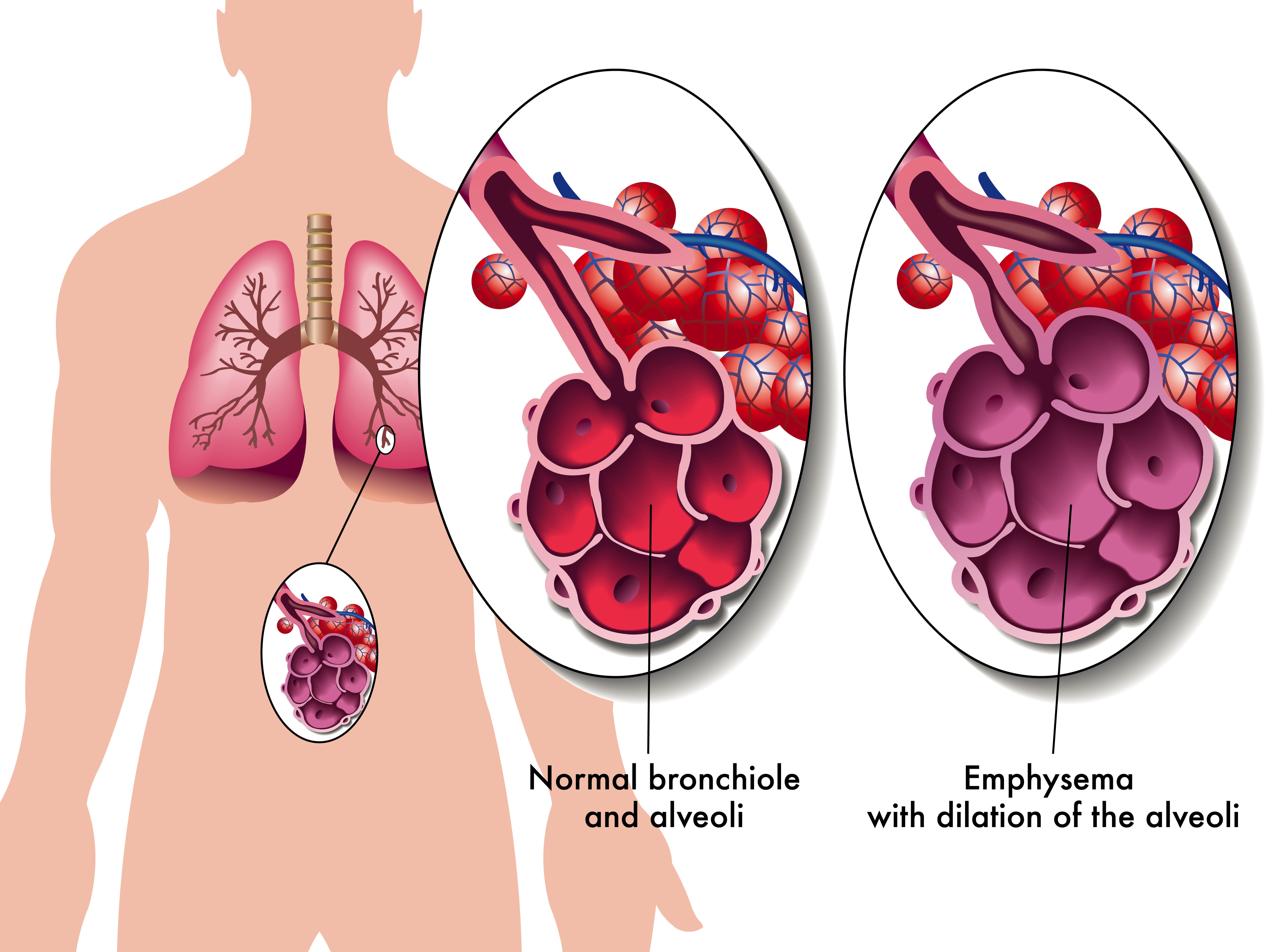
The alveoli play a vital role in the respiratory system because they transfer oxygen from the air that you breathe into the bloodstream. They also remove carbon dioxide from the bloodstream and send it back out of the lungs. This process is called diffusion and it is one of three processes that your lungs perform. Unfortunately, due to how complex the respiratory system is, if the process of diffusion is impaired, this can cause a lot of problems for the other two processes of the respiratory system: ventilation and perfusion.
Not only do alveoli transfer oxygen and carbon dioxide to and from the blood, but they’re also responsible for the spongy and elastic consistency of the lungs. As the walls of the alveoli break down, the elasticity of the lungs is lost and they become less efficient at absorbing air. Another issue this can cause is stagnant air that gets trapped in diseased areas of the lungs which can significantly increase the energy it takes to breathe and result in hyperinflation of the lungs. This also gives emphysema patients their “barrel-chested” appearance which is so often associated with the disease.
What Types of Emphysema Are There?
There are three types of emphysema that differ in terms of what causes them and the area of the lungs that are affected. Depending on which type of emphysema you’re diagnosed with, your doctor may have drastically different treatment options. No two cases of COPD are the same so your physician will work with you to determine what treatment will benefit you most.
Centriacinar Emphysema
Centriacinar emphysema (also called centrilobular emphysema) is a condition that affects the upper lobes of the lungs. Most often this type of emphysema starts in the middle of the lungs and progresses outwards. Centrilobular emphysema is almost always caused by smoking and second-hand smoke and it’s more common in people who’ve been diagnosed with coal workers’ pneumoconiosis (CWP) in the past.

Panacinar Emphysema
Panacinar emphysema (also called panlobular emphysema) is a condition that affects the entire acinus distal to the respiratory bronchioles. The acinus refers to the area at the end of the bronchioles and includes the alveolar ducts, alveolar sacs, and alveoli. It differs from centrilobular because it’s usually located in the lower parts of the lungs. Panacinar emphysema is most commonly caused by homozygous alpha-1 antitrypsin deficiency.
Alpha-1 antitrypsin deficiency (A1AD) is a hereditary disorder that causes low levels of the protein alpha-1 antitrypsin (A1AT) in the blood. This protein is made and released from the liver and it protects tissues in the lungs from being attacked by its own enzymes. A1AD patients may either experience abnormal proteins, poor production of these proteins, or both. All things considered, A1AD is a rare disease and it only amounts to a small percentage of the people diagnosed with COPD.
Paraseptal Emphysema
The third and final morphological subtype of pulmonary emphysema is called paraseptal emphysema. This type is usually localized around the septae or pleura in the lungs. This is a thin sheet of tissue that’s located around the outside of the lungs and inside the chest cavity. This type of emphysema is commonly associated with prior lung infections.
What are the Causes and Risk Factors of Emphysema?
Causes
Cigarette Smoking
Smoking is the most considerable cause of emphysema and all conditions under the umbrella term “COPD.” According to the Centers for Disease Control and Prevention (CDC), 80 percent of people with COPD have smoked in the past or are current smokers. Additionally, 38 percent of people who live with COPD continue to smoke. Despite these facts, only about 10 to 15 percent of smokers will develop some form of COPD. Smoking is more likely to cause cancer, heart disease, stroke, diabetes, and other chronic illnesses.

According to the Cleveland Clinic, the greatest predictor for someone developing emphysema from smoking is not whether or not they were a “light” or “heavy” smoker, it’s how long they smoked for — the longer someone smokes, the more likely they are to contract COPD. This is why doctors will always recommend immediate smoking cessation rather than simply “cutting back” on cigarettes.
Secondhand Smoke
Secondhand smoke refers to the inhalation of cigarette smoke involuntarily as a result of someone else smoking. While there is a commonly held belief that secondhand smoke is worse than actually smoking, this is not the case. The toxicology of tobacco smoke is the same regardless of whether it was inhaled intentionally or not. Either way, cigarette smoke in any form can cause COPD and emphysema.

It’s estimated that there are over 7,000 chemicals in cigarette smoke and smoke can linger in the air for several hours. In other words, living with a smoker or being in an area where someone has smoked recently will put you at a higher risk of chronic lung disease. Cigarette smoke dissipates more quickly outdoors so, generally speaking, it’s safer to be outside.
Air Pollution
Air pollution is a major contributor to the onset and progression of emphysema. According to the World Health Organization (WHO), there are five major types of air pollution: particulate matter, ground-level ozone, nitrogen dioxide, sulfur dioxide, and carbon monoxide. All of which can be inhaled into the lungs and cause permanent damage to the bronchioles and alveoli. Just like with cigarette smoking, the more you’re exposed to air pollution, the more likely it is to cause permanent damage to your lungs.
![]()
One great tool to help you learn about the air pollution in your area is AirNow.gov. All you have to do is enter your city or zip code and it will provide you a number between 0 and 500 with 0 being the least polluted and 500 being the most polluted. The EPA recommends that you should not go outside if the Air Quality Index (AQI) is above 150. However, if you already have a chronic lung disease like asthma or COPD, you should avoid going outside if the AQI is above 100.
What are the Four Stages of Emphysema?
Much like other chronic illnesses that take many years to progress, emphysema is broken down into different “stages” which medical professionals can use to identify the severity of your disease. Since early-stage emphysema has very mild symptoms, it’s often underdiagnosed or misdiagnosed as other chronic lung conditions such as asthma. Read below to learn about the four stages of emphysema.

Stage 1
Stage 1 emphysema is very mild. In fact, it’s often so mild that it is undetected and undiagnosed. People with stage 1 may experience a cough, minor chest pain, and some breathlessness. Stage 1 emphysema patients have a forced expiratory volume in one second (FEV1) of 80% or more.
Stage 2
Stage 2 is slightly more advanced than stage 1. This is when many people start to see their doctor because they begin to realize that their respiratory symptoms aren’t the result of aging or an acute condition. Stage 2 emphysema patients have an FEV1 between 50% and 80%.
Stage 3
By the time someone reaches stage 3 they have most likely received a diagnosis from their doctor. They’ve likely had several flare-ups in the past year and have been admitted to the hospital at least once. Stage 3 patients have an FEV1 between 30% and 50%.
Stage 4
Also known as “end-stage COPD,” this stage is characterized by severe breathlessness, coughing, wheezing, and fatigue which leads to exacerbations and hospitalization. Stage 4 patients have an FEV1 of less than 30%.
How is Emphysema Treated?
Supplemental Oxygen Therapy
Because emphysema can result in low blood oxygen levels (hypoxia) supplemental oxygen can be used to stabilize a patient’s oxygen levels and help alleviate emphysema symptoms like breathlessness, chest pain, and coughing. However, it’s important to note that oxygen therapy can be dangerous if it’s not used in the way that your doctor intends for you to use it. Oxygen is a controlled substance in the United States, so you’ll need a prescription in order to rent or buy an oxygen device.

There are many choices to consider when it comes to oxygen delivery devices so you’ll need to find one that best suits your needs and your lifestyle. Oxygen tanks are a very popular choice because they have a low upfront cost. However, they’re very heavy and need to be refilled constantly making them a poor choice for most oxygen users. Liquid oxygen tanks are an upgrade because they last longer and aren’t as heavy, but they cost more to maintain.

The best alternative to both of these is portable oxygen concentrators. An oxygen concentrator is an electronic device that takes in ambient air and removes nitrogen, argon, and other gases, then puts out medical-grade oxygen. The benefit of this is that you simply need to charge the batteries on your concentrator which is much more convenient than having to have an oxygen company fill your tanks.
Pulmonary Rehabilitation
Many years ago, exercise was not recommended for COPD patients because it was believed to exacerbate symptoms and increase the rate at which the disease progressed. However, in this day and age, pulmonary rehabilitation (exercise that’s focused on lung function) is championed as one of the best ways to treat chronic respiratory illness. This is due to a mounting body of evidence that shows even moderate exercise can improve COPD symptoms.

While you can exercise at home on your own time, it’s recommended that you start with a pulmonary rehabilitation program. Not only do these programs teach you how to exercise with emphysema, but they will also teach you important information about your disease and how it should best be managed. Read this post to learn more about how pulmonary rehabilitation works.
Dietary Changes
If you live by the motto “you are what you eat,” you probably understand the importance of a healthy, well-balanced diet. Nutrition affects everything from your heart health to your lung health and everything in between, so it’s wise to follow your doctor’s instructions on eating healthier meals. According to Lung.org, the metabolism of carbohydrates creates the most carbon dioxide, so they should opt for healthy fats instead which produce the lowest amount of carbon dioxide. HIgh-protein diets are also good for emphysema patients because they keep your lungs strong and efficient.
![]()
Medication
Emphysema treatment usually involves some combination of oral and inhaled medication. Oral steroids can provide you with short- or long-acting relief from your symptoms whereas inhaled medication like bronchodilators are designed to open up your airways quickly in the event of a COPD exacerbation. Your doctor will discuss with you exactly which medications you will need and when to use them.

Most oxygen patients are prescribed inhalers, nebulizers, or both. An inhaler is a portable device that administers medication in a mist form called “aerosol.” this enables the patient to administer the medication directly to their lungs thus allowing it to take effect more quickly. Nebulizers play a similar role in an emphysema treatment plan but they administer medication in a stream rather than a “puff” making them easier to use for most people.
Lifestyle Changes
There are many other lifestyle changes that you can make to treat emphysema and alleviate your symptoms. Focusing on getting more consistent and restful sleep is one way that you can feel more alert and prepared to take on the challenges of your disease. Ultimately, you should discuss your sleeping habits with your doctor to ensure that you’re doing everything you can to get a good night’s sleep.
![]()
Another lifestyle change you can make is changing your cleaning habits. Many common household cleaners are filled with dangerous chemicals like bleach and ammonia. When these substances are inhaled they can cause COPD exacerbation which leads to increased coughing, wheezing, and shortness of breath.
Conclusion
COPD is one of the most preventable chronic illnesses in the world and emphysema is one disease under this umbrella term. Emphysema patients experience impaired lung function due to a breaking down of the alveoli, or tiny sacs in the lungs that transfer oxygen and carbon dioxide to and from the blood. While there is no cure for emphysema, patients can experience significant relief and improved life expectancy with a carefully planned treatment routine.
Here at LPT Medical, we want COPD patients to experience relief from their respiratory symptoms while experiencing the freedom and independence they had before being diagnosed. If you haven’t done so already, ask your doctor if you might benefit from using a portable oxygen concentrator like the Inogen One G5 or the Caire FreeStyle Comfort. Both of these machines have a high oxygen output, they’re lightweight and easy to carry.
%20(1).png)
When we’re younger, we often take for granted our ability to get around with ease. Whether it’s a trip to the grocery store once a week or a month-long trip across the country, there are very few physical limitations setting us back. But as we get older, tasks that used to be second nature to us now become strenuous exercise. This is further complicated by the fact that older adults are more likely to suffer from chronic conditions like osteoarthritis, heart disease, and chronic obstructive pulmonary disease (COPD), all of which are debilitating.
According to Healthline, COPD is most commonly diagnosed in people over 40 years of age. However, the age groups that are most affected by COPD are women between the ages of 65 and 74 and men between the ages of 75 and 84. This is when people tend to struggle the most with mobility because the effects of aging begin to mix with the later stages of the disease. But despite the struggles these patients face, it is possible to regain a significant portion of the mobility that they lost.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
While every case of COPD is different, treatment is usually focused on pulmonary rehabilitation, which is essentially an exercise routine that’s focused on lung strength and education; a refined diet with an emphasis on protein and healthy fats; and finally, supplemental oxygen therapy which is designed to reduce the physical burden on the lungs and maintain blood oxygen levels which leads to improved systemic health.

If you’ve gone ahead and purchased a Caire FreeStyle Comfort, one of the lightest and most powerful portable oxygen concentrators on the market, you’re likely looking to enjoy your newfound freedom by taking a trip of some kind. Since the FreeStyle Comfort is approved by the Federal Aviation Administration (FAA), you’ll be able to fly anywhere in the country or worldwide with your new concentrator. In this post, we’ll go over 7 must-know tips before you travel with your Caire FreeStyle Comfort.
Speak With Your Doctor
Whether you’re taking a flight or a road trip, you should speak with your doctor before you even begin planning. Your doctor will not only provide you with advice on using your oxygen concentrator away from home but he/she will also make sure you understand all other facets of your treatment plan like your diet, pulmonary rehabilitation, and sleep schedule. Be sure to write down any questions you may have before you go in for a doctor’s visit.

Easily the biggest problem many COPD patients face when traveling is falling back or cheating on their new diet. Since your diet is inextricably linked to your lung health, making poor dietary choices can be devastating. Since most people tend to be “on the go” when they’re on vacation, they usually opt for simple snacks or fast food which are usually high in sodium, sugar, and unhealthy fats instead of protein and healthy fats like your COPD diet entails. This can put you at higher risk for exacerbations while you’re away from home.
Another aspect of your COPD treatment plan that might get neglected while you’re traveling is your exercise routine. It can be difficult to find the time to set aside time for important exercises that can boost your strength and improve endurance so your doctor may set you up with a special routine. On the other hand, if you’re going to be up and moving a lot anyways, your doctor may tell you not to worry about pulmonary rehab while you’re gone.
Lastly, you should consult your doctor for information about using your oxygen concentrator while away from home. He/she may have advice for you on adjusting your flow setting based on whether you’re sitting or walking. This way you can conserve battery life and experience more freedom during your trip.
Skim Through Your User Manual
There’s no doubt about it, the Caire FreeStyle Comfort is one of the easiest portable oxygen concentrators on the market to use. There are just three buttons on the user interface: two to control the flow setting up or down and one to turn the device on or off. While you’ll likely get the hang of using this concentrator almost immediately, it’s still a good idea to read the user manual in order to understand its more advanced features.
.jpg)
The user manual will help you get better acquainted with the various audio and visual alarms on the device. For example, there is a symbol when your battery life is getting low or if there is some type of malfunction. By learning these symbols, you won’t have to stress about them while you’re on vacation trying to enjoy yourself. Also, take some time to read through the “troubleshooting” section so that you can fix minor errors on your own while you’re away from home.
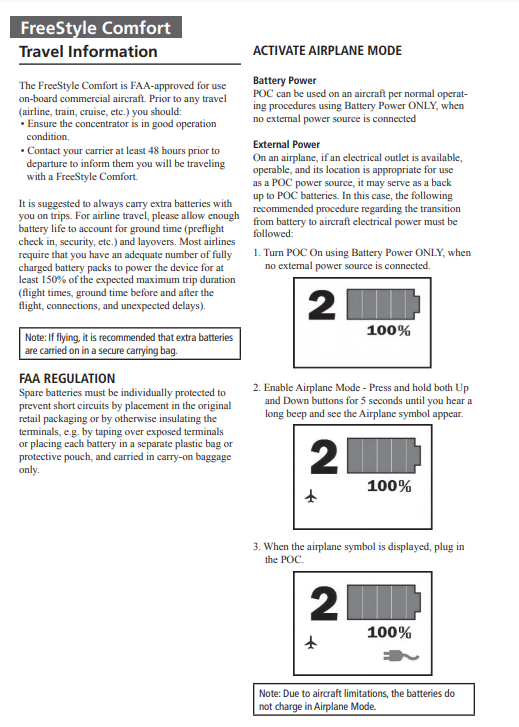
Another section of the Caire FreeStyle Comfort manual that you should pay special attention to is the one titled “Travel Information.” By reading this, you’ll learn some helpful tips for using your portable oxygen concentrator while on a flight including how to put it into airplane mode.
Pack Extra Batteries
Despite the Caire FreeStyle Comfort offering the longest battery life of any pulse dose portable oxygen concentrator on the market, it’s still a good idea to bring extra batteries with you when you travel. With an additional small 8-cell battery for the FreeStyle Comfort, you can double the battery life of your device and only add a small amount of weight. You can even upgrade to a large 16-cell battery and you’ll still be carrying less weight than most portable oxygen concentrators out there.

Another great advantage of these batteries is that they don’t take up very much space. You can easily fit several of them in your backpack or purse while still having room for other personal belongings like your keys or wallet. This is in stark contrast to oxygen tanks which take up significantly more space, not to mention the fact that they’re awkwardly shaped making it difficult to fit them in storage.
Other Accessories to Pack
Aside from extra batteries, there are a lot of other accessories out there for the Caire FreeStyle Comfort that you should consider taking on a trip. First and foremost, you need the AC charging cable. This accessory comes with every FreeStyle Comfort package and allows you to charge your device with any electrical wall outlet. If you’re traveling to another country, be sure to get an adapter to ensure you are able to charge your POC wherever you go.

Secondly, you will need a DC charging cable. This is similar to an AC charging cable but it allows you to charge your Caire FreeStyle Comfort in any car cigarette outlet. Most people don’t realize this, but you’re actually able to use your POC while it’s charging in the car. So, if you’re taking a long road trip you’ll always have a full battery. If you want to get out and stretch your legs or do some sightseeing, you’ll have peace of mind that you have a full battery to work with.

Last but certainly not least, you’re going to want to purchase and bring an external battery charger with you. Normally, you need to have a battery attached to your concentrator in order to charge it, but the external battery charger allows you to charge the battery when it’s not attached. In other words, you’ll be able to charge two batteries at the same time. This is perfect for people who are on-the-go a lot and don’t have much downtime.

For example, if you’re going back to the hotel for an hour or two, the external battery charger will let you charge your batteries much more quickly allowing you have more freedom once you leave. You can also charge two batteries overnight without having to wake up and swap out the batteries on your concentrator.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Learn About CAIREview™ Telehealth Technology
One of the most unique features of the Caire FreeStyle Comfort is its telehealth technology. Telehealth is a practice that’s progressing very quickly in this day and age. Essentially, it means health care professionals providing patients with services over long distances by taking advantage of video communication and other technologies. The Caire FreeStyle Comfort has its own built-in telehealth technology called CAIREview.
CAIREview is an advanced and cost-effective tracking solution that will help you better understand how you’re using oxygen and how you can improve your treatment. This information can also be shared remotely with your provider who can help you make changes to your routine. What’s more, you can rest assured that this is all done over a secure network that doesn’t share any personal information unrelated to your oxygen usage. To get started, you’ll simply need to install the CAIREview application and connect it wirelessly to your POC.
Decide How You Will Carry Your Device
The way you carry your oxygen device can make a huge difference when it comes to your ability to get around while you’re on vacation. For example, oxygen tanks are so heavy and bulky that the only way to carry them is with a rolling cart. This is not ideal because it can make it very difficult to get up a flight of stairs or move through crowded areas without bumping into people.

If you have a Caire FreeStyle Comfort, however, you will have many different options for how you transport it. Most people choose to use the custom carrying case that comes with the device because it can easily be swung over your shoulder and kept close to your side. The FreeStyle Comfort has an ergonomic curve design to keep it from sliding back and forth as you walk and you’ll have easy access to all the controls on the top of the device.
Another carrying option available to you is the FreeStyle Comfort backpack. With the backpack, you’ll have plenty of extra room to carry things like your keys, wallet, water bottle, or any other supplies you need for traveling. Some people find it more comfortable to carry their POC on their back because it spreads the weight between their shoulders, preventing back pain or soreness. However, it will always come down to your personal preference and what you’re trying to accomplish.

One final way you can carry your oxygen device is with a mobility aid like a wheelchair or rolling walker. Mobility aids are best for older COPD patients who are struggling to get around on their own. If you use a wheelchair, you can hang the concentrator over the back of the chair. Just be sure that there is no slack in the oxygen tubing so it doesn’t get caught on a wheel. Most walkers or “rollators” as they’re often called have a seat that can be used to rest your concentrator on as you walk.
Contact Your Airline Ahead of Time
While the FreeStyle Comfort is approved for all commercial airlines in the United States, you’ll still need to contact your airline of choice 48 hours before your flight. This is because they may have paperwork that you need to fill out about your respiratory condition or your oxygen usage before you can fly. Once you actually arrive at the airport you should also check in with the receptionist at your gate to make sure they’re aware of your oxygen usage. This is just to make sure that there isn’t any confusion or holdups before you have to get on the plane.
.jpg)
Another policy many airlines have is that you need to have 150% of the duration of the trip in battery life. Delays and malfunctions are not uncommon in the airline industry so they simply want to make sure you’re covered in the event that there is a delay. Make sure that you charge some extra batteries the night before you leave and have them in your carry-on bags ready to go.
Conclusion
Supplemental oxygen therapy is one of the most important aspects of a COPD treatment plan. As such, it’s important to be very well prepared before you travel with an oxygen concentrator. This means knowing when to use oxygen, what flow setting to use, as well as following all other aspects of your COPD treatment such as your diet, exercise routine, and sleep schedule.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Fortunately, travel is made a lot easier with a powerful pulse dose portable oxygen concentrator like the Caire FreeStyle Comfort. This POC weighs in at just 5 pounds with the single battery and only 6 pounds with the double battery, it offers up to 16 hours of battery life on a flow setting of 1, and it has a maximum oxygen output of 1,050 ml/min or a flow setting of 5. These are the best specs of any oxygen concentrator on the market, so it’s no wonder that so many people have bought one.

While the Caire FreeStyle Comfort is the best POC for the greatest number of people, we here at LPT Medical understand that everyone has different needs. If you have higher oxygen demands than what the FreeStyle Comfort is able to provide, we are here to help you find exactly what you need. We offer a wide range of continuous flow portable oxygen concentrators such as the Respironics SimplyGo or the Oxlife Independence, as while as a host of stationary oxygen concentrators including the Respironics EverFlo Q and the Inogen at Home.
If you have any questions, please don’t hesitate to contact us by phone or email.
.png)
Whether you have a friend or a loved one with COPD or you have COPD yourself, you can likely attest to the fact that this disease can cause significant problems with mobility. The top causes of mobility issues in COPD patients include poor pulmonary function, leg swelling (peripheral edema), and loss of muscle mass (muscle atrophy). Combined with the effects of aging and other chronic conditions like osteoarthritis, COPD patients can experience a lot of difficulties getting around in their day-to-day life.
Aside from supplemental oxygen therapy, a healthy diet, and pulmonary rehabilitation, another thing that can help you get around are mobility aids. A mobility aid is a device that’s used to help older people and people with chronic conditions walk more easily. They’re often designed to improve balance, reduce physical load, and in COPD patients, they can even help to prevent exacerbations and flare-ups. There is a huge variety of mobility aids and you’re not just limited to choosing one or the other.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’ll help you better understand the mobility options available to you as well as some other helpful information that will help you maintain your mobility as a COPD patient. As always, if you have any questions, please be sure to address them in the comment section or consult your doctor for more specific information pertaining to your disease and treatment plan.
Why Are Mobility Aids Important for COPD Patients?
According to an article published in the National Center for Biotechnology Information, balance deficit is a common issue among COPD patients. COPD is a progressive disease meaning it becomes worse over time. And as symptoms like breathlessness, chronic fatigue, and chest pain progress, so do issues related to balance and mobility. Believe it or not, studies have shown that COPD is one of the chronic illnesses with the highest rate of falls next to osteoarthritis.
Several months ago, we wrote an article discussing a common complication of COPD called peripheral edema. In short, this is a condition where your legs or feet begin to swell due to a buildup of fluid. One of the root causes of this condition is pulmonary hypertension or high blood pressure in the lungs. High blood pressure in the lungs puts more strain on the heart and prevents oxygen-rich blood from circulating to organs like the liver and kidneys. Since these organs are responsible for removing fluids from the body, swelling of the feet or legs are usually a sign of this happening.
While peripheral edema is a complex condition, it’s one of the issues contributing to the high risk of falls in COPD patients. As the disease progresses, COPD patients don’t just have to deal with increased respiratory symptoms, they have to deal with complications that can result from their disease. Someone with peripheral edema may not even realize they have it because it often comes on slowly and doesn’t cause any pain.
-jpg.jpeg)
Another issue contributing to the high rate of falls in COPD patients is muscle atrophy. In other words, as COPD progresses, patients tend to lose muscle mass from a variety of issues like a changed diet and reduced physical activity. Similar to peripheral edema, a patient may not realize that they are losing muscle mass until they experience a fall. This is why pulmonary rehabilitation is such an important part of any COPD treatment plan.
One final problem that can contribute to the fall rate in COPD is an exacerbation. An exacerbation is an event where respiratory symptoms suddenly worsen. According to COPD.com, the most common cause of exacerbation is a bacterial infection, but air pollution is another common cause. COPD exacerbations can lead to problems walking, balance issues, chest pain, headaches, and confusion, all of which can increase your risk of falls.

While mobility aids are not a replacement for your treatment plan, they play a crucial role in preventing falls, especially in people with late-stage COPD where the disease is the least predictable. Mobility aids don’t need to be prescribed by your doctor so it’s up to you and your loved ones to determine whether you need one or not. Continue reading to learn about some of the mobility options available to COPD patients.
Canes
Walking canes are the oldest type of mobility aid and they’re also one of the simplest. Most walking canes are made of wood or a light metal material meaning they’re easy to carry despite your level of physical impairment. Canes are also widely accessible, and you can buy them just about anywhere, or you could even make your own if you have time. Walking canes are great for taking weight off your joints and providing you with a little extra stability as you walk.

The key to improving your mobility with a cane is to get one that’s the appropriate size. While there is no hard and fast rule as to how you should choose a cane, it should be long enough that you aren’t bending over and straining your back in order to use it and it should be short enough that you can actually lean on it. For most people, this will be somewhere around their hip bone. Luckily, most modern canes are adjustable, so you’ll probably be safe buying one online rather than shopping around for one.

One thing to consider if you want to use a cane is how you will carry your supplemental oxygen device. If you have an oxygen tank and you wheel it behind you using a rolling cart, a walking cane might not be the best option for you because you won’t have any hands free to catch yourself if you fall. A cane is a better option if you carry your oxygen device on your back because it will help you keep a good posture as you walk.
Walkers
Walkers are another mobility option available to COPD patients. There are several different types including traditional walkers, two-wheel walkers, and four-wheel walkers. Traditional walkers tend to be a poor choice for most COPD patients because they need to be picked up as you walk which can be strenuous on your shoulders, arms, and back. Two-wheel walkers provide a little more mobility by allowing you to push the walker rather than lift it. However, for most people, four-wheel walkers, or “rollators” as they’re often called, will be the best option.

Modern rollators are more advanced than other types of walkers because they offer four swivel wheels that afford you more control. They also offer a braking system that’s controlled by two levers on the handlebars on either side of the device. They also provide a padded platform in the middle that you can either sit on or rest your oxygen device, purse, or handbag on as you walk. Some rollators even have a basket in front for added storage.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s a good idea to speak with a mobility aid expert if you want to get a rollator. Since these devices are so popular, there are many different versions and brands available to choose from. What’s more, it’s easier to use one if you’ve been shown how to do so by someone who’s experienced with them. You’ll also need to have one fitted unless you can find one that’s adjustable.
Wheelchairs
When you think of a mobility aid, chances are, wheelchairs are the first thing that comes to mind. They’re commonly used by people who are permanently disabled, but how do they fare when it comes to someone with limited mobility? The answer ultimately depends on your individual circumstances. COPD patients with poor upper body strength may find it difficult to get around in a manual wheelchair, but if you have a caretaker or loved one who can push you around it shouldn’t be a problem.

Another option for you are motorized wheelchairs or “power wheelchairs” as they’re often called. The benefit of investing in a power wheelchair is that you will have the same mobility as a manual wheelchair, but you won’t have to push it with your arms. Power wheelchairs have a joystick that you use to move in any direction. They’re not overly complicated to operate but they can be difficult to transport and you’ll need to keep it charged if you want to stay out of the house for extended periods of time.
Scooters
Mobility scooters are similar to power wheelchairs but they differ in terms of their design. Unlike power wheelchairs which use a joystick, scooters are controlled with handlebars similar to a bike. Scooters can either have three or four wheels depending on what your preferences are. They also have baskets on the front that you can use to store things like your portable oxygen concentrator, a purse, or other personal belongings. Since there are so many options available when it comes to mobility scooters, it’s important to speak with an expert who can align you with the exact product you’re looking for.

Stairlifts
Stairlifts are a mobility aid that many people have never heard of, but they’re incredibly useful. Essentially, a stairlift is a chair that moves up and down a rail that’s installed on a flight of stairs in your home. The chair has a built-in motor that can be controlled with a joystick on the handlebars. This allows you to navigate the stairs in your home without the risk of experiencing a dangerous fall. The one downside to stairlifts is that they can be very expensive and many people can’t justify spending the money to have one installed in their home.

Surprisingly, stairlifts are extremely versatile and can be installed on most staircases regardless of their size or shape. What’s more, if you like to get outside, there are specially designed stairlifts that can be installed on outdoor staircases. They can be installed in several hours so you won’t have to wait days or weeks to start using them.
Will Medicare Pay for a Mobility Aid?
Whenever it comes to medical equipment, questions about health insurance and Medicare are sure to follow. And while it would be nice if Medicare paid for medical expenses like you’d expect them to, it’s never that simple. More often than not, they will cut corners providing you coverage for mobility aids and find any way they can to offer you the bare minimum rather than what you deserve.

In short, Medicare will provide some compensation for manual or power wheelchairs and scooters. Mobility devices like these are covered under Medicare Part B and it is classified as durable medical equipment (DME) the same as oxygen tanks and portable oxygen concentrators. But it’s important to note that not all devices are covered. Medicare has a list of devices that are covered, and some of them require prior authorization. So, it’s best to consult with both the mobility aid supplier and a Medicare representative before you make any decisions.
.jpg)
Another thing to note is that Medicare has a long list of prerequisites that you need to meet in order to qualify for compensation. First and foremost, the doctor that has prescribed you with COPD and the mobility aid supply company needs to be enrolled in Medicare. Additionally, you’ll need a written order from your doctor stating that you have a medical need for a mobility aid. For a full list of requirements, refer to the wheelchair and scooter benefit page of Medicare Part B.
Get a Handicap Parking Permit
Once you have your mobility aid of choice, you may want to consider getting a handicap parking permit. This permit will allow you to park in any handicap spot in the country making it much easier for you to get around. This is especially useful for people who are using electric scooters or power wheelchairs because you won’t have room to unload it in a standard parking spot.

In order to get a handicap parking permit, you’ll need to apply at your local Department of Motor Vehicles (DMV). Every state has different policies but you’ll likely have to provide a doctor’s note which outlines your lung condition and symptoms. You’re more likely to get approved if you can prove that you use an electric scooter or power wheelchair as opposed to a cane or walker so it’s best to put time into finding a mobility aid first.
.jpg)
Last but not least, if you’re given the option between a handicap sticker that goes on your car or a placard that you hang on the mirror, always go with the placard. This is because you can transfer these to any car that you’re in whether it belongs to a family member or friend. Be aware that it is illegal for them to use the placard without you actually being present and most states require you to be recertified for your handicap permit every couple of years.
Conclusion
Making the decision to use a mobility aid is an important step for many COPD patients. People with chronic respiratory conditions are at a higher risk of experiencing falls than the general public, but mobility aids will help to support your balance whether you’re inside or outside the home. Unfortunately, there is no one-size-fits-all solution. Everyone has their own needs and preferences so you should consider all options available to you.
Canes and walkers are a good place to start because they’re affordable and they’re easy to carry. However, you may want to consider a more long-term solution like a mobility scooter or power wheelchair. These devices are generally safe and easy to use, and they will make it easy to carry around your oxygen devices such as your oxygen tank, liquid oxygen tank, or portable oxygen concentrator.
Lastly, you should check with your health insurance to see if your mobility device is covered. This could save you hundreds if not thousands of dollars. You can also file for disability and receive a handicap parking permit which will afford you more convenience and freedom whenever you leave the house. In the meantime, if you’re looking for a lightweight and easy-to-use portable oxygen concentrators such as the Caire FreeStyle Comfort or the Inogen One G5, don’t hesitate to reach out to your respiratory specialists here at LPT Medical.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!