If you live with COPD, asthma, or a similar chronic condition, it can sometimes feel like you’re walking on eggshells. These diseases cause the lungs, airways, and other areas of the body to become very sensitive to “triggers” like air pollution, infection, injury, and more. In certain situations, even your pulmonary rehabilitation routine can exacerbate these symptoms; this is why it’s always important to keep your doctor informed about what you’re experiencing.
Oftentimes, COPD patients may encounter symptoms that are seemingly unrelated to their lungs. These are called “complications” because they are not common symptoms of lung disease but lung disease can often be a catalyst for things like heart disease, vascular disease, and even mental health disorders like depression or anxiety.
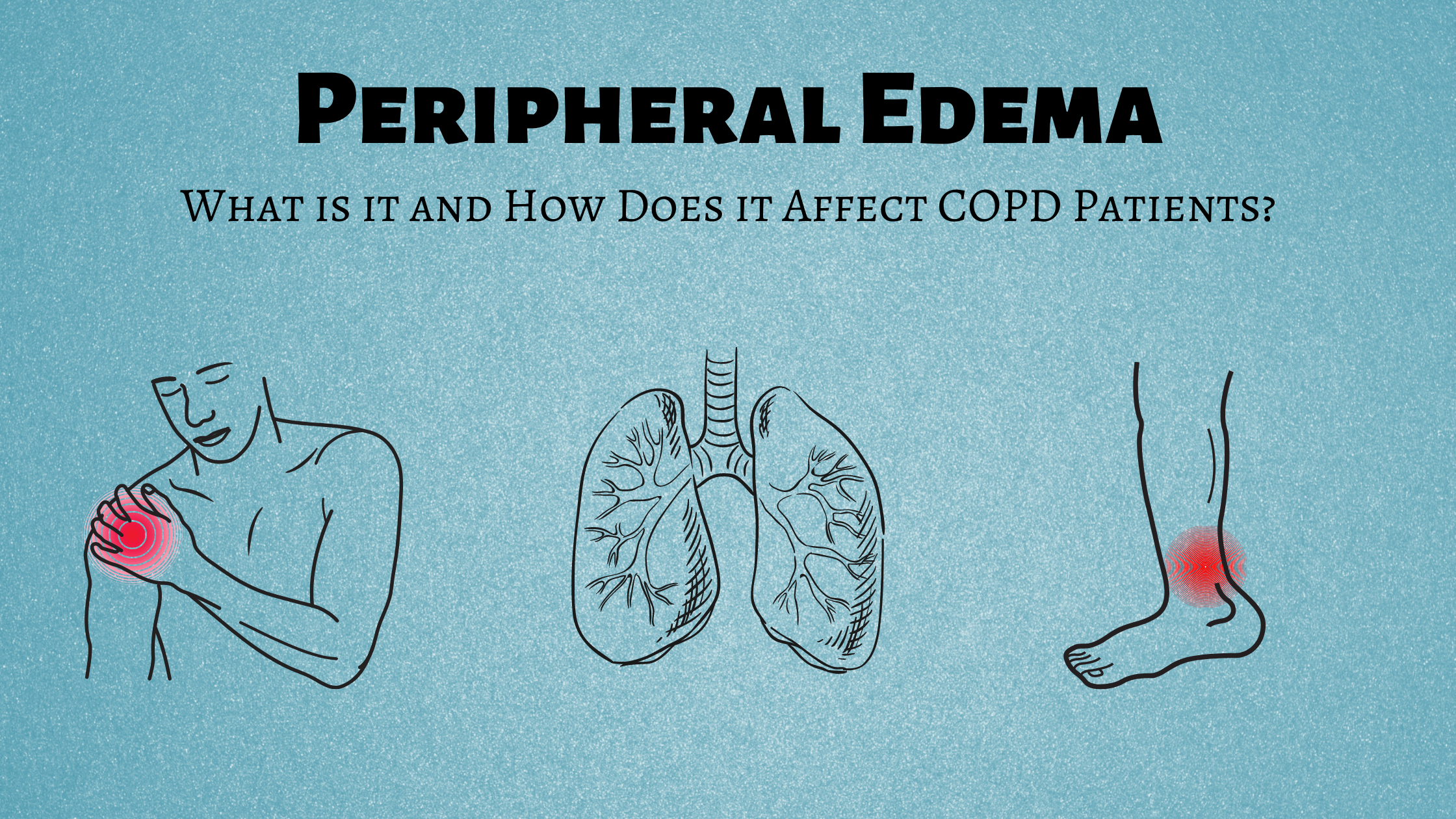
One frequent, but often overlooked complication of COPD is something called peripheral edema. The term “edema” refers to swelling in the body, usually due to the buildup of fluid and the term “peripheral” refers to areas away from the center of your body such as your legs, hands, or arms. In this post, we’ll help you better understand what peripheral edema is, what causes it, and what steps you can take to mitigate it.
If you have any questions, please feel free to leave them in the comment section below so we can get back to you.
What is Peripheral Edema?
“Peripheral edema” is the medical term for swelling in the limbs of the body. It can occur anywhere in the body, but it most commonly occurs in the lower legs or feet. Usually, edemas develop slowly over a couple of days or weeks, but in rare instances, it can happen over the course of a couple of hours. Many patients don’t realize there is swelling until they experience pain or they aren’t able to put on their shoes, shirt, or pants.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
There are six types of edema, but only three of them are known complications of COPD. These include peripheral edema, pulmonary edema, and pedal edema. Let’s take a look at each of the six types of edema to see how they compare.
Lymphedema
Lymphedema usually occurs in one of your legs or arms. Cancer patients who have damaged lymph nodes or people who have had them removed for cancer treatment often experience this symptom. Lymph nodes are an important part of the immune system because they block harmful substances, but if they are damaged they may cause your body to retain fluids, thus causing edema.
Cerebral Edema
Cerebral edema tends to be the most serious type of edema because it occurs in the brain. Some common causes of cerebral edema include head injuries, blood clots, tumors, and allergic reactions. Cerebral edema can often be life-threatening, so it’s best to seek immediate medical attention.
Macular Edema
The macula is at the light-sensitive area at the center of the retina in your eye. Macular edema occurs when blood vessels in this area begin to leak fluid and sometimes blood. If macular edema is left untreated, it can lead to permanent damage to the eyes or even blindness. If you’re experiencing pain in your eyes, a sharp headache, blurry, or impaired vision of any kind, you should immediately contact your doctor.
Pulmonary Edema
Pulmonary edema is the buildup of fluid in the lungs. This is most often caused by heart conditions like a heart attack, hypertension, or narrowed heart valves. Acute pulmonary edema which comes on quickly can be serious and even life-threatening, especially in patients who already have a chronic lung or heart disease.

Pedal Edema
This type of edema is found in the lower legs and feet. There are several known causes of this type of edema including venous edema which is the retention of low-protein fluid and increased capillary filtration. The second most common cause of pedal edema is lymphatic edema which we discussed earlier. These two different causes of pedal edema can either work independently or together to create swelling in the feet.
Peripheral Edema
The term “peripheral edema” is a little broader than the terms used above. While the others describe a specific type of swelling caused by a known condition, peripheral edema can occur in many parts of the body and it has many different causes.
What are the Symptoms of Peripheral Edema?
The primary symptom of peripheral edema is swelling in the extremities. This swelling is usually drastic enough that it will be noticeable by you or your loved ones, and as the swelling increases, you’ll likely have trouble putting on your shoes or clothing without having to force them on.
Another symptom of peripheral edema is reduced mobility. If you’re like most COPD patients, you’re probably trying to stay active in order to preserve your lung function and keep your muscles strong and efficient. If you’re developing peripheral edema, you may feel your legs becoming heavier or you may notice that you lose your sense of balance more easily than you did before.

In some, but not all cases, people with peripheral edema may experience pain and tightness in their legs or feet. As the amount of fluid increases in the affected area, you may notice the skin becoming shiny and red. You might also experience something called “pitting.” This is when you press on an area of your skin and the indentation remains there longer than it would on a healthier part of your body. Since the fluids that your legs or feet are retaining would normally be flushed out of the body, you might also see an increase in your body weight.
What Causes Peripheral Edema?
Peripheral edema has a variety of different causes. If your edema comes and goes within a day or two, this is likely a sign of a less serious underlying condition. But if the edema is chronic and it only seems to get worse as time goes on, this is likely a sign of a more serious underlying condition. Either way, it’s important that you speak with your doctor right away and be thorough about the symptoms you’re enduring. Since there are so many potential causes, peripheral edema is very difficult to diagnose accurately. As a result, the more information your doctor has, the better diagnosis he/she will be able to provide. Below are some of the top causes of peripheral edema.
Injuries
If you’ve ever had a fracture, strain, sprain, or bruise, you know that it’s usually accompanied by some swelling and pain. This is because your body releases white blood cells and other fluids to the area in order to repair the damage. Depending on the severity of the injury, it may take several days or weeks for the swelling to subside.
Prolonged Sedentary Behavior
Physical activity plays an important role in maintaining a healthy vascular system. Even moderate exercise that slightly raises your heart rate has significant benefits when it comes to promoting healthy circulation. However, as we age, it becomes increasingly difficult to exercise regularly. This sedentary lifestyle can affect blood flow throughout your body and lead to fluids building up in your extremities. Especially your legs.
High Sodium Intake
According to the U.S. Food and Drug Administration (FDA), the average American consumes about 3,400 mg of sodium per day but the recommended daily intake is 2,300 mg a day. Unfortunately, sodium plays a major role in the retention of fluids in your body and it can have adverse effects on your body’s ability to flush out toxins. Consuming high amounts of salt through processed foods can cause peripheral edema and if you’re already experiencing edema, it can make it worse.
Medications
Every drug, medication, or supplement has side-effects. Some drugs can cause or contribute to edema either by impairing lymph drainage or increasing the amount of fluid that is filtered from the blood capillaries into various tissues throughout the body. Here are a few of the medications that might cause complications:

- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Blood pressure medication
- Corticosteroids
- Hormones
- Diabetes medication
- Antidepressants
How Are Peripheral Edema and COPD Linked?
Peripheral edema is common in COPD patients. While COPD does not directly cause edema, it can result in a medical condition called pulmonary hypertension which causes peripheral edema. Oftentimes, when a COPD patient experiences swelling in the hands, legs, or feet, they don’t associate it with their lung condition. It’s often shrugged off as a sign of aging or they may take Benadryl or a similar drug thinking it’s an allergic reaction. Ideally, if you ever experience unusual symptoms it’s best to consult your doctor rather than trying home remedies because this may exacerbate the issue.
Pulmonary Hypertension
The function of the right side of the heart is to receive oxygen-poor blood and pump it into your lungs. As it passes through the lungs it is re-oxygenated by alveoli (tiny air sacs) then it moves through the left side of the heart to be pumped through the body. Pulmonary hypertension occurs when the blood pressure in your lungs is too high, thus resulting in strain on the right side of the heart. If this issue persists the heart can become overworked and enlarged, resulting in a condition called cor pulmonale.
Cor Pulmonale
Cor pulmonale is more commonly called right-sided heart failure and it’s usually an urgent medical condition. According to Medscape, COPD patients who develop cor pulmonale have a 30 percent chance of living for 5 years. Peripheral edema is sometimes, but not always, the result of cor pulmonale, so it’s imperative that you visit a doctor even if you don’t believe your swelling is due to any serious underlying condition.

COPD leads to pulmonary hypertension and eventually cor pulmonale through a process called hypoxic pulmonary vasoconstriction (HPV). This is a type of vascular remodeling that results in the constriction of vascular smooth muscle due to low partial pressure of oxygen (Po2). In other words, if your lung function is impaired due to emphysema or chronic bronchitis, the arteries in your lung will respond by reducing their size which will increase blood pressure.
Since pulmonary hypertension and cor pulmonale put so much strain on the heart, you may see the problems manifest in other areas of the body. Due to the force of gravity, blood and other fluids often start to pool up in extremities, primarily the feet and lower legs. If this is the cause of your peripheral edema, your doctor will need to treat your underlying lung problems and vascular problems in order to reduce the swelling. Supplemental oxygen therapy and blood thinners are often prescribed to treat pulmonary hypertension if you aren’t already on them.
How to Prevent Leg Swelling With COPD
If you want to prevent leg swelling with COPD, your best bet will be to follow your COPD treatment plan. Pulmonary rehabilitation is extremely important for preventing swelling because not only will it improve your endurance, but it will also strengthen your heart muscle, improve circulation, and reduce body fat which is a known contributor to peripheral edema. To combat leg swelling, your doctor may advise that you increase the amount of time spent doing pulmonary rehab, or he/she might advise that you split your exercise routines into shorter, more frequent intervals.

Hydration is another key treatment for leg swelling caused by COPD. Plasma, the primary component of your blood is made up of 90 percent water. And water is what keeps blood flowing freely throughout your body without clotting or pooling. So, it goes without saying that drinking more water will improve your circulation and keep you healthy. Most doctors will recommend around 8 to 12 glasses of water a day for the average COPD patient.
![]()
Last but certainly not least, you need to watch what you’re eating. Diet plays an extremely important role in your vascular health so eating the right food can relieve a significant amount of stress on your heart and thus prevent peripheral edema. Aside from staying hydrated, you’re going to want to consume less salt and sodium. What’s more, studies have shown that when coupled with a diet rich in calcium, magnesium, and potassium, low-salt and low-sodium diets are more effective.
Conclusion
If you’re currently experiencing swelling of the hands, legs, or feet with COPD, you’re not alone. This phenomenon can occur for a variety of reasons, most of which are not life-threatening. In fact, many seniors, even ones who are generally healthy, can experience it. But due to the fact that swelling can be a sign of pulmonary hypertension or right-sided heart failure you should plan on talking to your doctor as soon as possible, just to be safe.
In the meantime, you should plan on closely following your COPD treatment plan that you worked out with your doctor. While home remedies may help ease the discomfort and swelling a bit, the best way to treat peripheral edema is to treat the underlying disease that’s causing it. If you have any questions about what you read here, please feel to leave a comment or reach out to us.
_%20(1).png)
One of the most common questions we hear COPD patients ask is, “how can I clear my airways when they get congested?” As a COPD patient, you’re likely to experience coughing fits that are brought on by the buildup of mucus and sputum in the airways and lungs. And sometimes, no matter how hard you try, you feel like you can’t clear them in order to catch a breath of fresh air. This is far more common than you might expect and it can be a frustrating and sometimes even scary experience.
Another thing that many people don’t realize is that airway clearance can be a lot more complicated than learning how to cough correctly. There are many different techniques that can be applied, and it’s also helpful to know why your airways are becoming congested in the first place. In this post, we’ll help you understand some of these concepts and provide you with a step-by-step guide on how to clear your airways safely.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
As always, it’s imperative that you speak to your doctor if you experience ongoing issues with coughing, wheezing, or shortness of breath. These symptoms tend to get worse over time unless the root cause is dealt with. What’s more, coughing fits can lead to flare-ups and exacerbations which can put you in the hospital.
Why does COPD Make it Difficult to Clear Your Airways?
There are two different types of chronic lung disease: obstructive and restrictive. A restrictive lung disease like pulmonary fibrosis or interstitial lung disease is one that affects the lungs’ ability to expand. An obstructive lung disease like COPD or bronchiectasis, however, prevents you from fully expelling air from the lungs. This is especially problematic when the patient tries to cough because they may not have the force necessary to clear mucus and other substances from the airways.

Another reason that COPD makes it more difficult to clear your airways is that this disease is associated with changes in the way that mucus and sputum are produced in the body. In a healthy individual, mucus plays a vital role in the body’s immune function. The body carefully regulates the mucus lining the airways and lungs so that there is enough to trap bacteria but not so much that you choke or can’t breathe naturally. However, in COPD patients, there is usually an overproduction of mucus due to oversized mucus glands and an overabundance of goblet cells.
If you’re a current smoker, this could be another reason that you’re experiencing issues with airway obstruction. According to the Centers for Disease Control and Prevention (CDC), as many as 38 percent of COPD patients are current smokers. This study published in the Karger medical journal found that moderate and heavy smokers have a higher impairment in mucociliary clearance than their non-smoking counterparts. One of the key ways that smoking affects airway clearance is by damaging and killing cilia. These are tiny hair-like organelles that help to push mucus and other debris out of the airways.
Since there are so many different causes of airway obstruction in COPD, it’s important to have a comprehensive treatment plan to deal with these symptoms. Airway clearance therapy can and should be used, but it won’t be as effective if you aren’t following all other aspects of your treatment plan that your doctor has designed for you. Ideally, if you’re following your treatment plan carefully, you won’t experience mucus buildup as frequently and you’ll only need to use airway clearance techniques in rare circumstances.
What is Airway Clearance Therapy (ACT)
Airway clearance therapy, or sometimes called airway clearance techniques, is a group of scientifically backed methods used for clearing mucus from the airways. These techniques were developed as a more controlled version of our body’s natural airway clearance techniques like coughing and wheezing. A chronic and persistent cough or episodes of wheezing can be extremely unhealthy, especially if they lead to you losing sleep or feeling lightheaded or fatigued. Airway clearance techniques aim to not only make COPD patients more aware of how they’re coughing, but also provide them with some entirely new methods that may be more effective.
-jpg.jpeg)
Generally speaking, airway clearance techniques are divided into seven different categories. Everyone has a slightly different way of practicing these techniques, so don’t be alarmed if your pulmonologist tells you something that differs from what you have read here. Our goal is simply to provide you with an overview so that you can better understand how airway clearance therapy works.
1.) Controlled Coughing
Like we mentioned before, uncontrolled coughing is problematic in COPD patients. Without understanding how your lungs, airways, and mucus work, simply expelling air in an attempt to dislodge any obstruction can be more effort than it’s worth. One of the biggest problems associated with normal coughing or wheezing is that it often causes the airways to collapse, meaning that no matter how hard you cough, the mucus will be stuck. If you hear a wheezing or whistling noise when you cough, this is a sure sign that your airways collapse when you cough. Controlled coughing is focused on keeping the airways open so that you’re not wasting valuable energy and oxygen.

The first rule of controlled coughing is to avoid inhaling sharply through your mouth. This can send mucus back down the airways and be very counterproductive. Instead, inhale slowly but deeply through your nose. This way you have enough oxygen to cough correctly. It’s best to practice controlled coughing while sitting down and you should try to relax as much as possible. Especially try to eliminate the tension in your shoulders and chest because this can contribute to the airways becoming narrow.
Once you’re seated, lean forward slightly and place your hands on your abdomen. You’re going to cough three times and you should really focus on the quality of each one to ensure that the mucus is moving out of your airways rather than back down into your lungs. Be sure to take a deep breath through your nose between each cough to ensure that you move enough air. If you need to take a moment to relax between each cough, this can be helpful.
Another technique that’s similar to controlled coughing is huff coughing. For the most part, you will follow the same steps as you would for controlled coughing. However, instead of coughing, you’re going to be forcing air through your airways similar to how you would fog up a mirror or how you would clean a phone screen or your glasses. In other words, you’re expelling air out your mouth without creating any vibrations in your chest or throat.
2.) Autogenic Drainage (AD)
The aim of autogenic drainage is to move mucus from the smaller airways into the larger airways (peripheral airways into central airways). By doing this, it is much easier to dislodge the mucus because it’s all in one area. The rationale for autogenic drainage is based on a principle of solid mechanics called shear force. This is when unaligned forces are applied to an object causing it to bend in two different directions. In the case of autogenic drainage, the mucus and other secretions in the airways are the object that’s being manipulated. This is done through a series of carefully monitored breathing techniques.
3.) Postural Drainage and Percussion (PDP)
Postural drainage and percussion, also known as chest physical therapy (CPT), is a technique that involves using your hands to assist with airway drainage. While you can do PDP on your own, it’s often recommended that you have someone assist you with it, whether it’s a friend, loved one, or your physical therapist. Like autogenic drainage, PDP is a technique that will take some time to perfect so it helps to be patient as you learn the ins and outs of this method.
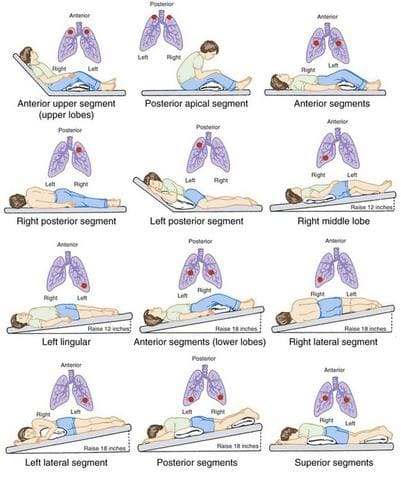
The reason this method is called “postural” drainage is that you are going to use different positions that leverage gravity in order to drain the mucus from your airways. The general rule of thumb is that your hips should be higher than your chest. Whether this means laying on your back, side, or stomach, you can do whatever is most comfortable for you. Many people prefer to use pillows or blankets to elevate their hips.
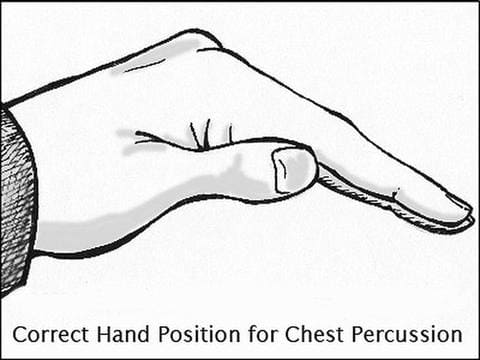
Once you’ve found a comfortable position you can begin the percussion. Most specialists recommend cupping your hand and placing it palm down on your chest. This will allow you to break up the mucus in your chest without hurting yourself. The percussion can also be done on your back but it’s best to have a partner to help you out with this.
4.) Positive Expiratory Pressure (PEP) Therapy
Essentially, the term positive expiratory pressure means experiencing greater resistance when you’re exhaling than when you’re inhaling. This is done with a PEP device which you hold to your mouth and breath into. The device allows you to inhale normally, but when you go to exhale, you experience resistance about four times greater than what you would normally experience. What this does is keeps your airways open as you exhale and allow the force of your air to get behind the mucus and push it out of the airways.

5.) Oscillating Positive Expiratory Pressure
Oscillating positive expiratory pressure therapy is very similar to the method above. However, an oscillating PEP device uses high-frequency oscillations that break up mucus as you exhale. Oscillating PEP devices look similar to traditional PEP devices but they have a ball inside that rattles around as you exhale. This is what creates the vibrations in your upper chest. After blowing into the device several times, you can take a break to clear out any mucus that the device brought up. Then simply repeat the process.
6.) High-Frequency Oscillating Vest
A high-frequency oscillating vest is another tool that can be used for airway clearance. This is an inflatable device that looks a lot like a life vest. The oscillating vest is connected to an air compressor via two hoses. Once it’s turned on, the vest inflates and deflates in rapid succession. The basic principle is that it uses positive and negative pressure changes in the chest to augment peripheral and tracheal mucus movement towards the airway opening. After a set period of time, the device is stopped and the patient can cough to bring up the mucus.

While high-frequency oscillating vests are very effective, they aren’t without disadvantages. These vests can be very expensive to purchase and maintain. What’s more, they’re not very portable in comparison to the PEP devices which we discussed earlier. If you’re someone who travels a lot you might find that high-frequency oscillating vests are more trouble than they’re worth.
7.) Active Cycle of Breathing Technique (ACBT)
The active cycle of breathing technique is an airway clearance method that combines positioning, breathing, and coughing. Since this is the most complex airway clearance technique it’s also the most flexible when it comes to being adapted to fit a variety of patient’s needs. The goals of ACBT include improving the effectiveness of your coughs, improving lung ventilation, and clearing secretions from the lungs. Below are the three different phases of ACBT:

Phase 1 - Breathing Control and Relaxation
The first step in ACBT is to bring your breathing under control and completely relax your body. The majority of the tension in your body will be located in your shoulders, chest, and back, and many people are unaware of how much this can affect the way you breathe. Start by closing your eyes and placing your hands on your stomach. Sit with your back straight and begin to practice pursed lips breathing. This is where you inhale slowly through your nose and exhale fully through pursed lips.
Phase 2 - Thoracic Expansion Exercises
As the title suggests, the aim of phase 2 in the active cycle of breathing technique is to expand the chest. During this step, you will take 3 to 5 deep breaths in through your nose and out through your mouth while keeping your shoulders and chest relaxed. At the peak of each inspiration, you will hold your breath for 2 to 3 seconds. After the allotted time, simply release the air rather than trying to force it out.
Phase 3 - Forced Expiratory Technique (FET)
The forced expiratory technique is another way of saying “huff” cough. Like we described under the “controlled coughing” section, a huff cough is a way of clearing mucus without allowing the airways to collapse. You’re simply pushing air out the lungs but putting more air behind it than you would with a normal breath. You should repeat this after each thoracic expansion that you do.
Other Ways to Prevent Airway Obstruction With COPD
Drink Plenty of Water
Your ability to prevent airway obstruction depends heavily on your level of hydration. Mucus is made up of about 97 percent water. However, slight variations in this can cause it to become extremely thick and difficult to clear from the airways. Since every organ in your body uses water, it’s imperative that you aren’t starving yourself of this vital resource. According to COPD.net, the average COPD patient should drink between 8 and 12 glasses of water every day.

As you work to increase your water intake, it’s also important to reduce your intake of other types of fluid. Milk, and dairy products in general, are known for thickening your mucus so you’re going to want to avoid these as much as possible. Much like salt, sugar has the ability to dehydrate you, so you should avoid sugary sodas, fruit juices, or sweetened tea. If you absolutely have to drink something other than water, try unsweetened hot green tea which will not only thin your mucus but has a number of other health benefits as well.
Maintain a Balanced Diet
Healthy eating is all about getting the right balance of nutrients that your body needs to stay healthy. For COPD patients and people with other respiratory illnesses, this could mean consuming less sodium and salt which contributes to problems like airway obstruction. You should also avoid highly processed foods which can contribute to bloating and thus making it more difficult to breathe. Most COPD patients tend to do better with a diet that is high in protein and healthy fat which is easy to digest and will support healthy lung function.
![]()
Use COPD Medications Effectively
Depending on how severe your COPD is, your doctor has likely prescribed you some medication for coping with your symptoms. One of the most common medications for COPD is called bronchodilators. These medications open up the airways so that you can breathe easier and they can make it easier for you to perform the airway clearance techniques listed above. Ask your doctor about changing up your treatment schedule to assist with airway clearance.

Another medication that can help with airway clearance is a class of drugs called expectorants. These are medications are designed to thin the mucus in your airways making it easier to clear. Expectorants aren’t designed specifically for COPD patients because they’re also used to treat congestion associated with the common cold and the flu. While expectorants are available for over-the-counter purchase, you should be sure to ask your doctor before using them because they may have adverse interactions with the COPD medications you already take.
Pulmonary Rehabilitation
Pulmonary rehabilitation (PR) is an exercise and education program focused on improving lung strength and function. COPD patients should begin pulmonary rehabilitation right after they’re diagnosed so that they learn the best way to take care of their lungs and slow the progression of COPD. Another benefit of PR that many people don’t realize is that it can help with airway clearance. According to a study published in the European Respiratory Journal, exercise improves mucosal clearance in the small airways by releasing moderators that increase fluid secretion and stimulate cilia beat frequency. What’s more, PR increases lung strength and endurance which can help you perform the airway clearance techniques listed above.

Get More Restful Sleep
Getting restful sleep is a problem that many people face for their whole lives. According to the Sleep Association, around 50 to 70 million people suffer from a sleep disorder in the United States. So, as you can imagine, there is a lot of overlap between people suffering from COPD and people suffering from sleep disorders. If you’ve never been diagnosed with a sleep disorder or provided with treatment for your sleep disorder, now is the best time to seek help. Addressing your sleep problems will have undeniable benefits when it comes to helping you manage your COPD. If you’d like to learn more about getting restful sleep with COPD, please read through this article.

Conclusion
Airway clearance therapy is an incredibly important skill for all COPD patients to learn. However, it’s not an all-in-one solution. Drinking enough water, getting enough sleep, eating right, and exercising are all great ways to prevent airway obstruction and prevent the need for alternative therapies. If you’re experiencing frequent coughing or wheezing, we recommend contacting your pulmonologist immediately so that you can address your concerns.
Here at LPT Medical, we specialize in life-saving oxygen equipment which can help you maintain your oxygen levels if you are experiencing a coughing fit or COPD exacerbation. We will help you get the best deal on the market for portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5. These devices are much lighter and reliable than traditional oxygen delivery devices allowing you to go more places without worrying about whether or not you’re getting enough oxygen. Since the oxygen is administered through a nasal cannula you can still do all of the airway clearance techniques above while you’re receiving oxygen.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s very important to us that you receive the oxygen concentrator that’s right for you. When you reach out to us, you will be connected with a respiratory specialist who will ask you questions about your oxygen use and lifestyle. If cost is a concern for you, we also have a variety of different buying options including new, used, and refurbished concentrators. We also have financing options available if you’d like to pay in easy monthly installments. Reach out to us either by phone or email for more information.
Chronic obstructive pulmonary disease otherwise known as COPD is a group of respiratory illnesses most commonly associated with emphysema and chronic bronchitis. This disease will damage the patient's lungs and it cannot be reversed.
That being said, there are many people who lead happy healthy lives and still deal with their COPD diagnosis everyday. You can as well, by adhering to the "dos and don’ts" in this article about living with COPD.
Do have a more positive outlook
While having a positive outlook is easier said than done, remember that if you have been diagnosed with COPD, you have a chance to turn your life around by altering bad habits, adjusting to a treatment regime, and the opportunity to be a part of clinical trials and break through medications. If your condition went undiagnosed and therefore untreated, your situation would be much much worse.

In a newsletter from The Gerontological Society of America as many as 30 million Americans are affected by COPD yet many patients are not diagnosed, and many publications agree that this occurs due to a variety of reasons.
COPD diagnosis can go undetected due to poor awareness of symptoms among patients and providers and unrecognizable suspicion of disease. It is estimated that over 30 million Americans have COPD yet so many cases go undiagnosed and untreated and only about 16 million people have been diagnosed and given a treatment plan.
If you are one of the ones who has been diagnosed with COPD, you are one of the lucky ones. You know that there is something happening in your lungs that is making it difficult to breath, and affecting your life everyday, and you get to do something about it!
The first thing you need to do is to change your perspective, and realize that even though COPD is not curable, there are treatments, medications, clinical trials, and other ways you can slow down the progression of the disease and live a long active fulfilling life.
It is better to know why certain things are happening in your body, rather than staying in the dark. Once you know what is happening, you can begin to understand why it is happening, from there you can do something about it.
There are still a few things you should know about the Dos and Don'ts of living with this disease, and you can find all of this information in this article.
Don’t continue to smoke

Just because you have COPD does not mean it is too late to quit smoking. As we mentioned earlier in this article, COPD is a progressive disease and it gets worse over time, especially if you continue bad habits, such as smoking.
Smoking will contribute to the breaking down and suffocating nature COPD already imposed on your lungs, by quitting, you are taking away the catalyst that is speeding up the deprivation of your lungs.
Unlike some diseases, COPD usually has an obvious cause and so there is a clear way of preventing it, and there are also ways to slow the progression of COPD. The majority of cases are directly related to cigarette smoking. Therefore, the best way to prevent COPD is to never smoke — or to stop smoking.
If you're a longtime smoker, these simple recommendations might seem impossible, especially if you've tried quitting before. But keep trying to quit. It's critical to find a tobacco cessation program that can help you quit for good.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Here are some resources that might help you quit smoking, try a few of these methods if one doesn’t work another strategy might:
Other than smoking, other exposure to chemical fumes and dusts is another risk factor for COPD patients. If you work with harmful fumes and lung irritants, talk to your supervisor about the best ways to protect yourself, such as using respiratory protective equipment.
Do get an annual flu vaccination

The annual flu shot and regular vaccinations against pneumococcal pneumonia will reduce your risk of catching some infections. By contracting a viral infection as a COPD patient you are subjecting yourself to exacerbations, also known as flare ups, which do impact the health and longevity of your lungs. Therefore, you should avoid exacerbations at all costs, not only because of the uncomfortable feeling experiencing one, but also the long-term damage poses a major risk of speeding up the progression of your disease into a more severe state.
COPD exacerbations are often caused when people with COPD come down with the cold or the flu. You can protect yourself by taking preventative measures and getting your annual flu vaccine. Keep in mind that it’s better to get a standard shot than a nasal spray vaccine, according to the Centers for Disease Control and Prevention. On top of getting an annual flu vaccine, it’s important to get the pneumonia vaccine at least once before the age of 65.
Medical professionals recommend guarding yourself against whooping cough, by getting a vaccine called Tdap, which also protects against other sickness like tetanus and diphtheria. If you’re over 60, you might also need a zoster vaccine which protects against shingles. By getting these vaccines, you’ll help minimize your risk for infections that can lead to severe COPD complications.
Nobody enjoys getting sick, but people with COPD have to be extra careful, because if they are to get sick, it can worsen their COPD symptoms beyond repair. If you want more information on this topic, we have an entire blog post dedicated to how people with COPD can enjoy life in a global pandemic while staying healthy and safe.
Don't expose yourself to germs
Especially at a time of this unprecedented global pandemic, do your best to steer clear of people who are sick, and stay aways from crowded areas. There are many other ways to steer clear of the coronavirus causing COVID-19, such as wearing a mask, disinfecting surfaces, avoiding grocery stores, and avoiding travel at all costs.
Living in isolation, and with COPD, is another battle that many people face, and it can be a very harsh reality for some people. If this is something that you experience, the first thing you can do is join Facebook groups and online forums that are set up to be COPD support groups. Simply search “LPT Medical COPD & Respiratory Support Group '' on facebook you will find a wonderful community of COPD patients and respiratory specialists who are ready to help answer your question and also eager to have like minded conversations and online friends.
You will see that many people are struggling with similar problems and you might find their advice helpful, you could also give some great advice to others.
Do consider being a part of COPD clinical trials

Clinical trials are regulated research studies that are set up to find better ways to prevent, screen for, diagnose or treat a disease. There are a lot fo COPD critical studies that are developed to answer specific questions about new interventions—which can be new vaccines, drugs and devices—and measure their effectiveness and safety for patients. The Food and Drug Administration (FDA) regulates clinical trials in the U.S.
There are several benefits to being a part of a study, as well as some risks. Depending on you COPD severity and some other factors can help to determine if you are a good fit.
Benefits:
- Access to new treatments that are not yet available to the public
- Access to expert medical care at a leading healthcare facility
- Playing an active role in your own health care
-
Helping others by contributing to medical research
There are also some potential risks:
- There may be unpleasant, serious or even life-threatening side effects from treatment
- Treatment may not be effective for some individuals
- The study may require a lot of time for traveling to the study site, receiving treatments, or hospital stays
- Your health insurance may not cover all the study costs
You can find clinic trails either though a reference form you doctor, or you can also search for clinical trials online.
here are some clinical trial programs to be aware of:
American Lung Association's clinical trials listing
CenterWatch Clinical Trial Research Center
Don't breathe hazardous air

Depending on where you live, breathing clean unpolluted air may or may not be possible at all times of the year. In most of the US right now (June through September) the western more arid land is experiencing horrendous wildfires, and the jet stream transports this smoke filled air across the country.
Smoke from wildfires can be disruptive to anyone's lungs, but people with COPD should be extra cautious. When the healthiest person inhales wildfire smoke, it can cause throat irritation, wheezing, sneezing, coughing, runny nose, congestion, chest discomfort, eye irritation, and shortness of breath—all triggered by the tiny particles in the smoke.
When a person with COPD inhales forest fire smoke, they experience all of the same irritations but the discomfort is multiplied and the effects will last much longer.
We wrote an entire blog post dedicated to how to cope with poor air quality due to forest fires, you can read more about it here.
Due to the amount of forest fires, air filters have been sold out in stores and online. If this is that case in your area, or if you want to save some money, you can build your own air filter in your home for about $25.
What you will need to build your own air filter is listed below, and all these materials can be found at a hardware store near you!
- 20" x 20" box fan
- 20" x 20" x 1" MERV 13 or FPR 10 filter
- Power drill*
- 3/4" screws*
- 2" corner brackets*
Use the tutorial video from the Puget Sound Clean Air Agency to build the filter. They have tested the performance of these do it yourself filter fans and they dramatically reduce fine particles and black carbon from the air.
To improve the air quality in your home for the long-term, you can start by getting rid of wall-to-wall carpets. Carpets hold dust particles, hair, and other allergens much longer than hardwood or tile, and these indoor air pollutants are not good to inhale. You should also clean with green products or with natural cleaners like soap and water, baking soda, and vinegar rather than any harsh chemicals or dense cleaning products.
Depending on where you live, you might have to deal with pollutants other than wildfire smoke such as humidity, smog, and annual allergies. While you cannot always control breathing some of these pollutants into your lungs, you can work to reduce your footprint and take certain actions to reduce overall air pollution.
If you want to contribute to a future with cleaner air, you can try to implement these tactics into your everyday life:

- Conserve energy i.e. turn off lights, fans, electronics - at home, at work, everywhere.
- Look for the ENERGY STAR label when buying home or office equipment.
- Carpool, use public transportation, bike, or walk whenever possible. Walking and biking are also great outlets for getting your daily exercise in.
- Follow gasoline refueling instructions for efficient vapor recovery, being careful not to spill fuel and always tightening your gas cap securely.
- Consider purchasing portable gasoline containers labeled “spill-proof,” where available.
- Keep your car, boat, and other engines properly tuned.
- Be sure your tires are properly inflated.
- Use environmentally safe paints and cleaning products whenever possible.
- Mulch or compost leaves and yard waste.
- Consider using gas logs instead of wood.
Do get exercise and daily physical activity
It might not seem like the most appealing advice especially when you feel short of breath, but getting enough exercise even if you have COPD is essential for maintaining a healthy weight and therefore lifestyle.
Your lungs may not work at their best capacity as they did before you had COPD, but working out your muscles and your lungs will build strength that you need to continue to do the things you love to do.

“Exercise” can be as simple as walking to and from your mailbox everyday. Soon enough you will be able to walk further or faster depending on how you like to exercise.
Exercise is one of the most important things you can do to treat COPD and make your life more comfortable at all hours of the day and night. It plays an essential role in maintaining a healthy weight and people with COPD shouldn’t be too heavy or too thin.
If you’re overweight, your heart and lungs have to work harder to supply your body with oxygen which with COPD is already hard enough. If you’re underweight, you might not be eating enough nutrients to get you the energy you need to do everyday tasks making you feel weak and short of breath more than you would if you were a healthy weight.
Exercise may be the last thing you feel like doing when you have COPD, but it improves COPD symptoms and will ultimately give you more energy, so talk to your doctor about how to develop an exercise regimen that will work for you.
In order to maintain a healthy weight, you must eat a well-balanced diet and get regular exercise, which can also improve circulation and help your body use oxygen more efficiently. If you’re not sure if your weight is healthy or unhealthy, talk to your doctor.

Here are some tips for eating well for COPD patients specifically:
- To lose weight: Choose fresh fruits and veggies over bread and pasta for the majority of your complex carbohydrates
- To gain weight: Eat a variety of whole-grain carbohydrates and fresh fruits and vegetables
- Limit simple carbohydrates, including table sugar, candy, cake and regular soft drinks.
- Eat 20 to 30 grams of fiber each day, from items such as bread, pasta, nuts, seeds, fruits and vegetables
- Eat a good source of protein at least twice a day to help maintain strong respiratory muscles, you can try all of these options: milk, eggs, cheese, meat, fish, poultry, nuts and dried beans or peas
- Choose mono- and poly-unsaturated fats, which do not contain cholesterol. These are fats that are often liquid at room temperature and come from plant sources, such as canola, safflower and corn oils. If you are trying to lose weight, you do not need to add these to your meals.
- Limit foods that contain trans fats and saturated fat. For example, butter, lard, fat and skin from meat, hydrogenated vegetable oils, shortening, fried foods, cookies, crackers and pastries.
Even though these suggestions are developed for people with COPD, speak with your doctor or a nutritionist about the best diet for you.
Dieting and regular exercise does not come easy to everyone, having a support system that is willing to cut out some junk food and focus on exercise more often is life changing for people with COPD.
Don't eat big meals

If you have COPD you should avoid the feeling of being “too full”, you might have noticed that you feel breathless after eating large meals. If you feel like you do not have an appetite, eating smaller meals can also help you get the nutrition your body needs. Breathing when you have COPD is more challenging and therefore requires you to burn more calories, so you should be sure that your meals provide high quality nutrition. To learn more about the type of meals you should be eating and how often, speak with a registered dietitian to help you understand how to make the most of your calories.
There are also lung specific diets that contribute to heart and lung health. Creating a food plan can be overwhelming, so having a buddy or partner that can do it with you is always a motivating factor.
Whatever you have to do to manage your diet, you should do. Whether you have to spend a little bit of money on a nutritionist or spend more at the grocery store to buy healthier foods rather than cheap junk foods.
While you might have to start spending more money to eat better, we will discuss in a later section ways you can supplement these expenses by saving money in other aspects of your life.
Do save money

Having COPD is not free, unfortunately there are costs associated with medications, hospital visits, oxygen devices, and much more. Depending on your financial situation, you might have to save money on certain things in order to pay for COPD treatments.
You can start by saving money on your COPD medication. Many people cannot afford the inflated prices of name-brand medications. Luckily, you can often find off-brand, generic versions of the same medication at a much lower cost.
If you want to save even more money on your medication, you can find other sources for your medication rather than your local pharmacy. Although they might be quick and convenient, brick-and-mortar pharmacies also tend to have the highest prices.
Many people don't realize that they have other options besides their local pharmacy. In reality, there are dozens or more legitimate online and mail-order retailers that sell prescription medications, too, and for less money. A certain amount of research about the online pharmacy is a precaution you should take thoroughly before entrusting it with your prescription. While many are trustworthy, some sites are unreliable, lack quality control, and even sell potentially dangerous counterfeit medications.
Here is a resource for you to learn more about saving money on your COPD medication: link
Hospital visits can also cost a pretty penny, and for the sake of your health and wallet, we hope you can avoid emergency and hospital visits if at all possible. However the truth is, you might experience an exacerbation that requires medical attention.
The way you can save a lot of money is being capable of determining when you need to go to the hospital and when you can confidently take care of yourself from home and just call your doctor. This is where COPD education and management comes into play.
You should feel confident and equipped to handle your COPD symptoms especially if they are not too severe. One of the best ways to avoid hospitalization is knowing which of your COPD exacerbation symptoms require emergency care.

An exacerbation happens when your lungs do not make the exchange of gases that is required in order to breathe. After your body uses oxygen, carbon dioxide is left on the inside. Your lungs are responsible for exchanging oxygen with carbon dioxide, essentially this is what inhaling and exhaling is.
A person with COPD has more difficulty inhaling and exhaling because their lungs don’t work as well. This could lead to a buildup of carbon dioxide and reduced oxygen levels.
If carbon dioxide builds up in your body or oxygen levels become too low, it can become deadly. Symptoms of too much carbon dioxide in your body include:
- Confusion
- Severe headache
- Difficulty walking even short distances
- Having a hard time catching your breath
If these symptoms occur, then it’s important to seek immediate medical attention.
If you have COPD, physical activity will typically leave you short of breath and this is not a reason to seek medical attention every time. But during an exacerbation, your symptoms can get much worse than normal.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Examples of COPD exacerbation symptoms include:
- Breathing in a fast and shallow pattern, as if you’ve just exercised very intensely
- Coughing persistently and more than normal
- Experiencing shortness of breath at rest or with minimal activit

We’ve all experienced what it’s like to be burnt out on something. Whether it’s your job, chores, or health routine, it’s not always easy to find a way to stay on track to meet your goals. What complicates this even further is that everyone experiences this for a different reason. For some people, it’s just a matter of learning how to stick to a routine, but for others, it could be a lack of mental or physical energy that’s holding them back.
Oftentimes, when people are trying to stick to a COPD treatment plan, the latter is true. After all, fatigue is the second most common symptom of COPD with about 50% of patients experiencing it. Knowing this information, it’s not hard to see why it can be difficult to stick to a routine. If you’re hit with a sudden wave of fatigue, grogginess, or breathlessness, it can make simple tasks seem overwhelming. Eventually, your health goals will seem unattainable and unrealistic.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this post, we’re going to provide you with some tips for having a fresh perspective on your COPD treatment plan. Regardless of the stage of COPD that you’re in, it’s never too early or too late to hit the reset button and start managing your COPD symptoms proactively. If you have any questions, feel free to leave them in the comment section below and we’ll get back to you.
Change Up Your Exercise Routine
As a COPD patient, you know how important your exercise routine is. While exercise does not magically reverse the effects of lung damage, it improves the efficiency of your body and lungs which inevitably leads to less breathlessness, less chronic pain, and a longer life expectancy. But you know as well as anyone that exercise routines are difficult to stick to, especially if you viewed it as a “chore” in the first place.

More often than not, COPD patients are taught how to exercise through a pulmonary rehabilitation program. These programs are aimed at educating patients about their lungs and disease, then applying exercise techniques that allow them to lead a happier life. Unfortunately, pulmonary rehabilitation programs don’t teach you how to make your exercise routine “interesting” or “engaging.” They simply tell you what needs to be done. As a result, many people find themselves in a situation a year or two down the road where they don’t have the motivation to continue.

At some point, you’re going to want to try new exercises that hold your interest. The important thing to remember is that you still need to follow the guidelines that you learned in pulmonary rehabilitation because this will ensure that you are making the most of your time and avoid injury. For example, if you implement a new exercise, you need to make sure it works the same muscle group and that it’s a similar intensity as your original exercise. If you have any doubts about it, you can always reach out to your doctor with any questions you may have.
Make Adjustments to Your Diet
What you eat also has a major impact on your ability to live a comfortable life with COPD. Unfortunately, your diet is also something that can become mundane if you’re eating the same things every day. Like with exercising, it’s okay to make changes to your diet, you just need to make sure that you’re getting the right nutrients. You also need to ensure that you aren’t increasing or decreasing your caloric intake too much. According to the COPD Foundation, breathing with COPD takes more energy than for a healthy individual, so you need to maintain your caloric intake.

Most COPD patients need a high protein intake. Protein plays an essential role in the structure, function, and regulation of body tissues. Most notably, protein helps you build muscle and counteract muscle atrophy which is common in COPD patients. Maintaining muscle mass is important for respiratory patients because strong muscles take less oxygen to function, thus reducing the burden on your lungs. While you probably get most of your protein through meat, there are many other great sources of protein, including but not limited to fish, eggs, dairy products, nuts, and beans.
You might think of fats as being “unhealthy.” But you may be surprised to find that many COPD patients are prescribed high-fat diets. The problem is that many people don’t know the difference between healthy fats and unhealthy fats. Unhealthy fats like saturated fat or trans fat include things like beef or pork fat, margarine, butter, and shortening. Eating too many of these things can lead to increased blood cholesterol levels and LDL cholesterol levels. Healthy fats, on the other hand, like monounsaturated fats and polyunsaturated fats include avocados, olives, nuts, olive oil, and more. Fatty fish like salmon is also a great source of healthy fats like omega-3.
While it may seem like COPD diets are pretty restricted, this is not necessarily the case. It’s important to avoid foods that are high in added sugars, sodium, and unhealthy fats. However, aside from that, you simply need to meet your minimum caloric intake for the day and any other requirements that your doctor sets. You still have plenty of freedom to choose what you eat and switching up your meals can even keep you on track for meeting your goals by preventing burnout.
Upgrade to a Portable Oxygen Concentrator
After being prescribed oxygen, many people choose the first oxygen device they think of — oxygen tanks. Most people know about oxygen tanks and they’ve seen people use them. But that doesn’t mean they’re the best option for you and your lifestyle. Although oxygen tanks are a popular choice, they tend to be heavy and bulky meaning they are difficult to maneuver. Fortunately, there is an alternative known as portable oxygen concentrators.

A portable oxygen concentrator is unlike an oxygen tank in that it doesn’t hold oxygen within the unit. Rather, it takes in ambient air, removes nitrogen and argon, and puts out medical-grade oxygen. POCs are electronic devices and they run off of powerful lithium-ion batteries, so you simply need to charge the battery via a car or wall outlet and you’ll be on your way. The most notable benefit of this is that you won’t have to keep going out of your way to refill or replace your oxygen tanks when they run out.
Another benefit of portable oxygen concentrators is their lightweight and compact design. Unlike oxygen tanks which are oblong-shaped, POCs are small enough and light enough to be carried on your shoulder. This opens up a world of possibilities and enables you the freedom to live life on your own terms without being defined by your disease. Inevitably, this leads to more options for you and a lower chance of experiencing burnout with your COPD treatment plan.
Reduce the Clutter
Sometimes it’s not our COPD treatment plan itself that’s causing us to feel burnt out, but all the extra clutter around us. The term “clutter” can be defined as anything that complicates our lives and occupies our thoughts but doesn’t provide any real benefit to us. If you live with clutter too long it can really start to become exhausting and you’ll notice yourself losing motivation in other areas of life such as your exercise routine, diet, and making it to doctor’s visits.

For some people, this might imply clutter within the home. For example, having a messy bedroom, bathroom, or kitchen can lead to a lot of discomfort in your daily life, and as a result, you might find yourself too distracted to follow your COPD treatment plan. Eliminating physical clutter like this is as simple as taking the time each day to organize your home and avoid getting to the point where it’s too much to manage. If you’re too busy to clean, you might consider hiring a caretaker who can help out around the home.

Another type of clutter is “mental clutter.” Think of this as the opposite of mental clarity. Instead of being able to concentrate on what you’re doing in the current moment, your thoughts are always wandering to something else. Mental clutter can certainly be caused by things like a messy home, but it’s more likely to be caused by something that takes your focus off of what you’re doing in the present moment. For example, watching the news for too long or spending too much time on social media are both things that can take your focus off the present moment.

Cognitive behavioral therapy (CBT) is one way of dealing with problems related to mental clarity. This is a type of therapy that’s focused on reversing negative or unproductive thought processes. CBT has become very common among people with chronic conditions like COPD as awareness around mental health problems has increased. During CBT, you will work one-on-one with a certified therapist who will guide you through the process.
Practice Meditation
Meditation comes in many different forms. However, in most cases, the goal is always to achieve a state of mental clarity and well-being. Meditation helps train your mind to think clearly and without distractions. It also promotes emotional well-being while reducing anxiety and in some cases even improving physical well-being. By far the most popular form of meditation for COPD patients is Tai Chi. This practice combines traditional meditation principles with martial arts. It’s popular for COPD patients because it teaches you to control your thoughts, breathing, and balance, all of which are important if you’re trying to improve your health. Read through this post we made about Tai Chi to learn more.

Speak With Your Doctor
Your doctor should be your first point of contact when it comes to anything related to your COPD treatment plan. If you know that you need to make changes, your doctor will be able to tell you what changes are acceptable and which are not. He/she may also be able to provide you with additional resources or direct you to another specialist who can help you deal with issues related to COPD burnout and fatigue. Sometimes burnout is due to poor sleep quality, so he/she may recommend that you get tested for obstructive sleep apnea (OSA) and other sleep disorders.

Another change your doctor may be able to do is make changes to your medication routine. Corticosteroids are one of the most common drugs used to treat COPD because they reduce inflammation in the lungs. However, these drugs are also known to have adverse psychiatric effects such as mania, depression, and cognitive impairments, all of which can contribute to burnout and a negative outlook of your disease. Your doctor may be able to reduce your dosage or prescribe you a different medication altogether.
Conclusion
Being “burnt out” on your COPD routine can be exhausting. On one hand, you may be tempted to revert to your old way of living and entirely forget about your COPD treatment plan. However, on the other hand, you understand that the best way to deal with the symptoms of your disease is through persistence and consistency. If you feel like you’ve reached this point, be sure to try some of the tips above to get back on track.
Ultimately, you will want to consult your doctor if you’re struggling to keep up with your treatment plan. It’s not unusual for someone to struggle, especially if they’ve had COPD for many years. Here at LPT Medical, we strongly believe that a portable oxygen concentrator can help you regain much of the freedom that you lost after being diagnosed with COPD. As a result, you’ll be able to approach your treatment plan from more angles and prevent burnout.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
We sell some of the top-rated portable oxygen concentrators in the industry such as the Caire FreeStyle Comfort, Inogen One G5, and the GCE Zen-O Lite. When you contact one of our oxygen concentrator specialists, they will work with you one-on-one to understand your needs and align you with a concentrator that matches them. We also have many different buying and financing options to help you manage payments in a way that works with your budget. To get started, simply give us a call or send us an email.
.png)
For the majority of people, summer is the best time for being active. No matter what type of physical exercise you like to do, everything tends to be more enjoyable and productive when it’s done outside rather than inside. What’s more, studies have shown many health benefits to being outdoors including lowering blood pressure, reducing stress, and preventing insomnia, a sleep disorder that often results from a lack of sunlight during the day.
On the other hand, if you have COPD or any number of chronic respiratory conditions, you may find it difficult to exercise during the summer. Hot weather can exacerbate your respiratory symptoms and sap your energy making you feel unmotivated to face the challenges of your disease. Additionally, several allergens such as pollen, mold, and insect bites are at their peak in the summer months, which can lead to a whole host of problems for COPD patients as well.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Despite the challenges of staying active during the summer, it’s imperative that COPD patients do so. Exercise is a key part of any treatment regime because it strengthens the lungs and makes your body more efficient at using oxygen, thereby reducing symptoms of breathlessness and fatigue. By having strong stabilizing muscles that you enhance by exercising, you’ll be able to reduce your risk of experiencing a fall or any other type of physical injury. In the following sections, we’re going to take a look at a couple of tips for staying active in the summer if you have COPD. Please don’t hesitate to leave a comment at the end of the article if you have any questions or concerns.
Plan Your Trips Carefully
The first, and probably the most crucial tip to help you stay active during the summer is to plan your trips carefully. Depending on where you are in the country, weather can be variable and sometimes even unpredictable. You should get in the habit of checking the weather regularly and comparing it across multiple sites so that you have a good picture of what the weather will be like. Even then, weather forecasts are never perfect so you should always plan for the worst-case scenario.

Generally speaking, the hottest time of the day is in the afternoon, so ideally, you’ll want to plan your outdoor activities in the morning or in the evening. However, this can vary if there is cloud coverage or precipitation. Since everyone with COPD has different severities of respiratory symptoms, it’s difficult to say what temperature is “too hot.” Most people know their limits and you may have a higher tolerance for hot weather if you’ve spent most of your life in a hot climate. According to Science Direct, about 4% of the population is heat intolerant. This means that they are not able to acclimate to high degrees of heat stress.

Aside from checking the weather before you leave the house, you should also check the air quality in your area. Summer is wildfire season in much of the country and there’s also a high risk of allergens like pollen and mold. And although car exhaust tends to dissipate better in the summer than in the winter, it’s still possible for there to be a lot of pollution during the summer, especially if it’s a little cooler and overcast.
Dress for the Weather
The way you dress can have an immense impact on how you tolerate heat while you’re outdoors. Short-sleeve, loose-fitting clothing is always ideal if you’re going to be outside for an extended period of time and you should be sure to wear lighter colors that reflect more heat. Another important thing to consider is the material of clothing that you wear. Breathable materials like cotton, polyester, and nylon are very light and perfect for a hot summer day. But you should be sure to avoid heavy materials like wool and insulated clothing like rain-resistant shirts or pants.

Another must-have article of clothing for a sunny day is a hat. If your face and head are exposed to too much sunlight you’ll feel fatigued much quicker and you might start to get a bad headache. You’re going to want to wear a wide-brimmed hat that keeps the sun off your face, head, and neck, but just like your shirt, it should be made of breathable material. According to the University of Michigan, 50% of the body’s heat is released from the scalp and face.
Stay Hydrated
When it’s hot out, your body releases more sweat in order to keep you cool. And since sweat is 99% water, you can become dehydrated very quickly by being out in the sun. The CDC recommends drinking at least 8 ounces of water every 20 minutes while you’re outside. And ideally, you should be drinking in consistent intervals so that your body isn’t working so hard to process it all at once. But you should also take care to stay hydrated before you exercise outdoors, not just during your exercise.
.jpg)
Equally important as drinking enough water is avoiding drinks or food that can dehydrate you. While salty foods may sound tempting while you’re outside exercising, be aware that you will have to drink more water to accommodate this. And while sugary sports drinks or energy drinks may give you a nice boost before exercising, they can also dehydrate you and you’ll experience an energy crash after its effects wear off. Ideally, you should stick with water and unsalted foods while exercising in the heat.
Keep Medications on Hand
Just like any other time you leave the home, you need to make sure you have all of the medications you need. Many COPD patients use fast-acting bronchodilators which are designed to quickly release tension in the chest and airways if you’re experiencing a flare-up or exacerbation of your symptoms. These are especially important to have on hand when you’re exercising and away from home because you won’t have many other options for alleviating your symptoms.

Know the Warning Signs of Heat-Related Illness
The easiest way to prevent heat-related illness is to simply know the warning signs. The sooner you realize that your body is overheating, the sooner you can make it to a shaded area or air-conditioned building so that you can begin to recover. Heat exhaustion can happen slowly over the course of a couple of hours or it can come on very quickly so you should always be on the lookout for any symptoms. According to Healthline, there are three different stages of heat emergency: heat cramps, heat exhaustion, and heatstroke.

Heat cramps are more common in older people who have been physically active. They’re also more common in people who are overweight or who have been drinking alcohol recently. The primary symptoms of heat cramps are muscle pain and tightness. The second stage of heat emergency is heat exhaustion which comprises a list of potential symptoms including:
- Headache
- Dizziness
- Mild confusion
- A fast heart rate or fast breathing
- Extreme thirst
- Nausea
- Heavy sweating
-
Muscle cramps
Heatstroke is the most severe form of heat emergency and it can include all of the aforementioned symptoms in addition to:
- Confusion
- Irrational behavior
- A body temperature over 104°F
- Rapid breathing or heart rate
- Loss of consciousness
- Seizures
If you’re outside exercising with a friend make sure that they are also aware of these symptoms and don’t be afraid to check up on each other regularly.
Focus on Moderate Exercise
One of the key mistakes many people make when starting their pulmonary rehabilitation routine is believing that they need to practice high-intensity exercise in order to stay healthy. However, for most COPD patients, high-intensity exercise is not necessary and it can even lead to a respiratory exacerbation if you’re not careful. What’s more important than anything is that you’re consistent with your exercise and that you don’t stay sedentary for long periods of time. Walking, hiking or moderate weight lifting exercises can all be beneficial for lung health.
![]()
Have a Safety Net in Place
A safety net is a must when you leave the house during the summer. Before you do anything, make sure to tell at least one person where you will be going and how long you will be gone. This way, if there’s an emergency, your friend or loved one will know exactly where to look for you. Secondly, you should create a list of contacts of people that you can call if you experience a flare-up in your symptoms and don’t feel comfortable driving or walking home alone. However, if you believe you’re experiencing a medical emergency, you should always call 9-1-1 first.
Use a Portable Oxygen Concentrator
There comes a time when oxygen tanks become too much to manage. While supplemental oxygen is a medical necessity for most COPD patients, oxygen tanks are extremely heavy and bulky making it difficult to get out of the house and enjoy the outdoors. Fortunately, there are alternatives to traditional oxygen tanks and they’re called portable oxygen concentrators. A portable oxygen concentrator puts out medical-grade oxygen just like a tank, but the difference is that it’s an electronic device that runs on batteries. Simply have a fully charged battery on hand and you’ll have access to an infinite supply of oxygen.

Another great thing about portable oxygen concentrators is that they’re very easy to operate so you won’t have any problems making adjustments to your flow setting on the go. POCs like the Caire FreeStyle Comfort and Inogen One G5 only have a few buttons on them so you can have it up and running in just a few minutes and feel confident about using it outside of the home. Both of these concentrators offer a high flow setting and they weigh under 5 pounds meaning they’re incredibly versatile. Most POCs also have a DC charging option available, so you won’t have to worry about running down your battery while you’re driving to whatever destination you’re going to.

All things considered, portable oxygen concentrators are a much more financially sound and practical long-term investment. While they do cost more money upfront than oxygen tanks, the important thing to remember is that you don’t have to keep paying to refill them. In the long term, this could save you hundreds if not thousands of dollars. What’s more, POCs often come with manufacturer warranties which will have you covered if anything goes wrong with your unit within the first couple of years after your purchase.
Speak with Your Doctor
As always, if you have any concerns about being able to cope with the hot weather this summer, you should address them with your doctor. Heat-related illness is a potentially serious condition. According to the CDC, there are about 702 heat-related deaths in the United States each year. Unfortunately, due to the symptoms of COPD including chronic breathlessness and fatigue, COPD patients are oftentimes at a higher risk of experiencing heat-related illness than the general public. This study found that hospitalization in COPD patients increased by 7.6% for each degree Celcius over 29°C (84°F).
As aforementioned, no two cases of COPD are the same so it’s impossible to say what advice your doctor will have for you. If you have more severe stage 3 or 4 COPD and heat-related illness runs in your family, he/she will likely recommend that you use a high degree of caution when it comes to exercising outdoors. But if you’re stage 1 or 2 and you don’t use oxygen regularly, your doctor’s guidelines might be a little more lenient.
Conclusion
As a COPD patient, consistent exercise is very important for your well-being. But severe weather conditions like high heat or excessive dryness or humidity can make this seem like an insurmountable task. So, if you want to exercise outdoor this summer, you should take some time to plan ahead, and as always, if you have any questions about coping with extreme weather, be sure to address them with your doctor or pulmonologist as soon as possible.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you’re looking for a brand new, used, or refurbished portable oxygen concentrator to help you get on your feet this summer, look no further than LPT Medical. We proudly offer pulse dose and continuous flow oxygen concentrators from some of the most reputable manufacturers on the market including but not limited to Caire, Inogen, and AirSep. While there are many different concentrators out there, our respiratory specialists will take the time to understand your wants and needs and recommend the perfect device for you. We also have a variety of different financing options available to help you pay off the device in a more manageable way. Reach out to us either by phone or email to speak with an oxygen concentrator specialist.

COPD, or chronic obstructive pulmonary disease, is a group of progressive lung diseases, the most common being emphysema and chronic bronchitis.
There are several benefits of mind-body exercise for people with chronic conditions, and even more specific exercise can be done if you have a chronic respiratory disease like COPD that are designed to stretch your muscles and open your airways.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In studies done looking at the benefits of yoga and tai chi for COPD patients showed how yoga postures, breathing exercises, and tai chi movements gave COPD patients overall improvement to their quality of life, and physical tests showed that their lung function improved!
Tai Chi

Tai chi may be the best exercise for you If yoga feels too hard and meditation feels too easy. Tai chi is a good balance between the two. Studies show that Tai Chi has a number of benefits for people with chronic obstructive pulmonary disease (COPD).
How can tai chi help with COPD?
Tai chi is a combination of slow flowing movements linked with breathing, and it is an ancient Chinese martial art. This is a great practice for COPD patients in any stage of the disease, because Tai chi exercises can be done standing or sitting.
This is also a great exercise option if you have limited resources, because no special equipment is needed. You just wear loose clothing, you need about a yoga mat's worth of space to preform the movements!
It may seem as if these movements are extremely easy, but the power you generate from the motion of the poses and the connection with your breath cultivates strength. It's great too, because these exercises are low-impact.

Not only does tai chi help strengthen your body, it can reduce stress, anxiety, and depression.
There has been a lifetime of experiments and research that explains how tai chi can help people with medical conditions like heart disease, osteoarthritis, and Parkinson’s disease. And now it is known that tai chi has significantly improved the quality of life for people with COPD.
It is also very likely that if you decide to join a pulmonary rehabilitation program that tai chi will be an effective part of your program.

Research about tai chi and COPD
Tai chi is commonly known to help many people with certain chronic conditions, and so there were additional studies done that would prove whether or not tai chi could improve the quality of life for people with COPD.

In an experiment, they tracked 120 people with COPD, half of the people were put on a traditional pulmonary rehabilitation program, and the other half were enrolled in a tai chi class.
In conclusion, the group of COPD patients who did tai chi had better scores in a survey about their respiratory health and they also performed better during a respiratory walking test.
Do you want to start doing tai chi?
If you think tai chi sounds interesting, the first step will be to get in contact with your doctor, talk to them about tai chi and whether or not this is a good exercise for you personally. Talking with your health care team is also a great way to learn about tai chi classes in your local area, and they may be able to recommend one.
They can also recommend online classes that would be a good fit for your respiratory level!

Tai chi has become very popular and during the pandemic, online workout courses became much more common, so if you like to exercise in the comfort of your home rather than go to a class, you could find classes to take online. Try searching for “beginner tai chi” or “tai chi basics” or “tai chi for people with respiratory health issues”.
There are usually tai chi classes at your local health club or gym, at community centers, or senior citizen organizations. You can also check your local hospital or healthcare center for a tai chi program.
Yoga

Yoga can be a great form of exercise if you have COPD because it is low-impact and can help to improve both your mental and physical health.
Yoga stands to benefit your health by:
- Lowering blood pressure
- Increasing relaxation and self-confidence
- Reducing stress and anxiety
- Improving fitness
Yoga will help you stay fit, flexible, and relaxed. There are different degrees of yoga classes, and there are specific yoga classes taught for people who are diagnosed with health conditions like COPD.
Yoga is a combination of physical postures and breathing techniques. Meditation and relaxation can be a big part of certain yoga practices as well.
The Physical Yoga Postures
Performing the physical postures of yoga can help improve your body’s ability to perform physical activity and will increase your:
- range of motion
- balance
- flexibility
- strength
Yoga postures can ultimately improve your energy levels and clear your mind from worry, and they also cultivate strength in your muscles and lungs.
Breathing Techniques
Breathing techniques can help utilize your breath more efficiently and teach you how to use your lungs more fully. Yoga is so great for COPD patients because these breathing exercises as you do the postures encourages your breath work outside of yoga and in your everyday life.
Benefits of Yoga for People with COPD
If you have COPD, taking a regular yoga class could be too much physically, and so modified versions of yoga have been developed so that you are capable of the practice without over-exercising.
Modified yoga classes are created with the health needs of people with COPD in mind and should provide you with a gentle, easy, and effective way to manage your health and emotional well-being.

The gentle stretches help to improve fitness and flexibility, while breathing exercises give you skills to manage any attacks of breathlessness. The techniques you learn should also be easy enough so you can practice at home.
Breathing techniques can help you manage symptoms of breathlessness by strengthening your respiratory muscles even when you are not doing yoga! The benefits of yoga spread into your daily life, and help you breathe better but will also help you manage stress and anxiety.
Yoga teaches you how to indulge in deep relaxation through breathing and meditation techniques. This helps to relieve stress and tension.

Before taking any yoga class, even if it is a class for people with your health condition, always consult your healthcare provider to get clearance before practicing any form of exercise. If your class is a normal yoga class that was not designed for people with COPD, check that your yoga teacher understands your needs as a person with COPD.
The right yoga teacher will show you how to breathe correctly in order to enhance your yoga practice and will give you modifications of poses that you are capable of doing.
You can try some of these yoga postures which can help you build strength and encourage healthy breathing:
Standing Mountain Pose
Stand tall to open up your chest. Your arms can be raised. or left at your sides.

Standing Backbend
This pose also helps to open up the muscles of your chest but needs to be practiced carefully to avoid muscle strain and breathlessness.

Seated Forward Folds
These poses help strengthen your respiratory system.

Standing Side Bends
These bends will help strengthen your diaphragm while also improving the flexibility of your rib cage.

Breathing exercises
Breathing correctly brings more oxygen into your blood and cultivates vital energy for your muscles and brain. Good breath helps your mind and body.
Pursed-lip breathing and diaphragm breathing are two of the most common breathing techniques for COPD and both have roots in yoga. They are often taught to people with COPD as part of their pulmonary rehabilitation program.
Exercising safely with COPD

Yoga and Tai Chi are generally safe ways to get in shape, but there are always things to be aware of, and if you have COPD be sure to take these precautions just to be sure.
Ask your doctor before performing any new exercise, they will have advice for practicing your exercise safely and considering your oxygen levels be able to recommend how much exercise you should be getting, so you get enough but also not too much. Your healthcare team may also have yoga classes or tai chi classes for COPD in your area.

Check the credentials of any yoga instructor or tai chi teacher before you begin classes and make sure they know about your condition and health needs before beginning the class.
The best thing about yoga and tai chi, is that you are practicing your own exercise, and there are no expectations to do anything that is uncomfortable or harmful to your body. Therefore, you should avoid any poses that restrict your breathing and put pressure on your diaphragm. Examples of yoga poses you should avoid are Child’s Pose or the Plough.
Yoga and tai chi are exercises meaning your heart rate could increase and your breathing can also speed up. Be prepared for this, and keep your inhalers or portable oxygen device close by when practicing tai chi, yoga, or any form of exercise.

Stop exercising immediately if you experience shortness of breath while exercising, taking breaks and allowing yourself to catch your breath is a helpful tool to use when you are experiencing an exacerbation or flare up. Use your medication and rest until you feel well enough to begin again.
Exercise for COPD Patients
It is way too common for COPD patients to not get enough exercise, and this is because they think that feeling breathless and tired is bad for their lungs, but this is not true. For COPD patients, it is crucial to get some exercise daily. Without exercise you will become less physically fit, and your breathing will get worse.
Overview

Exercises that are incredibly important for COPD patients include aerobic exercises, strength and conditioning, and breathing exercise. Yoga and tai chi are two forms of exercise that help with all of those aspects of exercise and they also help improve flexibility and mental health!
Tai Chi and yoga are two forms of exercise that can help COPD patients improve their blood pressure, help with relaxation and self-confidence, reduce stress and anxiety, and will help improve their overall fitness.
Keep an open mind and if your doctor agrees that yoga or tai chi would be a good option to improve your health, give it a try!


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!