Chronic obstructive pulmonary disease (COPD) is one of the most common lung diseases in the world. It’s estimated that about 16.4 million people in the United States alone have COPD and millions more are either undiagnosed or at high risk of contracting it. Despite this fact, many people are woefully unaware of what causes this disease and how it should best be managed.
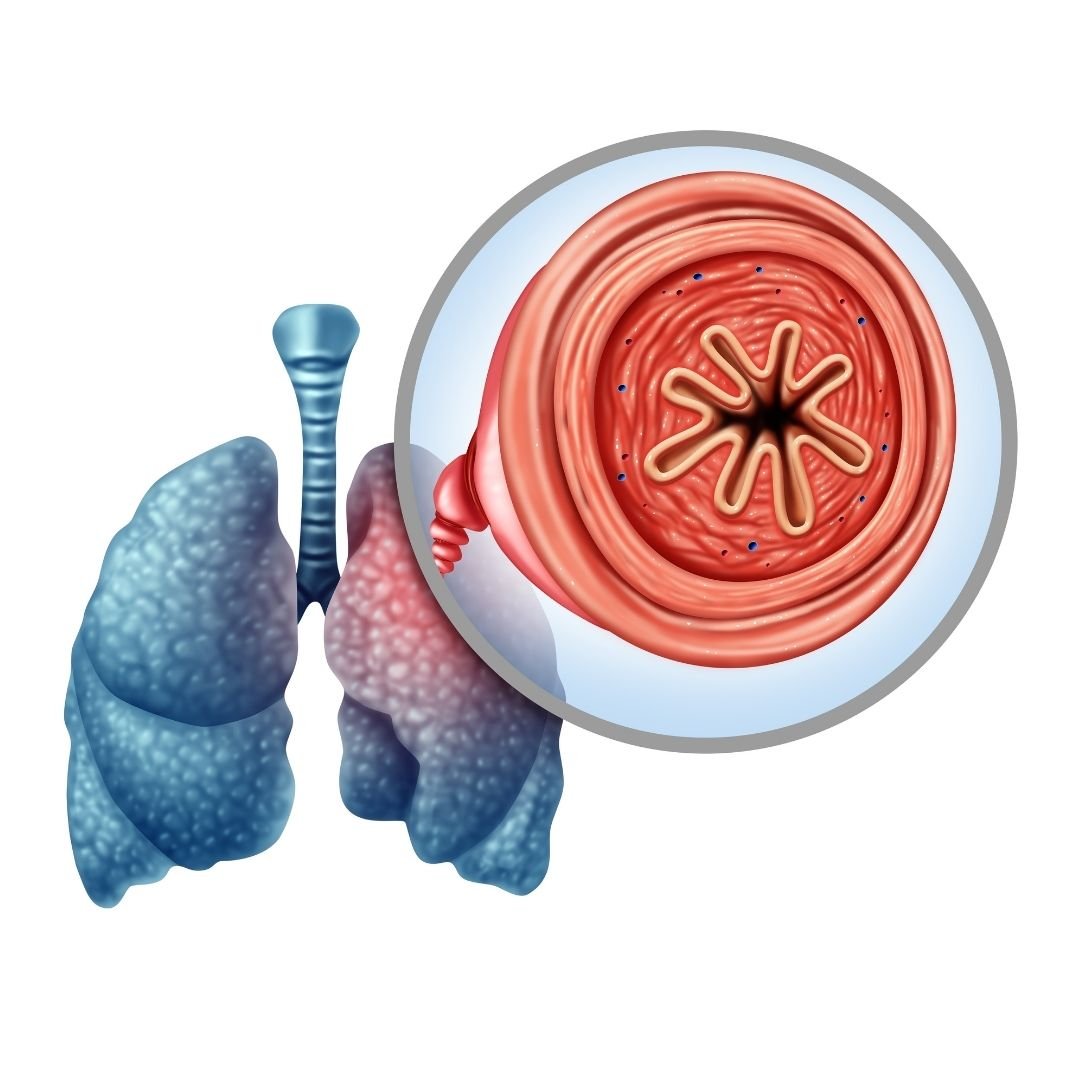
In short, COPD is an umbrella term that denotes two conditions: chronic bronchitis and emphysema. While the symptoms and pathogenesis of these two diseases are slightly different, they are both primarily caused by cigarette smoking. However, in rare instances, someone who has never smoked can contract COPD through something called alpha-1 antitrypsin deficiency (AAT deficiency).
One of the symptoms of COPD that’s particularly vicious is something called an exacerbation. This is similar to an asthma attack in that it causes respiratory symptoms such as breathlessness, chest pain, and sputum production to suddenly become worse, oftentimes requiring you to seek immediate medical attention. In this post, we will help you better understand COPD flare-ups and exacerbations, as well as how to avoid being hospitalized as a result.
If you have any questions or concerns, feel free to leave them in the comment section so we can address them.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What’s the Difference Between a Flare-Up and an Exacerbation?
Generally speaking, the terms “COPD flare-up” and “COPD exacerbation” are used interchangeably. They both refer to respiratory symptoms becoming worse due to environmental causes, infections, or any number of other things. However, when it comes to discussing these symptoms, it’s important to be precise not only about what’s causing them but how severe they are as well.

A mild COPD exacerbation is one that could lead to increased discomfort but is unlikely to cause any serious long-term consequences. These can typically be treated with short-acting bronchodilators (SABD) or “rescue inhalers” which work to quickly open up the airways allowing you to breathe better. Moderate COPD exacerbations should be supplemented with oral corticosteroids which suppress inflammation and antibiotics which can help fight inflammation.

The final type of exacerbation is a severe exacerbation, sometimes called an “acute” exacerbation. This type of exacerbation requires immediate medical attention and can even be life-threatening if it’s not treated appropriately. Ideally, the best way to prepare for this type of exacerbation is to have an action plan and ensure you always have someone on hand to either take you to the hospital or call an ambulance.
Why it’s so Important to Avoid Hospitalization With COPD
According to the American Journal of Respiratory and Critical Care Medicine, COPD is responsible for $72 billion a year in direct healthcare expenditures. The majority of these costs come from hospital visits which range from 4.5 to 8.8 days on average. Around two-thirds of all COPD hospitalizations are due to COPD exacerbations, and the majority of COPD exacerbations are caused by infections — specifically viral infections.

The primary reason it’s important to avoid hospitalization for COPD is because of the risks for your health. According to another study by the aforementioned medical journal, after testing over 2 million patients, the 1-year readmission rate was 64.2% and the 1-year mortality rate was 26.2% both of which were significantly higher than rates among the general COPD population. Readmission and mortality rates are also much higher among patients who were hospitalized with severe exacerbation of COPD.
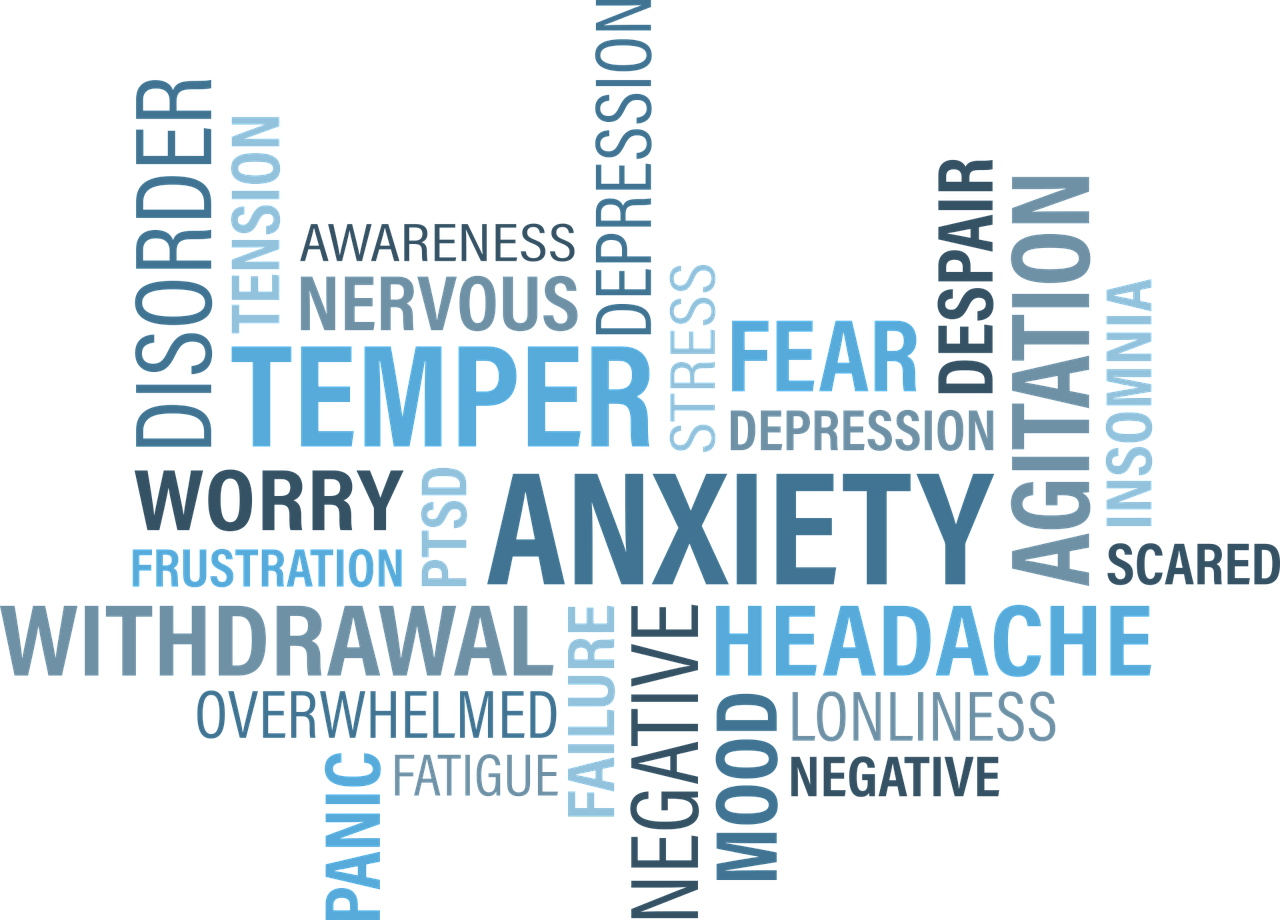
The second most important reason to avoid hospitalization due to COPD is cost. Frequent or long-term admissions can pose a significant financial burden on people with COPD which can also lead to stress, anxiety, and even depression. In our last post, we highlighted some key ways that you can avoid unnecessary financial costs due to COPD so check it out if you’re interested in learning more.
Have a Plan to Deal With Exacerbations
First and foremost, if you want to avoid hospitalization due to COPD exacerbation, you need to have a plan of action before an emergency occurs. An action plan is a sort of written outline that you will follow in order to accomplish a certain goal. This way, if you notice your COPD symptoms starting to worsen, you can refer to your sheet instead of worrying about making difficult decisions at the moment.

In order to prepare your COPD action plan, you should first consult your doctor. He/she will likely already have a template that you can fill out to make this process a little easier. On this action plan, you will need to create an “action” for every symptom you experience. For example, if the symptom is a gradual decrease in your blood oxygen levels, you might make a note to increase your oxygen flow setting or contact your doctor. If you experience sudden shortness of breath, you might make a note to use your rescue inhaler.
Another important thing to know about your COPD action plan is that it should not be private information. You should make it a priority to go over your plan with friends and family, especially if they spend a lot of time with you. This way, if you are in a situation where you are unable to act out your action plan, they will be able to help. In this post, we discuss how you can prepare for medical emergencies and hospital visits with COPD, so check it out if you want to know more.
![]()
Change Up Your Diet
Diet can be a very difficult topic to discuss in this day and age. Most people have access to more types of food than ever before and there is a near endless list of diets that people swear by. As a result, it can feel like an insurmountable task trying to find something that keeps you happy and healthy. The good news, however, is that many years of research have been dedicated to COPD diets, so you shouldn’t have to do much scrambling to make sense of it all.
![]()
Generally speaking, COPD patients should maintain a diet that’s high in protein, fiber, and fat, but low in carbohydrates. The reason for this is that the metabolism of carbs produces the highest amount of carbon dioxide in the body while the metabolism of fat produces the least. Adequate protein ensures your respiratory muscles stay strong and efficient, and fiber helps to control blood glucose levels and reduce cholesterol in the blood.
Another reason to keep your diet healthy, natural foods rather than processed ones is because weight management is vital to COPD management. Most often, people tend to become underweight after contracting COPD due to a loss of appetite or other factors. Sometimes, people experience a loss of appetite because consuming food is more physically exerting than it was previously, and bloating can contribute to breathing difficulties. COPD patients who are underweight may find that they lack the energy or endurance to make it through the day.
On the other hand, being overweight with COPD can contribute to breathing problems as well. While it is less common for a COPD patient to become overweight than underweight, the problems associated with it can be just as severe. Simply put, having a higher body mass index (BMI) can be obstructive to your breathing by putting more strain on your lungs when you inhale. However, some studies have found mixed results when it comes to being overweight/obese with COPD.
Be Consistent With Your Exercise Routine
Consistency is unbelievably important when it comes to treating COPD and preventing exacerbations. For example, your diet is much more likely to benefit you if you keep up with your goals week in and week out. But if you do well one week then cheat the next, you’re going to put yourself at a much higher risk of COPD complications like exacerbations. This works pretty much the same way when it comes to your exercise routine.

Oftentimes, exercise specialists will talk about getting into a “routine.” In other words, you do the same exercise each day for an allotted period of time. By doing so, it will be much easier to track your progress and catch yourself when you fall back on your plan. This works well for most people who want to commit to an exercise routine, but it’s especially useful for COPD patients who benefit more from consistent moderate exercise rather than high-intensity exercise.
Avoid Getting Sick
Lung infection is both the number one cause of severe COPD exacerbation and the number one cause of hospitalization due to COPD. With that being said, staying healthy and avoiding infection (especially lung infections) is vital. One of the best things you can do right now to avoid getting sick is to quit smoking or avoid second-hand smoke if you live around smokers.
It’s been known for quite some time that smoking reduces the immune response in the body and also makes the smoker more likely to have exaggerated responses to viral infections. During influenza outbreaks and with the current situation we face involving COVID-19, smokers have a much lower survival rate when compared to the general population. Not to mention that smoking and second-hand smoke can trigger COPD exacerbations even if an infection isn’t present.

Another thing you can do to avoid getting sick is to be more conscious of your daily habits. For example, do you wash your hands frequently throughout the day? Do you take care to avoid places that are unclean or unsanitary? Do you stay away from people who exhibit symptoms of the cold or the flu? Do you clean surfaces in your home like door handles, coffee pot handles, or faucet handles? Are you following all the precautions recommended by the World Health Organization (WHO) in order to prevent contracting the novel coronavirus?
Last but certainly not least, you should be getting the doctor-recommended eight hours of sleep each night in order to avoid getting sick. According to WebMD, sleep deprivation suppresses the immune system and puts you at a higher risk of contracting colds, the flu, and other ailments. This is an especially difficult topic for many COPD patients because respiratory symptoms can make it difficult to maintain a healthy sleep schedule. In this post, we take a look at some actionable tips to improve your sleep if you have COPD.
Avoid Environmental Triggers
It can be a scary world out there for anyone who values their lung health. From wildfire smoke to car exhaust and pollen, it’s easy to feel like no place is safe. The Environmental Protection Agency (EPA) even reports that indoor air can be two to five times more polluted than outdoor air. Fortunately, it’s not all grim news for COPD patients who want to avoid exacerbation triggers. Just by following a few simple steps, you’ll be well on your way to avoiding the most common triggers.

Despite summer ending last week, we are still in the midst of wildfire season. As a result, COPD patients need to be aware of when they go outside, especially when it concerns exercising outdoors. Air quality index (AQI) is the measurement we use to determine how safe outdoor air is to breathe. Each day before you go outside, be sure to check AirNow.gov for the AQI in your area. If the AQI is above 100, this is a sign that the air quality is too poor for people with lung diseases like COPD, asthma, or pulmonary fibrosis.
Another thing you should be wary of is seasonal allergies. Contrary to popular belief, allergies are a reality during all times of the year as opposed to only being active during certain seasons. In September and October, allergens like ragweed are typically at their peak. According to WebMD, if you get allergies in the spring, you are about 75% likely to have reactions to ragweed. So, if you’re outside this trying to enjoy the fall colors and cool weather this year, just be aware that allergies are still a reality.

The final airborne COPD exacerbation triggers we’d like to talk about are the ones found in your home. Like we mentioned earlier, indoor air can potentially be more dangerous than outdoor air. This is because the air in your home is extremely concentrated, so if you track things in like dust, allergens, or smoke, it will likely start to build up in one area of your home unless you take the time to clean regularly. While it may not seem that important, taking the time to vacuum, dust, and wipe down surfaces every day can go a long way to preventing COPD exacerbations. What’s more, it will help you get your daily exercise.
Use a Reliable Portable Oxygen Machine
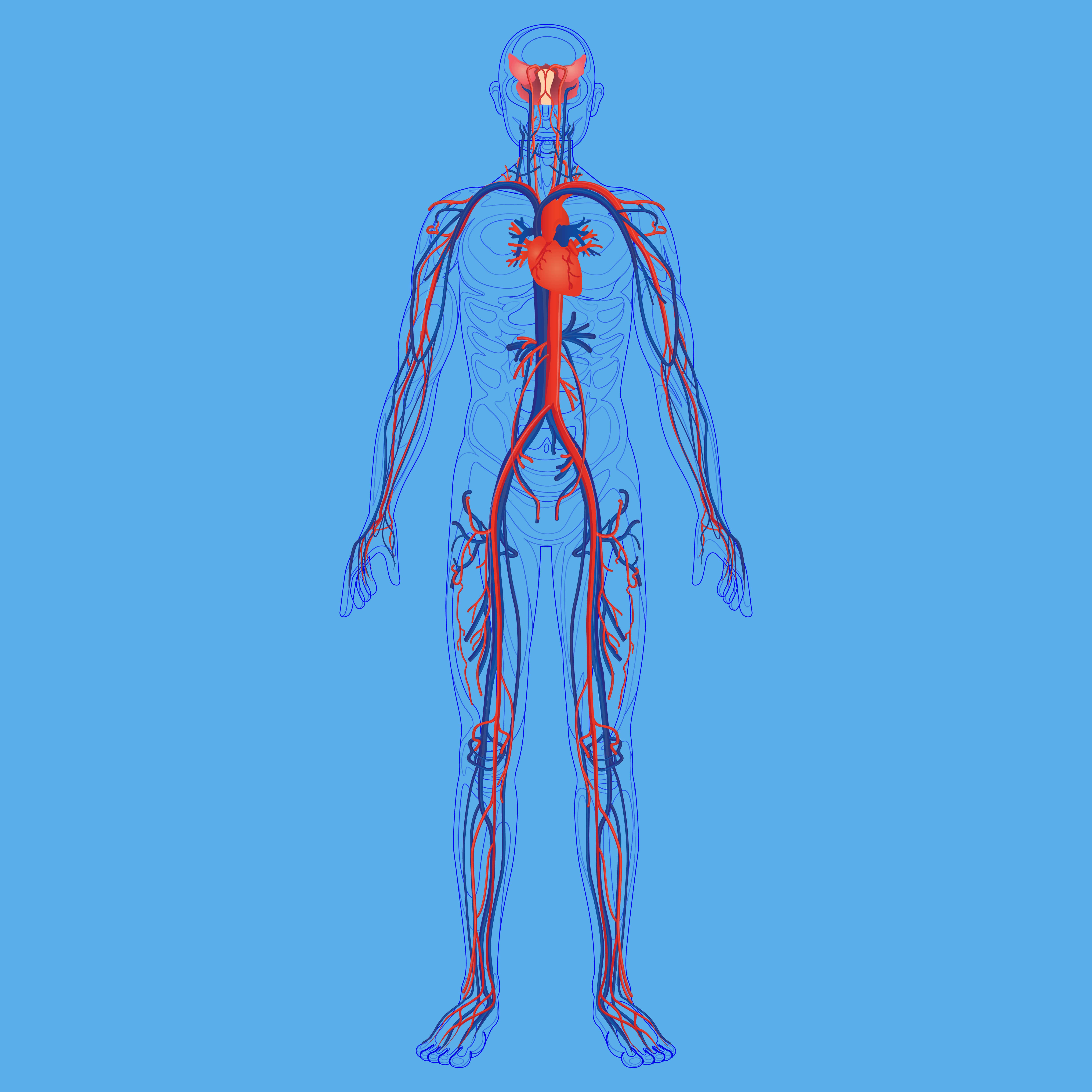
Last but certainly not least, having a reliable portable oxygen device that you can take anywhere will put you in the best position to avoid COPD exacerbations and hospitalization. For the vast majority of COPD patients, supplemental oxygen therapy is a medical necessity. Not only does it stabilize your lung condition, but it also ensures your blood oxygen levels are normal, which in turn saturates every organ in your body with the oxygen it needs to function properly.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
For the foreseeable future, portable oxygen concentrators are your best bet for reliable portable oxygen. Unlike oxygen tanks or liquid oxygen tanks, portable oxygen concentrators are electronic devices. So, instead of having to go out of your way constantly to have your tanks refilled by an oxygen specialist, you simply need to carry batteries with you. Fortunately, these batteries are lightweight and don’t take up very much space in your backpack or handbag.

Currently, the best portable oxygen concentrator on the market is the Caire FreeStyle Comfort. It weighs in at only 5 pounds and it offers 5 different flow settings that you can adjust on the fly as needed. One of the unique features of the FreeStyle Comfort is its ergonomic design which keeps the device comfortably at your side rather than jostling around as some other concentrators do.

Another portable oxygen concentrator we’d like to recommend is the Inogen One G5. While this POC came out last year, it’s still very relevant and a great choice for anyone who needs a reliable 24/7 medical oxygen supply. The Inogen One G5 has one more pulse flow setting than the FreeStyle Comfort and it weighs slightly less at just 4.7 pounds. Inogen is one of the top brands in the medical oxygen industry and they take pride in customer satisfaction.
In rare instances, your doctor may require you to use a continuous flow concentrator. If this is the case, we recommend the Respironics SimplyGo portable oxygen concentrator. This unit is twice as heavy as the Caire FreeStyle Comfort, but since it puts out a continuous flow of oxygen, it can be used with your CPAP or BiPAP machine if you have sleep apnea or another related sleeping disorder. If you’re looking for affordable portable oxygen concentrators, don’t hesitate to visit our online oxygen store.

Conclusion
Unfortunately, exacerbations and flare-ups are a reality for COPD patients. But that doesn’t mean that you can’t take steps to reduce your risk of experiencing hospitalization due to an exacerbation. Above all, following your treatment plan as closely as possible and preventing sickness like the cold or flu will be your best bet if you want to avoid hospital visits.
If you would like to learn more about managing chronic respiratory conditions such as COPD, stay tuned to our blog. We aim to equip our readers with the knowledge they need to combat breathlessness, chest pain, and fatigue in their daily lives, as well as learning how to cope with the mental aspects of chronic disease like anxiety and depression. Feel free to leave a comment below if you have any questions or concerns.
.png)
Chronic obstructive pulmonary disease (COPD) is one of the diseases with the greatest financial burdens worldwide and within the United States. Studies have shown that the average annual COPD-related expenditure is around $4,147. And while 51% of these costs are covered by Medicare according to the Centers for Disease Control and Prevention (CDC), that still leaves roughly $2,000 a year that COPD patients need to spend out-of-pocket. Combine this with the cost of aging and limited retirement funds and it’s not hard to see why COPD is such a major financial burden for so many people.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Without a doubt, the later stages of COPD pose the greatest burden for most people. It’s during end-stage COPD that you’re most likely to experience hospitalization due to exacerbation and you’re also more likely to be hospitalized for an extended period of time. Since symptoms tend to develop more quickly during this time, you’re also more likely to schedule more doctor’s appointments, use your medication more frequently, and seek out other treatment options for your disease.
In this post, we’re going to discuss end-stage COPD (also called late-stage or stage 4 COPD). We’ll take a closer look at what exactly this term means, what to expect, and how to prepare for this stage of COPD in order to mitigate some of the physical and financial challenges it poses. If you have any questions, either leave them in the comment section below or reach out to your doctor to schedule an appointment.
What is End-Stage Chronic Obstructive Pulmonary Disease?
Since COPD is a long-term condition that progresses slowly, it’s generally divided into four different stages. These stages help healthcare specialists identify the symptoms of your disease, predict the prognosis of your disease, as well as your life expectancy. And because COPD manifests differently in every patient, that also means the stages are going to look different for everyone. While researchers have a good idea of the average life expectancy of someone with COPD, what ultimately matters is your own health. In this way, it’s often better to think of COPD as a sort of “catalyst” for other health issues.

The best way to know that you’re approaching late-stage COPD is based on your symptoms. Someone with end-stage COPD will likely experience similar symptoms that they’ve experienced for many years such as coughing, breathlessness, fatigue, or chronic pain. In end-stage, however, these symptoms become significantly more debilitating to the point where they may need to rely on caretakers, friends, or loved ones to take care of them. They’ll also experience more frequent trips to the hospital due to flare-ups and exacerbations.
-jpg.jpeg)
The term “end-stage” is controversial in many ways because it can imply that the patient doesn’t have much time left to live, but this isn’t always the case. Even when it’s evident that symptoms are increasing in frequency and severity, that doesn’t mean that won’t outlive them and go on to live many more years. However, using this term can be helpful when it comes to planning and the approach that you use to treat your disease. For example, some people prefer to switch to palliative care which is a type of specialized medical care that’s focused on optimizing a patient’s quality of life and ease discomfort.
How to Recognize End-Stage COPD
As aforementioned, late-stage COPD looks different for everyone. This is why it’s important to maintain open lines of communication with your doctor who can provide you with detailed information about your disease prognosis as well as advice on how to plan. Generally speaking, however, you’ll be able to notice an increase in the frequency and severity of symptoms you’re experiencing. Take a look at some of the symptoms below and see if you notice any similarities to what you’re experiencing.
- You experience heavy coughing or wheezing throughout the day
- You experience shortness of breath even while at rest
- You lack the energy or will to maintain your diet
- You’re becoming more reliant on friends and family for simple tasks
- You experience dizziness, confusion, or trouble sleeping
- You experience more frequent or severe exacerbations that lead to hospitalization
Another way to recognize end-stage COPD is by performing a spirometry test. A spirometer is a simple device used to derive two different results: Forced Expiratory Volume in one second (FEV1) and Forced Vital Capacity (FVC). Combined, these results will tell you how well your lungs are functioning, and if you have spirometry results already, you and your doctor will be able to compare them to determine how quickly your lungs are deteriorating. FEV1 refers to the total amount of air you can force from your lungs in one second and FVC refers to the total amount of air you can expel from the lungs in one breath.

From a diagnostic perspective, stage four COPD is recognized as an FEV1/FVC ratio of less than 70% or an FEV1 less than 30%. Even if your FEV1 is above 30%, however, your doctor may classify you as stage four severe COPD if you have chronic respiratory failure. Several other tests your doctor may use to diagnose stage four COPD include lung volume tests, gas diffusion tests which measure how well oxygen moves from the lungs to the bloodstream, and exercise tests.
How to Ease End-Stage COPD Symptoms
All-in-all, your treatment plan for end-stage COPD shouldn’t look all that different from your treatment plan for any other stage of COPD, but you may need to make adjustments based on your physical, mental, and emotional abilities. What’s more, there are several additional strategies you can add to your routine that can ease some of the pain and increase your comfort.
Supplemental Oxygen Therapy
Oxygen therapy is likely the most consistent treatment you’ve used since being diagnosed with COPD. Since COPD leads to progressive lung obstruction, one of the best ways to remedy this is by helping your lungs out and providing them with a higher concentration of oxygen. By doing so, your body will have the resources it needs in order to stay healthy. Unfortunately, many COPD patients use oxygen incorrectly or they use an oxygen device that doesn’t suit their needs and lifestyle.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
When it comes to oxygen delivery devices, there are several options available to you. Oxygen tanks have been around the longest, followed by liquid oxygen tanks, home oxygen concentrators, and portable oxygen concentrators. While each of these can provide you with the oxygen you need, portable oxygen concentrators tend to offer the most comfort and convenience in end-stage COPD. There are many reasons for this, but above all, they don’t need to be refilled.
.png)
Rather than containing compressed oxygen like oxygen tanks do, portable oxygen concentrators run off of powerful lithium-ion batteries which allows you more freedom to move around on your own time. Instead of having to call an oxygen company to deliver full tanks to you, simply plug your POC into any wall outlet and you’ll be able to recharge your batteries. You’ll even be able to use the device while it’s charging.

There are several different types of POCs you can choose from depending on your wants and needs. Pulse dose portable oxygen concentrators like the Caire FreeStyle Comfort or Inogen One G5 closely monitor your breathing and only deliver oxygen when you inhale. These devices are incredibly efficient, lightweight, and small. On the other hand, you could opt for a continuous flow portable oxygen concentrator like the Respironics SimplyGo which provides the user with a constant stream of oxygen. These machines tend to be slightly bigger and bulkier than their counterparts.
Nutritional Counseling
Like we mentioned before, malnutrition is a significant problem that many stage-four COPD patients face. Symptoms like breathlessness and chronic fatigue can lead to a situation where patients simply don’t have the energy to eat or they don’t get the same satisfaction from it that they used to. Conversely, it could lead to someone choosing foods that are convenient and provide a quick energy boost. Unfortunately, these foods tend to also be filled with sugar and other problematic ingredients that don’t provide your body with the nutrients it needs.
If either of these situations sounds like you, it might be a good idea to consider nutritional counseling. This is a type of therapy that’s focused solely on your eating habits and it attempts to break down any barriers you might be facing that are preventing you from sticking with the diet that your doctor has provided for you. Contrary to popular belief, nutritional counseling isn’t just for people facing weight issues, it’s also extremely beneficial for people with chronic illnesses like COPD who struggle to get the nutrients they need. It’s also useful for anyone who believes that they have “unhealthy” or “unproductive” eating habits.
Complementary Therapies
Complementary therapies are any therapy that can help you ease the burdens associated with late-stage COPD. As you can imagine, this varies greatly depending on the patient because everyone faces different issues with their disease. For some, this might mean attending cognitive behavioral therapy (CBT) sessions in order to prevent anxiety or depression, for others it could mean speaking with a spiritual or religious leader who can help you settle any concerns or fears about living out the later stages of your life.

Cognitive behavioral therapy is a type of psycho-social intervention that’s focused on correcting negative or inaccurate thought processes or actions. It’s a type of therapy that’s become very popular among older adults, especially those with chronic conditions, who want to seek more fulfillment in their daily lives. CBT takes place over the course of several weeks, months, or however long it takes for the patient to feel comfortable on their own.
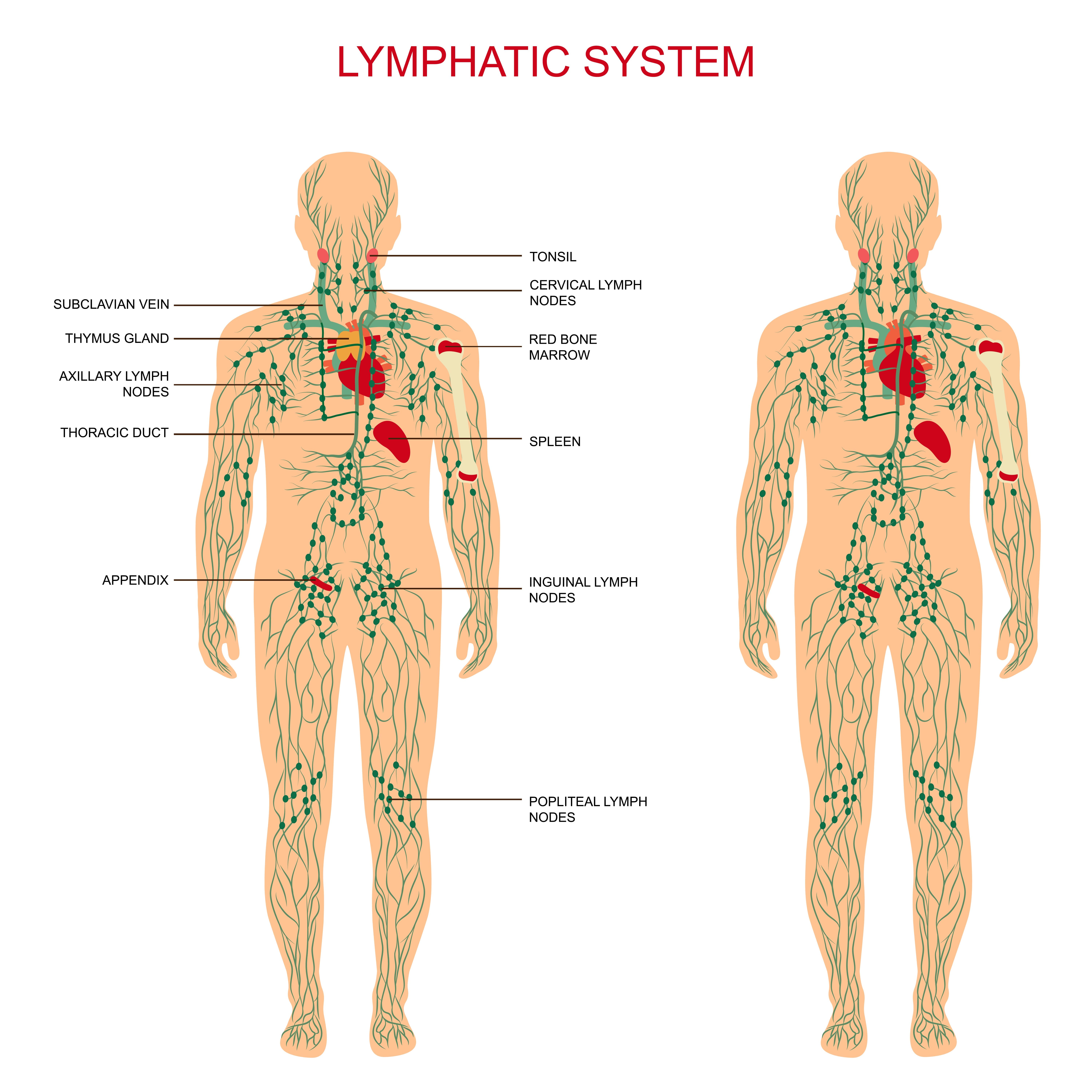
Another type of therapy you might want to consider when it comes time to plan for end-stage COPD is massage therapy. Studies have shown that anxiety can cause a lot of tension to form in our bodies and this tension can lead to more anxiety. Massage therapy is a great way to break this tension causing us to feel better both physically and mentally. According to this medical report, there are two reasons massage therapy is beneficial for COPD patients. Firstly, it causes hyperemia which is the increase of blood flow to different tissues. Secondly, it activates the lymphatic system which is responsible for draining your body of toxins.
A Revised Pulmonary Rehabilitation Routine
Most people are well-aware that with aging comes problems with mobility, endurance, and strength. It’s a natural part of life that we lose a lot of our physical abilities as we get older, but that doesn’t mean you can’t continue to do pulmonary rehabilitation. It simply means that you will need to find new ways to do it. Some people find that the best option for them is to switch to exercises that involve sitting as well as ones that don’t require them to leave the house or meet up with other people.

The important thing to remember is that any form of exercise will benefit your lung health, not just exercises that work your lungs specifically. In many cases, this mindset can even be counterproductive in late-stage COPD because most people don’t have the lung capacity to perform any strenuous endurance exercise that gets your heart rate up. Rather, targeting specific muscle groups in your body will improve your strength and circulation, thus easing some of the burden on your lungs. Studies have shown that muscle requires less oxygen to use and it produces less carbon dioxide as waste, ultimately resulting in less air that your lungs need to take in.

The thing that we would like to stress, like we’ve done many times before, is the importance of consistency when it comes to your pulmonary rehabilitation. Just like maintaining a healthy diet, your exercise routine will be more effective if you are able to do it everyday without letting yourself fall back on your goals. Ideally, you should have someone like a friend or family member who can hold you accountable at least until you are able to do so for yourself.
Address Your Concerns With Your Doctor
Just like with any other stage of COPD, you’re going to want to work closely with your doctor in end-stage COPD. This is because you’ll want to make sure that your goals are in line with or at least not counterproductive towards your treatment goals. Like we mentioned earlier, end-stage COPD should be all about improving your comfort and reducing chronic pain. But this doesn’t mean that you should completely ignore the treatment plan that you’ve followed throughout your whole life with COPD.

Another reason to consult your doctor is because he/she will likely have some helpful resources for you in regards to finding other health specialists such as nutritionists or mental health experts. This will not only save you a lot of time but it will set you off on the right path. You should also make it a priority to visit your doctor more frequently so that you can make healthy choices that fall in line with your COPD treatment plan.
Conclusion
Chronic obstructive pulmonary disease (COPD) is an ailment that develops and progresses over the course of many years — sometimes even decades. This is why it’s important to always be adaptive when it comes to your treatment plan and lifestyle. While during stage one COPD, you were likely very active and took the time to travel as much as possible, stage four COPD treatment should focus more on improving your comfort and ensuring your psychological, physical, and even spiritual needs are met.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
While you should take the initiative to do these things for yourself, it’s also important to consult your doctor to make sure you don’t leave out any aspect of your treatment plan in the process. Even in end-stage COPD, you’ll need to keep up with your oxygen therapy, dietary plan, pulmonary rehabilitation, and avoid environmental triggers such as pollution or airborne allergens.
.png)
Many people assume that the longer they live, the less capable they are of improving various aspects of their lives. For example, some people take for granted that you can’t learn a musical instrument as an adult. These people are often told throughout their lives by their parents or friends that if you want to learn something complex, you have to start when you’re younger. It’s also assumed that you’ll stop progressing very early on in your life.
Fortunately, this is not always the case. While studies have shown that children are able to learn more easily due to an undeveloped prefrontal cortex, this does not mean that adults can’t become well-versed in a particular skill. And more importantly, this doesn’t mean that there is no reason for learning something even if you’re faced with the reality that you will never reach your full potential.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Being diagnosed with COPD is similar to the situation discussed above. Many people diagnosed with COPD are immediately hit with a sense of inferiority. They begin to think that they’re no longer capable of things that they previously were. And for some people, this can even lead to a self-defeating attitude that can be very counterproductive when it comes to your health and happiness. In this post, we’re going to take a look at seven different things that you should never stop pursuing, even after being diagnosed with COPD.
Your Relationships
If you’re like most people, your relationships play a key role in your well-being and happiness. Despite how busy your day gets, you probably ensure that you put enough time aside to spend with your family and friends. Studies have shown that, not only do healthy relationships increase our perceived level of happiness, but they also have real clinical effects that can affect us both psychologically and physically. Furthermore, this study states that these relationships may be especially important in treating COPD due to the high levels of anxiety and depression among this demographic.
Family relationships primarily have an effect on the onset and course of depression. In other words, positive interactions with your loved ones may cause depression to develop more slowly and ease some of the burden when you have depression. This study also found that people who are dissatisfied with their marriage are about three times more likely to experience an episode of depression over the course of a year than people who are satisfied with their marriages. Finally, people who experience “perceived criticism” from family members are more likely to experience a release of depressive symptoms.
You’ll be happy to know that this isn’t the only study that confirms these findings. Depression has been studied in many other chronic conditions and relationships consistently rank among the most important determining factors. According to this study of lung cancer patients, people who were married had a greater survival rate than those who were not. It also found that people with the most severe symptoms had smaller social networks and were more likely to experience comorbid conditions like traumatic stress, anxiety, in addition to physical symptoms.

So now that we’ve established that your relationships play an important role in helping you manage COPD, you’re likely wondering how you can actually improve your relationships. Many people believe that they have good relationships already, so there’s no point in worrying about it. However, even if you already have positive relationships, there’s a good chance that you can take steps to improve them.
According to the University of Delaware, the first step in improving relationships with family members is to become a better listener. Rather than being quick to react to what someone is saying, take the time needed to fully understand what they’re saying and focus your attention equally on how they’re feeling as much as what they’re saying. It also helps to eliminate as many distractions as possible such as your cell phone, the TV, or anything else that could take your attention away from the conversation.

Another aspect of building good relationships is to make time for people. In this day and age, it’s becoming increasingly more difficult to make time for friends and loved ones because there are so many things to schedule around. This is no different for COPD patients because your day is likely full of pulmonary rehab, doctor’s visits, and you might even work a part-time or full-time job.
Your Hobbies and Pastimes
Hobbies and pastimes may not seem like something you should be focusing your attention on. But the truth is, the older you get and the more COPD symptoms progress, the more important your pastimes become. This is because even as your respiratory symptoms progress, you’ll still be able to improve at hobbies like playing music, card games, puzzles, and more. All of which will keep your mind occupied, improve your mood, and help prevent issues like anxiety and depression.
According to the Lung Institute, hiking, reading, and puzzles are three of the best hobbies you can have as a COPD patient. Hiking is one of the best ways to get out and enjoy the great outdoors without doing anything too strenuous. However, there are several important considerations you should make before going on a hike. Extreme weather, either hot or cold, can exacerbate your COPD symptoms. As such, it’s important to check the weather beforehand and make sure it’s comfortable enough for a hike. Read through this post to learn about preventing heat-related COPD symptoms. Another factor you should consider is outdoor air quality. Visit AirNow.gov and type in your ZIP code or city to check the air quality in your area.

Reading is the second hobby that the Lung Institute recommends. Reading is unlike any other hobby in that it allows you to learn about any topic you want without ever leaving the comfort of your living room. Whether you’re into historical books, fantasy, or educational books, there is something out there for everyone. What’s more, reading content is more accessible than it ever has been before. You can read books directly off your phone, computer, or tablet, order them online which is far more affordable than you might expect.

If reading isn’t exactly your thing, there are always puzzles or games. Jigsaw puzzles are a great way to occupy your time and they can even be used as a socializing tool or teambuilding exercise if you want to spend more time with friends and family. If you’d like to expand your vocabulary, crossword puzzles might be something to consider. Or if interested in working with numbers, give Sudoku a try. You can either print them off, find them in magazines, or install an application on your smartphone or tablet.
Your Exercise Routine
According to Everyday Health, moderate exercise makes it easier for COPD patients to breathe by strengthening respiratory muscles and helping the body use oxygen more efficiently. In many ways, however, this can be a vicious circle because many COPD patients find themselves unable to exercise in the first place. This can lead them to outright stop trying to implement an effective exercise routine into their lives.

The solution to this is to speak with your doctor about joining a pulmonary rehabilitation program. During this program, you will not only learn how to exercise correctly with COPD, but you will also learn what causes flare-ups and exacerbations so that you can avoid them in the future. Many COPD patients do not know very much about their condition or even what it is when they’re first diagnosed, so pulmonary rehab is one of the most effective ways to learn about it and address any concerns you may have.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Generally speaking, your exercise routine is something that you can always improve on. Whether you just started pulmonary rehab or you’ve been exercising on your own, it can be extremely beneficial to try new exercises. If you see improvements in your symptoms, you can make gradual adjustments to your exercise routine, however, if not you can try something else. If you’re in need of guidance be sure to consult your doctor.
Your Diet
Many people would argue that your diet is equally important, if not more important than your exercise routine. The food you eat is inextricably linked to your lung, heart, and circulatory health because the nutrients you gain from your food can benefit (or harm) your overall health. While you might believe that you already maintain a healthy diet, when it comes to coping with a chronic condition like COPD, it’s more about maintaining the right diet for your needs. For example, if you’re someone who’s underweight because of your COPD, you will need to consume more calories and more protein to get back up to a healthy weight.
![]()
Your Sleep Schedule
Sleep is vital for anyone’s health, but especially so for people with COPD and other chronic respiratory ailments. While COPD doesn’t cause sleep disorders or vise versa, they often occur simultaneously in a condition called COPD-OSA overlap syndrome. People may live their whole lives with this condition without realizing it and it can lead to loss of sleep, chronic daytime fatigue, and even increase your risk for conditions such as high blood pressure, heart attack, and stroke.

Aside from getting more sleep, you should take the opportunity to take a sleep test (polysomnography). These tests are done by trained professionals who will monitor your brain activity, breathing rate, and heart rate as you sleep. This information can be used to determine a number of things such as if a sleep disorder is present. It can even help your doctor understand how your COPD is affecting your sleep at night so that you know whether to increase or decrease your oxygen supply while you sleep.
Your Mental Health
While we’ve already mentioned two things you can do to improve your mental health including improving your relationships and spending time with your favorite hobbies, there are many other things you can do as well. Mental health issues look different for everyone. Some people experience regular anxiety or depression whereas others experience it off and on, like with a change of seasons. Others have had anxiety so long that they may not even realize they have it.

One of the best ways to combat mental health issues if you have COPD is to attend cognitive behavioral therapy (CBT). This is a type of intervention that’s designed to pinpoint where your negative or unconstructive thoughts are coming from and take steps to change them. CBT is used by people of all ages and with a variety of different mental or physical conditions. It’s becoming increasingly popular among COPD patients because the idea of seeking help for mental health conditions is becoming de-stigmatized.
Your Goals and Aspirations
Last but certainly not least, your goals and aspirations should never stop changing and improving even after you’re diagnosed with COPD. Far too many people believe that being diagnosed with a chronic condition means letting go of your dreams or goals, but this couldn’t be farther from the truth. While COPD should be taken seriously, it’s not a doomsday scenario like many people make it out to be. In fact, people who follow a strict treatment plan often see significant improvements to both their symptoms and their life expectancy.
![]()
If you want to stick with your short- and long-term goals, it’s always best to write them down. According to Forbes, there are two reasons why this is the case: external storage and encoding. External storage simply means that you will have a physical reminder of what your goals are. You can post sticky notes around your home or around the office to remind yourself to stay on track for what you’re trying to accomplish. The other aspect of this, encoding, refers to your brain's biological ability to remember things better when they’re written down. Studies have shown that note takers are able to retain about 23% more information than those who do not take notes.
Conclusion
COPD is one of the leading lung conditions in the world and it’s even one of the leading morbidities in general. While COPD can lead to debilitating symptoms like a chronic cough, chest pain, and shortness of breath, this condition is unique in that it develops over the course of many years. This means that it’s very possible to live a long and happy life after being diagnosed with COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
One of the most important aspects of happiness is being able to always learn and improve at things that are important to you. In this post, we highlighted seven things you should be focusing on. If you can think of anything else, however, be sure to create your own list and make reminders so that you remember you’re never too old to pursue things that are important to you.
If you’re interested in reading more articles about living a rewarding life with COPD, supplemental oxygen therapy, smoking cessation, or holistic health, be sure to bookmark our blog page. And if you have any questions, don’t hesitate to leave them in the comment section below or reach out to us by phone or email.
.png)
It seems like no matter where we go these days or what we’re doing, we’re always using technology. While several decades ago, it may have been possible to avoid using a cell phone or the internet, this becomes increasingly difficult as nearly everything around us is moving digital. According to the Pew Research Center, 95% of adults between the ages of 50 and 64 own a cell phone, and 79% of people in the same age group own smartphones. These numbers are only expected to increase over the years.
Although the pros and cons of smartphone use are hotly debated, it’s fair to say that they’ve afforded us easier access to information than ever before. And if you’re someone with a respiratory illness like chronic obstructive pulmonary disease (COPD), you know that technology enables you to stay connected more easily with friends and loved ones, and research information about managing and treating your disease. What’s more, most of these resources are free and easy to use.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you’re a COPD patient who’s interested in technology that allows you to interact with your disease in unique and beneficial ways, stick around. We’re going to be taking a look at some of the best mobile applications you can have on your smartphone. In the meantime, if you’re in the market for a portable oxygen concentrator, feel free to reach out to our respiratory specialists in Denver, Colorado. LPT Medical offers the lowest prices on the latest portable oxygen concentrators including the Caire FreeStyle Comfort, Inogen One G5, and the Respironics SimplyGo.
AirNow Mobile Application (Android and Apple)
If you’ve read any of our blog posts here at LPT Medical, you know how important air quality is to us. While cigarette smoking is still the primary cause of COPD, exposure to outdoor air pollution, and indoor irritants is still a significant risk factor for contracting COPD. this is why it’s of the utmost importance to be conscious about the air we breathe and take steps to plan our life around these issues. While there will always be poor air quality due to wildfires and carbon emissions, we can take steps to live healthier lives.

If you read our post about wildfires, you know that we discussed a very important component of air quality: the air quality index (AQI). This is a broad term used to describe the overall quality of air outdoors. It’s an aggregate score of five major types of pollutants including carbon monoxide, particle pollution (PM2.5 and PM10), ground-level ozone, sulfur dioxide, and nitrogen dioxide. The AQI scale runs from 0 being perfect air quality and 500 being the absolute worst. Generally speaking, COPD patients should not be outside if the AQI is over 100, but this will depend on the severity of your symptoms.
.jpg)
Rather than having to go to the AirNow website to check the AQI in your area, the AirNow Mobile application allows you to do it anywhere in the world from the convenience of your smartphone or tablet. You can save a variety of different locations to easily check the AQI all over the country and you can even view the AQI forecast in your area to make it easy to plan your week. Since all of the information is pulled straight from AirNow.gov, you can rest assured that it’s up-to-date and factual.
Breathe2Relax (Android and Apple)
Most people give very little or no thought to the way they breathe — but they should! The way we breathe is directly linked to many of the body’s functions including, sleep, digestion, and cognitive function. Simply by becoming more self-aware of our breathing habits and implementing techniques like deep breathing and diaphragmatic breathing, we can begin to reverse the negative effects of shallow, ineffective breathing. This is imperative for COPD patients who have significantly reduced lung function compared to the general population.
Another problem with ineffective breathing is that it can cause anxiety. The Breathe2Relax app was created specifically to target this type of breathing and correct it so that you can feel more at peace and relaxed in your day-to-day life. One of the techniques it focuses on is diaphragmatic breathing which teaches you how to breathe using the diaphragm muscles below the lungs rather than using the chest muscles to breathe. Many people find it difficult to learn this technique from simply reading about it, so this app is more interactive to ensure you do the exercises correctly. Another great feature of this app is that it can connect with your Apple Watch to measure your heart rate and provide you even more detailed information about your health.
If you’d like to learn more about breathing exercises for COPD, we’ve created a great comprehensive guide. In this post, we take a look at 6 key breathing exercises that all COPD patients should know about including:
- The stop, rest and continue technique
- Pursed lips breathing
- Coordinated breathing
- Deep breathing
- Diaphragmatic breathing
-
And a relaxed posture
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
NCI QuitGuide (Android and Apple)
According to the American Lung Association, 85 to 90 percent of COPD patients contract their disease through cigarette smoking. While not all people continue smoking after being diagnosed with COPD, you may be surprised to find that around 38% do. Unfortunately, many people believe that the damage has already been done, and continuing to smoke will not affect them, however, this couldn’t be further from the truth. Any amount of smoking, whether it’s one cigarette a week or a pack a day will contribute to lung inflammation, and thus, increase the rate at which COPD progresses.

Another problem with smoking as a COPD patient is that it significantly increases your risk of experiencing a flare-up or exacerbation. In short, an exacerbation is a sudden increase in respiratory symptoms such as breathlessness, chest pain, coughing, or wheezing. Acute exacerbations can be severe and even lead to hospitalization if they aren’t dealt with swiftly and efficiently. Smoking also impairs your immune system’s responsiveness making you more likely to contract a lung infection. Infections are also the most common cause of COPD exacerbations. For a more detailed look at the importance of smoking cessation, please visit our article titled: 15 Important Things That Happen When You Quit Smoking.
While there are many “quit smoking” apps out there, we chose NCI QuitGuide because it was created by the National Cancer Institute. This is one of 11 government organizations that makes up the Department of Health and Human Services (HHS) in the United States. NCI QuitGuide is not necessarily designed to be an all-in-one smoking cessation tool, but it can be used in tandem with other methods like nicotine replacement therapy and cognitive-behavioral therapy (CBT). Be sure to consult with your doctor to determine which method is best for you.

QuitGuide is a simple mobile application that allows you to track cigarette cravings, mood, and your reasons for quitting. It also displays information about your smoking cessation including the amount of money you’ve saved, days smoke-free, and provides you with milestones to reach. This app is perfect for anyone who wants to see the tangible effects of smoking cessation. The best part of all is that it’s free. There’s no need to worry about paying an upfront fee or paying a subscription of any kind.
The COPD Pocket Consultant Guide (Android and Apple)
We’ve referenced the COPD Foundation many times and you’re likely familiar with COPD360social, a free social networking site for people with COPD. However, you may be less familiar with their mobile application, the COPD Pocket Consultant Guide. This app has tools for healthcare providers, caretakers, and patients, so it’s important that you select the option that applies to you when you first open it. Once you have it set up, however, you’ll find that you have a variety of resources at your disposal.

The “For My Next Visit” section is designed to help you prepare for your next doctor’s visit. This is a simple tool that displays a bunch of “questions” and “symptoms.” You can then go through and select the questions you’d like to ask your doctor upon your next visit, along with any symptoms that have changed since your last one. You can then either save your results or print them out to show your doctor.
The “Wallet Card” section is designed to work like a digital version of your medical information card. Through this tool, you can save important information about your oxygen concentrator flow setting, CPAP or BiPAP settings, and a whole host of other things such as your physician contact information and insurance provider information. The best part about this feature is that it allows you to secure all of this important information using face identification technology. This way, you ensure that only you can view this information.

The third feature of this app is the training video section. Pulmonary rehabilitation, inhaler therapy, and nebulizer therapy are key components of most COPD treatment plans, and these videos will show you exactly how to do these things effectively. Believe it or not, studies show that many people do not follow their treatment plan, especially when it comes to using an inhaler. This app provides the easiest solution to this with all the training videos in one area.
The next feature of this app is the “Activity Tracking” section. This section lists out a bunch of daily activities such as cleaning, making the bed, and brushing your teeth, then you get to choose the level of difficulty you have doing these things. Fill out this form once a month and then print it out to see what kind of progress you’re making in your day-to-day life.
![]()
An action plan is a series of steps you will take if you encounter a specific problem. The COPD Pocket Consultant Guide divides your symptoms into three different categories: green, meaning you feel good; yellow, meaning you feel worse than normal; and red, meaning you are experiencing serious and disruptive respiratory problems. Go over this section of the app with your doctor so that you’re prepared for days where your symptoms increase.
Last but certainly not least, there is a section titled “more” that has additional resources for you to view. This includes links to COPD360social, the COPD Foundation blog, the COPD Patient-Powered Research Network (COPD PPRN), a COPD Assessment Test (CAT), and a help page if you’re experiencing any issues with the app or you have any questions about managing your disease.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
All Respiratory Disease and Treatment (Android)
The last mobile application we’re going to go over is not necessarily specifically designed for COPD patients, but it’s more of an educational resource about all respiratory diseases — chronic and acute — and how they’re treated. This is a useful app if you’re someone who simply enjoys learning about the lungs and how to take care of them. It can also help you put COPD into perspective and clarify any confusion about its similarities and differences when it comes to other lung diseases.
The best advantage of using this app is that you won’t have to waste time scouring the internet for information about COPD and other lung diseases. Simply open up the app and you’ll be able to view a substantial amount of information about COPD like a definition, risk factors, symptoms, causes, home remedies, and much more. It’s also handy to have on-the-go if a question comes to mind while you’re away from your computer at home. The only downside is that this app is only available on Android.
Conclusion
The world is a more connected place than ever before. One of the biggest benefits of this is that we can have easier access to information in the palm of our hands, pretty much wherever we go. If you’re a COPD patient, you need to stay up to date on how to treat your disease, as well as how to use things like inhalers, nebulizers, and oxygen devices. The apps listed above are just a few of the free resources you have available to you if you use a smartphone like an Android or an iPhone.
Looking for more ways to stay connected? Telehealth technology is reshaping the way we view healthcare and it’s becoming increasingly more accessible for COPD patients like you. Check out this blog post where we feature portable oxygen concentrators like the Caire FreeStyle Comfort and the Inogen One G5 and the unique technologies they’re bringing to the oxygen industry. And in the meantime, stay tuned to our blog where we discuss helpful information about COPD and COPD management.
.png)
Supplemental oxygen is a type of medical therapy used to treat chronic lung conditions like cystic fibrosis, pulmonary fibrosis, and COPD. The aim of supplemental oxygen is to maintain a patient’s blood oxygen levels which are vital for systemic health. Every organ in the body requires oxygen in order to function properly, so using supplemental oxygen as it’s advised by your doctor can provide you with immense short- and long-term benefits.
Despite how important supplemental oxygen is for respiratory patients, receiving a prescription for oxygen therapy can be a scary experience. You likely have a lot of thoughts and concerns running through your mind and you’re likely overwhelmed by the prospect of being connected to an oxygen delivery device. While these concerns are certainly justified, it’s important to take a step back and begin to clarify your concerns with your doctor. Chances are, as you learn more about oxygen therapy and become more experienced with using it, many of your concerns will begin to disappear.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
To help you organize your thoughts, we’re going to be discussing 14 questions you should ask your pulmonologist about supplemental oxygen therapy. Feel free to either print out this article or take notes so that you know exactly what to ask your doctor during your next visit. If you enjoy this article and you’re looking for more information, be sure to read through our post titled “16 Questions You Should Ask Your Doctor About COPD.”
1.) Is Oxygen a Necessity or a Suggestion?
Chances are, you or someone that you know has fallen back on a prescription at some point. Either you never make it to the pharmacy to pick up your medication or you simply stop using the medication for one reason or another. This Harvard Medical report states that many people either forget to use their medication, or they never fill it due to high copayments. So, naturally, you might wonder whether or not your oxygen therapy prescription will follow a similar trend. As a general rule of thumb, you should take what your doctor says seriously, because it’s unlikely that he/she would make you go out of your way or spend extra money on something that isn’t necessary. However, it doesn’t hurt to address these concerns so that your doctor can clarify the rationale behind your oxygen prescription.

2.) What are the Benefits of Oxygen Therapy?
The second thing you should ask your pulmonary doctor about are the benefits you can expect to reap from using supplemental oxygen. The air around us contains about 21% oxygen, but for someone with impaired lung function, this is not always enough for them to sustain their blood oxygen levels. The goal of oxygen therapy is to provide the lungs with a higher concentration of oxygen in order to reduce the load on the lungs. You may experience additional benefits from using supplemental oxygen based on the severity of your disease. Be sure to ask your doctor about this.

3.) What is My Flow Rate?
Your flow rate determines the amount of oxygen that you will be receiving when you put on the nasal cannula. It’s imperative that you know the exact amount of oxygen that you should be receiving because inhaling too much oxygen can lead to a condition called oxygen toxicity. This condition results in dizziness, fatigue, nausea, and eventual lung damage. Conversely, receiving too little oxygen will not provide you with the full benefits of supplemental oxygen.

Oxygen flow is measured using one of two different measurements. Pulse dose oxygen devices are measured in milliliters per minute (ml/min) and continuous flow oxygen devices are measured in liters per minute (LPM). The amount of oxygen that you’re prescribed will be based on the severity of your respiratory impairment, but generally speaking, most people need less than 2 LPM of oxygen.
4.) How Many Hours a Day Should I Use Oxygen?
Knowing how long you should be using oxygen is just as important as knowing your oxygen flow setting. If you’re using oxygen inconsistently, you might see a lot of your respiratory symptoms start to return. Long-term oxygen therapy is usually done for at least several hours a day, and your doctor will work with you to determine the best time to use it. If your doctor prescribes you with 24/7 oxygen, then you should discuss with your doctor about using an oxygen concentrator which doesn’t need to be refilled constantly like oxygen tanks or liquid oxygen tanks.

5.) What Type of Oxygen Device Should I Buy?
You might be surprised to find out how many oxygen devices there are on the market. You’ll have a whole host of options to choose from including traditional oxygen tanks, liquid oxygen tanks, stationary oxygen concentrators, and portable oxygen concentrators. But as someone who’s new to supplemental oxygen, you likely don’t know where to even begin with choosing one of these. Your doctor will likely have some information for you regarding which oxygen devices you should avoid and which ones you should consider.

It’s important to be careful when you’re purchasing an oxygen device. You may encounter companies that try to sell you oxygen without a prescription or that boasts prices that are significantly lower than any other company. However, these are most likely scams. Before making any decisions, be sure to research the company that you’re buying from to make sure that their products are reliable and that they follow all laws and regulations. For more information about how the U.S. Food and Drug Administration (FDA) regulates oxygen, please visit this page.
6.) Is it Okay to Adjust My Flow Rate Depending on How I’m Feeling?
If you have a chronic respiratory condition like COPD or pulmonary fibrosis, it’s not uncommon for symptoms to come and go. One day, you might be out of breath or lightheaded and the next you could feel perfectly fine. Because of this, you’re going to want to clarify with your doctor when it’s okay to adjust your oxygen flow and when you should not adjust your oxygen flow. The reason it’s important to ask this question is because your increase in symptoms may be due to something completely unrelated to your blood oxygen levels. In which case, increasing your oxygen flow would not benefit you.
.jpg)
7.) How Can I Track My Blood Oxygen Level?
A pulse oximeter, or pulse ox device, clips onto your finger and measures the saturation of oxygen in your blood (SpO2). They are noninvasive and they work by passing rays of light through your finger to measure the amount of oxygen-carrying hemoglobin. While they aren’t the most accurate method of measuring blood oxygen levels, they are very lightweight and portable meaning you can pack one in your purse or handbag for easy access. If your doctor hasn’t already provided you with one, it’s worth mentioning it so that you have a way of monitoring your oxygen levels. To learn more about blood oxygen levels, read this post.

8.) Is Oxygen Therapy Safe?
Since oxygen is a controlled substance in the United States and requires a prescription, you may be wondering if it’s even safe to use in the first place. The answer to this question is “yes,” however, there are some things you should be aware of. Firstly, as aforementioned, using more oxygen than you’re prescribed will put you at risk of experiencing oxygen toxicity. Secondly, the safety of oxygen therapy depends heavily on the type of oxygen device you’re using.
Traditional oxygen tanks are the most dangerous because they contain compressed oxygen and they’re also heavy and bulky. Portable oxygen concentrators are the least dangerous oxygen device because they are lightweight and do not contain compressed oxygen. Oxygen is an “oxidizer” meaning it increases the flammability of anything it comes into contact with. So, you should never smoke near your oxygen device or use it near an open flame.
9.) Should I Be On Oxygen When I Sleep?
If your doctor prescribes you with 24/7 oxygen, you might be wondering how this will work when you’re sleeping. Your breathing rate and depth fluctuate a lot when you sleep so the amount of oxygen that you’re receiving could change throughout the night. This is why it might be worth it to invest in a portable oxygen concentrator like the Caire FreeStyle Comfort or the Inogen One G5. Unlike oxygen tanks, these devices closely monitor your breathing as you sleep and adjust your intake accordingly.

If you have a sleep disorder like obstructive sleep apnea (OSA), you may need to use your PAP device and your oxygen device at the same time while you sleep. PAP therapy is of critical importance for OSA patients because it keeps their airways open as they sleep allowing them to get restful sleep without interruptions. To use your CPAP device with your oxygen device, you need to be using a continuous flow oxygen unit and have a bleed in adapter that connects the tubing together. The Respironics SImplyGo is the perfect portable oxygen concentrator for CPAP compatibility.
10.) How Can I Eliminate Discomfort While on Supplemental Oxygen?
For the most part, oxygen therapy shouldn’t cause any discomfort. However, some people encounter issues with the nasal cannula such as irritation inside the nose due to dryness or some other reason. Humidifiers can actually be attached to your oxygen device to help ease the discomfort and there are a number of other accessories you can purchase that make the process more comfortable. We actually wrote a guide discussing some of the issues oxygen patients face and how to solve them. Check it out here.

11.) Can I Exercise on Oxygen?
Consistent moderate exercise is crucial for pulmonary wellness. Not only does exercise improve the strength of your lungs but it also increases the efficiency that your heart pumps oxygen throughout your body. So, just because you’ve started oxygen therapy does not mean that you should stop exercising. Check out this post which has some tips for exercising with an oxygen device and be sure to ask your doctor for advice as well.

12.) What Do I Need to Know to Travel With Oxygen?
Traveling around the world with COPD is much easier than ever before thanks to portable oxygen concentrators. The Federal Aviation Administration (FAA), the organization that oversees all commercial flights in the United States has approved most POCs for in-flight use. However, to make sure you have everything you need, you should contact your airline at least 48 hours before your flight. Most airlines require that you have at least one and a half times as much battery life as the duration of the flight. This will make up for any delays that may occur before and after you land.

13.) How Do I Maintain My Oxygen Device?
With the advent of the novel coronavirus, cleaning has taken on a whole new meaning. No matter what type of oxygen device you decide to use, you should take the time to clean it regularly. What’s more, nasal cannulae and oxygen tubing should be replaced every two weeks to ensure it’s clean and ready for use. If you purchase a portable oxygen concentrator you should remove the particle filters each week and wash them off. This will ensure that the air you’re inhaling through the cannula is clean and free of dust and dirt.

14.) Will I Need to Get Retested For Supplemental Oxygen?
Doctors typically use arterial blood gas analysis, pulse oximetry, and various lung tests to determine your need for supplemental oxygen. However, you may need to take on-going tests to help your doctor determine whether or not you still need oxygen in the future. Ask your doctor what kind of tests you will need to take and how often you should come in for a checkup once you are using your oxygen device. Some patients find it helpful to get a certificate of medical necessity which can help you file insurance claims and apply for benefits.

Conclusion
Supplemental oxygen is a very important facet of your treatment regime if you have COPD, pulmonary fibrosis, cystic fibrosis, or any other number of lung conditions. Unfortunately, it’s something that takes time to get used to and learn about if you’ve never done it before. Many people don’t even know what questions they should be asking their doctor so we hope that this guide will help with demystifying oxygen therapy.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Here at LPT Medical, we take your search for an oxygen therapy device very seriously. We work with some of the top brands in the industry such as Inogen, Respironics, AirSep, and Caire in order to provide our patients with the best oxygen devices on the market for an affordable price. Our respiratory specialists will work with you one-on-one to determine what your medical needs are, then they will help you narrow down your options based on your lifestyle and preferences. We also have a number of buying options like new, refurbished, and used units so you can choose which one best fits your needs.
Feel free to reach out to us either by email or phone to get started finding an oxygen device for you.
.png)
When you think about your day as a whole, how much time do you spend thinking positive thoughts? What about negative thoughts? And have you ever wondered how these two different lines of thinking are affecting your well-being and your ability to cope with your lung disease? Chronic obstructive pulmonary disease (COPD) is an unbelievably complex disease. Like we’ve discussed in previous posts, it’s a “systemic disease’” meaning it can have manifestations in other areas of the body. So, we can’t even begin to imagine all of the ways it affects our physical and mental health.
But despite the complexity of COPD, seemingly small and insignificant things can have a considerable impact on the outcome of the disease. For example, getting on your feet and moving around for just a couple of minutes extra each day could reduce your risk for heart disease and stroke, while helping your body manage hypertension, muscle pain, and stiffness, all of which are common in COPD. What’s more, making small adjustments to your diet like reducing sugar intake and consuming more protein and healthy fats can also have a big impact on your disease outcome.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
While you may think of “positivity” as something that only impacts your happiness, we’re going to show you in the following sections how it’s inextricably linked to the outcome of your disease and how just a few adjustments to your thought process can make your life a lot easier. As always, if you have any questions for us, feel free to leave them in the comments below or reach out to us via phone or email.
Positivity Promotes Productivity
While you may think of COPD patients as mostly retired people, there is a surprising amount of them who still work part-time or full-time jobs. According to a study published in the European Respiratory Journal, it’s common for COPD patients to miss work due to exacerbations, recurring lung infections, or simply feeling burnt out from dealing with their disease. Another thing to consider is the types of jobs that people work. Someone who works an office job might be less inclined to miss work than someone who works outside in the sun or in a factory where air pollution can lead to respiratory exacerbations.
Equally important to productivity in the workplace is productivity at home. Many COPD patients have obligations at home such as cleaning, paying the bills, and taking care of their children or grandchildren. Completing these obligations can make you feel satisfied and whole so it’s best to stay positive and focus on what you’re trying to accomplish rather than focusing on how challenging it can be with a respiratory disease. But at the same time, everyone has their limits, so you should know what they are and be sure not to cross them.
Positivity Results in Better Decision Making
Good decision-making is paramount to COPD management. Ultimately, your decisions will mean the difference between managing your respiratory symptoms effectively or letting them run their course. For example, on any given day, you have the opportunity to use your medication as it’s prescribed or deal with the side effects of using it improperly. While it may be tempting to increase your dosage if you feel that it isn’t helping, a better decision would be to connect with your doctor first to see if it will have any unintended consequences.

One of the terms you might hear thrown around in the COPD community is something called “shared decision making.” In short, this refers to healthcare professionals working one-on-one with patients to make decisions about the patient’s health. In other words, the doctor isn’t simply telling the patient what to do. The patient is playing an active role in their own health decisions. This benefits the patient because they feel like their personal needs are being met and it benefits the doctor because he/she can learn more about what’s important to COPD patients.
Positivity Prevents Anxiety and Depression
Anxiety and depression are two of the most common mental health conditions. It’s estimated that around 18.1% of the population or 40 million people in the United States have anxiety. What’s more, these mental health conditions are significantly more common among COPD patients than in the general population. According to this study from the European Respiratory Journal, COPD patients are 85% more likely to experience an anxiety disorder when compared to healthy control subjects, and studies regarding depression have shown similar results.
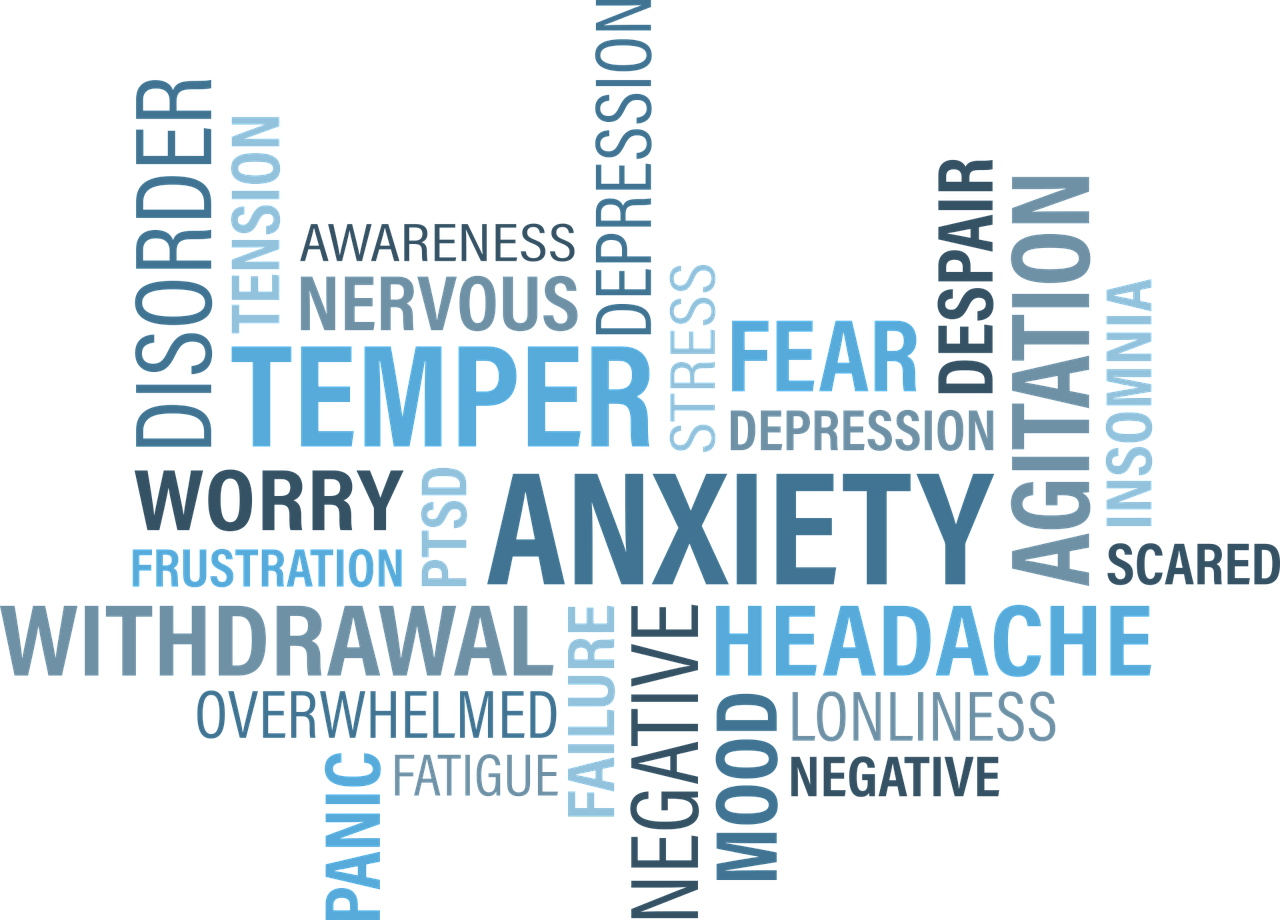
There are several reasons for the high rates of mental illness among COPD patients. One possible reason is that COPD patients spend more time thinking or worrying about their health. From making it to the doctor’s office to taking medication, exercising, and maintaining a strict diet, your illness is something that’s always top of mind. As symptoms escalate, you’ll likely put even more of an emphasis on your health and well-being.

Another reason COPD patients have higher rates of mental illness is due to the physical effects of the disease. COPD is known to cause breathlessness, fatigue, and chronic pain, and rapid changes to your diet and sleep routine due to flare-ups and exacerbations can leave you feeling irritable and groggy. Studies have shown that COPD can even affect our hormones and brain chemistry which can manifest itself as behavioral changes. This is why treating your underlying disease is not only important for your physical health, but your mental health as well.
Positivity Improves Systemic Health
Believe it or not, having a positive attitude can also have beneficial effects on our systemic health. This study found that emotional well-being improves recovery time and survival after physical illness. Other studies have found that positive attitudes in older adults result in a stronger immune system. This is essential for people with COPD because a poor immune system can lead to infections, the primary cause of COPD exacerbation and hospitalization.
Several other health-related benefits of positive thinking include lower blood pressure, a lower risk of heart disease, easier weight management, and healthier blood sugar levels. Weight management, in particular, is an issue that many COPD patients face because they expend a lot more energy and burn more calories than they used to, meaning they tend to be underweight. However, the opposite can also be true. Some people tend to “stress eat” when they’re experiencing anxiety or unhappiness, which can lead to unhealthy weight gain.
Positivity Leads to More Social Support
Social support is extremely important for people with chronic conditions. Between daily conversations with friends and family and interactions with caretakers and healthcare providers, it’s your social support system that is keeping you motivated. If your disease progresses, you may find yourself relying even more on those around you. There’s nothing wrong with this, of course, but you should take care to foster positive relationships early on so that you have that extra support later in life.

If you think about it, you probably enjoy spending time around people who are positive and uplifting, so it’s only natural that others would feel the same. What this means is that, despite how difficult the challenges of COPD may become, it’s always beneficial to remain positive and to spread that positive energy to other people. One of the ways many patients like to spread positivity is through online social platforms like COPD360Social. This is a patient engagement platform that’s hosted by the COPD Foundation and allows COPD patients to discuss treatment options and coping mechanisms for their disease.
Positivity Helps You Stay in Control
“Control” is a very important topic to discuss when you have a chronic disease. Many people who have been diagnosed with a chronic illness suddenly feel like they have lost control of their lives and that their disease now defines who they are and what they are capable of. However, when you look at the big picture, you start to realize that this is not the case at all. Many of the world’s greatest achievers have had some form of chronic illness and the thing that sets them apart the most is that they were able to adapt and overcome the challenges that they were presented with. None of this would be possible without having control.
The first step to maintaining control of your life despite your COPD diagnosis is understanding that there is no “right way” to do something. For example, you might be someone who makes use of mobility aids like canes, walkers, manual scooters, or electric scooters. But you shouldn’t feel guilty or self-conscious about using these things even when people around you are not. Instead, you should feel overjoyed knowing that you’re doing what you can in order to stay active and maintain your independence.

Another important note about control is that you likely have a lot more of it than you believe. While the lung damage caused by COPD is not reversible, your lungs are not the only things that affect your breathing. Your breathing is also affected by your fitness level, your diet, heart health, blood circulation, and many other things. So, if you want to stay in control, focus on things that you can change like eating right, staying active, drinking plenty of water, keeping up with your oxygen therapy, and visiting the doctor regularly. Once you realize that you have control over all of these things, you’ll be a lot happier and more positive about your condition.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The alternative to being “in control” is having a “lack of control.” If you take on the mentality that you’re not in control, you might begin to believe that your disease, healthcare providers, friends, or family members are responsible for your happiness and well-being. And well you should certainly rely on these people for help, it’s ultimately up to you to make a difference in your own life and do what’s necessary to improve your health.
How to Increase Positivity in Your Life
While negativity has a huge impact on the outcome of your respiratory disease, the good news is that there are many different ways to promote positive thinking in your life. The first and possibly most effective method is something called cognitive behavioral therapy (CBT). This is a form of psycho-social intervention that’s used for a number of different purposes including treating alcohol and drug abuse, eating disorders, marital problems, and mental illness. Recently, it’s come to light how effective CBT can be when it comes to providing coping skills to people with chronic conditions like COPD.

CBT is based on the premise that mental health conditions like anxiety and depression are caused by inaccurate thinking patterns and patterns of unproductive behavior. CBT aims to identify these things and take steps to reverse them and replace them with productive and positive thoughts and behaviors. During CBT, you will work one-on-one with a psychologist who will guide you through the process of correcting these things. The ultimate goal is to teach you the skills you need to be able to correct them on your own without the help of a professional.
Conclusion
COPD is one of the leading causes of morbidity and mortality worldwide. It’s estimated that around 65 million people in the world have been diagnosed with COPD and it affects some 16 million people in the United States alone. While these numbers may be shocking, it helps to know that many of these people have gone on to live long and happy lives by making healthy lifestyle choices like exercising, eating a well-balanced diet, and following their doctor’s instructions when it comes to oxygen therapy and medication.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Modern medical research has proven beyond a shadow of a doubt that mental well-being also plays a role in our overall health. People who embrace a positive line of thinking are better equipped to deal with anxiety and depression and in turn, they can mitigate many of the risks associated with COPD such as heart disease, high blood pressure, and stroke. Taking steps to reverse negative thinking can have many beneficial effects in both the short and long term. For many people, cognitive behavioral therapy is the preferred method for accomplishing this.
.png)
Here at LPT Medical, we want to make it as easy as possible for COPD patients to lead happy and productive lives. That’s why we offer lightweight and reliable portable oxygen concentrators like the Caire FreeStyle Comfort and the Inogen One G5. Unlike oxygen tanks, these devices will allow you to travel wherever and whenever you please. And since they’re so easy to use, you’ll be able to focus more of your attention on living your life rather than worrying about whether or not your oxygen needs are being met.
To learn more about portable oxygen concentrators, reach out to us either by phone or email.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













