
Managing chronic obstructive pulmonary disease (COPD) can feel like a balancing act a lot of the time. On one hand, you want to do everything you can to reduce the symptoms and prevent the progression of your disease. However, on the other hand, you don’t want to use any treatments that could cause serious side-effects. It’s not always easy to find a balance between these two things and create a routine that works for you.
This has never been more true than with home remedies. Simply put, a home remedy is an easy and accessible treatment option for an ailment that you can do at home. Home remedies are not prescribed by a doctor and they typically have more anecdotal evidence to prove their efficacy than hard scientific fact. What’s more, home remedies aren’t always focused on treating a specific disease like COPD. Instead, they could be focused on improving your health in general which, in turn, could help you treat your COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Rather than taking a risk with home remedies you may find on social media or elsewhere on the internet, we’re going to outline some COPD home remedies that are proven to be safe and effective. Just remember that home remedies should never be put before the treatment plan prescribed by your doctor including but not limited to supplemental oxygen therapy, pulmonary rehabilitation, and an improved diet. As always, if you have any questions about what you read here, don’t hesitate to leave a comment and we’ll get back to you as soon as possible.
Dietary Supplements
Dietary supplements are commonly misunderstood in today’s world. Many people are under the impression that dietary supplements can replace a healthy diet and others are convinced that dietary supplements do nothing at all. However, the truth is somewhere between these two points of view. Supplements can potentially enhance your diet, but there are also a few things you need to be aware of in order to use them safely.

Dietary supplements are not considered “medication” by any means. In fact, the Food and Drug Administration (FDA) classifies them as a “food product.” The good news is that this means they are widely available and you won’t need a prescription in order to buy them. But the bad news is that supplements are not regulated the same way as medication. It also means you’ll have to do your due diligence and research supplements, as well as the company selling them before you make any commitments.
Vitamin D Supplements
It’s a well-known fact that many people develop vitamin D deficiency after contracting COPD. According to the National Emphysema Foundation, over half of all COPD patients develop vitamin D deficiency because they consume fewer foods that are high in vitamin D and they are less likely to spend time outside in the sunlight which is a major source of vitamin D for many healthy people.

The main problem associated with vitamin D deficiency is osteoporosis, a condition where the bones become weak and brittle. Vitamin D plays an important role in the absorption of calcium which gives the bones their structure and strength. Vitamin D also plays an important role in the growth and function of muscles which is also very important for COPD patients.
Ginseng
Ginseng has a long history of use in Chinese medicine. It’s an herb that’s believed to improve pulmonary function as well as respiratory endurance. It’s known for both its antioxidant and anti-inflammatory effects as well as being able to regulate blood sugar levels. While the benefits of ginseng look promising, it’s important to discuss with your doctor before using it because it’s known to interfere with certain COPD medications.

N-Acetylcysteine (NAC)
This is an antioxidant supplement that’s shown potential when it comes to thinning mucus, reducing phlegm, and clearing the airways. Like ginseng, NAC is a widely available supplement that can be bought without a prescription. However, it is also known to interfere with certain medications, so it’s important to consult with your doctor before using it to treat your COPD.
Smoking Cessation
The vast majority of people who have COPD have smoked in the past and about 38 percent of current COPD patients are also smokers. Many people believe that, since they’ve already contracted COPD, there is no reason to put in the effort to quit smoking. But this could not be farther from the truth. The main reason to quit smoking is to slow the progression of COPD, but there are a whole host of other reasons as well.

Smoking increases your risk of conditions like heart disease, heart attack, diabetes, and more. What’s more, current evidence suggests that smoking is associated with increased severity of disease and a higher likelihood of death in COVID-19 patients. Smokers are known for having impaired immune systems which could also put you at a higher risk of contracting respiratory infections.
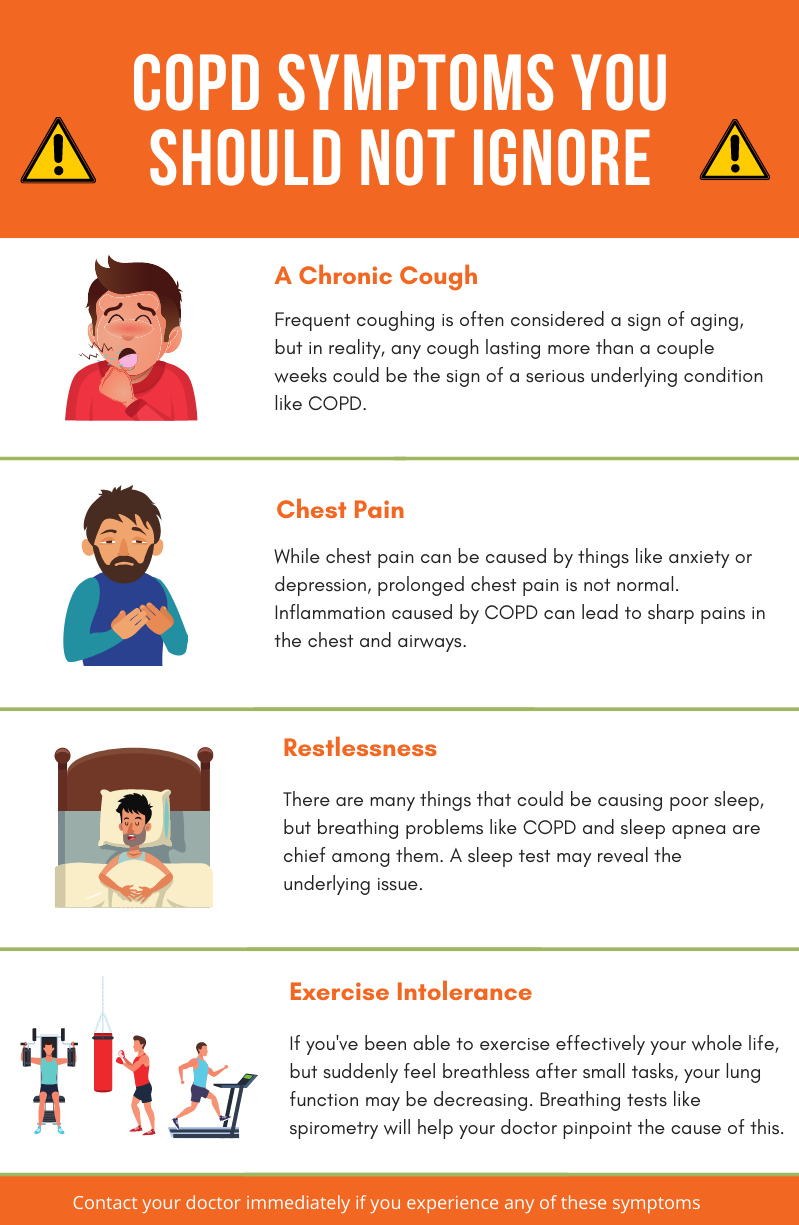
While there are many prescription medications you can use to quit smoking such as Chantix or Zyban, there are also many natural methods for quitting smoking. One thing you should know about smoking and other types of addictions is that you need it in order to feel normal. If you’re deprived of it for too long, you will likely start to experience feelings of withdrawal. When this happens, you’ll experience intense cravings, along with headaches and a change of mood. This is when you’re most likely to fall back into your smoking habits.
In order to avoid these intense feelings, you may have to slowly wean yourself off cigarettes or use a common technique like nicotine replacement therapy. Unfortunately, many smokers feel like they’re up against impossible odds when it comes to smoking cessation. Maybe you’ve seen others around you fail at losing cigarettes or you just don’t feel like you have it in you. But the truth is, it takes many attempts to quit smoking. This study suggests that it could take anywhere between 8 and 14 attempts to drop a smoking habit for good.
Cleaning Your Home
For most people, cleaning the house is a chore. But for someone with COPD, it can be a lifesaver. There are two reasons you should clean your home on a daily basis: first and foremost, it helps to eliminate airborne allergens and bacteria from your home, and secondly, cleaning is a therapeutic activity that helps you feel accomplished and whole. When your living environment becomes messy or dirty, you’re far more likely to experience issues like anxiety and depression.

Before you start cleaning, you need to make sure you’re using safe cleaning products that don’t contain dangerous chemicals that could exacerbate your respiratory problems. Unfortunately, the cleaning product industry is rife with hazardous chemicals that, if inhaled, can lead to coughing, wheezing, chest pain, shortness of breath, and even permanent lung damage. In COPD patients, inhaled chemicals can even cause severe exacerbations.
Volatile organic compounds (VOCs) are some of the most common hazardous materials you should keep an eye out for. Some common personal and home care items that include VOCs are:
- Disinfectants and cleaners
- Pesticides
- Air fresheners
- Deodorant and cosmetics
- And fuel

Other hazardous things in cleaning products include bleach, ammonia, ethylene glycol, monobutyl acetate, sodium hypochlorite, and trisodium phosphate. If at all possible, you should entirely avoid using cleaning products with these chemicals in them. However, if you absolutely have to use them, you should ensure that the room is well-ventilated, you should always wear a mask, and avoid getting the cleaning product on your hands or near your eyes or mouth. Refer to the Cleveland Clinic for more information on cleaning safely if you have COPD.
Breathing Exercises
Breathing exercises may seem silly to someone who has never tried them. However, the more you look into them, the more you begin to realize the bad breathing habits people develop over the course of their life. As a society, we spend more time sitting and remaining sedentary than ever before. This has caused many people to develop a shallow, ineffective breathing method that can be dangerous for someone with COPD or other respiratory conditions.
Breathing exercises are very easy to practice in the comfort of your own home and they are the perfect thing to incorporate into your daily routine. Not only will breathing exercises help you correct bad breathing habits, but they will also teach you how to reduce and manage anxiety more effectively.
.jpg)
One of the worst habits for COPD patients to develop is chest breathing. This type of breathing is focused on using the chest muscles in order to expand the lungs which can be exhausting with inflamed and obstructed lungs. Chest breathing should be replaced with diaphragmatic deep breathing which is focused on using the diaphragm, the thin sheet of muscle above the stomach to expand the lungs.
Anxiety Management
Cleaning regularly and practicing breathing techniques are both great ways to reduce anxiety, but they aren’t the only ones. The tricky thing about anxiety, depression, and other mental health disorders is that they can be triggered by just about anything. Some people may experience anxiety about their health whereas other people may experience anxiety for reasons that are purely biological.
The first step to preventing anxiety is to simply follow your treatment plan as closely as possible. Your treatment plan is designed with your long-term well-being in mind and that includes your mental health. Things like exercise and a healthy diet will help with full-body wellness and they’re always the first things you should commit to if you want to feel happier and more motivated. If you’ve tried all of this and you’re still experiencing anxiety, cognitive behavioral therapy (CBT) is the best alternative.
Weight Management
COPD is commonly linked with weight loss. Due to the increased energy that it takes to breathe with COPD, a changing immune system, and other factors like a loss of appetite, many COPD patients find themselves losing an unhealthy amount of weight. Oftentimes, this weight can be muscle mass rather than fat which is the most dangerous part about it. Your body needs muscle strength in order to breathe and get around more efficiently, so it’s very important to keep a healthy weight with COPD.

Weight management is something that can be done at home. Your doctor has likely set you up with a new diet plan that includes high protein, fiber, and healthy fats. You should follow this plan as closely as possible. What’s more, you should eat regularly throughout the day instead of eating one or two big meals each day. This will prevent you from feeling exhausted or bloated after eating and keep your energy levels stable throughout the day.
![]()
The second thing you should be aware of is your exercise routine. Pulmonary rehabilitation isn’t just designed to keep your lungs strong, it’s also important for helping you manage your weight by keeping fat off and muscle on. Like your diet, the most critical thing with pulmonary rehab is consistency so try to incorporate fitness into your daily routine.
Healthy Sleep Habits
Your sleep/wake cycle doesn’t just affect your alertness throughout the day, it also affects your energy levels and your ability to take on the challenges that COPD presents. For example, someone with a healthy sleep schedule will have a better mental attitude and a better willingness to make lifestyle changes that will positively impact their respiratory health. A poor sleep schedule can also contribute to anxiety which can further exacerbate COPD.

The key to a healthy sleep schedule is consistency. Adults should be getting between 7 to 9 hours of sleep each night and your sleep schedule shouldn’t vary night-to-night. Try to get to bed and wake up at the same time each day. Doctors also recommend avoiding naps throughout the day, getting plenty of exercise, and avoiding using electronics before you go to bed.
If you’re concerned that you’re losing sleep at night due to low oxygen levels, you may want to speak with your doctor about using supplemental oxygen therapy while you sleep. You are likely already on some form of oxygen therapy, but using an oxygen concentrator while you sleep will ensure that your blood oxygen levels remain stable throughout the night. Portable oxygen concentrators like the Caire FreeStyle Comfort or the Inogen One G5 are great options because they’re small, quiet, and can be plugged into any wall outlet meaning they’ll never turn off on you in the middle of the night.

If you have obstructive sleep apnea (OSA) and need to use a CPAP or BiPAP machine while you sleep, you will need to use a continuous flow portable oxygen concentrator like the Respironics SimplyGo. This concentrator is designed to put out a constant stream of oxygen, so if your breathing is interrupted for any reason while you sleep, you can rest assured that you’ll still be receiving medical-grade oxygen.
Conclusion
When it comes to treating COPD, you need a comprehensive approach that takes into consideration all facets of your life from your sleep schedule to your mental well-being. Home remedies are a great way to make you more conscious about how your lifestyle is affecting your health and what steps you can take to reverse these issues.
At the same time, however, you need to be careful about what home remedies you use. Some people will make unfounded claims about dietary supplements or other remedies which can actually make your symptoms worse. This is why you should always consult your doctor before using a new product or making drastic changes to your lifestyle.
Above all, you should be focusing on the treatment plan that you’ve created with your doctor. Doing so will help you alleviate breathlessness, chest pain, and coughing associated with COPD and you can expect to see a better prognosis for your disease.
.png)
The novel coronavirus has completely reshaped the way that we view sanitation. Over the past year, organizations and individuals alike have taken steps to control the spread of disease, and the population as a whole has become more aware of the impact of infectious disease. Another thing that people have become more aware of is the impact of chronic respiratory diseases such as COPD, asthma, and pulmonary fibrosis. Studies have shown us that these people are “high risk” when it comes to infectious disease, so we need to take steps to protect their health.
Unfortunately, simply telling someone to “clean more often” or “clean more thoroughly” is bad advice. These statements fail to acknowledge that cleaning products themselves can actually put our health at risk. Many household cleaning products are filled with toxic chemicals that can irritate the eyes, skin, and throat. And in the worst cases, they can even contribute to COPD symptoms by exacerbating chest pain, difficulty breathing, and chronic coughing.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In this post, we’re going to provide you with a comprehensive list of steps for cleaning your home as a COPD patient. We’ll give you advice on choosing cleaning products, how often you should clean, and other things you should take into consideration. If you have any questions, feel free to leave a comment. And if you find this information helpful, don’t hesitate to share it to help us get the word out about safe cleaning habits.
How to Choose Cleaning Products With COPD
The first step in cleaning your home is to choose the cleaning products that you will use. While this may sound like the easiest step, it’s actually the hardest. Cleaning products are rife with volatile organic compounds (VOCs). These are compounds that have a high vapor pressure and low water solubility. Many VOCs are artificial meaning they’re man-made, and they contain chemicals such as methyl tert-butyl ether (MTBE), trichloroethylene, oxygenates, and other industrial solvents.

According to the Environmental Protection Agency (EPA), concentrations of VOCs are up to ten times higher indoors than they are outdoors. This is largely due to the fact that VOCs are found in many household cleaning products and many homes are not ventilated well enough to rid them of harmful chemicals. But VOCs aren’t the only harmful ingredients found in home cleaning supplies. Many of them also contain carcinogens, chemicals that are known to cause cancer.
![]()
As a COPD patient, your goal should be to eliminate all hazardous cleaning products from your home. However, it’s especially important to avoid cleaning products that can exacerbate your respiratory symptoms. Products like air fresheners are particularly harmful to COPD patients because aerosol droplets can remain suspended in the air for long periods of time, meaning they can be inhaled. Generally speaking, “scented” cleaning products should be avoided at all costs. While we may enjoy a fresh smell and equate it with a clean home, most of these products contain harmful chemicals.
Before heading out to the store, create a list of ingredients that you should avoid. The ingredients below are commonly used in cleaning products and should be avoided:
- Perchloroethylene (PERC)
- Formaldehyde
- 2-Butoxyethanol
- Ammonia
- Sodium Hydroxide
- Chlorine
Some common cleaning products you should avoid include:
- Bleach
- Spray cleaners
- Fragrance sprays
- Carpet fresheners
- Fabric softeners
- Varnishes
-
Drain cleaners

Another thing to note is that you should be wary of anything labeled “green,” “organic,” or “eco-friendly.” Just because something is “organic” does not necessarily mean that it is healthy or safe. However, you may see products labeled as “safer choice.” These cleaning products are actually regulated by the Environmental Protection Agency (EPA) and they’re aimed at reducing, eliminating, or preventing pollution at its source. In many cases, these cleaning products can be a safer alternative for COPD patients but many of them still contain chemicals.
How to Make Safe Cleaning Products at Home
Believe it or not, homemade cleaning products can be extremely effective and they can also be much safer to use than store-bought items. When you make your own cleaners, you’ll know exactly what’s in them and you won’t have to worry about reading through and researching a long list of ingredients.

According to Healthline, some of the safest and most effective ingredients you can use to make homemade cleaning products include white vinegar, lemon juice, methylated spirits (denatured alcohol, and baking soda. Unlike the harsh chemicals found in store-bought products, COPD patients typically don’t have any reactions when exposed to these ingredients.

If you want to clean your floor or countertops, combine boiling water with either lemon juice, white vinegar, or methylated spirits. This will make a great degreaser and prove much more effective than a wet rag. If you want to clean a mirror, vinegar and water is a great combination. For removing stains, soda water is your best bet.
Keep Your Home Well Ventilated
Ventilation is imperative when it comes to keeping your home clean. Simply put, ventilation refers to the healthy exchange of air between the inside of your home and outdoors. This prevents harmful chemicals, moisture, and other allergens from concentrating in your home and posing a serious health risk. One of the best ways to ventilate your home is to simply crack a window when you’re cleaning.

If you’re worried about allergens making it into your home through the window, you can install a screen. While this won’t block out all allergens, it will prevent some of the larger particles from entering your home. Another thing you can do is change up the air filters on your HVAC system. The air filter or “particle filter” is designed to remove allergens from the air as it’s circulated throughout your home. However, over time, these filters can become very dirty. Not only will this start spiking your utility bills, but it won’t filter airborne pollutants correctly.
Choose the Right Tool for the Job
Aside from choosing the right cleaning products, you also need to choose the right tools for cleaning your home. COPD is a debilitating condition so you may need to find creative ways of doing things that won’t add any unnecessary strain on your lungs and the rest of your body. For example, if you need to clean in a hard-to-reach area, be sure to use a cleaning device with an extendable handle. This way, you won’t have to strain yourself or risk falling just to clean your home.

If you’ve been prescribed long-term supplemental oxygen therapy, another thing that can help is a portable oxygen concentrator. If you already use a stationary oxygen concentrator or oxygen tank for your oxygen needs, a portable oxygen concentrator will provide you with much more freedom to navigate your home with ease. Rather than having to be plugged into a wall outlet, POCs operate off of powerful lithium-ion batteries so you won’t be relegated to one room of the house.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Portable oxygen concentrators like the Caire FreeStyle Comfort and Inogen One G5 are very lightweight and compact, so you can carry them around all day without feeling exhausted or out of breath. The FreeStyle Comfort even has an ergonomic curve design that will prevent the unit from sliding around at your side while you’re cleaning the house. Once you’re ready for a break from cleaning, simply plug your device into the wall and by the time you’re ready to go again, you’ll have a full battery.

If you’re someone who needs more oxygen to keep you going, the Respironics SimplyGo may be the portable oxygen concentrator for you. This is a continuous flow unit meaning it puts out a constant stream of oxygen rather than “boluses” of oxygen like the FreeStyle Comfort and the Inogen G5. While the Respironics SimplyGo is a bit heavier than these two, it will provide you with more options including the ability to use your POC with your CPAP or BiPAP machine while you sleep.
Don’t Forget to Declutter Your Home
While you’re up and about cleaning your home, it’s also a good idea to spend some time decluttering your home. “Decluttering” simply means reorganizing or getting rid of some of your belongings in order to make your home more comfortable and easy to navigate. This is very important if you’re a COPD patient because having to navigate a messy home can be very challenging and dangerous.

We briefly discussed decluttering in our post about COPD and balance issues, but the basic idea is that you want to create a living space that’s accommodating of your lung condition. First and foremost, you should remove any belongings from the floor that could be a tripping hazard such as clothing, cables, and even furniture. Taking the time to move these things out of the way of where you walk in your home can go a long way toward making your home safer and more accommodating for you and your guests.

If you want to go the extra mile, you might want to consider installing a medical alert system in your home. This consists of a receiver that’s plugged into the wall and a small button that can be worn around your neck. If you take a fall or experience a COPD exacerbation in your home, simply press the button and medical personnel will immediately be sent to your home. These are a must-have for any COPD patient, especially if you don’t have friends or caretakers who visit your home regularly.
Get Outside When You Can
According to the EPA, indoor air pollution can be 2 to 5 times greater than outdoor air pollution. The reason for this is because indoor air pollutants are concentrated in a small area whereas outdoor air pollution can dissipate. While you can and should take the time to clean your home, you should be going outside as much as possible to get some fresh air.

AirNow.gov has a great air pollution map that will give you a good idea of how clean the air is in your area. Simply visit their site and type in your ZIP code. You’ll be given a number anywhere between 0 and 500 with 0 being the least polluted and 500 being the most polluted. It’s recommended that COPD patients avoid going outside if the air quality index (AQI) is over 100. However, people with severe COPD may only want to go outside when it’s below 50 AQI.
.jpg)
While the AQI is a good indication of the air quality in your area, it’s not 100% accurate. If you live in a very urban area with a lot of traffic, the air quality may be lower than what the website tells you. As such, it’s important to use your best judgment before going outside. Try going out when traffic has settled down and try to stay away from the roads as much as possible.
The temperature is another important factor to consider before going outside. Extreme conditions of any kind can lead to exacerbation of COPD. Low temperatures can be particularly difficult for COPD patients because inhaling cold air can thicken your mucus making it more difficult to breathe. Hot temperatures can cause you to feel exhausted more quickly and also exacerbate respiratory problems.
![]()
Schedule a Home Inspection
If you want to take the extra step towards making your home as accommodating as possible for your COPD, you should consider scheduling a home inspection. This is when a professional safety inspector walks through your home and performs a variety of tests designed to determine the safety of your home. While you may think of a home inspector as someone who examines the structural integrity of a home, they also play an important role in determining its cleanliness as well.
One important thing your home inspector will do is evaluate your HVAC system. This includes things like your heater, air conditioner, air ducts, and air filters. He/she will check to ensure that there are no leaks and that your system is circulating clean air throughout your home. The inspector will also look for water damage or plumbing leaks throughout the home that could lead to the growth of mold. Several types of mold, like black mold, can be very hazardous to your health. Black mold poisoning is associated with a chronic cough, fatigue, and irritation in the throat and eyes.

Home inspectors won’t fix these issues within your home. Rather, they provide you with a list of potential problems in your home and advise you on what to do or who to call to get the issues resolved. However, hiring a home inspector is still a very important step because you may be exposed to harmful airborne irritants unknowingly. Many people live with health issues for years only to find out they had a mold or HVAC problem that they were unaware of.
Recruit Help With Cleaning
There’s no doubt about it, cleaning can be exhausting. If you feel like you have a lot to clean and not a lot of time to do it, you may want to start outsourcing work to friends, family, or even a caretaker. While physical exercise is a must for any COPD patient, too much exercise or overexertion can lead to a flare-up in your symptoms, most notably chest pain, breathlessness, and fatigue.
.jpg)
There’s no shame in asking for help with cleaning your home, especially when your well-being is at stake. However, if you decide to recruit help from a friend or family member be sure to let them know about your safe cleaning routine. Let them know that you’re concerned about the chemicals in common store-bought cleaning products and show them how to make the homemade cleaning products we discussed earlier in this post.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Maintaining a healthy living environment is one of the most important things you can do as a COPD patient. Poor air quality in your home will not only irritate your skin and eyes, but it can damage your lungs and lead to flare-ups in your respiratory symptoms. COPD patients who do not breathe clean air are more likely to experience exacerbations that can lead to hospitalization.
Unfortunately, simply cleaning more often or more thoroughly is not the solution. You need to be careful about what cleaning products you’re using and how they affect the quality of air within your home. You should also take additional steps like ensuring your home is well-ventilated and that you’re keeping dust and mold in check.
If you found this post useful, don’t forget to bookmark it so you can refer back to it in the future. And if you have any questions or concerns, please don’t hesitate to leave them in the comment section below

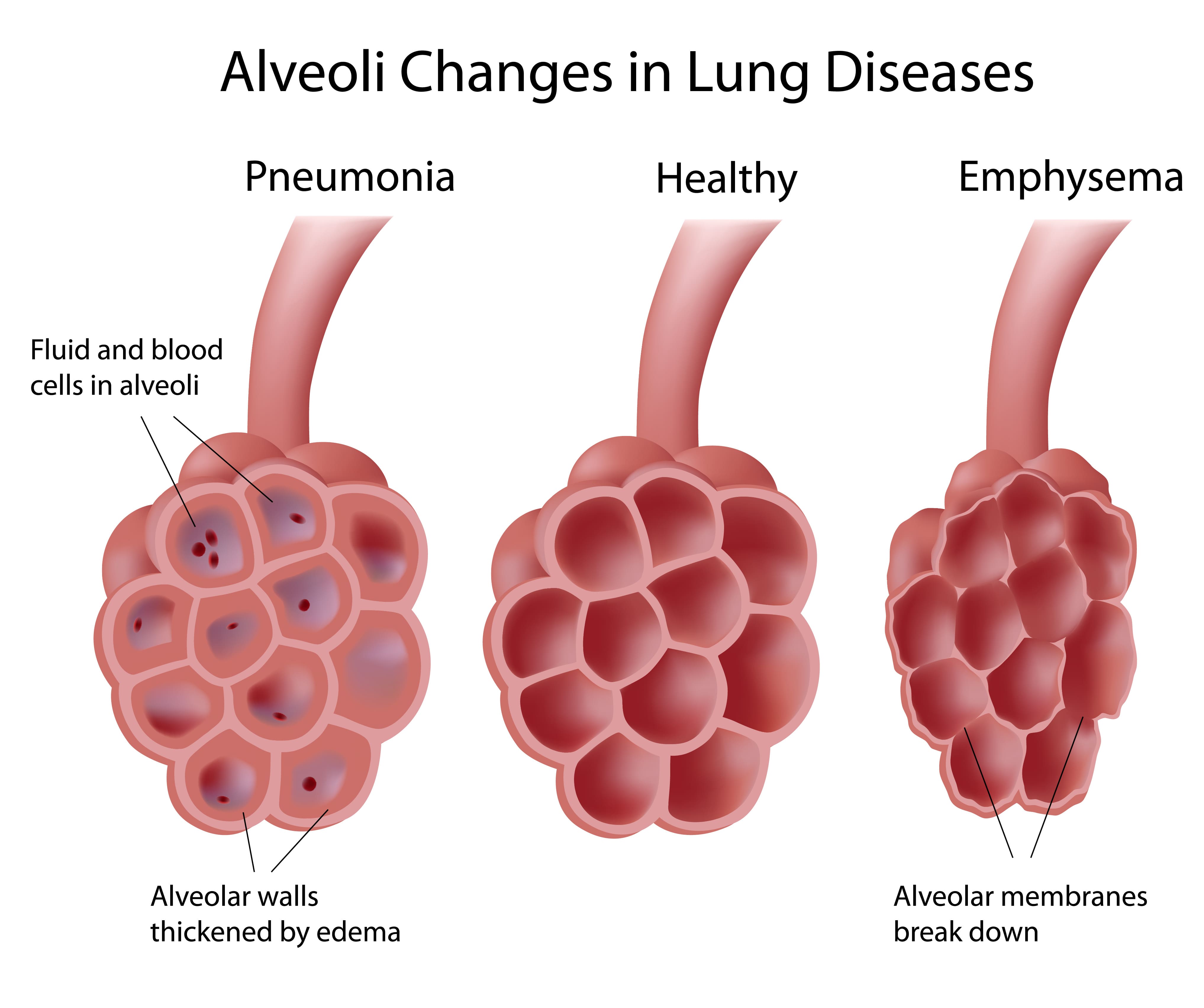
Chronic obstructive pulmonary disease (COPD) is an umbrella term used to describe one of two different respiratory ailments: chronic bronchitis and emphysema. The former is characterized by swelling and inflammation of the bronchial tubes and the latter is characterized by damaged alveoli, the small air sacs in the lungs that are responsible for the transmission of oxygen and carbon dioxide to and from the blood.
When COPD is diagnosed, patients aren’t simply given a “one-size-fits-all” treatment plan. Instead, doctors will look at several different variables such as how developed the COPD is, where it’s located, and what caused it. By doing so, he/she will be able to create a treatment plan that is customized to your specific condition.
In this post, we’re going to be looking at the early stages of COPD. This is commonly referred to by medical professionals as “stage 1 COPD” because it’s when the signs of COPD first start to emerge. If you’re diagnosed during this stage, there are several things you should know, so stay tuned to find out, and be sure to get in touch with us if you have any questions.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Symptoms of Early-Stage COPD
1.) You’re Not Alone
Did you know that about 16.4 million people in the United States have COPD and an estimated 328 million people have COPD worldwide? While it’s easy to feel alone when you’re diagnosed, in reality, it’s one of the most prevalent health conditions in the world ahead of lung cancer, diabetes mellitus, and even Alzheimer’s disease.

Unfortunately, most COPD patients don’t get this impression from watching the news, reading the paper, or simply going about their daily lives. Despite how common COPD is, it sorely under-discussed and underfunded. What’s more, there seems to be a general lack of understanding of what COPD even is.
According to the National Chronic Obstructive Pulmonary Experience (COPDE) Survey, 60 percent of respondents reported not having an action plan for dealing with exacerbations and 16 percent reported not even knowing what a COPD exacerbation was. Another study published in the European Respiratory Journal found that only about 50 percent of current or previous smokers surveyed knew what COPD was.
It’s difficult to say why COPD has less awareness in the general population and among smokers than other lung diseases, but there are definitely some likely causes. For starters, cancer often takes the spotlight these days. Cancer is one of the most talked-about chronic illnesses in this day and age. It’s the second-leading cause of death in the country, but only about one-fourth of the total cancer deaths are caused by lung cancer. This could lead to people unknowingly inflating the prevalence of lung cancer.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Another potential cause of the lack of awareness for COPD is the way it develops. While COPD tends to develop very slowly over the course of many years, lung cancer is often the opposite. Lung cancer is often considered to be one of the fastest-growing cancers and small cell lung cancer (SCLC) patients, in particular, often die after just 5 years. Another problem with lung cancer is its tendency to spread to other parts of the body.
Finally, you need to consider the fact that COPD is often affected by diagnostic error. In other words, someone may have COPD and not know it, or they might visit a doctor for their symptoms and get diagnosed with a condition other than COPD such as asthma or pulmonary fibrosis. Studies suggest that about one-fifth of smokers over the age of 40 show signs of COPD, but millions of them do not receive a diagnosis.

When you take all of these factors into consideration, along with the fact that lung cancer and COPD share the same awareness month (November), it’s not hard to see how COPD can often be overshadowed. It’s important to not diminish the awareness surrounding lung cancer because it is a very serious disease, however, it’s also important for COPD patients to know how common their illness is. What’s more, errors in spirometry testing can also lead to misdiagnosis of COPD.
2.) There is an Active COPD Support Community
Now that you’re aware of how common COPD is, you’re likely wondering what options you’ll have to get involved in the community. Luckily, there are a whole host of COPD communities out there composed of COPD patients, caretakers, researchers, medical specialists, medical device manufacturers, and more. And with how connected modern technology is, you’ll be surprised to find just how easy it is to get started.

We made a blog post in the past that covers this topic in detail, however, we’ll summarize its points here for your convenience. In simple terms, a COPD community is a place for people with COPD to come together to support each other and raise awareness for the problems they face. COPD communities can either be organized by an individual like a patient or a caretaker, or they can be created by an organization.
For example, the COPD Foundation created an online COPD forum called COPD360 Social. This forum is designed to connect and foster communication between COPD patients, healthcare professionals, caretakers, academic institutions, and researchers in order to aid in COPD prevention and management. Like other forums on the internet, COPD360 Social has a badge system that allows you to upvote a user’s responses. This way, the community decides which users are the most helpful and trusted. In order to make this platform accessible to people all across the world, it’s 100% free to use.

Another COPD organization that offers an online community is the American Lung Association. While the ALA puts a lot of their focus on lung cancer and creating cleaner air for future generations, they also host an online forum similar to the one offered by the COPD Foundation. The forum is accessed through Inspire.com. One of it’s best features is that it has a mobile application meaning you can access it via your phone or tablet from anywhere in the world.
One final COPD organization you should be aware of if you’ve just been diagnosed with early-stage COPD is COPD.net. This forum is hosted by Health Union, a social media platform designed to leverage technology to create more productive, impactful, and meaningful conversations between people with chronic illnesses. When you subscribe to COPD.net’s Help Center, you’ll receive weekly surveys and research opportunities, an e-newsletter, and you’ll be given access to the Q&A tool online.
Another great way to get involved is through social media sites. Facebook, for example, has a feature called “groups” that can be created or joined by any user. These groups are designed to bring people together to discuss specific topics and there are hundreds of them that discuss respiratory illness, smoking cessation, and other topics relevant to COPD patients. Getting started is easy. Simply go up to the search bar and type in the topic that interests you. Then click on “groups” and it will display a list of results. You can then join any group you want and begin conversing with other likeminded people.
Becoming involved in the community is extremely important for COPD patients, no matter what stage of their lives they’re in. A study published in PubMed, a public access journal, found that — regardless of the severity of COPD — most patients feel a strong desire to feel involved in social gatherings like holidays, one-on-one communication, or social media interactions. In other words, being engaged rather than simply participating gave them more of a sense of purpose in their daily lives.
3.) COPD Can’t Be Reversed, But it Can be Treated
One thing many people do when they’re first diagnosed with COPD is they immediately start searching for a cure. Unfortunately, COPD is not like an infection that can be cured with antibiotics and it’s not like a headache that will go away with time. COPD is permanent and it’s progressive meaning it can only get worse.

While this may seem like a pretty grim reality, it’s actually not! If you’re careful to implement effective lifestyle changes you’ll be able to drastically slow the progression of your disease, reduce respiratory symptoms, and experience peace of mind. But in order to make these changes, you need to know a little about COPD and what causes it.
COPD is the result of chronic inflammation in the lungs and airways. 85 to 90 percent of COPD cases are the result of cigarette smoking, but there is also a condition called Alpha-1 deficiency that leads to the onset of COPD in non-smokers. Alpha-1 is a protein that regulates immune reactions in the lungs, and when it’s not produced in high enough quantities, it can make your lungs vulnerable to permanent damage.

Over time, this inflammation becomes worse and further impairs your breathing so it’s imperative that you avoid anything that could irritate it such as cigarette smoke, car exhaust, or any other type of air pollution. It’s also important to avoid infection because this is the leading cause of COPD exacerbations (when symptoms rapidly get worse).
Supplemental oxygen therapy is one of the best ways to stabilize your condition, reduce respiratory symptoms, and improve your life expectancy. In the past, COPD patients would need to carry around bulky oxygen tanks, but portable oxygen concentrators have since replaced them as a lightweight and more convenient alternative.

Another key component of a COPD treatment plan is pulmonary rehabilitation. This is similar to how you would go through a physical therapy course if you sustained an injury to your legs or back but it focuses on the lungs. Not only will pulmonary rehab show you how to exercise effectively with COPD, but you will learn important lessons about how your lungs function and how to keep them healthy.
Last but certainly not least is the dietary component of your treatment plan. While it may not seem like your diet would have an immense impact on COPD progression, it actually does. Evidence suggests that antioxidants found in fruits and vegetables have anti-inflammatory properties that have positive effects on people with COPD and asthma. Similar studies also found that soluble fiber intake has the potential to protect against airways inflammation.
Conversely, foods that lead to weight gain, obesity, and fatigue can all add to your COPD symptoms. Studies have found that obesity can lead to alterations in immune function, insulin resistance, and dyslipidemia (an abnormal amount of lipids in the blood). However, being underweight with COPD has its problems as well, so a healthy weight should be your goal.
Supplemental oxygen, pulmonary rehab, and diet are a few, but not the only methods of treating COPD. Above all, you should be open and honest with your doctor about your symptoms so that he/she can create a treatment plan that’s based on your needs.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
4.) It’s the Best Time to Quit Smoking
If you haven’t done so already, now is the perfect time to quit smoking. As aforementioned, 85 to 90 percent of COPD cases are caused by smoking but it’s also important to remember that the majority of people who smoke are never diagnosed with COPD. Rather, they develop other chronic diseases such as lung cancer, diabetes, and heart disease. According to the Cleveland Clinic, smokers have a 70 percent higher risk of dying from coronary artery disease than nonsmokers.

Since smoking causes COPD, it can also make COPD symptoms worse by increasing the rate of inflammation in the lungs and airways. Smoking is known as an immunosuppressant drug meaning it reduces your body’s ability to prevent infection temporarily. Since infection is the leading cause of COPD exacerbation and we’re in the middle of a pandemic, smoking is the last thing you want to do!
5.) It’s the Best Time To Implement Long-Term Goals
Many people go their whole lives without implementing long-term goals. This can be very detrimental if you want to achieve your full potential, especially when it comes to your health. Whether you’ve been a long-term planner before or you’ve always stuck to short-term goals, there’s never been a better time to start.
As we’ve already established, smoking cessation should be your first goal, but ideally, this should be a short-term goal because immediate cessation is will help you better achieve your long-term goals. But aside from this, your first goal should be to create a COPD action plan and implement it successfully.
A COPD action plan is a personalized plan for managing your symptoms and exacerbations. For example, it could remind you how much you need to exercise each day or what foods you need to avoid in order to prevent respiratory flare-ups. We made a whole blog post about this subject so don’t hesitate to check it out.
6.) It’s Not the End
The last, but probably most important thing you should know about early-stage COPD is that it does not signify “the end” of your life. Not only that, but it is not even the beginning of the end. While being diagnosed with COPD is certainly not a positive experience, it is possible to achieve a positive outlook by changing your mindset and practicing healthy habits.

One positive thing to focus on is that COPD patients enjoy a far greater life expectancy than people with other chronic diseases. On average, a current smoker with stage 1 COPD has a life expectancy of 14 years. Compare this to the 50 percent of heart disease patients who live past 5 years or the 16 to 24-month median survival rate for small-cell lung cancer patients.
But it’s not just about survival rate, it’s also about quality of life. COPD patients who implement effective and proven treatment strategies like supplemental oxygen therapy, pulmonary rehabilitation, and an improved diet see improved quality of life.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Final Thoughts
COPD is a serious debilitating disease, but it is by no means the final straw. Even if you have been diagnosed with early-stage COPD, you have a lot of life to live and it can be enhanced by closely adhering to your doctor’s instructions.
In the meantime, getting involved in the COPD community, taking care of your mental health, and quitting smoking are all important steps to take after you receive a diagnosis. Doing so will ensure that you live a long, happy, and fulfilling life.
.png)
Chronic obstructive pulmonary disease (COPD) is one of the most substantial health burdens in the world. According to the Centers for Disease Control and Prevention, “chronic lower respiratory disease” (primarily COPD) is fourth on the list of leading causes of death worldwide, behind heart disease, cancer, and unintentional accidents. And despite the fact that fewer people are smoking than ever before, experts are expecting the number of COPD cases to rise within the next 50 years.
While the vast majority of COPD cases are caused by cigarette smoking, many people are surprised to find that COPD is a diverse group of diseases that have a multitude of different causes. One of the other major causes of COPD is alpha-1 antitrypsin deficiency. This is a genetic condition that inhibits proteins that are responsible for protecting the lungs from inflammation and long-term damage. Other factors such as air pollution, irritants, and chemicals can contribute to the onset of COPD. However, these are more commonly associated with interstitial lung disease (ILD).
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
COPD is divided into two different types: chronic bronchitis and emphysema. Bronchitis affects the airways and emphysema affects the lungs. Many COPD patients have both of these diseases simultaneously but it is possible for someone to contract one without the other. And while many people think of emphysema as one disease, it’s actually divided into three different morphological categories. Depending on which one you have, you may require different treatments to manage your symptoms effectively.
In the following sections, we will provide you with an overview of emphysema as well as the three different subtypes. If you have any questions, don’t hesitate to reach out to us by leaving a comment or contacting us by phone or email.
What is Emphysema?
Emphysema is a condition that’s caused by the deterioration of lung function due to the loss of lung elasticity and the deterioration of the alveolar walls. The alveoli are tiny air sacs located at the end of the bronchioles, the small airways that lead into the lungs. There are around 300 to 500 million alveoli in the lungs, and they’re microscopic, so they’re extremely sensitive to foreign substances like cigarette smoke, chemicals, and air pollution.
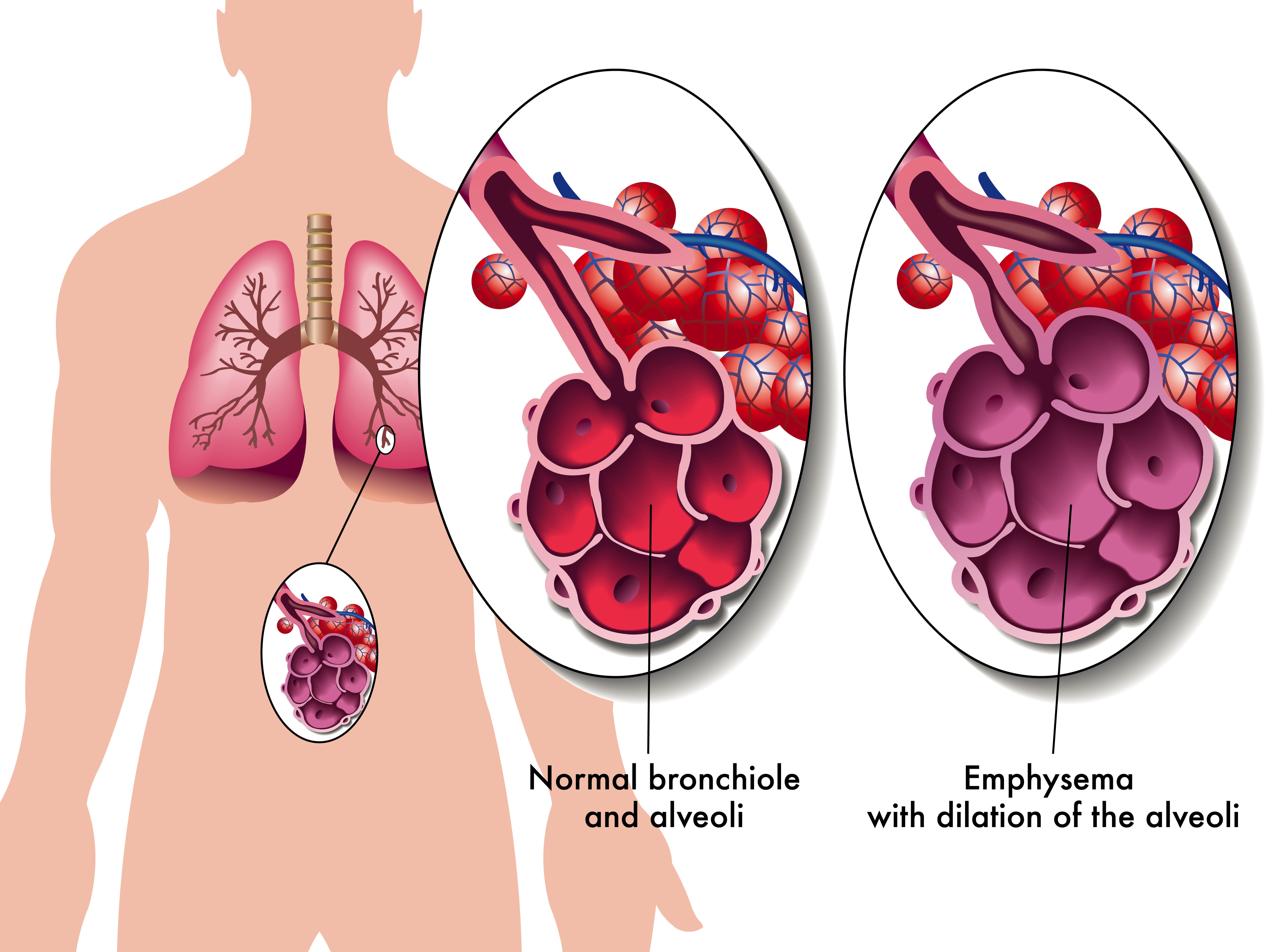
The alveoli play a vital role in the respiratory system because they transfer oxygen from the air that you breathe into the bloodstream. They also remove carbon dioxide from the bloodstream and send it back out of the lungs. This process is called diffusion and it is one of three processes that your lungs perform. Unfortunately, due to how complex the respiratory system is, if the process of diffusion is impaired, this can cause a lot of problems for the other two processes of the respiratory system: ventilation and perfusion.
Not only do alveoli transfer oxygen and carbon dioxide to and from the blood, but they’re also responsible for the spongy and elastic consistency of the lungs. As the walls of the alveoli break down, the elasticity of the lungs is lost and they become less efficient at absorbing air. Another issue this can cause is stagnant air that gets trapped in diseased areas of the lungs which can significantly increase the energy it takes to breathe and result in hyperinflation of the lungs. This also gives emphysema patients their “barrel-chested” appearance which is so often associated with the disease.
What Types of Emphysema Are There?
There are three types of emphysema that differ in terms of what causes them and the area of the lungs that are affected. Depending on which type of emphysema you’re diagnosed with, your doctor may have drastically different treatment options. No two cases of COPD are the same so your physician will work with you to determine what treatment will benefit you most.
Centriacinar Emphysema
Centriacinar emphysema (also called centrilobular emphysema) is a condition that affects the upper lobes of the lungs. Most often this type of emphysema starts in the middle of the lungs and progresses outwards. Centrilobular emphysema is almost always caused by smoking and second-hand smoke and it’s more common in people who’ve been diagnosed with coal workers’ pneumoconiosis (CWP) in the past.
Panacinar Emphysema
Panacinar emphysema (also called panlobular emphysema) is a condition that affects the entire acinus distal to the respiratory bronchioles. The acinus refers to the area at the end of the bronchioles and includes the alveolar ducts, alveolar sacs, and alveoli. It differs from centrilobular because it’s usually located in the lower parts of the lungs. Panacinar emphysema is most commonly caused by homozygous alpha-1 antitrypsin deficiency.
Alpha-1 antitrypsin deficiency (A1AD) is a hereditary disorder that causes low levels of the protein alpha-1 antitrypsin (A1AT) in the blood. This protein is made and released from the liver and it protects tissues in the lungs from being attacked by its own enzymes. A1AD patients may either experience abnormal proteins, poor production of these proteins, or both. All things considered, A1AD is a rare disease and it only amounts to a small percentage of the people diagnosed with COPD.
Paraseptal Emphysema
The third and final morphological subtype of pulmonary emphysema is called paraseptal emphysema. This type is usually localized around the septae or pleura in the lungs. This is a thin sheet of tissue that’s located around the outside of the lungs and inside the chest cavity. This type of emphysema is commonly associated with prior lung infections.
What are the Causes and Risk Factors of Emphysema?
Causes
Cigarette Smoking
Smoking is the most considerable cause of emphysema and all conditions under the umbrella term “COPD.” According to the Centers for Disease Control and Prevention (CDC), 80 percent of people with COPD have smoked in the past or are current smokers. Additionally, 38 percent of people who live with COPD continue to smoke. Despite these facts, only about 10 to 15 percent of smokers will develop some form of COPD. Smoking is more likely to cause cancer, heart disease, stroke, diabetes, and other chronic illnesses.

According to the Cleveland Clinic, the greatest predictor for someone developing emphysema from smoking is not whether or not they were a “light” or “heavy” smoker, it’s how long they smoked for — the longer someone smokes, the more likely they are to contract COPD. This is why doctors will always recommend immediate smoking cessation rather than simply “cutting back” on cigarettes.
Secondhand Smoke
Secondhand smoke refers to the inhalation of cigarette smoke involuntarily as a result of someone else smoking. While there is a commonly held belief that secondhand smoke is worse than actually smoking, this is not the case. The toxicology of tobacco smoke is the same regardless of whether it was inhaled intentionally or not. Either way, cigarette smoke in any form can cause COPD and emphysema.

It’s estimated that there are over 7,000 chemicals in cigarette smoke and smoke can linger in the air for several hours. In other words, living with a smoker or being in an area where someone has smoked recently will put you at a higher risk of chronic lung disease. Cigarette smoke dissipates more quickly outdoors so, generally speaking, it’s safer to be outside.
Air Pollution
Air pollution is a major contributor to the onset and progression of emphysema. According to the World Health Organization (WHO), there are five major types of air pollution: particulate matter, ground-level ozone, nitrogen dioxide, sulfur dioxide, and carbon monoxide. All of which can be inhaled into the lungs and cause permanent damage to the bronchioles and alveoli. Just like with cigarette smoking, the more you’re exposed to air pollution, the more likely it is to cause permanent damage to your lungs.
![]()
One great tool to help you learn about the air pollution in your area is AirNow.gov. All you have to do is enter your city or zip code and it will provide you a number between 0 and 500 with 0 being the least polluted and 500 being the most polluted. The EPA recommends that you should not go outside if the Air Quality Index (AQI) is above 150. However, if you already have a chronic lung disease like asthma or COPD, you should avoid going outside if the AQI is above 100.
What are the Four Stages of Emphysema?
Much like other chronic illnesses that take many years to progress, emphysema is broken down into different “stages” which medical professionals can use to identify the severity of your disease. Since early-stage emphysema has very mild symptoms, it’s often underdiagnosed or misdiagnosed as other chronic lung conditions such as asthma. Read below to learn about the four stages of emphysema.

Stage 1
Stage 1 emphysema is very mild. In fact, it’s often so mild that it is undetected and undiagnosed. People with stage 1 may experience a cough, minor chest pain, and some breathlessness. Stage 1 emphysema patients have a forced expiratory volume in one second (FEV1) of 80% or more.
Stage 2
Stage 2 is slightly more advanced than stage 1. This is when many people start to see their doctor because they begin to realize that their respiratory symptoms aren’t the result of aging or an acute condition. Stage 2 emphysema patients have an FEV1 between 50% and 80%.
Stage 3
By the time someone reaches stage 3 they have most likely received a diagnosis from their doctor. They’ve likely had several flare-ups in the past year and have been admitted to the hospital at least once. Stage 3 patients have an FEV1 between 30% and 50%.
Stage 4
Also known as “end-stage COPD,” this stage is characterized by severe breathlessness, coughing, wheezing, and fatigue which leads to exacerbations and hospitalization. Stage 4 patients have an FEV1 of less than 30%.
How is Emphysema Treated?
Supplemental Oxygen Therapy
Because emphysema can result in low blood oxygen levels (hypoxia) supplemental oxygen can be used to stabilize a patient’s oxygen levels and help alleviate emphysema symptoms like breathlessness, chest pain, and coughing. However, it’s important to note that oxygen therapy can be dangerous if it’s not used in the way that your doctor intends for you to use it. Oxygen is a controlled substance in the United States, so you’ll need a prescription in order to rent or buy an oxygen device.

There are many choices to consider when it comes to oxygen delivery devices so you’ll need to find one that best suits your needs and your lifestyle. Oxygen tanks are a very popular choice because they have a low upfront cost. However, they’re very heavy and need to be refilled constantly making them a poor choice for most oxygen users. Liquid oxygen tanks are an upgrade because they last longer and aren’t as heavy, but they cost more to maintain.

The best alternative to both of these is portable oxygen concentrators. An oxygen concentrator is an electronic device that takes in ambient air and removes nitrogen, argon, and other gases, then puts out medical-grade oxygen. The benefit of this is that you simply need to charge the batteries on your concentrator which is much more convenient than having to have an oxygen company fill your tanks.
Pulmonary Rehabilitation
Many years ago, exercise was not recommended for COPD patients because it was believed to exacerbate symptoms and increase the rate at which the disease progressed. However, in this day and age, pulmonary rehabilitation (exercise that’s focused on lung function) is championed as one of the best ways to treat chronic respiratory illness. This is due to a mounting body of evidence that shows even moderate exercise can improve COPD symptoms.

While you can exercise at home on your own time, it’s recommended that you start with a pulmonary rehabilitation program. Not only do these programs teach you how to exercise with emphysema, but they will also teach you important information about your disease and how it should best be managed. Read this post to learn more about how pulmonary rehabilitation works.
Dietary Changes
If you live by the motto “you are what you eat,” you probably understand the importance of a healthy, well-balanced diet. Nutrition affects everything from your heart health to your lung health and everything in between, so it’s wise to follow your doctor’s instructions on eating healthier meals. According to Lung.org, the metabolism of carbohydrates creates the most carbon dioxide, so they should opt for healthy fats instead which produce the lowest amount of carbon dioxide. HIgh-protein diets are also good for emphysema patients because they keep your lungs strong and efficient.
![]()
Medication
Emphysema treatment usually involves some combination of oral and inhaled medication. Oral steroids can provide you with short- or long-acting relief from your symptoms whereas inhaled medication like bronchodilators are designed to open up your airways quickly in the event of a COPD exacerbation. Your doctor will discuss with you exactly which medications you will need and when to use them.

Most oxygen patients are prescribed inhalers, nebulizers, or both. An inhaler is a portable device that administers medication in a mist form called “aerosol.” this enables the patient to administer the medication directly to their lungs thus allowing it to take effect more quickly. Nebulizers play a similar role in an emphysema treatment plan but they administer medication in a stream rather than a “puff” making them easier to use for most people.
Lifestyle Changes
There are many other lifestyle changes that you can make to treat emphysema and alleviate your symptoms. Focusing on getting more consistent and restful sleep is one way that you can feel more alert and prepared to take on the challenges of your disease. Ultimately, you should discuss your sleeping habits with your doctor to ensure that you’re doing everything you can to get a good night’s sleep.
![]()
Another lifestyle change you can make is changing your cleaning habits. Many common household cleaners are filled with dangerous chemicals like bleach and ammonia. When these substances are inhaled they can cause COPD exacerbation which leads to increased coughing, wheezing, and shortness of breath.
Conclusion
COPD is one of the most preventable chronic illnesses in the world and emphysema is one disease under this umbrella term. Emphysema patients experience impaired lung function due to a breaking down of the alveoli, or tiny sacs in the lungs that transfer oxygen and carbon dioxide to and from the blood. While there is no cure for emphysema, patients can experience significant relief and improved life expectancy with a carefully planned treatment routine.
Here at LPT Medical, we want COPD patients to experience relief from their respiratory symptoms while experiencing the freedom and independence they had before being diagnosed. If you haven’t done so already, ask your doctor if you might benefit from using a portable oxygen concentrator like the Inogen One G5 or the Caire FreeStyle Comfort. Both of these machines have a high oxygen output, they’re lightweight and easy to carry.
.png)
Whether you have a friend or a loved one with COPD or you have COPD yourself, you can likely attest to the fact that this disease can cause significant problems with mobility. The top causes of mobility issues in COPD patients include poor pulmonary function, leg swelling (peripheral edema), and loss of muscle mass (muscle atrophy). Combined with the effects of aging and other chronic conditions like osteoarthritis, COPD patients can experience a lot of difficulties getting around in their day-to-day life.
Aside from supplemental oxygen therapy, a healthy diet, and pulmonary rehabilitation, another thing that can help you get around are mobility aids. A mobility aid is a device that’s used to help older people and people with chronic conditions walk more easily. They’re often designed to improve balance, reduce physical load, and in COPD patients, they can even help to prevent exacerbations and flare-ups. There is a huge variety of mobility aids and you’re not just limited to choosing one or the other.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following sections, we’ll help you better understand the mobility options available to you as well as some other helpful information that will help you maintain your mobility as a COPD patient. As always, if you have any questions, please be sure to address them in the comment section or consult your doctor for more specific information pertaining to your disease and treatment plan.
Why Are Mobility Aids Important for COPD Patients?
According to an article published in the National Center for Biotechnology Information, balance deficit is a common issue among COPD patients. COPD is a progressive disease meaning it becomes worse over time. And as symptoms like breathlessness, chronic fatigue, and chest pain progress, so do issues related to balance and mobility. Believe it or not, studies have shown that COPD is one of the chronic illnesses with the highest rate of falls next to osteoarthritis.
Several months ago, we wrote an article discussing a common complication of COPD called peripheral edema. In short, this is a condition where your legs or feet begin to swell due to a buildup of fluid. One of the root causes of this condition is pulmonary hypertension or high blood pressure in the lungs. High blood pressure in the lungs puts more strain on the heart and prevents oxygen-rich blood from circulating to organs like the liver and kidneys. Since these organs are responsible for removing fluids from the body, swelling of the feet or legs are usually a sign of this happening.
While peripheral edema is a complex condition, it’s one of the issues contributing to the high risk of falls in COPD patients. As the disease progresses, COPD patients don’t just have to deal with increased respiratory symptoms, they have to deal with complications that can result from their disease. Someone with peripheral edema may not even realize they have it because it often comes on slowly and doesn’t cause any pain.
-jpg.jpeg)
Another issue contributing to the high rate of falls in COPD patients is muscle atrophy. In other words, as COPD progresses, patients tend to lose muscle mass from a variety of issues like a changed diet and reduced physical activity. Similar to peripheral edema, a patient may not realize that they are losing muscle mass until they experience a fall. This is why pulmonary rehabilitation is such an important part of any COPD treatment plan.
One final problem that can contribute to the fall rate in COPD is an exacerbation. An exacerbation is an event where respiratory symptoms suddenly worsen. According to COPD.com, the most common cause of exacerbation is a bacterial infection, but air pollution is another common cause. COPD exacerbations can lead to problems walking, balance issues, chest pain, headaches, and confusion, all of which can increase your risk of falls.

While mobility aids are not a replacement for your treatment plan, they play a crucial role in preventing falls, especially in people with late-stage COPD where the disease is the least predictable. Mobility aids don’t need to be prescribed by your doctor so it’s up to you and your loved ones to determine whether you need one or not. Continue reading to learn about some of the mobility options available to COPD patients.
Canes
Walking canes are the oldest type of mobility aid and they’re also one of the simplest. Most walking canes are made of wood or a light metal material meaning they’re easy to carry despite your level of physical impairment. Canes are also widely accessible, and you can buy them just about anywhere, or you could even make your own if you have time. Walking canes are great for taking weight off your joints and providing you with a little extra stability as you walk.

The key to improving your mobility with a cane is to get one that’s the appropriate size. While there is no hard and fast rule as to how you should choose a cane, it should be long enough that you aren’t bending over and straining your back in order to use it and it should be short enough that you can actually lean on it. For most people, this will be somewhere around their hip bone. Luckily, most modern canes are adjustable, so you’ll probably be safe buying one online rather than shopping around for one.

One thing to consider if you want to use a cane is how you will carry your supplemental oxygen device. If you have an oxygen tank and you wheel it behind you using a rolling cart, a walking cane might not be the best option for you because you won’t have any hands free to catch yourself if you fall. A cane is a better option if you carry your oxygen device on your back because it will help you keep a good posture as you walk.
Walkers
Walkers are another mobility option available to COPD patients. There are several different types including traditional walkers, two-wheel walkers, and four-wheel walkers. Traditional walkers tend to be a poor choice for most COPD patients because they need to be picked up as you walk which can be strenuous on your shoulders, arms, and back. Two-wheel walkers provide a little more mobility by allowing you to push the walker rather than lift it. However, for most people, four-wheel walkers, or “rollators” as they’re often called, will be the best option.

Modern rollators are more advanced than other types of walkers because they offer four swivel wheels that afford you more control. They also offer a braking system that’s controlled by two levers on the handlebars on either side of the device. They also provide a padded platform in the middle that you can either sit on or rest your oxygen device, purse, or handbag on as you walk. Some rollators even have a basket in front for added storage.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
It’s a good idea to speak with a mobility aid expert if you want to get a rollator. Since these devices are so popular, there are many different versions and brands available to choose from. What’s more, it’s easier to use one if you’ve been shown how to do so by someone who’s experienced with them. You’ll also need to have one fitted unless you can find one that’s adjustable.
Wheelchairs
When you think of a mobility aid, chances are, wheelchairs are the first thing that comes to mind. They’re commonly used by people who are permanently disabled, but how do they fare when it comes to someone with limited mobility? The answer ultimately depends on your individual circumstances. COPD patients with poor upper body strength may find it difficult to get around in a manual wheelchair, but if you have a caretaker or loved one who can push you around it shouldn’t be a problem.

Another option for you are motorized wheelchairs or “power wheelchairs” as they’re often called. The benefit of investing in a power wheelchair is that you will have the same mobility as a manual wheelchair, but you won’t have to push it with your arms. Power wheelchairs have a joystick that you use to move in any direction. They’re not overly complicated to operate but they can be difficult to transport and you’ll need to keep it charged if you want to stay out of the house for extended periods of time.
Scooters
Mobility scooters are similar to power wheelchairs but they differ in terms of their design. Unlike power wheelchairs which use a joystick, scooters are controlled with handlebars similar to a bike. Scooters can either have three or four wheels depending on what your preferences are. They also have baskets on the front that you can use to store things like your portable oxygen concentrator, a purse, or other personal belongings. Since there are so many options available when it comes to mobility scooters, it’s important to speak with an expert who can align you with the exact product you’re looking for.

Stairlifts
Stairlifts are a mobility aid that many people have never heard of, but they’re incredibly useful. Essentially, a stairlift is a chair that moves up and down a rail that’s installed on a flight of stairs in your home. The chair has a built-in motor that can be controlled with a joystick on the handlebars. This allows you to navigate the stairs in your home without the risk of experiencing a dangerous fall. The one downside to stairlifts is that they can be very expensive and many people can’t justify spending the money to have one installed in their home.

Surprisingly, stairlifts are extremely versatile and can be installed on most staircases regardless of their size or shape. What’s more, if you like to get outside, there are specially designed stairlifts that can be installed on outdoor staircases. They can be installed in several hours so you won’t have to wait days or weeks to start using them.
Will Medicare Pay for a Mobility Aid?
Whenever it comes to medical equipment, questions about health insurance and Medicare are sure to follow. And while it would be nice if Medicare paid for medical expenses like you’d expect them to, it’s never that simple. More often than not, they will cut corners providing you coverage for mobility aids and find any way they can to offer you the bare minimum rather than what you deserve.

In short, Medicare will provide some compensation for manual or power wheelchairs and scooters. Mobility devices like these are covered under Medicare Part B and it is classified as durable medical equipment (DME) the same as oxygen tanks and portable oxygen concentrators. But it’s important to note that not all devices are covered. Medicare has a list of devices that are covered, and some of them require prior authorization. So, it’s best to consult with both the mobility aid supplier and a Medicare representative before you make any decisions.
.jpg)
Another thing to note is that Medicare has a long list of prerequisites that you need to meet in order to qualify for compensation. First and foremost, the doctor that has prescribed you with COPD and the mobility aid supply company needs to be enrolled in Medicare. Additionally, you’ll need a written order from your doctor stating that you have a medical need for a mobility aid. For a full list of requirements, refer to the wheelchair and scooter benefit page of Medicare Part B.
Get a Handicap Parking Permit
Once you have your mobility aid of choice, you may want to consider getting a handicap parking permit. This permit will allow you to park in any handicap spot in the country making it much easier for you to get around. This is especially useful for people who are using electric scooters or power wheelchairs because you won’t have room to unload it in a standard parking spot.

In order to get a handicap parking permit, you’ll need to apply at your local Department of Motor Vehicles (DMV). Every state has different policies but you’ll likely have to provide a doctor’s note which outlines your lung condition and symptoms. You’re more likely to get approved if you can prove that you use an electric scooter or power wheelchair as opposed to a cane or walker so it’s best to put time into finding a mobility aid first.
.jpg)
Last but not least, if you’re given the option between a handicap sticker that goes on your car or a placard that you hang on the mirror, always go with the placard. This is because you can transfer these to any car that you’re in whether it belongs to a family member or friend. Be aware that it is illegal for them to use the placard without you actually being present and most states require you to be recertified for your handicap permit every couple of years.
Conclusion
Making the decision to use a mobility aid is an important step for many COPD patients. People with chronic respiratory conditions are at a higher risk of experiencing falls than the general public, but mobility aids will help to support your balance whether you’re inside or outside the home. Unfortunately, there is no one-size-fits-all solution. Everyone has their own needs and preferences so you should consider all options available to you.
Canes and walkers are a good place to start because they’re affordable and they’re easy to carry. However, you may want to consider a more long-term solution like a mobility scooter or power wheelchair. These devices are generally safe and easy to use, and they will make it easy to carry around your oxygen devices such as your oxygen tank, liquid oxygen tank, or portable oxygen concentrator.
Lastly, you should check with your health insurance to see if your mobility device is covered. This could save you hundreds if not thousands of dollars. You can also file for disability and receive a handicap parking permit which will afford you more convenience and freedom whenever you leave the house. In the meantime, if you’re looking for a lightweight and easy-to-use portable oxygen concentrators such as the Caire FreeStyle Comfort or the Inogen One G5, don’t hesitate to reach out to your respiratory specialists here at LPT Medical.
Chronic obstructive pulmonary disease (COPD) is an umbrella term used to define two different types of lung disease: chronic bronchitis and emphysema. The former is a condition that impairs the bronchioles, the airway tubes that lead into the lungs. The latter affects the tiny air sacs in the lungs called the alveoli. These are responsible for the transfer of oxygen and carbon dioxide to and from the bloodstream. Both chronic bronchitis and emphysema are called “obstructive” diseases because they make it more difficult for the patient to expel air from the lungs, thus leading to a buildup of CO2 in the blood.
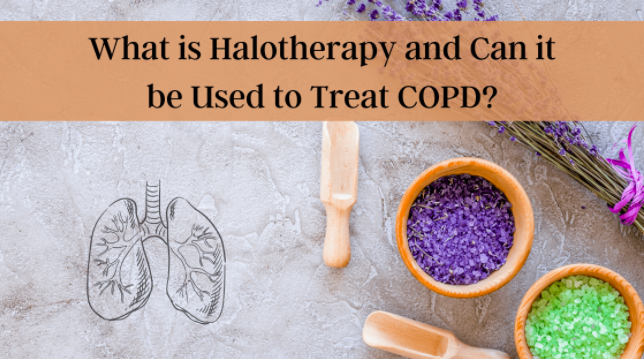
When a patient is diagnosed with COPD, they’re typically prescribed a standardized treatment plan including but not limited to supplemental oxygen therapy, a specialized diet, pulmonary rehabilitation, and breathing exercises. These are all clinically proven techniques that will help to prevent breathlessness, chest pain, and improve long-term prognosis. While most COPD patients adhere to these well-researched practices, some people look for additional “home remedies” to treat their disease. These are usually referred to as “alternative therapies.”
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Here at LPT Medical, we don’t advise using any type of alternative therapy unless it’s explicitly approved by your doctor or pulmonologist. Some alternative therapies and medications are touted as “cure-alls” or “cheap alternatives” to standardized medications, but more often than not, they don’t live up to their hype and they can even result in further damage to your lungs. In this post, we’re going to tell you all about the alternative therapy called halotherapy, or more commonly known as salt therapy. If you have any questions, please feel free to leave them in the comment section below and we’ll get back to you as soon as possible.
What is Halotherapy and How is it Used?
The term “halotherapy” comes from the Greek word “halos” meaning “salt.” In other words, it’s the use of salt as a therapy for a variety of different ailments. The idea of using salt as a type of therapy is believed to have originated in Europe several hundred years ago. Miners, who are known to contract deadly lung diseases (pneumoconiosis) like black lung and silicosis due to their exposure to mineral dust, did not experience the same effects when they worked in salt mines. Rather, salt mine workers appeared to thrive and experience great lung and skin health.

It wasn’t until 1826 that the first salt therapy facility was opened by a Polish physician named Feliks Boczkowski. At this treatment facility, he offered salt baths from naturally occurring underground brine. After World War II, Dr. K.H. Spannahel created a systemic approach to the climatological conditions of salt caves and attempted to confirm their medical effectiveness. Together, these two physicians helped to lay the foundation of modern speleotherapy (salt cave therapy).
Nowadays, there are many different types of salt therapy used to treat a variety of different conditions. Below are just a few:
Wet Salt Therapy
This therapy got its name because it involves the use of salt combined with water vapor. Wet salt therapy is one of the most common types of salt therapy and it’s also one of the easiest and most accessible for most people. It includes things like salt scrubs, salt baths, salt nebulizers, and saline solutions.

Dry Salt Therapy
This is a type of salt therapy that is completely void of moisture or humidity. This is considered the most “traditional” type of salt therapy and it includes salt caves, salt grottos, salt rooms, and salt chambers. Dry salt therapy is said to have many benefits for the body including improved breathing and softer skin.
Speleotherapy
“Speleo” is derived from the Greek word spḗlaion meaning caves. Speleotherapy is a type of salt therapy that involves going into naturally occurring caves below the earth’s surface. It’s believed that the natural climate and environment of these caves is great for treating respiratory diseases like asthma and chronic obstructive pulmonary disease.

Active Salt Rooms
This type of salt room uses a halogenerator. This is a device that crushes pure sodium chloride into a fine powder that can be dispersed as an aerosol into the room. This is done in a confined room where the amount of salt in the air can be closely monitored by a specialist. The climate and humidity of these rooms are also closely monitored.
%20(2).jpg)
Passive Salt Rooms
This is similar to active salt rooms but there is no halogenerator that puts out salt particles in the air. Rather, a passive salt room simply has blocks of various types of salt including Himalayan, Mediterranean, Caribbean, or Rock salt, and they’re designed to mimic the effects of being in an actual naturally occurring salt cave. Many people claim that having large quantities of salt like this in a confined space creates positive energy frequencies and a clean-air environment. This is also a major selling point for products like salt lamps which are very popular nowadays.
Can COPD Patients Benefit from Salt Therapy?
Now that you know a little bit about what salt therapy is, you’re probably wondering if there are any proven benefits for COPD patients. Unfortunately, there isn’t a simple “yes” or “no” answer to this. Despite being around for hundreds of years, there isn’t a significant amount of research done on the topic, and many health experts have conflicting opinions about how it should be used, or if it should even be used at all.

The reason salt therapy is associated with COPD in the first place is because of its antibacterial and anti-inflammatory properties. Hundreds of years ago, before the invention of refrigerators, salt was used to preserve meat. This worked because salt draws the moisture out and prevents harmful bacteria from forming. Proponents of salt therapy believe this can also benefit the respiratory system of COPD and asthma patients by killing harmful bacteria that could lead to infection.
Proponents of salt therapy also claim that salt can reduce inflammation in the lungs and airways, loosen excess mucus, and reduce immune system oversensitivity, all of which are symptoms of COPD. However, most of these claims have very little evidence backing them up and many studies have even shown that salt therapy can actually exacerbate the issues above rather than help to cure them.
According to the Asthma and Allergy Foundation of America (AAFA), inhaling concentrated salts (hypertonic saline) or any crystalloid solution containing more than 0.9% saline is proven to make asthma and COPD worse by irritating the airways, increasing mucus production, and causing a cough. As such, it’s important to understand the concentration of salt in the therapy you’re receiving.
Another important thing to note is that the popularity of salt therapy does not affirm its efficacy. Just turning on your TV or browsing the internet, you’re likely to see advertisements for salt therapy caves, salt lamps, and salt inhalers, and you likely hear claims that they can cure chronic illness, but this doesn’t make them true. Since salt therapy is not classified as an FDA approved medication, it’s also not regulated the way that your traditional COPD medication is.
That doesn’t make them completely immune to responsibility, however. With the advent of the novel coronavirus (COVID-19), salt therapy companies have been under close watch by the FDA when it comes to the claims they make about their products. Some salt therapy companies have made wild claims about their products curing or treating COVID-19 when there is little or no evidence to suggest this is the case. If you’d like to learn more about how these types of products are regulated, read through our post about dietary supplements.

Last but certainly not least, there’s a problem with a placebo effect concerning salt therapy. A lot of the research on salt therapy has been inconclusive because it’s based on anecdotal evidence. In other words, many patients are reporting that salt therapy is beneficial to their health, but there is little evidence to suggest there was a physical change to their disease. Rather they have an expectation that something will change, so that’s what they believe. This is a great selling point for many salt therapy companies because, generally speaking, people trust the opinion of others.
Should COPD Patients Use Salt Therapy?
The most important thing to remember when it comes to alternative therapies or home remedies is to always consult your doctor first. Your doctor may have additional insight into why you should or should not be using salt therapy and he/she will help you weigh the risks. You should also do research on the specific salt cave that you want to visit. While some of these places are sanitized regularly, others are teeming with bacteria which could increase your risk of respiratory infection.
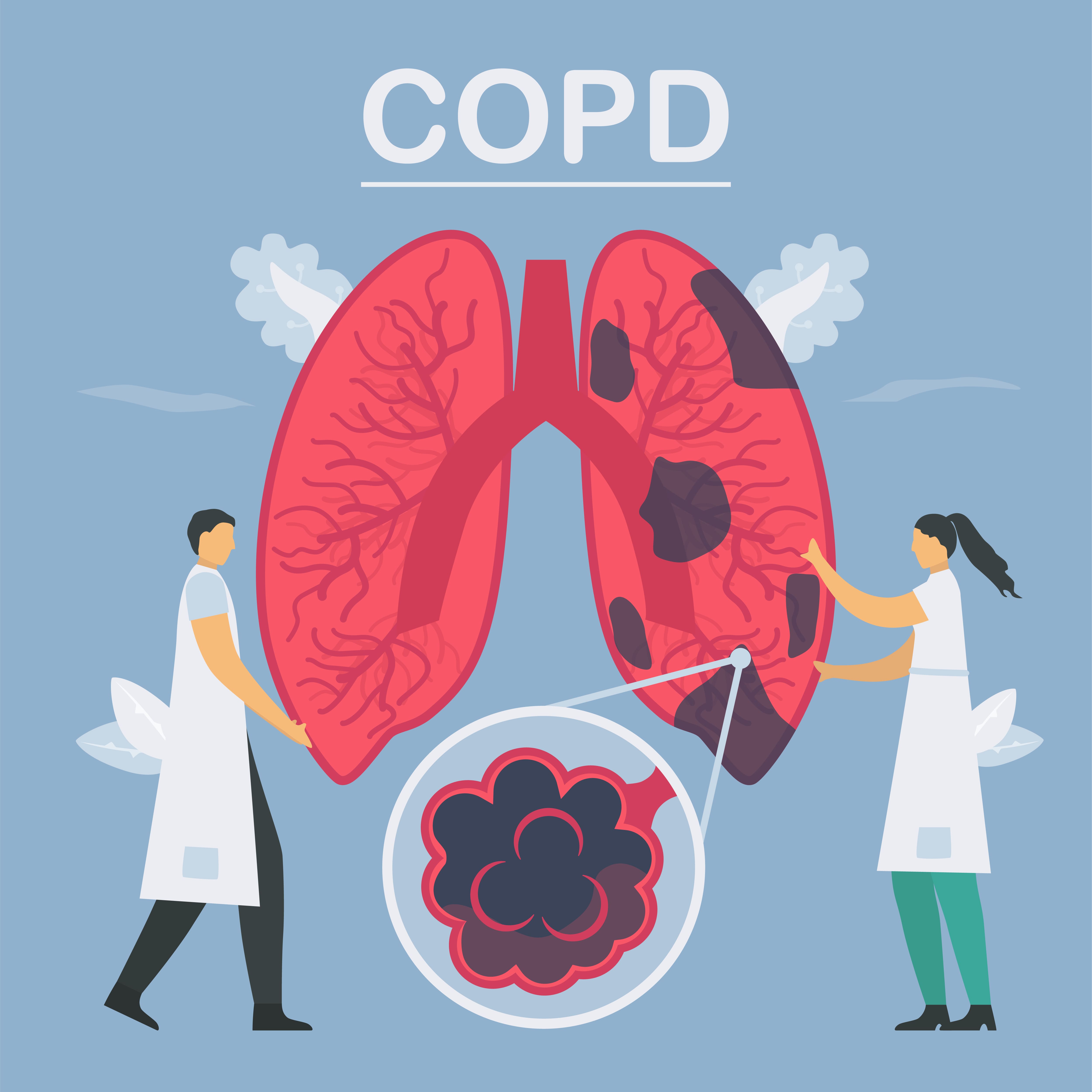
It’s also important to weigh the risks of different types of salt therapy. For example, salt therapy caves or chambers are designed to have a very high saline concentration, so it’s more likely this type of therapy could exacerbate your symptoms. Conversely, simply having a salt lamp around your home is unlikely to result in a high concentration of salt in the air, so you can assume that they’re safe to use. Just don’t expect there to be any significant benefits for managing your disease.
What Should COPD Patients be Doing Instead of Salt Therapy?
While it may be tempting to join in on a fad like salt therapy, the best way to treat your COPD symptoms is with traditional methods that have been researched for hundreds of years and backed by thousands of different studies. Let’s take a look at each of these treatment options.
An Improved Diet
Your lungs play an extremely important role in a process called cellular respiration. This is a set of metabolic reactions in the cells of your body that convert chemical energy into adenosine triphosphate (ATP). In other words, the oxygen that your lungs take in is directly linked to the breakdown of nutrients in your body and it’s absolutely necessary for your body to produce energy that it can use. One of the most important things to note as a COPD patient is that certain foods create more waste products (carbon dioxide) than others do which can make breathing even more difficult.
![]()
Pulmonary Rehabilitation
Regular exercise is one of the most important things you can do for your health. Whether you’re young, old, sick, or healthy, exercising improves blood flow, heart strength, and reduces your risk of life-threatening conditions like heart disease and diabetes. Pulmonary rehabilitation is a type of exercise that’s specifically designed for people with COPD and other chronic respiratory diseases because it’s focused on strengthening the lungs, reducing breathlessness, managing weight, and preventing exacerbations. Learn more about how pulmonary rehab works in this post.

Supplemental Oxygen Therapy
Another standard treatment for chronic obstructive pulmonary disease is supplemental oxygen therapy. Since COPD patients have less efficient lungs than the general population, oxygen therapy is designed to supply them with a higher concentration of oxygen. In turn, this will alleviate difficulty breathing, ensure blood oxygen levels remain stable and help to prevent exacerbations and other complications. Many people are intimidated by oxygen therapy because they believe it will prevent them from getting around and living life on their own terms.

Fortunately, this is not necessarily the case. While older outdated oxygen devices like oxygen tanks and liquid oxygen tanks can be bulky and difficult to maneuver, they’ve since been replaced by lightweight portable oxygen concentrators. Unlike oxygen tanks, concentrators are battery-powered machines that never need to be refilled by an oxygen company. They’re also fully approved by the Federal Aviation Administration (FAA), so you’ll never have to worry about being restricted in where you can travel. For more information on portable oxygen concentrators, be sure to reach out to our respiratory specialists here at LPT Medical.
Smoking Cessation
Smoking cessation can be one of the greatest challenges for many COPD patients. Some people have smoked for decades, so being faced with a COPD diagnosis and the task of quitting immediately, it can be somewhat overwhelming. However, it’s also the single most important thing you can do to alleviate your symptoms and ensure the best long-term prognosis of your disease. Several months ago, we wrote a three-part guide on smoking cessation and recovery so be sure to check it out if you’re interested.

Inhaled Therapy
It’s important not to confuse “oxygen therapy” and “inhaled therapy.” Oxygen therapy is meant to increase blood oxygen levels whereas inhaled therapy is meant to administer COPD medication via a mist called “aerosol.” By inhaling medication rather than taking it orally, you’ll experience greater benefits and you’ll experience the effects almost immediately. Inhaled therapy is usually administered through either an inhaler or a nebulizer device.

Conclusion
While salt therapy (halotherapy) is a trendy topic these days, that doesn’t necessarily mean it’s an effective treatment option for COPD. Although salt therapy has been around for hundreds of years, it’s surprisingly understudied and there is very little empirical evidence to go off of. With that being said, salt therapy has been found to be rather safe as long as you’re not exposed to it in high quantities.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Regardless of what you’re trying to change with your COPD treatment plan, you should always consult your doctor first. He/she may want to take a look at your medical history before determining if it’s safe for you to use salt therapy, or may completely advise against it if there’s a chance it could make your symptoms even worse. You should also take time to plan your day ensuring that you’re focusing on things that you know will improve your symptoms.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













