The clear and simple answer is that there is currently no cure for Chronic Obstructive Pulmonary Disease (COPD). That being said, there is evidence that shows early diagnosis, combined with disease management programs, can reduce the impact of COPD and slow the disease from progressing into a more severe state.
If you are struggling with accomplishing activities you used to do with ease by becoming short of breath, experiencing chest tightness or low energy, or getting frequent respiratory infections, being diagnosed with COPD can be a blessing in disguise.
In the United States 12.7 million adults are estimated to have COPD, but close to 30 million are living with impaired lung function, suggesting that many more people have COPD but aren’t being diagnosed.
This means that about half of the people with COPD are missing out on valuable treatments that will slow the progression of their disease and improve their over-all quality of life.
This is why it is so important to check with your doctor and get tested if you are experiencing:
- A nagging cough
- Decreased ability to exercise
- Shortness of breath
- Frequent respiratory infections
New research displays that many doctors may miss the early signs of COPD in up to 85 percent of cases.
That being said, there are multiple ways to be tested for COPD, and you might suggest to your doctor that you would like to be tested for COPD just to be sure that you do, or do not have it.
A spirometry test will test your Lung function and measure the amount of air you can inhale and exhale, and will determine whether your lungs deliver enough oxygen to your blood.
A chest X-ray can show whether or not you have emphysema, which is one of the main causes of COPD. An X-ray can also rule out other lung problems or heart failure.
A CT scan of your lungs can help detect emphysema and lung cancer. It is the test administrated to determine if you would benefit from surgery for COPD.
An arterial blood gas analysis measures how well your lungs bring oxygen into your blood and remove carbon dioxide.
Basic steps toward slowing disease progression
After getting one or multiple tests, and once you realize why you are experiencing symptoms, there are multiple ways to improve your quality of life, slow disease progression, reduce mortality and keep you out of hospital.
There are many people just like you, who have been diagnosed with COPD who found that after they knew the reason behind their breathing complications they were able to adjust their lifestyles, and actually changed their lives in a positive way!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In order to change your COPD diagnosis from a "death sentence" into a blessing to start anew, here are the basic steps you must take in order to slow the progression of your COPD.
One of the most important aspects and the easiest habit it form, is staying healthy in aspects of your life like diet, and weight. You can begin to research the correct food that you need to supplement you breathing issues and lung deterioration. You would be surprised how a healthy gut can influence your mood and your energy levels!
Make sure that all of you vaccinations are up-to-date and that you always get the fly vaccine every year in order to to protect yourself from influenza and pneumonia. These sickness can induce flare-ups, meaning more sever symptoms and extreme trouble breathing, which will inevitably lead to more hospitalization in the future.
It is also important that you understand and are always learning about COPD education. You should know all of the steps you must take in the case of an emergency, you should know how and when to take you medication, and you should know your treatment plan through and through.
Most important steps towards slowing COPD progression
The following steps are more challenging and require more planning and effort, however this section about slowing your COPD disease progression is the most vital.
Quitting smoking is the utmost important action you must take to reduce the rate at which your lungs are deteriorating. If you have COPD and continue to smoke year will be taken off of your life expectancy. However, if you are a life-long smoker, and quit smoking after being diagnosed with COPD, the rate at which your COPD progresses into more severe stages will decline.
For some folks, exercise has never been a high priority. But if you have COPD, it is crucial for your health and longevity, that you start taking steps towards a more active lifestyle.
This does not mean you should start training for a marathon, instead try walking around your house more often, then try climbing the stairs multiple times a day, and before you know it your tolerance for exercising more regularly will begin to grow.
You will be able to walk or hike and get outside (if it is not allergy season), you can begin pulmonary rehabilitation classes, and adding breathing exercise into your daily routine.
This last step is critical for people who need extra oxygen, and need to begin on supplemental oxygen therapy. so that you can breathe easier and you can stay more active. Even if you don’t need oxygen therapy now, you may need it later if your COPD does progress into a more severe stage.
There are a few options you have when it comes to choosing the method in which you receive supplemental oxygen. The overwhelming consensuses is that portable oxygen concentrators (POC) are the most innovative and hassle-free pieces of equipment for oxygen therapy available.
POCs are lightweight ranging from 4-8 pounds depending on the model. They are battery powered, and depending on the flow setting and battery module capacity can last up to 16 hours.
POC are also safe, and do not create an oxygen rich environment like an oxygen tank does, this means you can safely travel by plane, car, boat with ease. The POC brings in surrounding air, purifies and concentrates the air into medical grade oxygen.
COPD is very serious chronic illness and should not be taken lightly
COPD is a very serious respiratory disease, and because it cannot be cured yet, it is crucial to take all of the suggestions within this article and apply it to your lifestyle everyday if you can.
If you are diagnosis with any stage of COPD, you need to set up a strict treatment plan where so that you are able to successfully slow down the disease progression, and minimize lung deterioration.
By following all of theses disease management tesuniqes, you will be able to continue living a rather normal if not more active lifestyle than before your diagnosis.
If you struggle with physical activity, one of the best ways to help you get into the habit of exercising is with the help of a portable oxygen concentrators. An Inogen brand portable oxygen concentrator, Caire Freestyle Comfort portable oxygen concentrator, or the Respironics SimplyGo Portable Oxygen Concentrator will help you to exercise with less shortness of breath, travel freely and independently, and never have to worry about up-keeping costs associated with refilling any oxygen canisters.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you are not at the stage where you need supplemental oxygen therapy, be sure to take all of these steps to avoid progressing to that stage of COPD later in life.
.png)
In this fast-paced, busy world that we live in, it can be difficult to find the time or the means to practice mindfulness. From going to work to cooking dinner, dealing with family matters, and spending time with friends, we often don’t take the time to decompress and ensure that our thoughts and feelings are in line with what we’re trying to accomplish.
What’s more, if you have a chronic illness like COPD, the problem of having an overburdened mind is often compounded by physical symptoms like breathlessness, chest pain, and fatigue. Many COPD patients describe feeling “claustrophobic” or “confined” within their own body, leaving them little recourse but to focus on the negatives of their disease rather than the positives.
Ultimately, this mindset is not sustainable, so you’ll need to find some way to set your mind at ease. For many people, meditation is the best way to do this. Meditation is the use of various different techniques designed to train your mind to focus on a particular activity or thought. What results is that you’ll have more control over your mindset pertaining to your disease and its progression.
In this post, we’ll discuss a variety of different types of meditation and we’ll give you some tips for implementing them into your life as a COPD patient. If you’re looking for further reading, check out our post about 6 Effective Breathing Techniques and Exercises for COPD and Techniques for Coping with COPD and Anxiety.
What is Meditation?
Many people live their whole lives without trying or even considering the use of meditation. It’s often written off as a religious or spiritual practice that’s not useful for most people. And while this is partially true — meditation is used in many religious traditions such as Buddhism — it’s actually more commonly used in a non-religious context.
According to Positive Psychology, meditation is a practice that’s been around for thousands of years, but it was first depicted by wall art paintings in India around 5000 to 3500 BCE. Meditation moved to the west as early as the 1700s, but it wasn’t until the 1900s that it began to be separated from its religious roots.

Today, the beneficial effects of meditation are well-studied and well-documented. The practice has been examined extensively by prestigious institutions and has yielded mostly positive results, especially when it comes to treating depression and anxiety. What’s more, other studies have shown a positive correlation between meditation and easing the pain caused by a chronic illness such as COPD.
How Does Meditation Affect the Brain?
In this day and age, we have an incredible amount of technology that can be used to examine what goes on in the brain. Technology such as polysomnography has enabled researchers to study what goes on in the brain during sleep and has made it easier for doctors to diagnose conditions like obstructive sleep apnea (OSA) and insomnia.
Similar technology has been used to study the brain during physical activity and even meditation. Magnetic resonance imaging (MRI) is one such device that’s used to produce pictures of the anatomy and the physiological processes of the body. It allows researchers to precisely monitor changes in brain wave activity during different activities.
Brain waves are the electrical impulses which oscillate at different frequencies and at different wavelengths. Brain waves are altered depending on the state of consciousness that we’re currently experiencing. For example, if someone is wide awake, they will have different brain wave activity than someone who is in light sleep or deep sleep.
Researchers have found that people who are anxious or tense they often have more high-frequency beta waves present. This includes people with mental disabilities such as ADD, ADHD, or learning disabilities, but it can also include people with chronic conditions like COPD who might experience a higher degree of anxiety than the general public.

In many cases, trying to force these feelings out can exacerbate them, leading to a negative feedback loop. However, if you learn to influence brain waves through meditation and neurofeedback training, you can reduce feelings of anxiety. As we come to better understand brain waves and how to influence them, we will likely see more doctors prescribing it as an alternative to anxiety medication which always has some negative side-effects.
Can Meditation Alter the Course of COPD?
Now that you know meditation can be used to treat anxiety and depression caused by COPD, you’re likely wondering whether meditation can help alter the long-term prognosis of your disease. In other words, are there any physical manifestations of the benefits that we see from people who meditate regularly?
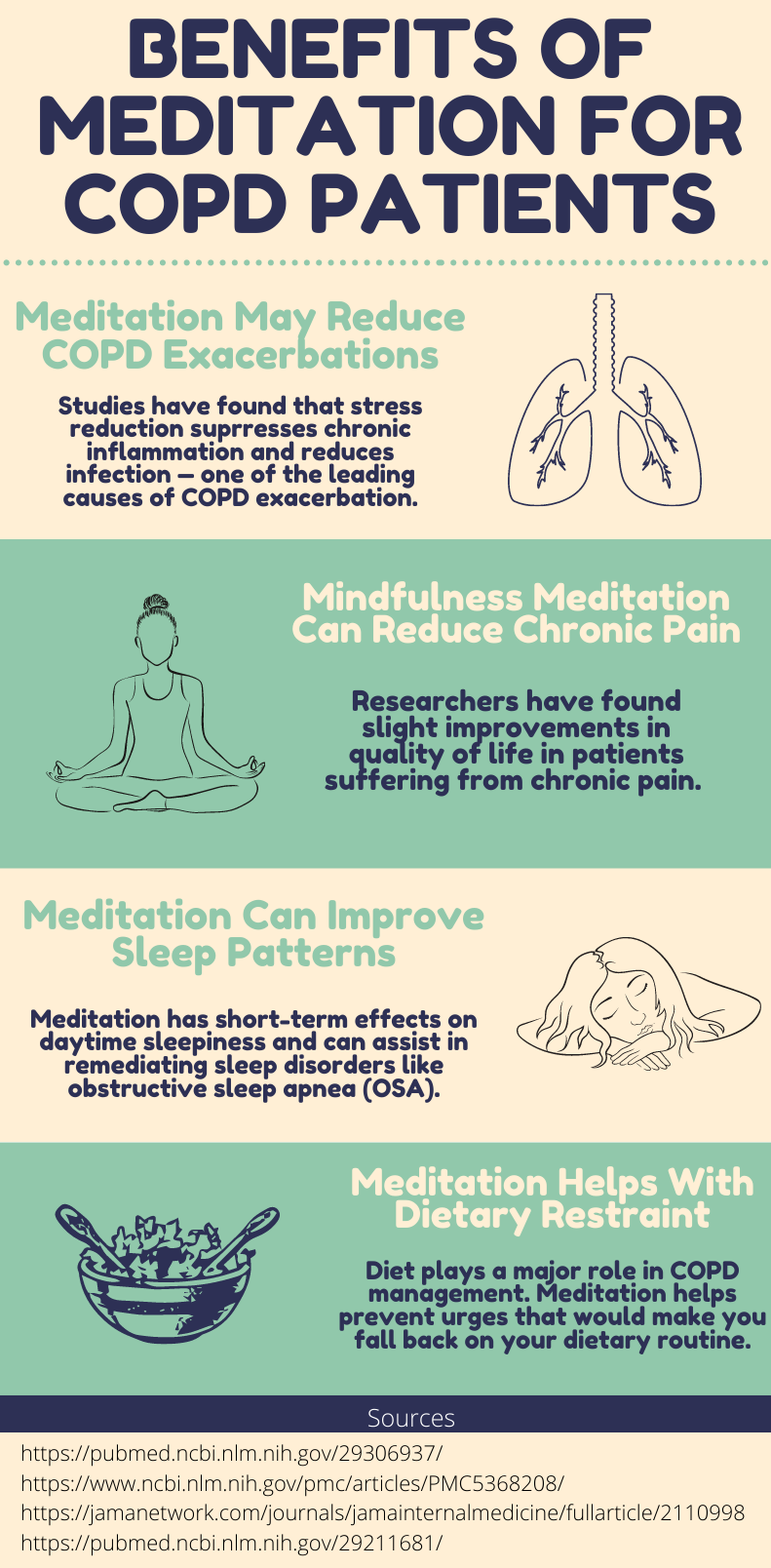
Unfortunately, it’s a little more complicated than a simple “yes” or “no” answer. Generally, meditation is accepted as an effective method for treating not only comorbid anxiety from COPD but physical respiratory symptoms as well. This study found that after 12 weeks of yoga training, many COPD patients saw improved lung function, inflammation, and quality of life.
.jpg)
Other studies, however, have cast more doubt on the effectiveness of meditation for COPD patients. This study found that meditation presenting emotionally-triggering skills such as mindful awareness to emotions or dyspnea can actually contribute to anxiety. However, both of these studies were limited by a small sample size.
Possibly one of the most popular forms of meditation for COPD patients is something called “movement meditation.” This practice focuses on being mindful of your body’s movements rather than focusing on the goal of the movement. According to a study found in COPD News Today, COPD patients practicing Tai Chi (a type of movement meditation) five hours per week saw more benefits after 12 weeks than those practicing standard pulmonary rehabilitation.

While there is limited evidence suggesting that meditation directly improves outcomes for COPD patients, there are plenty of ways that it improves outcomes indirectly. Anxiety is a well-known contributor to the frequency and severity of COPD exacerbations and anxiety can cause sleep disruptions which can lead to fatigue and other factors that make COPD more difficult to cope with. Therefore, treating anxiety with meditation has undeniable benefits when it comes to COPD outcomes.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What Types of Meditation Are There?
Focused Meditation
Focused meditation is a practice where you concentrate intently on one object, sound, tactile sensation, smell, or taste. This is often used as a sort of stepping stone to classical meditation which requires you to block all thoughts.
.jpg)
Focused meditation is a great place to start because it doesn’t require you to have an instructor and it’s very accessible for most people. By having a focal point of thought, you’ll be able to more easily control your internal dialog and catch yourself whenever your mind starts drifting. Another great thing about focused mediation is that you can start with shorter sessions. Just five minutes a day of focused meditation will get you started on the right foot.
Movement Meditation
Like the name suggests, movement meditation is a type of meditation you do while you’re physically moving. It’s the perfect exercise for anyone who wants to experience a greater connection between their mind and body, as well as people who have difficulty concentration their thoughts while they are sitting still.

Movement meditation is one of the most popular types of meditation for people with COPD and other respiratory conditions because it helps them eliminate anxiety while mastering their breathing and motor functions. Movement meditation is also a great exercise to complement pulmonary rehabilitation routines because it can build endurance and muscle.
Tai Chi is one of the most practiced forms of movement meditation in the world and it’s especially popular among older adults and seniors who suffer from chronic illness. It originated in ancient China where it was originally intended as a form of fighting. However, over time, Tai Chi was adopted and developed by many different cultures, making it what it is today.
We’ve already written in great detail about Tai Chi and its many benefits for COPD patients, however, we’ll summarize it here for your convenience. Essentially, Tai Chi is a form of low-impact exercise that combines a variety of different poses with fluid and controlled movements. In other words, you won’t be moving your legs and arms around erratically without purpose; you’ll instead be focusing on making every movement meaningful.

Creating this mind-body connection is very important for people with COPD because as your disease progresses, it becomes increasingly difficult to control things like your breathing which are unconscious motor movements in people with healthy lungs. As such, it’s recommended that COPD patients learn Tai Chi as soon as they’re diagnosed because it will take some time to learn how this form of movement mediation works, and its benefits will increase exponentially as time goes on.
Tai Chi also has several undeniable benefits when it comes to mindfulness. One of the reasons anxiety and depression are so common among COPD patients is that they feel a loss of control. Chest pain, fatigue, breathlessness, and exacerbations caused by COPD cannot always be predicted, so Tai Chi affords these people the ability to be in full control of something. Many people swear by this, saying that it has renewed a sense of control and purpose in their life.
There are three different ways to practice Tai Chi: as an individual, in a group setting, or with an instructor. Currently, due to COVID-19, it’s recommended that you practice Tai Chi on your own, however, if you can find a group that takes social distancing measures seriously, this could be an option too. If you’re doing it on your own, this guide will be helpful in getting you started on the right foot.

Yoga can also be considered a type of movement meditation, however, whereas Tai Chi is more focused on the act of moving, yoga is more focused on the various positions. Another difference between the two is that Tai Chi is usually performed in a standing position while yoga is done on the ground. Since yoga requires a lot of strength and agility, it’s not always recommended for people who are physically impaired.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Mantra Meditation
A “mantra” is a word, syllable, or phrase that’s repeated during meditation. This is very similar to focused meditation in that you’re concentrating on one specific thing, however, mantra mediation differs because there is usually a purpose or a meaning behind the sound that’s being produced. Mantras can also be repeated by the mediator whereas the sounds produced in focused meditation are usually external.
.jpg)
The idea behind mantra meditation is that every sound is a tool for transforming consciousness. So, instead of simply training your mind to concentrate, you’re also altering your state of mind rather than just your thoughts. The type of sound that you produce, its frequency, and volume will all be determined by what state of mind you’re trying to produce. One of the most popular types of mantra meditation is called transcendental meditation.
Mindfulness Meditation
Mindfulness meditation is directed at helping you be more present in the current moment. In other words, whereas focused meditation and mantra meditation are aimed at focusing on one specific sensation, mindfulness mediation is designed to help you better understand the urges and feelings you are currently experiencing.
Another core component of mindfulness meditation is understanding your breathing. Unlike with breathing techniques, there is no special way that you have to breathe. As the name “mindfulness” suggests, you should be focusing on how your breathing is in the current moment, not how you want it to be.
Benefits of Meditation for COPD Patients
Conclusion
Mindfulness is something that many people struggle with. It’s easy to forget that an overworked mind that’s crowded with thoughts can not make decisions effectively. And living with this burden for months or years on end can be exhausting to say the very least.
There are many different types of meditation, but they’re all aimed at helping you control your thoughts and motor functions, and giving you the skills you need to live in the moment rather than being distracted by thoughts of the past or future.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
As a COPD patient, there is no understating the importance of effective meditation. If you become overwhelmed by negative thoughts about your disease, you may want to take a step back and start incorporating meditation techniques into your daily routine.
While meditation is by no means a replacement for your COPD treatment plan, certain types of meditation like Tai Chi and yoga can be used in tandem with your pulmonary rehabilitation plan and breathing techniques. But as always, be sure to check in with your pulmonologist to learn the best way to do this.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!









