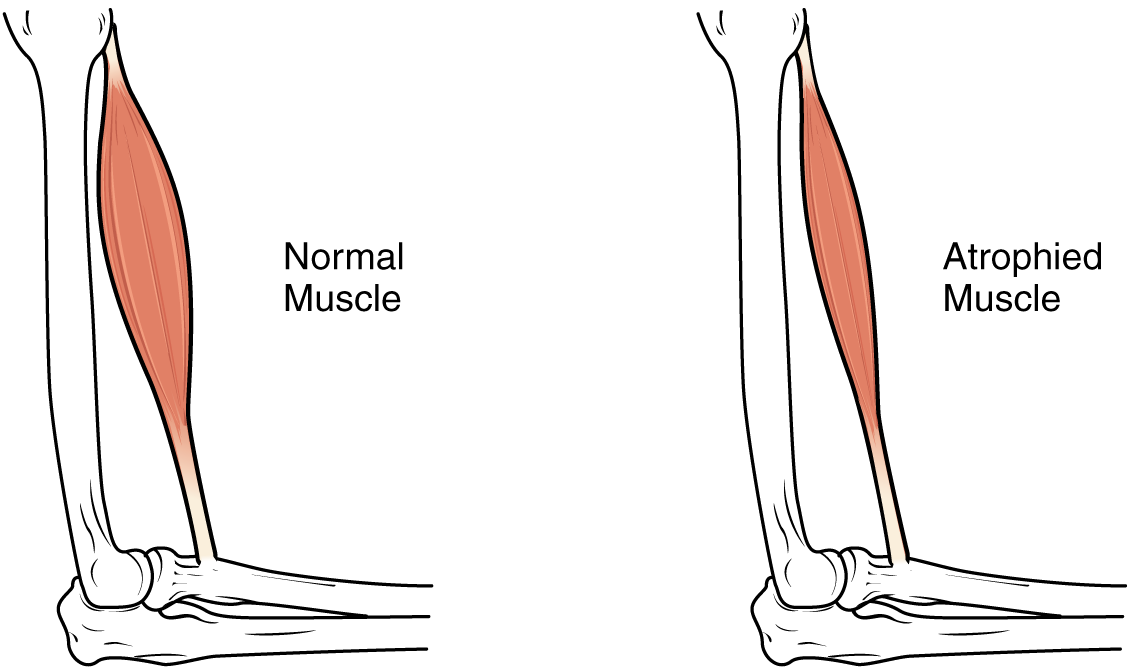
Maintaining a healthy amount muscle mass is a constant struggle for many COPD patients, especially those in the later stages of the disease. COPD not only causes weight loss and loss of muscle mass, but it makes it more difficult to build muscle as well.
This is due in part to the nature of the disease, and partially due to COPD symptoms that make it difficult to exercise and build strength. Many people with COPD also get caught in negative habits, like avoiding exercise and meals, or suffer from psychological conditions like anxiety or depression.
All of these things lead to weight loss and muscle wasting, and eventually an overall physical decline. It's not something to take lightly; COPD patients with very low body weight and muscle mass tend to have highest mortality rates and are prone to a variety of complications.
But even though COPD makes it more difficult to build and maintain muscle, it is definitely possible to do. All you need is the right diet, eating habits, and exercise routine to keep your body strong and maintain a healthy BMI.
In this article we're going to tell you everything you need to know about building muscle mass and COPD. We'll explain how the disease affects your muscles, how muscle mass affects your health, and show you a variety of different techniques you can use to better gain muscle and prevent weight loss with COPD.
What Causes Weight and Muscle Loss in People with COPD?

As many as forty to seventy percent of people with COPD experience weight loss and muscle wasting, especially in the later stages of the disease.
There are a variety of reasons why this happens, but lack of exercise and eating too little are the main causes. People who suffer from COPD also have difficulty maintaining their muscle mass because of inflammation and the fact that their damaged lungs need extra calories and nutrients.
Here's a more detailed look at the four main causes of muscle wasting and weight loss in people with COPD:
Too Little Exercise

Most people with COPD have at least some difficulty exercising as a result of respiratory symptoms like shortness of breath. This causes many people with the disease to neglect their exercise needs, which makes the problem even worse.
It's extremely important to get enough physical activity as early on as possible if you have COPD. Those who get diagnosed at early stages of the disease are at an advantage for this reason.
If you stay sedentary for too long, your muscles will get weaker, your respiratory symptoms will worsen, and it will become more and more difficult to tolerate exercise and even mild physical activity. That's why easier to prevent muscle loss than it is to gain it back once it's already gone.
If you have COPD, sticking with you doctor-prescribed exercise routine and being active is the only way to prevent physical decline. There are only two choices when it comes to your muscles: use them or lose them.
Too Little Food
Many people with COPD experience worsened symptoms when they eat. Some patients feel breathless from the energy and act of eating alone, but eating can also cause the stomach to swell and put pressure on the lungs, causing discomfort and shortness of breath.
Because of this, many patients avoid eating or are not able to finish their food at mealtimes. This leads to weight loss and malnutrition, which then causes muscle weakness and wasting. Malnutrition also suppresses your immune system, which significantly increases your chances for infections, exacerbations, and hospitalization.
That's why proper diet and calorie-rich foods are so important for people who have COPD. If you don't eat enough calories and nutrients to sustain your body's needs you will have less energy, you will lose weight, and your body will begin breaking down its own muscles out of necessity.
Depression

It takes a lot of energy and mental strength to cope with getting diagnosed with COPD. It's normal to feel a great deal of anxiety, especially at first, but for some people it can lead to serious depression.
Depression makes it easy to give up on the habits and activities that keep you healthy. It can make you feel too exhausted and anxious to get out of bed, let alone keep up with your prescribed exercise, diet, and treatment regimens.
Because of this, many people with COPD who get depressed let themselves become sedentary and malnourished. This leads to a loss of muscle mass as well as weight loss that can lead to even worse depression and COPD symptoms.
Mental health and physical health are closely intertwined, which is why it's very important to seek help if you are struggling. Look out for the symptoms of depression in yourself and loved ones with COPD, and don't hesitate to talk to a mental health professional if you're having trouble coping on your own.
Untreated anxiety and depression can lead to a variety of health problems and it's no way to live your life. It's possible to find hope and happiness in the midst of managing a chronic illness, and your doctor or psychiatrist can help you take the first steps toward feeling better.
Inflammation

Studies show that people with COPD produce more inflammatory compounds than healthy individuals and show signs of inflammation all throughout their bodies. Researchers have found that this chronic inflammation could be part of the reason that COPD patients are especially prone to muscle wasting.
Inflammatory molecules inhibit the body's ability to generate muscle mass, which makes it difficult to build strength and reverse muscle loss. Instead of putting its energy toward rebuilding and maintaining your muscles, your body has to focus its most of its energy on repairing the tissue damage caused by inflammation.
Chronic inflammation also saps your energy and makes you feel fatigued, which makes it even more difficult to exercise and maintain your muscle mass. This makes people with COPD even more prone to muscle loss, weight loss, and adopting a sedentary lifestyle.
Increased Calorie Requirements
Many people with the disease don't realize that COPD makes you burn more calories than healthy adults. Lungs damaged by COPD have to use up to ten times the amount of energy to breathe, which means you have to eat more food to make up for it.
The more your lung function declines, the more energy it takes to breathe, which means that your calorie needs will likely increase as your disease progresses. If you don't eat extra food to make up for the extra calories you burn, you're bound to lose weight and possibly even muscle as your body breaks down its muscle and fat reserves to get the energy it needs.
Since eating can already difficult and exhausting when you have COPD, many patients are unwilling or unable to get the extra calories and nutrients they need from their meals. That's why many doctors recommend calorie-dense foods like milk and nuts; it allows you to get more sustenance from a smaller amount of food, so it's easier to eat enough to meet your body's needs.
The Dangers of Weight Loss & Muscle Loss for People with COPD
Both a certain amount of muscle and a certain amount of fat are necessary to stay healthy and strong, especially if you have COPD. Additionally, both weight and muscle mass are closely related; weight loss usually leads to muscle wasting and muscle wasting can also lead to weight loss.
If you have COPD, it's not just important, but vital to stay at a healthy weight and keep up your muscle mass as much as possible. It's considered to be a very bad sign if you start losing weight or muscle mass quickly, and reversing the loss is the only way to preserve your lung function and health.
Research shows that COPD patients with a BMI under 20 have less energy, worse symptoms, and quicker respiratory decline. A low BMI also puts you at risk for infections, exacerbations, hospitalizations, and other serious complications.

Another consequence of being underweight is malnutrition, which can be devastating for someone with COPD. Being underweight and undernourished depresses your immune system, causes muscle wasting, and leaves you without enough energy to exercise or do normal daily activities.
This starts a downward spiral that leads to even more muscle loss, more difficulty exercising, and worse COPD symptoms. Because of this, low body weight and muscle mass (if not treated and reversed) are considered reliable predictors of a quicker overall decline in physical health.
Rapid, severe weight loss is a sign of a very serious problem, and you should never ignore it. If you have COPD and experience significant unexplained weight loss, you should schedule an appointment with your doctor without delay.
How to Gain Weight and Build Muscle Mass with COPD
Since weight loss and muscle wasting is such a common and serious problem for people with COPD, researchers have spent a lot of time studying how to prevent it. Luckily, scientists have so far found a variety of methods to reduce muscle wasting and help COPD patients build muscle mass more effectively.
The Importance of Strength Training

Many people with COPD have difficulty exercising, and for a long time researchers believed that breathing difficulties were the main cause. However, it turns out that lack of muscle strength, not just shortness of breath, is the culprit behind many COPD patients' lacking tolerance for exercise.
Because of this, researchers believe that strength training is one of the most important things you can do to improve your health when you have COPD. It not only prevents muscle wasting, but also can improve your exercise endurance, emotional health, and overall quality of life.

In fact, studies comparing COPD patients who followed an exercise plan focused on aerobic activity with patients who followed a strength training regimen show that strength training often leads to better outcomes. Patients who undergo strength training tend to see the biggest improvements in their muscle mass and exercise tolerance.
What is perhaps most telling, however, is the fact that COPD patients who do strength exercises report the largest improvements to their quality of life. This is likely because strength training helps patients feel stronger, gain mobility, and do more daily activities without feeling tired and fatigued.
Strength training is like a positive feedback loop that leads to better strength, better mood, and better health. It goes like this:
-
The more muscle you build, the more exercise you will be able to handle. The more exercise you can handle, the more muscle you can build.
-
The more muscle you build, the better you can manage your COPD symptoms. The better you can manage your COPD symptoms, the more you can exercise.
-
The more you exercise, the less depressed and anxious you will feel. When you feel less depressed and anxious, it makes it easier to exercise and eat a healthy diet.
-
When you eat a healthy diet, your body is better nourished. When you're better nourished, you'll have more energy, which allows you to build even more strength.
- The stronger you are and the better you can manage your symptoms, the more mobile and active you can be in your daily life. This leads to even more physical activity, more strength, and a better quality of life overall.
Strength Training Exercises for COPD

Resistance exercises like push-ups, squats, and weight lifting are the most effective ways to build body strength and muscle mass. Many people enjoy strength training using weights and other equipment you can find at the gym, but you can also do effective strength training exercises with minimal equipment at home.
You can buy a small set of light free weights for lifting at home and choose exercises that use your own body weight as resistance to build strength. If you have severe COPD symptoms or limited energy, there are a variety of chair exercises you can do that are designed specifically for people with limited strength and mobility.
Most doctors recommend doing strength training sessions at least three days a week in order to see an improvement in strength and muscle mass. You should start slow, doing only as much as you can handle without feeling too breathless or fatigued.
You can add in extra muscle groups and repetitions as time goes on and your strength and endurance increases. Just make sure you talk to your doctor before starting any new exercise routine, and don't be afraid to ask for advice, either.
Here are some examples of resistance exercises you can do to build strength and muscle mass:
- Leg lifts
- Bicep curls
- Squats
- Knee raises
- Chair exercises
If you are having difficulty exercising on your own, consider joining a pulmonary rehabilitation class. It's like a special exercise and education course for people with respiratory diseases, and doctors recommend it to anyone who has COPD and struggles to keep up with their exercise plan.
At pulmonary rehabilitation you can learn how to better control your symptoms when you exercise, use your medications effectively, and even get opportunities to learn and practice new exercises. They often also include dietary education, mental health support, and group therapy sessions to allow patients to share their worries, struggles, and successes.
Use Supplemental Oxygen

Shortness of breath is one of the major barriers that prevents many people with COPD from exercising and eating as much as they should. Luckily, many patients find it much easier to do both of these things when they use supplemental oxygen at the same time.
Using supplemental oxygen at mealtimes can reduce breathlessness and fatigue while you eat, making it easier to get the calories and nutrients you need to stay healthy. When you exercise, supplemental oxygen can help you keep your respiratory symptoms under control so you can have better endurance and build more muscle.
If you regularly struggle to breathe when you exercise or when you eat, talk to your doctor about using supplemental oxygen during these activities. Your doctor will assess your lung function to determine your oxygen needs and help you learn how to manage your oxygen flow and concentration when you do different activities.
Talk to Your Doctor about Supplements

When it comes to building muscle and maintaining a healthy weight, many COPD patients need some extra help. Studies show that supplementing your diet with certain nutrients like protein or creatine can prevent muscle wasting in people with COPD and help them gain weight and muscle mass more quickly.
Some doctors recommend protein shakes or other nutrient-rich shakes to people with COPD who have trouble getting enough calories from their meals. Shakes are quick and convenient to prepare, and take very little energy to drink compared to solid foods.
It is important to always get your doctor's approval before taking new supplements, using nutrient shakes, or significantly changing your diet in any way. Your doctor can ensure that what you're taking is healthy and won't interfere with any of your other treatments or medications.
Supplements known to improve muscle and weight gain in patients with COPD:
- Creatine
- Protein shakes
- High-calorie nutrient shakes
Eat More Meals

When you eat a lot of food all at once, it can cause your stomach to expand and press on your lungs. For people with COPD (and especially emphysema), this is a common problem that can cause extreme discomfort and make it difficult to breathe during and after meals.
These symptoms can make it difficult to finish meals or cause people with COPD to dread or avoid eating food. That's why doctors recommend patients who struggle with breathlessness at mealtime to change their eating schedule to include more meals and smaller portions.
Instead of three large meals a day (breakfast, lunch, and dinner), many doctors recommend that people with COPD eat six smaller meals spaced out throughout the day. Doing this cuts the size of each meal in half and gives your stomach time to digest and empty in-between meals.
This way, you can eat smaller portions that won't cause discomfort but still get enough food to prevent weight and muscle loss. It's a great solution if you struggle with breathlessness because it allows you to get all the calories and nutrients you need with a much lower risk of triggering breathing difficulties at mealtimes.
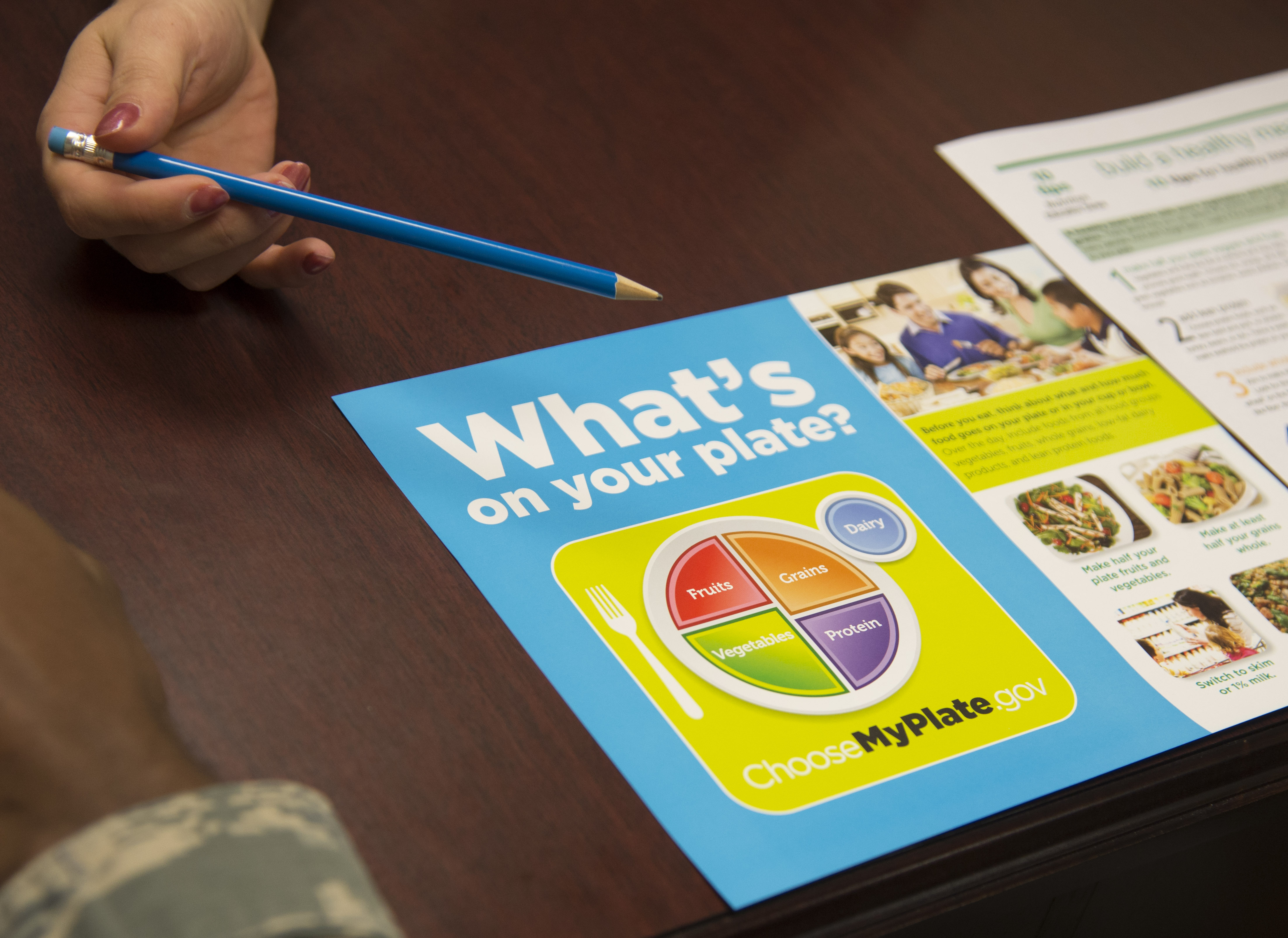
Prioritize Your Food

If you have trouble finishing meals because of breathlessness or other COPD symptoms, it can be helpful to prioritize the food on your plate. Eat the most calorie-dense and nutrient-dense foods first, that way you get the most out of your meal even if you can't finish it all.
If you often feel full or breathless before finishing a meal, it can also help to limit the amount of water and other liquids you drink. If you avoid drinking before or during meals, you'll have more room in your stomach for food. You can make up the fluids by drinking more water in-between meals, instead.
If you have trouble building up an appetite, try starting your meals with a treat or a food that you really enjoy. You will dread eating less if you have something to look forward to, and starting with a favorite food might whet your appetite and make it easier to continue eating.
Here are some examples of nutrient-dense foods to add to the beginning of your meals:
- Eggs (cooked in oil)
- Nuts and nut butters (e.g. peanut butter)
- Milk and cottage cheese
- Meats (chicken, fish)
Eat More Protein

Protein is necessary for your body's basic functions, and it's something your body absolutely cannot do without. If you don't get enough protein in your diet, your body will take it from the next-best source: your muscles.
This type of muscle wasting is a problem that happens often in COPD patients who are weak and malnourished. That's why it's so important to maintain a healthy diet when you have COPD.
When the food you eat isn't enough to meet your body's energy and nutrient requirements, your body will not hesitate cannibalize your own muscles for the nutrients it needs. The solution is to make sure that you are eating enough and have a balanced diet with protein-rich foods.
Most doctors recommend that you get most of your protein from lean meats and plant protein sources. Adding extra portions of chicken, fish, eggs and beans to your meals is a healthy way to add more lean protein into your diet.
On the other hand, you should avoid the less-healthy fatty meats and processed meats like bacon, sausage, and ham. Also, if you need to make room for more protein in your diet, it's best to eat fewer simple carbs like sugars, white breads, and white pastas.
Here are some examples of healthy proteins to add to your diet:
- Fish (salmon, cod, tuna, etc.)
- Chicken
- Lean beef
- Eggs
- Tofu
- Beans & Legumes
Consult a Dietitian
Sometimes, no matter how hard you try, you just can't manage a healthy diet on your own. COPD can make getting proper nutrition very difficult, especially because it causes you to need extra calories and nutrients.
If you have trouble gaining muscle or continue to lose weight despite your best efforts, it's time to talk to your doctor or a licensed dietitian. They can help you figure out exactly how many calories you need to eat and what amounts of different nutrients your bo
Changes are occurring within us, both physically and emotionally, our entire lives and yes, one day those changes become stressful and even hard to manage, we call it old age.
Vitality you once had as a young man or woman seems to be fading away, however, it is not gone. This does not go without saying that the aging process can be physically and mentally exhausting even painful, but there are measures you can take to manage the changes that are happening in your body and mind.
In this article, we will take an in-depth look at a few of the changes occurring in your bones, heart, and lungs as you age.
Once you understand some of these changes, you can begin implementing goals into your daily life to make the most out of the vitality in you.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Your aging bones, why are they thinning?
Age-related bone loss is a gradual decline in bone mineral density. This means that with increased age there can also be a reduction in bone formation, which can result in osteoporosis, bone thinning, and it is perfectly normal.
Bone thinning can occur in men and women, and it puts so many people at risk of breaking bones more easily. Of course, more broken bones means limited mobility and less independence which is something you can work to avoid.
By using the research below, you will have the tools to set goals to in the form of exercise and diet geared towards improving your bone health.
Pursuing one or all of these goals will help you to maintain your bone health and density as you age.
#1. Start doing these effective exercises for enhancing your bone density and bone health
As we grow older it becomes exceedingly harmful to associate older age with a decline in our physical activity, especially when healthy bone density depends on how much you work out your bones.
By exercising regularly, your bones adapt to the changes in force, and your body will generate more cells which strengthens bone density and your overall health.
There are specific types of exercises that will offer the most effective results for building and maintaining strong bones; weight bearing exercises and strength-training exercises.
- Weight Bearing exercises describe any activity you do on your feet that works your bones and muscles against gravity. Activities include:
- Brisk walking
- Climbing stairs
- Jumping up and down or jumping rope
- Hiking
- Jogging
- Step aerobics
- Tennis
-
Yard work
- Strength-training exercises involve resistance added to movement in order to make muscles work harder. This can involve:
- Using free weights
- Resistance bands
- Weight machines
-
Push ups
-
Flexibility exercises are to be performed when your muscles are warmed up so that your joints are able to move gently and slowly without pain. For a person at risk of osteoporosis, avoid bouncing, twisting, flexing your spine, and bending at the waist while stretching.
- Stability and balance exercises will help your muscles work in conjunction with your brain. This is very important to reduce the risk of falling. Try some of these exercises:
- Standing on one leg
- Closing your eyes and standing on one leg
- Tai chi
- Modified yoga poses
If you are eager to create an exercise training program specific for enhancing your bone density and strength, start by incorporating one of each of these types of exercises into your daily routine. By doing so, you can prevent or reverse almost 1% of bone loss per year.
Your program should be personalized to your body, and should avoid high-impact exercises, bending, and twisting. Also, it is always prudent to speak with your doctor or physical therapist to ensure the exercises you want to accomplish everyday are a good match for your body and bones.
#2. Incorporate calcium and vitamin D rich foods in your diet for stronger bones
Food and drinks can play a critical role in osteoporosis prevention, and by incorporating these foods into your daily diet can prevent further bone thinning.
Important nutrients for strong bones include: Calcium, vitamin D, magnesium, potassium, and vitamin K.
Here is a table with foods that are rich in bone heathy nutrients:
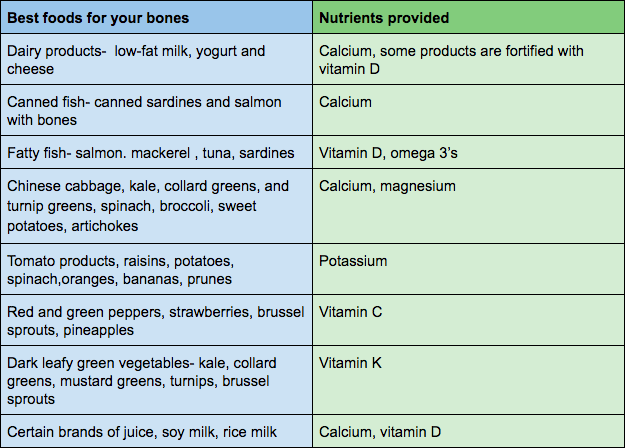
Changing your diet entirely can be intimidating. So try making it more simple by adding one food source from the table above into one meal a day.
From there try starting a meal plan, you can begin your research by searching the most cost effective ways to prep meals for your dollar and your body.
Time to take better care of your aging heart
The most common threat aging has on the heart is increased stiffness of the large arteries, called arteriosclerosis, and this will often lead to heart disease.
This happens when plaque builds up in the coronary arteries and reduces blood flow to your heart muscle, it can cause high blood pressure, or hypertension.
With all of the evidence and information surrounding the causes of heart disease, comes a plethora of preventative and manageable measures one can take everyday to relieve some symptoms and maintain your livelihood with heart disease.

#3 Start doing more physical activity for a healthier heart
Physical activity is one of the most important aspects of preventing and even reversing some risk factors associated with heart disease. Your heart is a muscle, and like any other muscle they must be utilized regularly or they will fatigue and weaken.
Cardiac based exercises aim to restore people with heart disease to health, and exercise has been found to reduce the likelihood of dying from heart disease.
So the question remains, how much exercise is right for you and your heart?
Of course this can be discussed with your doctor, but a basic 30 minutes a day five days a week is recommended by the American Heart Association.

Physical activity can be defined as any type of movement, if you’re moving, you’re likely burning calories. However being physically active when you struggle with heart disease can be daunting.
Take expert advice and start small by integrating some of these steps into your daily routine:
- Start slow:
-
do less reps (repetitions of movements), use light weights or no weights, go short distances, move at a slow pace
- Always begin you workouts by warming up your muscles and bones
-
take a short brisk walk around your house or neighborhood. Light jogging or biking are other options for more advanced exercisers
- Allow yourself to rest after aerobic exercise
-
Give your heart time to come down to a normal heart rate. Try stretching and deep breathing exercises in-between activities
- When it is hot outside, exercise in the morning or evening, or consider walking around the grocery store
-
Adding heat to a workout can rapidly increase your heart rate
- When it is cold outside, cover your nose and mouth when exercising, or consider walking around the grocery store
-
Breathing in cold air can cause discomfort in your lungs, making it harder to breath
#4 Maintain a heart healthy weight
It is very important to maintain a healthy weight when your heart is at risk of arteriosclerosis and heart disease, this means balancing the calories you eat and drink with the calories burned by being physically active.
If you are determined to maintain a healthy weight, ask your doctor or research the ideal weight for your gender, height, and age. Find out if you need to gain or lose weight or stay relatively the same.
Maintaining a consistent and healthy weight over a long period time of has extremely important health benefits that your heart will thank you for:
- Controlled blood sugar levels
-
controlled blood sugar levels are connected to reduced blood pressure and cholesterol levels and subsequently reduce the risk for heart attack, stroke and heart-related death
- Effectively burn fat
-
Burning fat reduces the level of unhealthy cholesterol in your blood.
- Regulated cholesterol levels
- With high cholesterol, you can develop fatty deposits in your blood vessels and it becomes difficult for blood to flow through your arteries
#5 Start a diet focused on heart health
Diet is critical when heart health is in question, and what you eat has a large impact on how your heart functions. Nutritionists recommend fiber as the most essential nutrient for a healthy heart.
Soluble fiber: Is found abundantly in oats, barley, beans, apples, citrus fruits and carrots. Soluble fiber is so imperative for a healthy heart because its properties bind to cholesterol and sugars preventing their absorption into your bloodstream. Bottom line, It helps reduce cholesterol.
Insoluble fiber: comes from whole grains like whole wheat flour, wheat bran, nuts, beans and vegetables, such as cauliflower, green beans and potatoes.

Beyond fiber, you can follow this list below to incorporate other heart healthy nutrients in your diet like omega 3 fatty acids, monounsaturated fats, folate, quercetin, lycopene, magnesium, plant sterols and stanols.
-
Leafy green vegetables supply a wealthy dose of vitamin k and will help protect your arteries and prompt proper blood clotting.
-
Dark green vegetables are packed with nitrates that can reduce blood pressure and relieve arterial stiffness.
-
Whole grains such as oatmeal, whole wheat bread, brown rice, and quinoa have been proven to improve heart health because of the high fiber content and subsequent reduction of systolic blood pressure.
-
Berries like strawberries, blueberries, and raspberries are packed with antioxidants and protect against oxidative stress and inflammation which contributes to heart disease.
-
Avocados are a source of monounsaturated fats
-
Fish like salmon are loaded with omega-3 fatty acids
-
Walnuts contain fiber and micronutrients like magnesium and copper
-
Dark chocolate is loaded with antioxidants including flavonoids
-
Tomatoes are rich in lycopene, and lots of antioxidant properties
-
Almonds are an incredibly good source of heart-healthy monounsaturated fats and fiber
-
Seeds including chia seeds, flaxseeds, and hemp seeds are all great sources of fiber and omega-3 fatty acids
#6 Get a goodnight's sleep
Sleeping better and sleeping more are underrated goals associated with promoting heart health, but it should become a high priority if you are dedicated to improving your heart and your livelihood.
Lack of sleep leads to health problems that will negatively impact your heart, these include:
-
High blood pressure. During normal sleep, your blood pressure goes down. If you are not sleeping well your blood pressure will stay high for a longer amount of time. High blood pressure is one of the leading risks for heart disease and stroke.
-
Type 2 diabetes. Diabetes is a disease that causes sugar to build up in your blood, a condition that can damage your blood vessels and subsequently your heart. Getting more sleep and better sleep can help improve your blood sugar control.
-
Obesity. Not getting enough sleep can affect a part of the brain that controls hunger, leading to unhealthy weight gain and more heart issues.

Sleeping is not always an easy goal to task yourself with, even if you do not have a sleep disorder, sleeping better and sleeping more is a job that requires discipline and consistency.
Now that you understand how impactful a restless night’s sleep can be for your aging heart, here are some ways you can sleep through the night, fall asleep quicker, and sleep more consistently:
- Find a pattern in your body’s natural sleep-wake cycle. Try to go to sleep and get up at the same time every day, avoid sleeping in, even on weekends, limit naps to 15 to 20 minutes, fight giving into drowsiness before bedtime
-
Control your exposure to light, and blue light in particular. Melatonin is a naturally occurring hormone controlled by light exposure that helps regulate your sleep-wake patterns. Your brain emits more melatonin when it’s dark, making you sleepy, and less when it’s light, making you more alert.
-
Exercise during the day. Even light exercise such as walking for just 10 minutes a day improves sleep quality
- Keep your room dark, cool, and quiet
#7 Oxygen therapy may benefit heart patients with intense breathing complications
Congestive heart failure means that your heart can no longer pump blood as well as it should. It is most common as you age, because over time your heart begins to weaken.
There are 4 stages of heart failure and treatments vary based on the stage and condition of an individual's heart. Oxygen therapy or supplemental oxygen is commonly prescribed for patients in certain stages of heart disease.
While this is not a cure for heart failure, oxygen therapy can help you breathe in the extra oxygen your heart is unable to pump on its own. Utilizing supplemental oxygen could be a wonderful option for you if you are eager to be more active and mobile by reducing your shortness of breath.
There are a lot of personal goals you must be willing to set in order to reap the benefits of supplemental oxygen therapy. One place you can start is understanding the benefits of using a portable oxygen concentrator.
The first several, most obvious, benefits of using a portable oxygen concentrator:
-
You won’t have to worry about a lack of oxygen or your oxygen tank running out- this peace of mind alone will open reduce anxiousness and open up space to care for your loved ones and expand on new and exciting endeavors
-
It is much more discreet and lighter weight than bulky oxygen tanks
-
You can find a sense of independence just being able to move about the house more easily
-
You will have the ability to exercise without shortness of breath, improving your heart beat, bone structure, and mental health
-
Sleeping better is very important for avoiding heart problems associated with high blood pressure, diabetes, and obesity.
-
Stamina and vitality boosts when you are capable of accomplishing tasks you couldn't do before due to breathing implications and tiredness
- Overall mood increases when steps 1-6 kick in
Aging lungs
Lung health requires growing attention as we get older, but it is not something to become discouraged or shy away from.
The loss of strength and ability to breath easily as we age is a normal development in many people’s bodies, whether it is due to genetics, inhaling smoke, or working in a hazardous environment.
While there are natural effects of aging lungs, you do not have to accept a fate that leaves you immobile, unhealthy, and bored. Instead use the goals listed here to help you reduce the breathlessness associated with lung disease, and reduce your risk of lung problems over-all.
#8 Your lungs need more physical activity
If you are struggling with COPD or any long-term lung conditions, regular exercise and physical activity can help improve your breathing threshold, allowing you the freedom to breathe more easily while going about your daily activities.
It can be very uncomfortable to become quickly out of breath for anyone with or without healthy lungs, and motivation to exercise is sometimes hard to muster up.
That being said, It is important for the health of your lungs to avoid temptation of letting another day go by with no exercise. By accomplishing more physical activity, you become more fit and capable to handle daily activities with ease.
The first step towards a more active lifestyle, is to ask your doctor or physiotherapist for the best exercise plan that falls within your lung capacity and is safe for you. From there, you can begin to develop a high quality exercise program. It should be built up over time to allow your body to adapt and strengthen at your own pace.
If you reach a point where you are too breathless to talk, slow down the pace, or take a short pause, don't feel discouraged. Instead, remind yourself that the more you do, the more you will be able to do!
Intermittent exercises can help you to deal with shortness of breath when you are beginning to implement physical activity into your life. To accomplish these exercises, you will move for 1–2 minutes, and in between movements you rest or slow down your pace.
Aerobic exercises are the best form of physical activities for lung disease patients because these exercises involve large muscle groups moving in rhythmic and steady movements.
By using multiple muscle groups at one time, your heart and lungs will be working hard to move oxygen to all of your muscles involved, and subsequently enhancing the capabilities of your lungs.

Here are some examples of great aerobic exercises for your lungs:
- Walking
- Biking
- Swimming
- Jogging/ running
- Elliptical
- Low-impact aerobics works outs
- Water aerobics
- Dancing
- Hiking
- Low intensity kick boxing
#9 It is never too late to quit smoking, even if you already have COPD
While quitting smoking won't cure COPD, kicking the habit can stop the rapid rate of decline in lung capacity that happens in smokers with COPD.
By quitting smoking, you're giving your lungs more capacity, this means more chances to exercise, and more exercise leads to more freedom accomplishing daily activities with less shortness of breath.
Studies show that COPD smokers who quit:
- Have fewer COPD exacerbations
- Have fewer hospital admissions
- Have less risk of dying from COPD
Quitting is much easier said than done, and like kicking any habit, it may take a few attempts before anything really sticks. Oftentimes, hearing your doctor tell you, “Quitting is your only option” will get the ball rolling in the right direction.
And for patients with COPD, quitting is a nonnegotiable treatment plan.
There are countless efforts you can take to kick the hardest habit in the book, and it may take time and research to find the right process for you.
Here are some places to start:
- Do not smoke at all
- Stay busy
- Attend a stop-smoking group or follow a self-help plan
- Drink more water and juice
- Drink less or no alcohol
- Avoid individuals who are smoking
-
Avoid situations wherein you have a strong urge to smoke
#10 Limit exposure to air pollutants
As you age, you must also grow aware of the air surrounding you. Over-saturation in the air, usually meaning relatively high humidity or pollution, can introduce a variety of respiratory issues.Those with pre-existing lung issues are particularl
Even if you are not short of breath, or experiencing symptoms of breathlessness, you blood oxygen levels could be dangerously low! Read this blog to learn about how much oxygen you are getting compared to how much you need.
The hallmark symptoms of COPD are shortness of breath, or feeling breathless. It's certainly one of the most common symptoms, as well as that most invasive. Whether you're the person with COPD or the caregiver, shortness of breath is scary and unsettling for everyone involved.
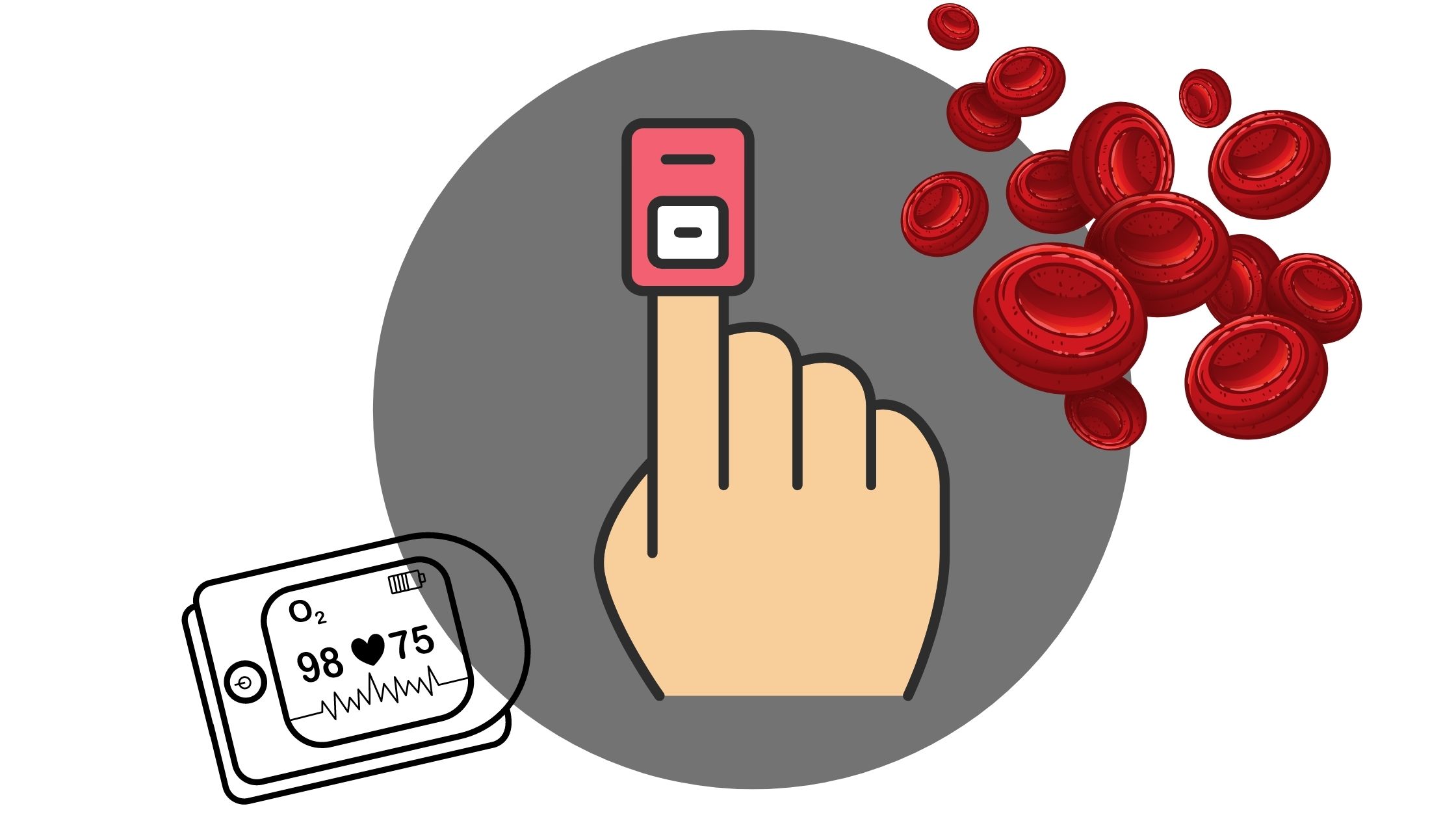
There are devices called pulse oximeters, which measure your oxygen saturation levels. This is important for COPD patients to know how much oxygen they are able to process. Pulse oximeters have become more popular and accessible in recent years.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
This is both a good and bad thing because COPD patients may be relying as much on their oximetry results as their actual symptoms when evaluating their breathing capabilities. It can cause a lot of confusion.
The confusion comes from having a "normal" oxygen saturation level, but still feeling extremely short of breath. Also, it might be hard to notice any symptoms even when your oxygen saturation levels are dangerously low.
We are going to clear up this confusion in this blog.
The Difference Between Shortness of Breath and Being Hypoxic
There are the three main factors that impact how well your body is able to take up and use oxygen.
- How well your lungs absorb oxygen into your body and release carbon dioxide.
- How well your heart is able to pump oxygen throughout your body.
- How well your cells and muscles use the oxygen they get from your blood.
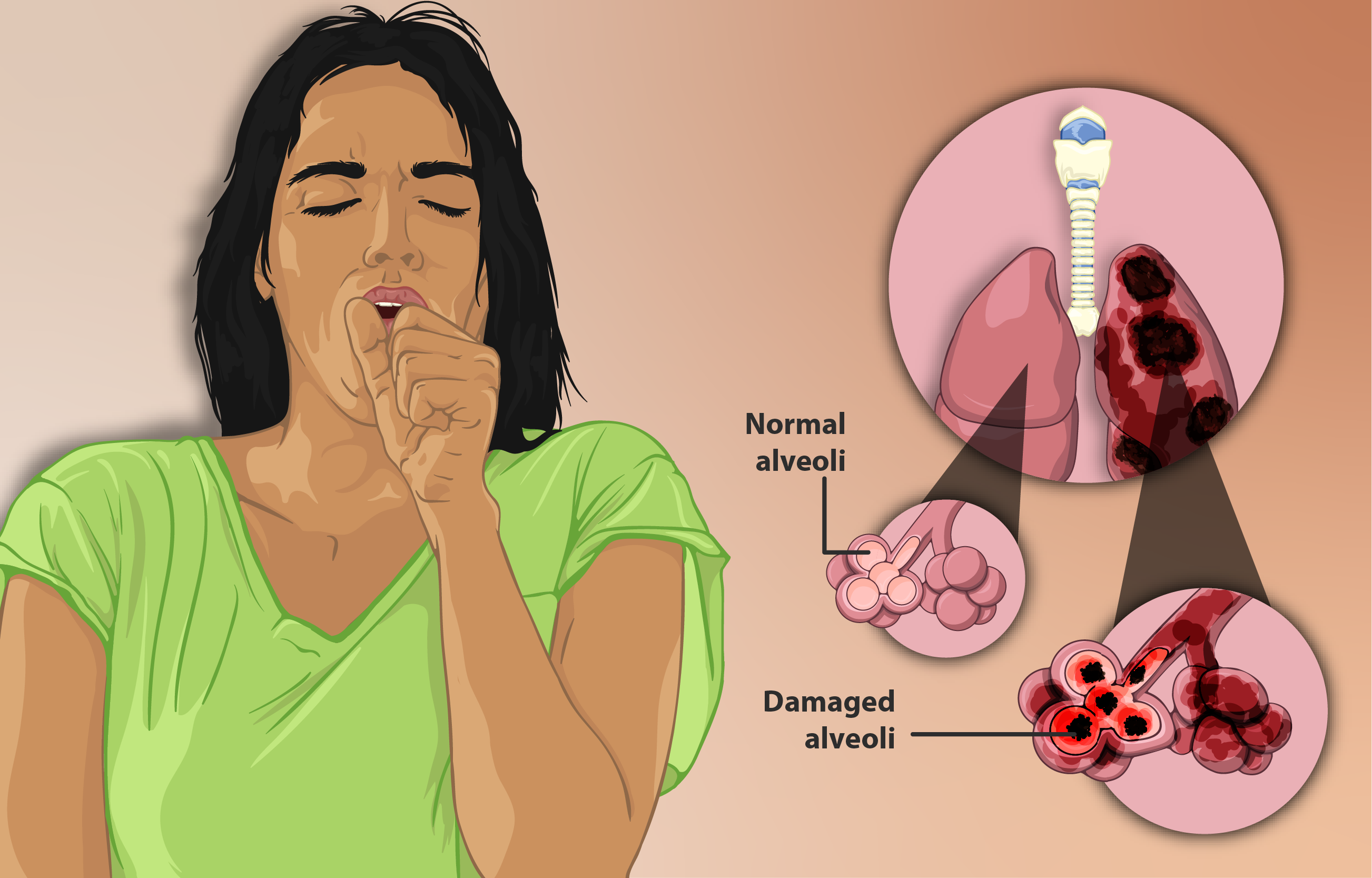
Obviously, various diseases like COPD or heart disease will inhibit some or all three of those factors. COPD causes intense lung damage, and even cardiac problems, that definitely can impact all three of these.Treatment methods including medication, supplemental oxygen therapy, and exercise can help in improving the way your body utilizes oxygen, and in turn, making you less short of breath.

Feeling breathless
Have you ever felt yourself gasping for air, or feeling out of breath even when you’re not exerting yourself? Well this can happen to anyone, and while it is a common symptom of COPD, not everyone who feels short of breath has COPD.
![]()
Breathlessness is associated with lung damage and/or airway inflammation but it can also be caused by:
- Heart health
- How fit you are
- Emotions
- Weather
- Altitude
- Infection
- Low red blood cell count (anemia)
![]()
Even if you are t feeling breathless, this does not always mean that you are hypoxic.
Being Hypoxic or Having Hypoxemia

There is a difference between hypoxemia and being hypoxic. Hypoxia is when there is a low level of oxygen in your blood. Being hypoxic means that not enough oxygen is getting to your body's cells.
These impact your body at two different stages when your body is working to absorb oxygen.
You can find your oxygen saturation level and test whether or not you have these conditions. There are two ways to measure it:
- Arterial blood gases test. This takes place at your doctor’s or a with a lab tech
- Using a pulse oximeter. This you can do on your own, and the small device fits over a finger tip. It uses infrared rays to measure the percentage of oxygen in your blood.

Oxygen saturation is largely dependent on your overall health. This can be indicated by how fast you are breathing during activity and rest.
A typical healthy person has oxygen saturation levels that range from 95 to 100%.When saturation levels drop to 90% and below that is considered low and unhealthy. COPD patients often dip below 90% at times.
Feeling Breathless But Not Hypoxic
Now that you have an understanding of oxygen saturation, and the symptoms associated with low levels of oxygen, you might be wondering, “Why am I so short of breath, but my oxygen levels are still normal?"
Well, even if you're experiencing extreme breathlessness, but your oxygen saturation levels remain in that 95% - 100% healthy range, then supplemental oxygen will not solve your problem.
Instead, you need to learn how to recover from breathlessness. Try stopping what you’re doing and resting right away.

After stopping the action that caused your breathlessness try these additional actions:
- Remind yourself that you know what to do. Taking action can help you overcome the anxiety that often goes along with being short of breath.
- Position yourself to breathe easier. Leaning forward or bending over helps drop your abdomen away from your lungs, making breathing easier. Lean your arms on your knees or on some stationary object like the wall or a counter. (I remember often seeing my dad doing this, especially after a severe coughing spell.)
- Work on controlling your breathing. If you know how to do diaphragmatic or pursed lip breathing, then do so. If you haven't learned those techniques yet, then at least work on slowing and deepening your breaths in and out.
- Once you are feeling better and more in control of your breaths, it may be time to resume whatever you had been doing. But you may need to modify the intensity to avoid re-triggering your breathlessness.
Pulmonary rehab is another great tool that can be beneficial in teaching you how to avoid and/or deal with this symptom. These are classes you take with trained professionals, they teach you breathing exercises and physical activities that are good for your level of health.
You can also look into a rescue, or quick-relief, inhaler. Talk with your doctor about these options, because they can offer some relief in your situation.
Hypoxic But Not Feeling Breathless

Even if you are not feeling at all breathless, your oxygen levels can still be low, and this is an important concept to understand. Low oxygen saturation levels are not healthy, do not ignore it. Get your oxygen levels tested regularly, even if you are not short of breath.
If you do measure low oxygen levels during a blood test, or while conducting pulse oximeter tests. Speak with your doctor right away about the next steps you must take to get your levels to normal.
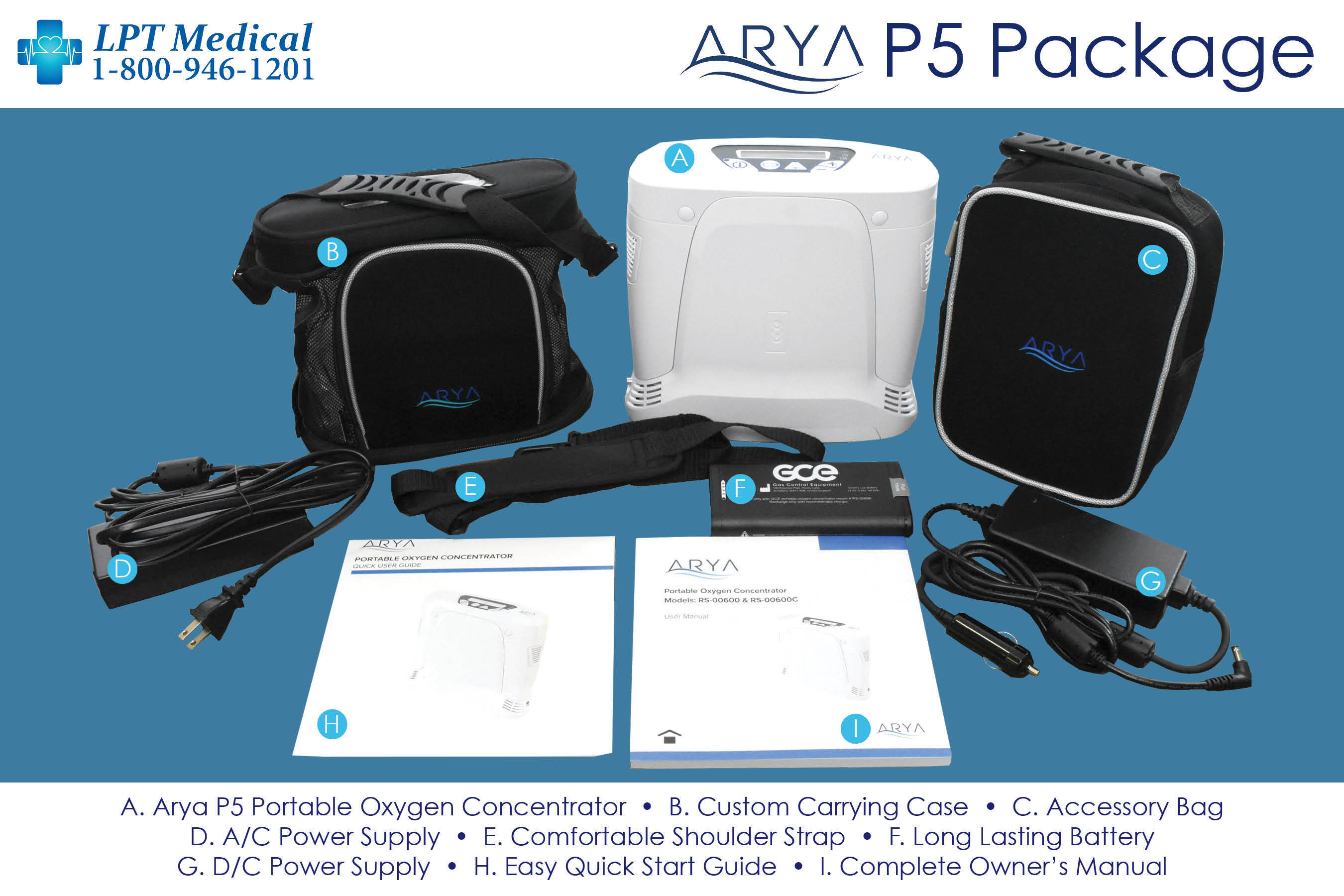
This is often when people need a portable oxygen concentrator to use as their additional source of oxygen. Devices like the Inogen One G5, and the ARYA P5 Portable Oxygen Concentrator often oxygen patients medical grade oxygen they can use 24/7.
It means your blood and tissues are not getting the oxygen they need to survive, and it needs to be addressed right away.
The answer to hypoxia is supplemental oxygen therapy. However, how much and how often you need oxygen depends on the progression of hypoxia you are experiencing and your health care team will determine this. It is also important that your healthcare team helps you with a plan for how often to measure your oxygen levels with a home pulse oximeter.
Overview

If you have COPD, remember that shortness of breath (and other symptoms, such as coughing) are an important thing to take note of. Track your symptoms to measure your current health status and how your health changes over time.
As far as knowing your oxygen saturation level, you will need to monitor this regularly because even if you are not short of breath your oxygen levels could be low, and that is dangerous. This is around the time you will need to call LPT Medical at 1+(800)-946-1201 to talk about your oxygen device options. On the other hand, and unfortunately so, it is entirely possible to be short of breath, but have healthy oxygen saturation.
If you have COPD, then you know that it can be dangerous when your symptoms suddenly get worse. That's why preventing flare-ups and exacerbations is one of the main goals of treatment for people with COPD.
A COPD exacerbation (also known as an acute exacerbation) happens when you get sick or your lungs get especially inflamed, making your symptoms much worse for an extended period of time. Even though they go away eventually, exacerbations can cause serious health complications and permanent damage to your lungs.
When you have COPD, your quality of life depends greatly on how much you prioritize your health and avoid habits and environments that put your lungs at risk. That means doing everything you can to keep your body strong and prevent acute exacerbations.
In this article we're going to help you do just that by explaining a variety of ways you can reduce your risk of experiencing a COPD exacerbation. We'll help you understand why exacerbations happen, how to recognize the warning signs.
Most importantly, we'll show you a variety of practical methods and techniques you can start using today to avoid flare-ups and exacerbations in the future. So if you're ready to improve your quality of life and take charge of your health today, continue reading for 15 practical ways you can reduce your risk for acute COPD exacerbations.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What is a COPD Exacerbation?
Most COPD patients are able to keep their symptoms under control most of the time, but flare-ups and exacerbations are always a threat. The frequency of exacerbations varies from patient to patient and depends on a variety of risk factors, including age, disease severity, and physical activity level.
On average, COPD patients experience at least one or two exacerbations every year. This does not include minor flare-ups, which might happen much more frequently in response to mild irritants.
Flare-ups Versus Exacerbations
A COPD flare-up is a temporary increase in symptoms that can happen when you breathe in respiratory irritants like dust, smoke, or dry air. Flare-ups are generally mild, short-lived, and treatable at home.
Exacerbations, on the other hand, last longer and are more serious than mild flare-ups. They usually happen as a result of a respiratory illness or infection that causes inflammation, excess mucus, and reduced lung function.
Exacerbations often require a trip to the doctor, although they can sometimes be treated at home. It's important to talk to your doctor about what you should do in the case of an exacerbation and how long you should wait to call your doctor when your symptoms start to get worse.
In general, it's safest to talk your doctor as early as possible if you think you might be experiencing an exacerbation. That's why it's very important to recognize the early symptoms and warning signs of an oncoming acute exacerbation.
Unlike flare-ups, exacerbations can have extended or even permanent effects. Sometimes, even once an exacerbation passes, the COPD symptoms don't improve all the way. Some patient's conditions don't ever get back to the baseline that they were at before the exacerbation, and they have to cope with a minor, yet permanent, increase in symptoms from that point on.
Exacerbations can be life-threatening at any stage of the disease, but they are particularly dangerous for people with advanced COPD. Flare-ups are common in all COPD patients, although sensitivity to respiratory irritants and the severity of the flare-up can range significantly depending on the patient's physical condition and disease stage.
How to Recognize an Exacerbation

Exacerbations are serious business, and recognizing the early symptoms could save your life. An exacerbation can be debilitating, life-threatening, and is are not something you should ever take lightly. Most researchers agree that preventing exacerbations is one of the most important things you can do to live longer and slow down the progression of COPD.
Some exacerbations are mild, but some are serious and require early and immediate treatment to prevent serious complications. Severe exacerbations can cause you to be hospitalized or even end in death.
That's why it's vital to pay attention to how you feel and be able to recognize the early warning signs of an acute exacerbation. You should always be monitoring your symptoms and looking for signs that indicate they're getting worse. Often, the only early warning sign of an exacerbation is a worsening of the symptoms you already have.
If your worsened symptoms don't start to get better soon, you should talk to your doctor right away and begin any additional medication
or therapies that your doctor recommends. The earlier you begin treating an acute COPD exacerbation, the better your chances of avoiding life-threatening symptoms and hospitalization.

If you ignore worsened symptoms, they're likely to continue getting worse. The longer you wait to seek help, the more you'll be at risk for serious complications and the less likely you'll be to make a full recovery.
Here are some of the early warning signs of a COPD exacerbation:
- Rapid, shallow breathing
- More difficulty catching your breath than usual
- More coughing or wheezing than usual
- A change in mucus color (yellow, green, or blood-tinged in color)
- Increased mucus in your lungs and airways
- Feeling unusually sleepy or fatigued
- Difficulty sleeping because your symptoms keep you up
- Having less energy than usual to do normal daily activities
- Breathlessness and fatigue at rest or after extremely light activities
- Confusion
If you think you're experiencing the early symptoms of an exacerbation, follow your COPD treatment plan and talk to your doctor as soon as possible. If your symptoms get significantly worse or you can't catch your breath, seek emergency medical care immediately.
There are certain symptoms that are a sign of serious oxygen deprivation and require immediate medical care. If you experience confusion, a severe headache, difficulty catching your breath at rest, a bluish tint to your skin, or have a sudden difficulty walking short distances, you should seek emergency medical attention immediately.
What Happens When You Have an Exacerbation?
When you have an exacerbation you'll experience increased symptoms and increased mucus production that makes it more difficult than usual to breathe. This happens because of inflammation that reduces your lung function and causes inflammation in your lungs and airways.
Mild exacerbations can sometimes be treated at home, although you should always talk to your doctor about when you should call him first. Your doctor might recommend a variety of medications to use in the short term to manage your symptoms until the exacerbation passes.
Here are some common medications used to treat exacerbations at home:
-
Bronchodilator Inhalers: Your doctor might recommend that you use your bronchodilator medication more often or prescribe you a different inhaled medication than you usually use. This will help open up your airways and make it easier to breathe.
-
Corticosteroid Medications: Inhaled or oral corticosteroids are common treatments for COPD exacerbations. They help reduce inflammation in your lungs, reduce swelling, and open up narrowed airways.
- Antibiotics: If a bacterial infection is the cause behind your exacerbation, your doctor might prescribe a course of antibiotics to treat it.
However, if an exacerbation gets worse, you might need to go see your doctor or be hospitalized if it gets severe. You should seek emergency medical care if you experience unusually severe symptoms, can't catch your breath, or show signs of low blood oxygen (like confusion, a severe headache, a bluish color to your skin, or extreme fatigue).
If admitted to a hospital, you will receive more intensive treatment that may include bronchodilators, systemic corticosteroids, supplemental oxygen, and breathing support. If your lungs aren't working well enough on their own, you may have to use a ventilator or a positive expiratory pressure (PEP) device to keep your airways open.

Without prompt medical treatment (and even with it), a serious exacerbation can be life-threatening. That's why preventing exacerbations is one of the most important things you can do to stay healthy and live longer with COPD.
What Causes COPD Exacerbations?
|
|
| Photo by Senior Airman Anthony Sanchelli |
There are many different COPD triggers, including dust, pollen, and cold air, that can cause your symptoms to get worse. However, these irritants usually only cause minor flare-ups, not full-blown exacerbations.
However, exposure to COPD triggers like respiratory irritants can significantly raise The majority of the time, exacerbations are caused by a respiratory illnesses or infection, not respiratory irritation alone.your risk of subsequent exacerbations.
According to research, respiratory illnesses cause 70 to 80 percent of exacerbations experienced by people with COPD. That's why it's so important to do whatever you can to avoid getting sick, including getting vaccinations, practicing good hygiene, and living a healthy lifestyle.
Here is a list of some of the most common causes of COPD exacerbations:
- Pneumonia
- The flu
- Seasonal allergens
- Smoke
- Air pollution
Unfortunately, in up to one-third of cases doctors are unable to determine the cause of a COPD exacerbation. It's important to make choices that limit your risk of having an exacerbation, but there's no way to reduce that risk to zero.
There are certain risk factors for exacerbations that you have little or no control over, like your age and the severity of your disease. Here are some common factors that put you a greater risk for exacerbations if you have COPD:
- A history of frequent exacerbations
- If you've had an exacerbation within the past year
- If you have more severe COPD symptoms (e.g. a severe daily cough or severe breathlessness every day)
- You have severely reduced lung function
- Low BMI
- Lack of exercise
- Old age

Taking care to avoid exacerbations is one of the most important things you can do to stay healthy, stay strong, and maintain your quality of life while living with COPD.. If you are ready to learn what you can do to protect your lungs and maintain your quality of life, continue reading to learn about fifteen different ways to avoid COPD flare-ups and exacerbations.
How to Prevent a COPD Exacerbation
Now that you understand the risk factors for exacerbations, why exacerbations happen, and how to recognize the early warning signs, it's time to learn how to prevent them. Even though you can't always avoid exacerbations, there are many different things you can do in your daily life that reduce your risk.
In these next sections, we're going to show you how you can avoid exacerbations by incorporating simple habits and techniques into your everyday life. We'll go in-depth into a variety of activities, useful techniques, and special precautions you can take to reduce your risk.
Don't put it off any longer; continue reading to learn about a variety of practical steps you can take today to reduce your risk of experiencing a COPD exacerbation.
Avoid Weather and Temperature Extremes
Hospitalizations for COPD-related exacerbations and complications go up significantly in extreme temperatures and weather. That's why you have to be particularly careful to protect yourself during the summer and winter months.
In general, it's a good idea to avoid going outdoors whenever it is extremely hot or cold outside. Both hot and warm air are hard on your lungs, make it difficult to breathe, and can make you more prone to flare-ups and exacerbations.
Avoiding Hot Weather

For some people with COPD, the summer heat brings relief and decreases their symptoms. But for those who are not so lucky, the hot air can make a variety of COPD symptoms worse.
When you spend time in the heat, it raises your body temperature, which makes your body have to work harder to cool you down. This is taxing on your lungs, which already need extra energy to function, and can make it much more difficult to breathe.
You are also more likely to get dehydrated and feel fatigued when you are out in the hot, humid air. Hot weather also tends to correspond with higher ozone pollution levels, which can irritate your lungs and make you even more prone to flare-ups and exacerbations.
Here are some tips for staying healthy and avoiding exacerbations in hot weather:
-
Always stay indoors when it is very hot or the air quality is low. Plan exercise and outdoor activities for milder days.
-
Plan activities during the early morning or early evening, when the temperatures are cooler. The hottest temperatures tend to occur between 11 am and 3 pm every day.
-
Drink lots of water during the summer, especially when you exercise or spend time outdoors. Always bring a bottle of water with you when you go out.
-
Keep your home cool and air-conditioned. If you don't have air conditioning, go to a public place that does have AC, like the library or mall, on very hot days.
-
If you feel overheated, try taking a cool bath or shower to cool down.
- Use a fan in your bedroom at night or any other rooms that tend to get hot and stuffy. You can also get a hand-held, battery-powered fan to bring with you whenever you go outdoors in the heat.
-
Drink a sports drink or salty food after sweating or spending time in the heat to replenish lost electrolytes.
-
If you are sensitive to allergens, always check your local pollen and allergen forecast. You can check it online at pollen.com.
- Bring your inhaler and any quick-relief medications with you whenever you go out in case your symptoms flare up.
Avoiding Cold Weather

Cold weather can also make COPD worse and put you at a much greater risk for exacerbations. In fact, one study showed that cold weather caused a significant increase in hospital admissions, with up to a 20% increase in hospitalizations for people with COPD. The main factors increasing the risk were lower temperatures, windchill, cold weather that lasted for more than a week.
Winter weather causes an increase in symptoms in part because cold air is denser, drier, and more difficult to breathe. Cold, dry air dries out your airways and nasal passages, causing inflammation that worsens symptoms and increases mucus production.
Together, these effects make it more difficult to breathe and increase your risk of getting an illness or infection. The effects are the worst at temperatures below freezing, but COPD hospitalizations increase at temperatures as high as 41 degrees Fahrenheit.
That's why it's so important to stay indoors and take extra precautions during the winter months. Here are some tips for avoiding cold weather and staying healthy during the winter:
-
Stay indoors on cold days and when the air quality is low. Don't exercise or do other physical activities outdoors; instead plan them for warmer days or save them for a warmer season.
-
Always dress warm for cold weather and use layers so you can add or remove them if your comfort level changes.
-
Always breathe through your nose, not your mouth. This allows the air to warm up and pick up moisture as it travels through your airways to your lungs.
-
Cover your mouth with a scarf or cold weather mask anytime you have to be out in the cold air. This traps the heat and moisture from your breath in order to warm and humidify the air you breathe.
- If you use supplemental oxygen, cover your oxygen tank and tubing when you go outdoors. You can string your tubing underneath your jacket or coat to keep it warm.
Humidity

Humidity is yet another weather condition that can have a significant effect on people with COPD. Most people do best when the humidity is around 40 percent, and a humidity range between 30 and 50 percent is recommended for people with respiratory conditions and diseases.
Both too little and too much humidity makes it difficult to breathe and can make your COPD symptoms worse. Dry air is harsh and irritating to your lungs, while extra-humid air is heavy and hard to inhale.
Humidity tends to be highest in warm weather, because warm air is able to hold more moisture. The air tends to be much drier during the winter, and the dense, cold air tends to make air pollution worse as well.
But humidity isn't just about the weather; even if the humidity is ideal outdoors, the humidity inside your house can still get high. Running a shower or bath and using appliances like your dishwasher or washing machine can raise the humidity in your home if you're not careful.
Humidity effects everyone differently, so pay attention to what humidity levels make your symptoms better or worse. To reduce your chances of flare-ups and exacerbations, you should avoid spending time outdoors any time the air is especially humid, especially dry, or polluted.

Here are some general tips for dealing with dry and humid weather:
-
Get a humidifier for your home and use it during the dry winter months. You can get one for your bedroom and any other space you tend to spend a lot of time in, or you can get a whole-house humidifier that hooks up to your home's main ventilation system.
-
When the humidity outdoors is very high, keep your windows and doors closed to keep the moist air out of your home.
-
Make sure any appliances that release moisture into the air, including your washing machine, clothes dryer, stove, and dishwasher well-ventilated.
-
Whenever you take a shower or bath be sure to open a window or turn on your bathroom fan to vent extra humidity.
- Use the vent fan on your stove when cooking steamy or smoky foods.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Attend Pulmonary Rehabilitation
Getting exercise and living an active life is another one of the best things you can do to keep your body healthy, strengthen your breathing muscles, and reduce your risk of COPD exacerbations. But in order to get enough exercise, you need to know how to manage your symptoms and control your breathing while you work out.
That's why many doctors recommend that COPD patents attend pulmonary rehabilitation, a special class designed specifically to help people with respiratory diseases live healthier, happier lives. Many people begin pulmonary rehabilitation after they have difficulty exercising and managing their disease on their own.
But pulmonary rehab is about more than just exercise; it's about learning how to manage all the different aspects of your life that are affected by COPD. You'll learn how to keep your lungs healthy, how to manage your symptoms, and how to handle the stress and emotional strain of living with a chronic disease.
Classes are usually run by medical specialists or social workers who have a wealth of knowledge and experience to share. Classes usually focus on these main areas:
- Exercise training classes
- Learning and practicing breathing techniques
- Diet and nutritional counseling
- Lung health and disease education
- Learning how to conserve energy for what's most important
- Mental health counseling and group support sessions
- Learning how to use oxygen and other medications to manage respiratory symptoms
Research shows that taking a pulmonary rehabilitation class increases exercise capacity and overall health in people with COPD. Multiple studies have also found that pulmonary rehab significantly reduces patients' risk of future exacerbations and hospital admissions, too.
Pulmonary rehabilitation is like a crash course on how to live the best possible life while managing your COPD. It's one of the best things you can do to jump-start your COPD treatment and learn how to integrate positive, healthy habits into your everyday life.
Find a Pulmonary Rehabilitation Class Near You

Pulmonary rehabilitation classes vary depending on where you live and what kind of help you need. Some programs are hosted as group classes at hospitals and clinics, some offer individual instruction, and some can even be done partially or fully at home.
If you have COPD, talk to your doctor about whether or not you could benefit from pulmonary rehabilitation. Your doctor can give you a referral and help you find a class in your local area that works for you.
Here are some resources to help you locate a pulmonary rehabilitation program near you:
Personal hygiene is one of those things that everyone knows is important, but few actually take seriously enough. For most people, hygiene is simply a routine part of life, not something they go out of their way to think about pay attention to.
But if you suffer from COPD, it's important to make good personal hygiene a top priority in your daily routine. Proper hygiene is your very first line of defense against illnesses and dangerous COPD exacerbations that can make your disease even worse.

LPT Medical's newest and most impressive portable oxygen concentrator, the ARYA P5 portable oxygen concentrator
However, practicing good personal hygiene takes more effort than most people think. Doing it right takes extra time out of the busy day, and it's very tempting to cut corners to save time.
That's why everyone should take the time to review the important components of good personal hygiene now and then. If you have COPD, then you have even more at stake, and you should take extra care to learn all the proper techniques.
In this post, we're going to show you what good personal hygiene looks like and how it can help you protect your lungs and manage your COPD. This guide will discuss a variety of important hygiene issues, both general and COPD-specific, and help you learn the skills you need implement good hygiene practices in your everyday life.
Why Hygiene is So Important for People with COPD
Most people understand the basics of good hygiene, but not everyone is great at practicing it consistently. Even so, imperfect hygiene is not usually a problem for most healthy adults.
However, good personal hygiene is much more important for people who suffer from COPD. The disease suppresses patients' immune systems, which makes them particularly vulnerable to disease-causing germs like viruses and bacteria.
Even worse, it can be very dangerous to get even a little bit sick if you have COPD. Respiratory illnesses, in particular, can wreak havoc on your lungs and immune system, making it much more difficult to breathe and control other COPD symptoms.
That's why practicing good hygiene is so vital; it protects you from the germs, bacteria, funguses, and respiratory irritants that cause you to get ill. You can't always control whether or not you get sick, but practicing good personal hygiene is one of the few effective things you can do to reduce your risk.
Even minor viruses like the common cold can worsen breathing problems significantly and permanently damage your lungs. Because of blockages and narrowing in your airways, COPD also makes it harder to flush viruses and bacteria out of your respiratory tract.
This significantly raises your risk for secondary lung infections like pneumonia if you get sick. COPD also makes it more difficult to recover from illnesses and infections.
In this way, COPD not only causes you to get sick more often, but also causes you to stay sick for a longer period of time. Unfortunately, one of the consequences of staying sick longer is an increased probability of minor illnesses causing serious infections and permanent damage to your lungs.
In the most serious cases, getting sick when you have COPD can lead to respiratory failure, hospitalization, and even death. That is why it is so important to practice impeccable hygiene if you suffer from COPD.
The Benefits of Good Hygiene

The main benefit of good hygiene is a significantly reduced chance of getting sick. That's because, when you practice good hygiene, you prevent a myriad of disease-causing pathogens like viruses, bacteria, and parasites from making it into your body.
Good personal hygiene is also good for those around you because it prevents you from spreading germs and sicknesses to other people. By practicing good hygiene, you can help protect other people with immune-suppressing diseases like COPD and prevent them from getting illnesses that could potentially threaten their lives.
Along with these physical benefits of good hygiene, there are social and psychological benefits as well. When you keep yourself clean, healthy, and groomed, you are likely to feel more confident and capable in other ways, as well.
Here are some of the main benefits of healthy hygiene habits:
- Improved overall health
- Reduced risk of disease and infections
- Reduced exposure to allergens and other respiratory irritants
- Reduced risk of COPD exacerbations
- Reduced risk of hospitalization
- Reduced risk of spreading germs and illnesses to others
- A cleaner, healthier living environment
- Improved confidence, self-image, and self-esteem
- Other people see you as more healthy, desirable, and attractive when you have good hygiene
What Does Good Personal Hygiene Look Like?

You probably already know the basics of good hygiene like bathing and washing your hands. But there's also a good chance you don't know, or have forgotten, the details of what good hygiene entails.
Still, knowing the basics works well enough for most people most of the time. At worst, most healthy adults will only get a mild illness every so often if they expose themselves to germs.
However, living with COPD means you can't cut any corners without putting your health in serious risk. That means you need to go out of your way to practice impeccable hygiene, even if you've gotten away with an average amount of effort so far in your life.
But to do that, you need to understand what good hygiene is and exactly what you have to do to practice it. Fortunately, practicing good hygiene is relatively easy to do and even simpler to learn.
The basics of good personal hygiene include:
- Knowing when to wash your hands
- Knowing how to wash your hands properly
- Knowing how to prevent yourself from spreading germs to others when you are sick
- Knowing how to avoid transferring germs to your body in public places
- Knowing how to practice good dental hygiene
- Knowing how to clean your body and your clothes to prevent germ buildup
How to Practice Good Hygiene to Improve Your COPD
In this guide, we're going to give you a refresher course on how to practice good personal hygiene. We'll also address a variety of personal hygiene issues and challenges that affect people with COPD specifically.
In these next sections, we will go through each important hygiene issue step by step so you can learn the proper techniques. We'll also give you tips for how to practice good hygiene every day and fit important hygiene practices into your daily routine.
Learning the tips and techniques we explain in this guide will help you ensure that you are doing everything you can to protect yourself from sickness and disease. That way, you can live your life more safely, more confidently, and with a reduced risk of serious COPD complications.
Wash Your Hands Often

Even though washing your hands might seem like obvious advice, it is so essential to personal hygiene that it's still important to review. It is the first step to practicing good hygiene and one of the most effective ways you can protect yourself from disease.
Unfortunately, most people are not as diligent about hand-washing as they should be, even knowing how important it is. Many people remember to wash their hands before eating or going to the bathroom, but get lazy or forget to do it in other situations.
Another problem is that most people don't take enough time to wash their hands thoroughly enough, which makes their hand-washing less effective. As a result, their hands may still harbor harmful bacteria even after washing up.
How to Wash Your Hands the Right Way

If all you do is rub your hands together with soap while giving them a quick rinse under the faucet, then you're not washing them well enough. In fact, if it takes you less than a full twenty to thirty seconds (count it!), then you probably need to correct your technique.
Here is a quick overview of proper hand-washing technique, as recommended by the CDC:
- Use clean, running water to rinse and wet your hands before applying soap.
- Rub the soap between your hands until it forms a lather.
- Scrub your hands for at least twenty seconds, getting your nails, wrists, and between your fingers.
- Rinse off all the soap under clean, running water.
- Dry your hands off on a clean towel.
To wash your hands properly, you need to make sure you scrub every part of your hands thoroughly with soap, including your fingers, fingernails, palms, wrists, between your fingers, and the backs of your hands. Any kind of regular, non-antibacterial soap will do the trick, including bar soap, liquid soap, and foaming soaps.
You may need to wash the skin above your wrists and further up your forearms after cleaning, washing dishes, or doing anything else that is likely to fling bacteria around. If your hands are especially dirty, you should also use a nail brush to scrub around and underneath your fingernails to remove excess dirt and grime.

Here are some more tips for more effective and hygienic hand washing:
- Avoid antibacterial soaps and hand sanitizers: Using antibacterial soaps and hand sanitizer is almost never necessary because regular soaps and sanitizers are effective. Additionally, anti-bacterial soaps are bad for the environment, and may even be bad for your health.
- Keep your hand towels clean and dry: If your hand towel stays moist for too long, it creates a perfect environment for mold and bacteria to grow. Let your hand towels dry thoroughly between uses and wash them regularly, especially if you notice a bad or musty smell.
- Don't re-contaminate your hands: After you get your hands all clean, you don't want to have to start over again. That's why you should be careful not re-contaminate them right away by touching a dirty faucet or door handle on your way out of the bathroom. When using a public bathroom, cover your hand with a tissue if necessary to avoid touching dirty public surfaces.
To see proper hand-washing technique in action, check out this video from the CDC.
When to Wash Your Hands

You probably already know that you should wash your hands before and after eating and after you use the bathroom. However, there are many other situations that call for thorough hand-washing, and some are less obvious than others.
In general, you should wash your hands after completing any activity that puts you in contact with germs. That includes anything that involves handling dirty items, touching public surfaces, or coming into contact with someone who is sick or injured.
Here is a more complete list of situations in which you should wash your hands:
- Before and after handling food
- Before and after eating
- Before and after treating a wound
- Before and after touching your face, especially your eyes, nose, and mouth
- Before and after caring for a sick person
- After sneezing, coughing, or blowing your nose
- After using the bathroom
- After changing a diaper or handling pet waste
- After touching a pet or other animal
- After touching another person
- After handling garbage or waste
- After touching a public item or surface (like a public pen or ATM)
- After smoking
Use Hand Sanitizer

Sometimes, you won't have access to a sink when you need to wash your hands. In case this happens, it's a good idea to keep hand sanitizer with you whenever you leave the house.
For the best protection, you should always use alcohol-based hand sanitizers instead of antibacterial ones. To be effective, your hand sanitizer should contain no less than 60 percent alcohol.
These hand sanitizers can kill the majority of bacteria and fungi on your hands as well as many viruses. The higher percentage of alcohol the sanitizer contains, the more effective it will be against all kinds of microbes.
However, hand sanitizer only works effectively if you use it right. If your hands are greasy or grimy when you apply hand sanitizer or you wipe the solution off too soon, then you won't get its full protection.
But even though it can be good in a pinch, hand sanitizer is not a good substitute for hand-washing in all cases. Using hand sanitizer is not nearly as effective as washing your hands, and you should only use it as a backup for times when hand-washing is not an option.
Here are some tips for using hand sanitizer correctly to protect yourself from illnesses and infections:
- Use hand sanitizer by pouring a dime-sized dollop into the palm of your hand and rubbing the solution thoroughly into your palms, fingers, and the backs of your hands.
- Make sure you don't have dirt, oils, or grime on your hands before applying hand sanitizer, otherwise it may not be effective.
- Once the solution has been absorbed into your skin, let your hands air dry. (Don't wipe your hands off; it should only take a few seconds for the solution to dry on its own.)
- Do not rely on hand sanitizer to clean harmful chemicals like pesticides off your hands.
Bathe Often for Healthy Skin and Lungs

No matter how careful you are to avoid germs, your body inevitably picks plenty of them up from your environment throughout the day. When you go outside, cook, clean, and sweat, you are exposed to all sorts of bacteria, fungi, and other harmful particles that stick to your hair, clothes, and skin.
<

Giving your lungs a break is an important daily task you, as a responsible COPD patient, should work towards.
Every time you are able to make your lungs work less, you are bettering your condition and your livelihood. This can be as simple as getting an air purifier in every room of your home and should be as constant as adhering to your oxygen prescription daily.
In this blog we talk about the easiest way to give give you lungs a break. The best thing you can do is acquire a portable oxygen concentrator that will help you move through the day and your life with ease. In order for that to be a possibility, you need a supplement oxygen device unit this is lightweight, reliable, and affordable!

As you probably know Chronic Obstructive Respiratory Disease is a progressive illness that is not curable. Therefore, your treatment and how you manage this disease is essential to ensure your COPD does not progress quickly into a more severe stage of COPD.
Resting you lungs is, in itself, a treatment for managing COPD. By reading this blog, you can expect to learn the best oxygen units that will help you to manage your disease effectively and subsequently improving your quality of life with COPD.
Taking your Oxygen Therapy Seriously

If you are prescribed oxygen therapy, adhering to your prescription as you doctor orders is essential for taking care of your lungs, and overall health and well-being.
Long-term oxygen therapy is the only known treatment for COPD that is proven to extend the life expectancy of COPD patients. Therefore, using your oxygen equipment correctly can help you live a better quality life longer.
In this section we will discuss three portable oxygen concentrators all of which are reliable but each device is designed to cater to a different oxygen patient.
The ARYA P5 portable Oxygen Concentrator

The ARYA P5 portable oxygen concentrator is already making a name for itself in the oxygen industry as one of the smallest and quietest portable oxygen concentrators on the market. It is one of the newest portable oxygen concentrators available and it's not only small, it's also reliable, gets great battery life, and offers 10 different oxygen settings for more accurate dosing.
Along with being one of the smallest and quietest portable oxygen concentrators on the market, the ARYA P5 portable oxygen concentrator has some amazing features that set it apart from the rest of the units on the market.
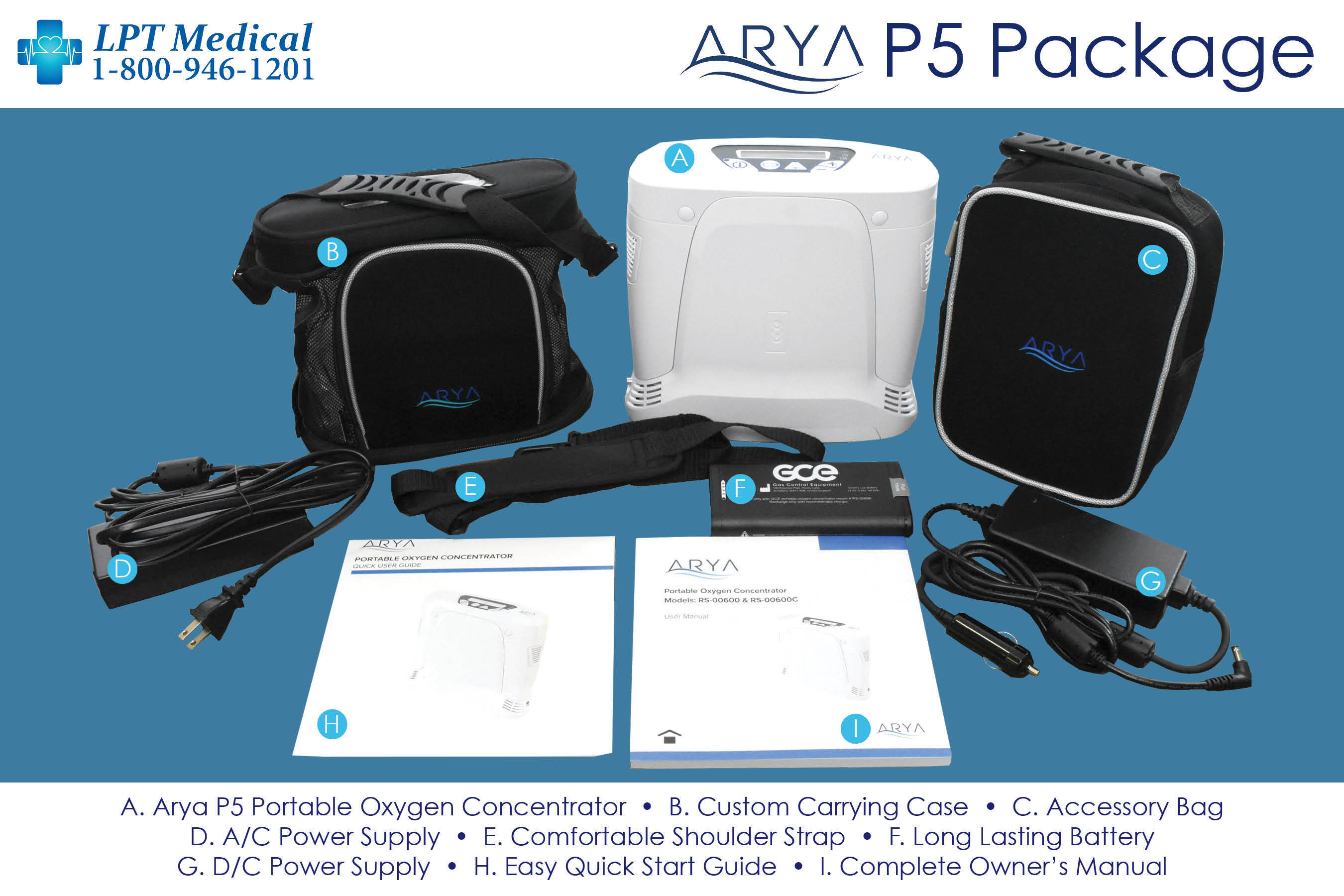
The ARYA P5 is going to make getting back to living an active life as easy as possible. It’s lightweight with long-lasting battery life helping you regain your freedom and independence. It gets up to 8 hours of battery life and offers 10 different oxygen settings! There’s no other lightweight portable oxygen concentrator on the market that will give you more accurate oxygen dosing while running for up to 8 hours
There are several reasons why oxygen patients should be excited about the new ARYA P5 portable oxygen concentrator. The first, and most importantly, is that the oxygen delivery service is unmatched.

When looking for a portable oxygen concentrator, the second most important priority should be the weight and size of the oxygen device.
As mentioned above, the ARYA P5 is one of the smallest and lightweight portable oxygen concentrators money can buy! It weighs just 5.5 pounds with the battery installed, and it stands 9.8” W x 3.8” D x 9.25” H.
At 5.5 pounds, the ARYA P5 is going to be a great companion for anyone that is interested in a healthy and active lifestyle. Exercise becomes easier, being more mobile and independent is also an option now. Traveling no longer seems like a chore, but it is something to be excited about!
Not to mention, with the ARYA P5 you will have the oxygen you need without sacrificing other parts of life. Go exercise, grab lunch with your friends, or spend a day golfing without feeling weighed down by your oxygen.
The ARYA P5 is a device that will help first time oxygen users and long time oxygen users by giving everyone who needs supplemental oxygen therapy the freedom and independence they need.
The ARYA P5 offers a high oxygen output to accommodate as many oxygen users as possible. The ARYA P5 has 10 adjustable oxygen settings. It offers pulse flow settings 1-5 and increases by increments of 0.5. This precision oxygen delivery is important for people so they are getting the exact amount of oxygen their bodies require, not too much and not too little!

It offers pulse flow settings 1-5 that can be adjusted in 0.5 increments. So whether you’re exercising, feeling sick, or are experiencing an exacerbation you will be able to increase the machine’s oxygen output to get the oxygen you need. Just remember to check with your doctor before you increase the flow rate on your machine.
The ARYA P5 also comes equipped with RATE RESPONSIVE THERAPY™ (RRT) that delivers oxygen on demand! Everytime the device senses an inhalation, the breadth th triggers the device to respond accordingly. Whether a patient is climbing the stairs or taking a walk, ARYA P5 will automatically respond to the breath rate by adjusting the amount of oxygen needed to ensure the patient remains saturated.
The ARYA Portable Oxygen Concentrator

The ARYA Portable Oxygen Concentrator is a pulse flow portable oxygen concentrator (POC) that can cover oxygen patients that need pulse flow oxygen delivery less than 5 liters per minute.
One of the best things about the ARYA portable oxygen concentrator aside from it being lightweight (5 pounds) and having a long lasting battery (up to 16 hours) is the comprehensive warranty. It's not often you see a manufacturer give you an extended warranty on the portable oxygen concentrator as well as the sieve beds!
With the ARYA portable oxygen concentrator you will have added peace of mind knowing you get lifetime warranty on the unit and an industry leading 5 year warranty on the sieve beds!
Most manufacturers offer a 3 year warranty on their unit and a 1 year warranty on the sieve beds. But ARYA truly stands behind their product like no one in the industry.
The Respironics SimplyGo

The Respironics SimplyGo is both a pulse flow and continuous flow POC. It has the capabilities to support oxygen patients that need pulse flow operation up to 6 liters per minute or 2 liters of continuous flow.
Weighing in at a mere 10 pounds and standing 10" H x 6" D x 11.5" W, the SimplyGo is one of the smallest and lightest continuous flow portables available! You will be able to bring it with you wherever you go and you will have no problem finding a place to store it.
Your SimplyGo will easily fit underneath the seat in front of you on the airplane, you can store it on the floor of your car or in the passenger seat as you drive, and when you don’t need to use it you will be able to put it in your closet without having to clear space for it.

Although 10 pounds is extremely light for a continuous flow portable oxygen concentrator, it’s still pretty heavy to carry. But you won’t need to worry about that! Your SimplyGo package will include a custom carrying case and a wheeled travel cart so you have the option to carry it over your shoulder or you can pull it behind you on the travel cart.
The SeQual Eclipse 5

The SeQual Eclipse 5 POC is a popular continuous flow device that is also reliable and durable. It is rated to last for years and the POC of choice of the U.S. military!
The pulse flow settings range from 1-9 and the continuous flow settings range from 0.5-3.0 LPM, so it is able to cover most oxygen patient’s needs, and some!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
As mentioned above, the SeQual Eclipse 5 is one of the most, if not the most, popular continuous flow portable oxygen concentrators on the market. That is largely due to its long-standing track record for being durable and reliable. If it’s good enough for the US Military, that should tell you something.
The hard-bodied shell of the Eclipse 5 is extremely protective. It will keep your concentrator protected from everyday wear and tear, accidental bumps and bruises, and if you have pets or grandkids in the house it will be able to withstand their crazy antics.
One of the best things about the Eclipse 5 is that it requires very little maintenance from you to keep it running. All you need to do is wash your filter once every week or two depending on how often you use your Eclipse and you are good to go!


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!