One of the things that makes COPD so dangerous is the fact that it makes your body more vulnerable to disease. It not only makes you more likely to get sick, but it makes it harder to recover from illnesses, too.
For people with COPD, any sickness—even a common cold—can be serious or, in some cases, even life-threatening. Even worse are respiratory infections like pneumonia, which can cause permanent damage to lungs affected by COPD.
Because of this, it is imperative for every person with COPD to take good care of their immune system. Because your immune system is so closely linked with all of your body's other systems, that means making healthy choices when it comes to your diet, sleeping habits, personal hygiene, and even your mental health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this guide, we're going to tell you everything you need to know about how to keep your immune system in the best shape possible while managing your COPD. Using the practical tips in this article, you can make sure you are giving your body everything it needs to protect itself from illnesses and infections.
Because you never know when sickness will strike, it's important to make your immune system's health a priority now, and not put it off for the future. By building healthy immune habits early and continuing to be diligent, you may be able to prevent a number of illnesses that could worsen your COPD.
In this Guide:
- What Works and What Doesn't
- How Your Immune System Works
- How COPD Affects Your Immune System
- Practical Tips You Can Use to Boost Your Immune System the Right Way
- Vitamins and Nutrients You Need for a Healthy Immune System
- The Anti-Inflammation Diet
- Things that Don't Help Your Immune System
What Works and What Doesn't
The world around us is full of products that make lofty claims about boosting your immune system and staving off disease. You've probably seen them advertised on TV, in magazines, health food stores, and even your local supermarket.
Unfortunately, these products are usually nothing more than glorified snacks that won't boost your immune system in any way. So far, scientists haven't been able to confirm that any health food or supplement on its own will reliably improve your resistance to illness.
However, researchers have identified a variety of healthy habits and nutrients that support your immune system and keep it running smoothly. On their own, they are unlikely to make much of a difference, but putting them all together will help you build a healthier lifestyle that boosts your body's ability to fight off infection and disease.
It's important to know that keeping your immune system healthy isn't about taking a certain supplement or miracle vitamin; it's about giving your immune system everything it needs to stay strong. It's also about avoiding activities and habits that weaken your immune system's ability to respond to threats.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In these next sections, we're going to tell you all about all the nutrients, healthy habits, and other treatments like vaccines that you need to keep your immune system primed and ready to fight disease. While none of these things are miracle cures, they are the most effective, proven ways to keep your immune system strong and working as effectively and efficiently as possible.
How Your Immune System Works

The immune system is a very complex system that protects your body in a variety of different ways. It not only fights off pathogens, like viruses and bacteria, that make you sick, but it also helps your body destroy harmful toxins and misbehaving cells like cancer cells.
Your immune system is made up of many different tissues, cells, and molecules that are spread all throughout your body. But in general, your immune system can be categorized into two main parts: the innate immune response and the adaptive immune response.
The Innate Immune Response

The first step of your body's immune response is often referred to as the “innate” immune response. This is a broad, generalized immune reaction that gets triggered whenever you are sick, injured, or your body detects pathogens or irritation.
The innate immune response is quick, and its goal is to destroy any bacteria, viruses, parasites, or other harmful pathogens that enter your body. It does so by mobilizing pathogen-destroying cells (called leukocytes) and triggering inflammation.
Inflammation causes changes in your body that allow your immune system to heal the injury more quickly. It also triggers reactions like fever, runny nose, coughing, and sneezing that help your body flush pathogens out of your body more quickly.
In some cases, your innate immune response can become over-sensitive and react to things that are not harmful, causing it to trigger the inflammatory response when it is not needed. This can lead to chronic inflammation, which is linked to a variety of chronic diseases, including heart disease and COPD.
One of the most important parts of the innate immune system is a category of cells called leukocytes, also known as white blood cells. Leukocytes are one of the most important parts of the immune system and they come in a variety of different types.

The primary responsibility of leukocytes is to track down and destroy all kinds of viruses, bacteria, and other pathogens, and each type of leukocyte has its own pathogen-hunting specialty. For example, phagocytes, which make up one category of leukocytes, kill pathogens by surrounding them and dissolving them with a cocktail of toxic chemicals.
Leukocytes lie in wait in many different places throughout your body, ready to spring into action as soon as they detect a pathogen to destroy. They can also travel around in your bloodstream, which allows them to quickly get to any place in the body where they are needed.
The Adaptive Immune Response

One of the most incredible talents of the immune system is its ability to learn and adapt to its environment. This is the job of the second main part of your immune system, the “adaptive” immune response.
Unlike the innate immune system, which fights pathogens in general, the adaptive immune system is responsible for tracking down and killing specific pathogens. It does this by creating antibodies whenever it encounters a new type of pathogen that it hasn't seen before.
Antibodies are molecules that can only stick to one specific type of pathogen, such as a specific type of virus or a particular bacteria species. When an antibody encounters the matching pathogen, it binds, or sticks, itself to the pathogen's surface.
This tag alerts leukocytes to the pathogen's presence and marks it for destruction. As a result, your immune system will recognize the pathogen much more quickly than it would if there were no antibodies around to help.
In this way, antibodies act as a sort of “memory” that allows your immune system to quickly identify viruses and bacteria that it has encountered before. This helps your immune system respond more rapidly and effectively to threats, reducing your chance of getting sick.
How COPD Affects Your Immune System
COPD has long been known to weaken the immune system and make patients more prone to disease. While researchers still do not fully understand why this happens, the link between COPD and poor immune system function is clear.
One reason for this is chronic inflammation, which afflicts the vast majority of patients with COPD. Studies show that chronic inflammation has a detrimental effect on the immune system, reducing its ability to fight disease.
Usually, inflammation triggers your immune system to act and neutralize whatever caused the inflammation. But in the case of chronic inflammation, your immune system overreacts when there is no real physical threat to neutralize.
As a result, the inflammation continues indefinitely and your immune system stays perpetually preoccupied with the imaginary threat. This unchecked inflammation puts a great deal of stress on your body (including your lungs) and makes your immune system less effective at countering real threats.
As the Cleveland Clinic puts it, “sustained, high levels of inflammation point to an overworked, over-tired immune system that can't properly protect you.” Unfortunately, chronic inflammation is a reality for the majority of people with COPD.
This has led some researchers to believe that COPD may be, at least in part, an autoimmune disease. An autoimmune disease is a disease that causes your body's immune system to mistakenly attack your body's own healthy cells.
The immune systems of people with COPD tend to overreact to minor irritants that you breathe in, causing inflammation in the lungs. Instead of attacking just the irritant, the immune system may end up attacking healthy lung tissue, resulting in permanent damage to the lungs that researchers believe may both cause and worsen COPD.
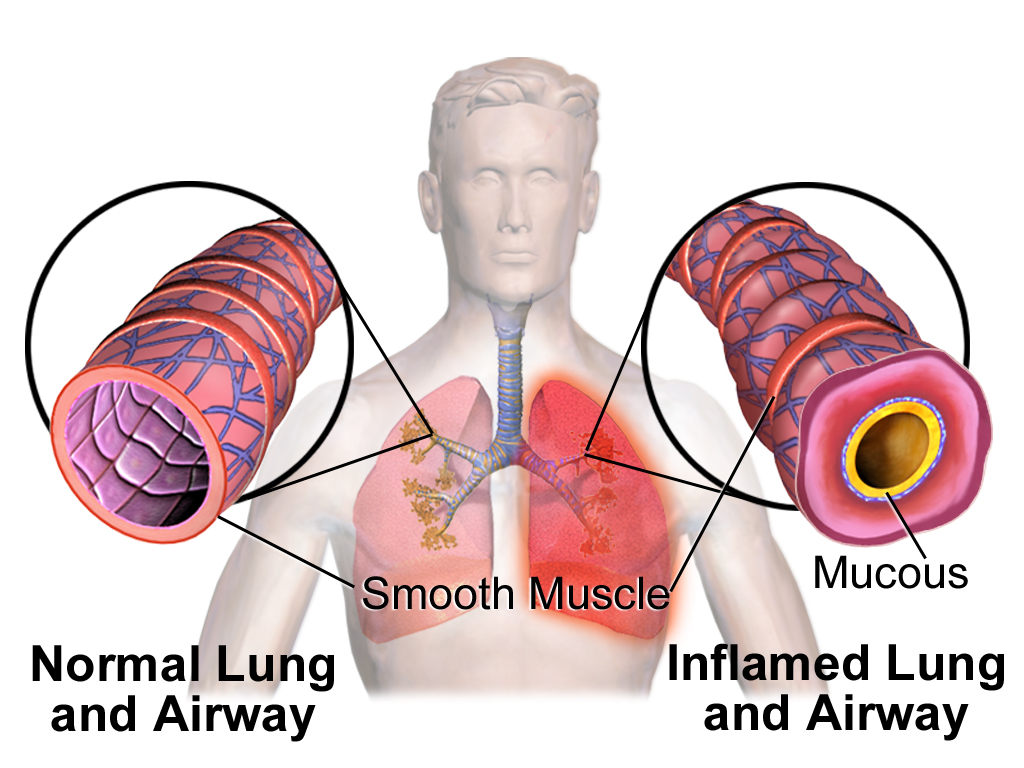
Chronic inflammation in the lungs can also make the lung tissue more susceptible to bacteria that cause respiratory illnesses and infections. Another problem is constant airway blockage from excess mucus and airway constriction, which makes it easier for infections to take hold in your lungs and airways.
It is also very common for COPD patients to suffer from anxiety, stress, and depression, which are known to weaken your immune system. COPD also impairs many patients ability to sleep, and lack of sleep is also linked to poor immune system function.
Other immune system problems faced by patients are indirectly caused by the symptoms of COPD itself. For instance, patients who get short of breath easily often struggle to keep up with healthy habits that are necessary for a healthy immune system, including exercising and eating a healthy diet.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
However, probably the most important reason that COPD patients have to take extra good care of their immune systems is to avoid COPD exacerbations. Exacerbations can be triggered by even mild illnesses and infections, and a healthy immune system is your first line of defense against getting sick.
Exacerbations make your COPD symptoms much worse and they can last for weeks or longer, which makes it very difficult to stay active and live a healthy lifestyle. Serious exacerbations can be even more devastating, causing permanent lung damage, sending you to the hospital, or even leading to respiratory failure and death.
Practical Tips You Can Use to Boost Your Immune System the Right Way
Because the immune system is so complex and varied, there is no one, definitive way to “boost” it. However, that doesn't mean that that your lifestyle and behaviors don't affect how your immune system works.
Lots of factors, including your nutrition, exercise habits, mental health, and more can have a significant effect on how efficiently your immune system functions. Luckily, that means that there are many things you can do in your daily life to keep your immune system healthy.
Stop Smoking

Smoking tobacco is bad for your immune system and makes your more prone to getting sick. Because most people who have COPD are smokers or former smokers, this is a common problem among COPD patients.
Smoking negatively affects the leukocytes in your body and suppresses your immune response. It also causes inflammation in your lungs that can make your COPD symptoms much worse.
Smoking also causes damage to other cells all throughout your body, which triggers a chronic state of inflammation. This inflammation increases your risk for infections, heart disease, and other serious health conditions.
However, if you quit smoking, your immune system can and will recover. If you have COPD and you still smoke, then it is absolutely imperative that you quit.
Quitting smoking is one of the best things you can do to improve your health and your overall quality of life with COPD. If you need help, visit the CDC's website to learn about a variety of quit smoking resources that can help you succeed.
It's never too late to stop smoking. Doing so will not only help your immune system, but it can also improve your COPD symptoms and prevent other serious diseases.
Don't Drink Too Much

While there's nothing wrong with a drink now and then, too much alcohol can hurt your immune system. It does this by suppressing the activity of leukocytes and reducing your immune system's ability to recognize and respond to threats.
Any kind of excessive drinking, including binge drinking and chronic alcohol use, can weaken your immune system. In fact, studies show that alcohol effects your immune system within twenty minutes of taking a drink, and that just one instance of binge drinking can significantly increase your risk for infection for days after you've sobered up.
This leaves your body more vulnerable to illnesses, infection, and other diseases like cancer. In combination with the already present immune-suppressing effects of COPD, excessive drinking can be particularly dangerous for COPD patients.
That's why, if you have COPD, you should be especially careful to avoid alcohol or at least drink in moderation. US guidelines for alcohol use recommend that you drink no more than seven standard drinks per week.
If you struggle with alcohol abuse or need help quitting or reducing your drinking, visit the Alcohol Rehab Guide to learn about a variety of resources that can help.
Stay Active

If you have COPD, then you know that staying active is important for keeping your heart and lungs healthy. However, physical activity is just as important for your immune system, as well.
Researchers aren't sure exactly why, but getting regular exercise improves your immune system's ability to fight off disease. One study showed that just twenty minutes of physical activity every day can reduce inflammation and help your immune system function more effectively.
Even though COPD can make exercise difficult, it's important to find some physical activities that you find engaging and fun. Even if you have to start small, you can improve your physical strength and endurance with time.
If you need help working out a feasible exercise plan, don't be afraid to ask your doctor for advice. If your COPD symptoms are preventing you from exercising, your doctor may be able to recommend another treatment, like pulmonary rehabilitation or supplemental oxygen, that can help you stay active.
Getting regular exercise can be as simple taking daily walks, bicycling, or doing aerobic exercises at home. For more tips on how to stay active with COPD, visit our guide to exercising at home with COPD here.
Vaccination
Vaccination is the only targeted treatment scientists have found that can reliably and significantly boost the immune system on its own. That's why doctors often urge COPD patients to get vaccinated as a first line of defense against illnesses like the flu and pneumonia.
Vaccines work by exposing your body to a tiny amount of a disease-causing pathogen that has been weakened or killed. The vaccine doesn't contain enough of the pathogen to get you sick, but it contains just enough for your immune system to recognize it and respond.
Your immune system reacts to the vaccine by making specific antibodies that target the pathogen in the vaccine. Then, if you are ever exposed to the pathogen in the future, your immune system will be primed and ready to destroy it before it has a chance to get you sick.
Here are the vaccines typically recommended for people with COPD:
- The Influenza Vaccine: Get vaccinated every year to protect yourself before flu season.
- Td Vaccine: Get vaccinated once every ten years to protect yourself from tetanus.
- Pneumococcal Vaccine: Get vaccinated once before the age of 65, and then twice again after the age of 65 to protect yourself from bacterial pneumonia
If you are not sure if you are up to date on these or any other vaccines, talk to your doctor. He can review your records and tell you what vaccines could be beneficial for you.
Reduce Stress
Chronic stress and other mental disorders like depression are well-known triggers for inflammation and immune system distress. Because of this, keeping stress at a minimum and treating anxiety and depression are important for keeping your immune system in good shape.
For instance, a variety of studies have found that people who experience chronic stress are more likely to contract a common cold. Chronic stress can also reduce your body's ability to heal itself, fight cancer, and gain immunity from vaccines.
Depression has also been linked to chronic inflammation and reduced immune system function. While researchers are still trying to understand exactly why this happens, they do have some idea of how it works.
Stress increases the amount of a “stress chemical” known as cortisol, which triggers inflammation. It also reduces the number of leukocytes in your body, making it harder for your immune system to fight off disease.
Unfortunately, chronic stress, anxiety, and depression are very common among people with COPD. Fortunately, there are many different things you can do to reduce your stress, treat depression, and improve your mental and emotional health.
Check out these guides for managing stress, anxiety, and depression:
- How to Treat Depression When You Have COPD
- How to Treat Anxiety and Panic Attacks When You Have COPD
Get Good Sleep
Sleep is an incredibly undervalued activity in the modern world. Despite the fact that it's necessary for survival, many people don't sleep enough and don't understand the importance of high quality sleep.
Many studies have shown that you are more likely to get sick when you don't get proper sleep. Being sleep deprived can also hamper your ability to recover from illnesses and infections, causing you to stay sick for longer.
Poor sleep has particularly serious consequences for people with COPD and can significantly increase their chances of experiencing a COPD exacerbation. Some studies have also found that sleep deprivation significantly impairs COPD patients' ability to breathe.
That's why it's so important to make sleep an important priority in your life. Most adults need at least 7-8 hours every single night, and any less can significantly affect your quality of life.
Unfortunately, COPD patients in particular often struggle to sleep because of their disease. This is partially because many COPD symptoms, including breathlessness, airway blockage, and chest discomfort, get worse for many patients in bed at night.
Fortunately, there are many things you can do to improve your sleep quality and your ability to fall sleep at night. It's all about establishing a consistent, relaxing nighttime routine and making sure you have a comfortable sleeping environment.
Here are some tips for improving your sleep when you have COPD:

Beside oxygen therapy, and utilizing a portable oxygen concentrator, people with COPD are left with few other options to explore that would potentially add years to their lives. Studies have shown that hypoxic patients’s respiratory health improves greatly from long-term oxygen therapy but a viable treatment beyond oxygen therapy, still must be explored.
There is a lot of research being done right now that is dedicated to new treatment methods for COPD. COPD is the fourth leading cause of death in adults in the United States, and over 16 million Americans are diagnosed with COPD currently. This disease is preventable, but once you have COPD, you have the disease for life. There are, however, actionable ways to control COPD and the symptoms involved, but it requires diligence and attention to your treatment plan that you have set up with your health care team.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Beyond the common treatments for COPD such as, long-term oxygen therapy, medication, exercise, diet, it is possible that you will still feel unwell and incapable of doing things you once loved to do.
This is very common among COPD patients, and it can lead to mental health disorders like depression and anxiety.
![]()
Avoiding further degradation of your respiratory health and overall well being is essential if you want to live a long and happy life with COPD.
In this blog, we summarize a lot of the research being done that can help you treat your COPD even further, either through surgery, new and innovative medications, and other treatments.
New Respiratory Drug Discoveries
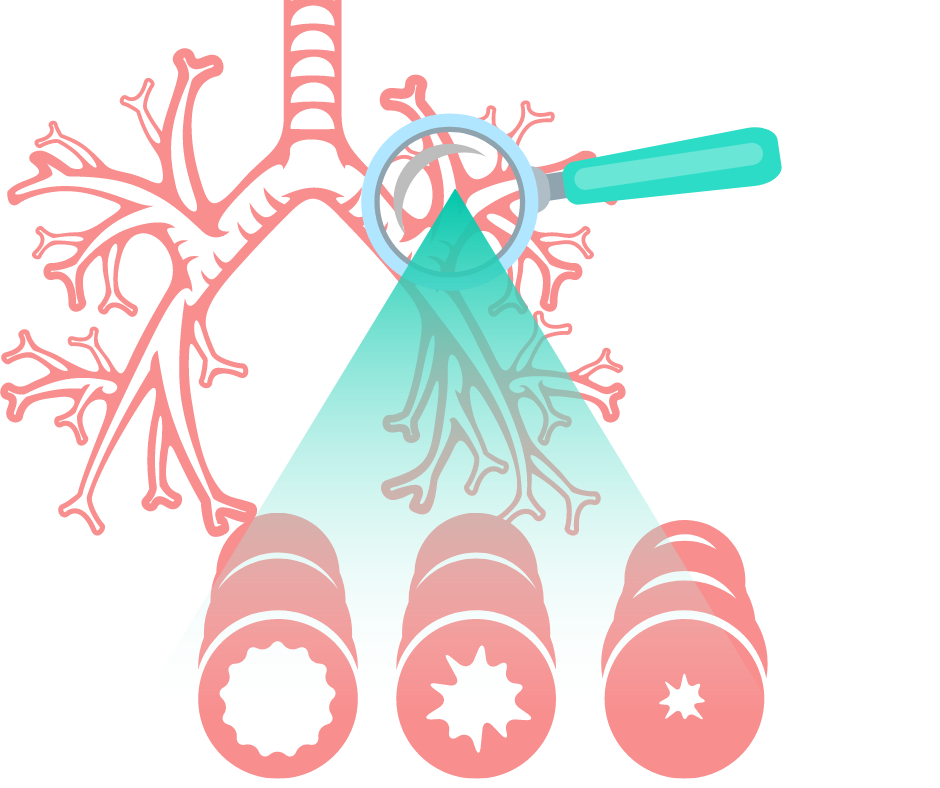
Currently, Only about 50 percent of asthma patients, and an even lower percentage of people with COPD, suffer from lung inflammation and cannot open up their restricted airways even with the help of readily available medications. It is evident that there is still a lot of work to be done to develop medications that can help all people with obstructive respiratory diseases breathe better.
Medication - TASR5 Bitter Taste Receptor for COPD Patients 2021

If you have asthma or COPD, the tightening of smooth muscles surrounding your bronchial tubes narrows your airway and reduces air flow, this is often why you cannot breathe well. Dr Liggett's lab has discovered a TASR5 bitter taste receptor that can open your airway when activated. This is a promising new study that has paved the road for looking into new drugs to treat asthma and other obstructive lung diseases.
This new medication targets smooth muscle to open up constricted airways.
The medication is a promising bronchodilator agonist that shows a lot of potential in treating respiratory diseases. In the preclinical study, this new bronchodilator was 1,000 times more potent than some of the other agents that were tested.

The goals of this new mediation are to find a more potent agent that will activate this smooth muscle receptor and for it to accurately deliver the potencies by inhalation. T5-8 was the bronchodilator agent that showed the most promise.
Luckily, there were others options that worked well too, so there are multiple potential new drugs to carry out the next steps!
Zephyr Valve for COPD Patients in 2021

It is likely that your lung disease will begin to advance into a more severe state as you get older, even with proper treatment. Once your disease begins to get in the way of taking care of business the way you are used to, it is time that you do something.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
If you have chronic obstructive pulmonary disease (COPD), but noticed it getting worse over the past few years, it can easily begin to get in the way and you will be unable to do the things you love.
Things like attending family events, hobbies like golfing, or taking care of the house can soon become unattainable and sound impossible.

COPD affects 16 million people, and is the fourth leading cause of death in the United States.. The main symptoms, including chronic cough, fatigue, and shortness of breath, secondary symptoms include, mood swings, fatigue, and mental health issues all of which tend to worsen over time.
There is still no cure for COPD, but there are drugs and therapies readily available to treat these symptoms, however they are not always potent enough. Treatments include pulmonary rehabilitation, bronchodilators and corticosteroids, and lung volume reduction surgery help many people living with COPD.
A new option called the Zephyr Valve, which was FDA approved in 2018, is offering hope for people who suffer from COPD in an advanced state. The Zephyr Valve is designed for patients with advanced COPD, who’s breathlessness at rest or with activity is extremely high, and even with optimal medical treatment, they still suffer from significant hyperinflation and air trapping due to deterioration of lung tissue.
Another not so commonly noted problem with the way COPD affects patients is how the lungs become bigger, or hyperinflated. Shortness of breath and uncomfortable gastrointestinal symptoms are the result of overinflated lungs pressing down on the diaphragm.
The valves in the Zephyr Valvae are extremely small, they work by being implemented into the ‘bad’ diseased parts of the lung, in order to block the air from going into those sections. As a result, the non-diseased portion of the lung can expand and relieve the pressure on the diaphragm, allowing patients to breathe better.
If you treat your COPD properly- take your medications, adhere to your oxygen prescription, exercise and eat properly, and still your disease progresses past a certain degree, your pulmonologist may suggest you look into the Zephyr Valve placement.

If you qualify, there is no guarantee you’ll be completely better and feeling 100% all of the time, but there is overwhelming hope that you’ll have a better quality of life. You can get back to doing what you love or enjoying the simple things, will you still get tired? Yes, because you still have COPD. But the progress towards a happier more active life is a pursuit you can begin on!
Stem Cell Therapy for COPD in 2021
![]()
There is potential to help patients with COPD by using Mesenchymal Stem Cells. Stem cells work by promoting healing and regenerating, they do this by creating extra messenger cells called "cytokines".
Stem cells are amazingly unique, and they are capable of changing into any cell in the body. Once they are inserted, they can find damaged tissues around organs and rejerate new healthy cells within those organs. In your case, as a respiratory disease patient, it is your lungs that are deteriorating and damaged, and so stem cells can repair damaged lung tissue to combat emphysema or chronic bronchitis.
While stem cells rebuild healthy cells, they also have natural anti-inflammatory properties that can clear your airways as well.

Studies have shown the results of stem cell therapy and its effects on COPD. Over 82% of COPD patients that have tried stem cell treatment have significant improvements in their quality of life after their therapies.
The positive reported impacts stem cell therapy after transfusion are increased lung capacity and the ability to walk. These reports have highlighted stem cells' ability to be viable options for current patients with COPD.

And while stem cell treatment still will not cure COPD, it is able to repair damaged lung tissue and it being a relatively noninvasive procedure compared to other options, stem cell therapy is an attractive alternative for COPD patients. Studies have shown that certain cells- expanded cord tissue-derived mesenchymal cells- have very high anti-inflammatory properties and tissue regeneration capabilities, that are perfect for patients with COPD.
Cost of Stem cell therapy for COPD
The most affordable option for COPD patients is to find patient-funded clinical trials. COPD patients who get stem cell therapy can pay anywhere from $10000 - $35,000.
While you are researching stem cell clinics for COPD, be sure to find out how many cells are included in the treatment protocol, and what type of cells you would be receiving.
Currently, Medicare does not cover the cost of stem cell therapy for COPD.

Currently Available Treatments for COPD
New medications such as the TASR5 bitter taste receptor to treat COPD are not yet available for COPD patients, and the Zephyr Valve and Stem Cell Therapy may be out of your price range or you simply do not qualify for those treatments based on the current state of your disease.
Other more common treatments for chronic respiratory disease go a long way in cultivating a healthy lifestyle and improvements in your wellbeing.
Supplemental Oxygen Therapy

Oxygen therapy is among the most effective treatments there will ever be for COPD and patients with chronic hypoxia.
Supplemental oxygen therapy should be administered at least 15 hours a day, and for the best results, 24 hours per day, but this depends on your doctor’s recommendations and the prescription they will base upon your spirometry test results.
You will get your supplemental oxygen therapy administered with an oxygen device that you will bring with you everywhere you go. Having the best oxygen equipment will help you live a high quality life while getting the oxygen saturation your body needs to survive.

Portable oxygen devices are a great option for people who value the ability to exercise, run errands, and get out and about rather than spending a lot of time at home!
The best portable oxygen devices are called portable oxygen concentrators and they are the most efficient because they are battery powered oxygen devices so you can take them on airplanes, they are lightweight, and it extracts air from its surroundings so you never have to get them refilled with oxygen.
Pulmonary Rehabilitation

The goal of pulmonary rehabilitation is to rebuild strength so you can start to enjoy a more full and active life. These programs are set up to improve your lung function, reduce the symptoms you experience, and improve quality of life.
The courses are a mixture of educational classes and physical exercises that will increase your awareness about your lungs and your disease.
Your pulmonary rehab team is a team of doctors, nurses, physical therapists, respiratory therapists, exercise specialists and dietitians. With all of their help and expertise, you will develop a unique program that meets your specific needs.

Overview
As a company that works with respiratory patients on a daily basis LPT Medical has readily available reading material that will help answer all of your questions about your respiratory illness, how to treat it, and everything else you may want to know, just visit our respiratory resource center page.

This is not the end of COPD research in fact, it is the beginning. New and innovative mediations, procedures, and other respiratory devices will become available in 2021 and beyond that will help you breathe easier, and reduce the symptoms you experience from COPD.
Watch this space, and be sure to like LPT Medical on Facebook, subscribe to our newsletter, and comment on this blog because we are always posting news and information about respiratory illnesses, and learning about your disease is as important as treating it everyday.
.png)
In the 21st century, we are highly dependent on energy sources like natural gas and electricity. We use fuel to power our cars, cook and heat our homes, and we use electricity to charge our phones, computers, and more. But what happens when we lose access to these resources due to a natural disaster or some other problem? In some situations, this can be a minor nuisance; but in others, it could be life-threatening.
Fortunately, hospitals and other medical facilities have back-up generators that allow them to use life-saving medical equipment even in the event of a power outage. But what about individuals living at home who are reliant on electronic devices? What safety measures are in place to ensure these people are able to use the medical devices they need to stay healthy?
The truth is that there aren’t many safety nets in place to help people experiencing power outages, so this is why it’s always important to be prepared, especially if you depend on electricity to power your medical equipment. In this post, we are going to highlight all the steps you should take to be prepared for a power outage if you have COPD or any other chronic respiratory disease.
What Causes Power Outages?
Before we can discuss the different ways to plan for power outages, it’s important to understand what actually causes them. According to the U.S. Energy Information Administration, the average household experienced one outage in 2016, accounting for 112 minutes of lost power. Although this is the average, this does not mean that power outages cannot last longer. Depending on what causes the power outage, they could last anywhere between several days and several weeks. So you should always plan for the worst-case scenario.

According to Constellation, the most common cause of power outages are severe weather and natural disasters. High winds, snowstorms, and thunderstorms can all knock power lines over causing entire neighborhoods to lose power. Extreme temperatures can also lead to power outages if it results in people overusing their air conditioners or heaters. There are so many different variables that come into play, so it’s best to always be prepared for an outage, regardless of the time of year and what the weather is like.
Install an Emergency Power System
The first thing you should do to prepare for power outages is to have an emergency power system in your home. There are many different options for powering your home in the event of an emergency, so you will have to do a lot of research to determine which one will best meet your needs. However, a good place to start is by contacting your utility company. Some utility companies provide backup generators for people with medical conditions free-of-charge. Others may add an additional fee to your monthly utility bills. Below are some of the most widely used emergency power supplies:
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Home Backup Generators
A home backup generator, also known as a standby generator, is a permanent power generator that is installed outside of your home. These generators resemble air conditioning units and they run off of your existing natural gas or LP fuel supply. While home backup generators are the most costly option for backup power, they are also the most convenient and reliable. These units are designed to turn on automatically when a power outage is detected, so you won’t have to go outside to turn it on. Since these generators are permanent, they will give your home’s value a nice boost if you ever decide to sell it. As you can imagine, home backup generators are extremely advanced, so you will need to hire a professional to install one for you.

Portable Generators
A portable generator, also known as a recreational generator, is a type of generator that’s commonly used for camping and other outdoor activities. However, they can also be a good way to power your home during a power outage. Unfortunately, these devices don’t start automatically when your power goes out, so you’ll have to go through the hassle of setting it up when your power goes out. What’s more, these units use fossil fuels which can exacerbate your respiratory symptoms, so be sure to never use one inside of your home. The benefit of portable generators is that they are much more affordable than home generators.

Solar Generators
Just like the name suggests, solar generators are powered by the sun. The only scenario where you should purchase a solar generator is if you live in an area that is very sunny to ensure that your generator is fully charged when you need it most. Since these generators don’t burn any fuel, they won’t exacerbate your lung symptoms and they aren’t noisy. Solar generators are fairly expensive but they are worth the price for many people.
Install a Medical Alert System
An emergency alert system is a device designed to alert medical professionals if you experience a medical emergency like a COPD exacerbation or a fall. Each medical alert system comes with a pendant that you wear around your neck and a receiver that plugs into the wall. In the event of an emergency, press the button on the pendant and an ambulance will be dispatched to your home.

What many people don’t know is that many medical alert systems have backup batteries that will kick in if there is a power outage. Generally speaking, most backup batteries will last a day or two, but you should speak with the company that manufactures it to learn the full details. Medical alert systems are an invaluable tool to have when the power goes out so be sure to get one installed as soon as possible.
![]()
Another way to prevent falls when the power goes out is to have a flashlight on hand. Chances are, even if you have a generator in your home, you’re going to want to conserve energy by keeping as many lights off as possible. A flashlight will help you navigate your home safely while doing so.
Keep Backup Batteries or Oxygen Tanks
COPD patients have a variety of options at their disposal when it comes to medical oxygen. Some of the most popular options include oxygen tanks, liquid oxygen tanks, and oxygen concentrators. The one you choose as your “backup” oxygen supply in the event of a power outage will depend on what your needs are.

The most notable benefit of having backup oxygen tanks is that they don’t require electricity in order to operate. Oxygen tanks have compressed oxygen inside them, so all you need to do is connect your nasal cannula and you’ll have access to medical-grade oxygen. However, the downsides of oxygen tanks are that they are very heavy and bulky so you won’t be able to get around your home while you’re using one.
Liquid oxygen tanks work a little differently than normal oxygen tanks. Rather than storing the oxygen as a gas, these tanks store oxygen as a liquid. Since gas is expanded, storing it as a liquid allows you to carry more of it with the same size and weight tank. This will allow you more freedom in the event of a power outage. However, there is one glaring flaw with liquid oxygen tanks which makes them impossible to recommend for this situation. Oxygen needs to be stored at very low temperatures in order to stay as a liquid, so over time liquid oxygen will begin to evaporate, According to the Lung Institute, liquid oxygen will evaporate in a week or two depending on the type of tank you have.
.png)
Last but certainly not least there are oxygen concentrators. Unlike the previous two oxygen devices, concentrators are electronic devices. They work by drawing in ambient air and putting out medical-grade oxygen. It may seem silly to use an electronic oxygen device during a power outage, but you may be surprised to find that they are actually the best backup oxygen device for this situation. Portable oxygen concentrators run off detachable batteries that can be stored for emergencies.

These batteries are also very small and only weigh about a pound so you can store as many as you’d like. One important thing to note is that batteries should be used from time to time in order to help them keep their charge. Be sure to swap out the batteries occasionally so that each one is being used. Let’s take a look at some of the best portable oxygen concentrators to have during a power outage.
Best Oxygen Concentrators for a Power Outage
The Caire FreeStyle Comfort
The FreeStyle Comfort is currently one of the most popular portable oxygen generators on the market. It’s a pulse dose portable oxygen concentrator meaning it has built-in technology that tracks your breathing and only delivers oxygen when you inhale through the nasal cannula. What this means is that it’s able to conserve electricity while still giving you the oxygen you need to stay healthy. With the larger 16-cell battery, the FreeStyle Comfort can run for up to 16 hours on one charge.

The FreeStyle Comfort is one of only a few portable oxygen concentrators that weigh at or under 5 pounds. Additionally, it’s one of the most compact concentrators so you can carry it around on your shoulder with ease. In the event of a power outage, the FreeStyle Comfort will provide you with plenty of battery life, ease-of-use, and mobility. It has a maximum oxygen output of 1,050 milliliters per minute (ml/min).
The Inogen One G5
The Inogen G5 is another pulse dose portable oxygen concentrator under 5 pounds. With the 8-cell battery, the G5 weighs only 4.7 and has a battery duration of 6 ½ hours. The battery life can be doubled with the 16-cell battery affording you up to 13 hours of battery life on one charge. Just like with the FreeStyle Comfort, the batteries are very small and lightweight so you can store as many as you think you’ll need to make it through a power outage.
.png)
One of the great things about the Inogen G5 is the number of accessories there are for it. The G5 external battery charger is very useful if you’re planning for a power outage because it allows you to charge one battery separate from the G5 unit itself. In other words, it allows you to charge your batteries more quickly so that you can always be prepared. Another great accessory to have during a power outage is the DC charging cable. This is a type of cable that allows you to charge your G5 in the car via a cigarette outlet. Keep a DC charging cable in your car so that you’re always prepared if you need to leave the house in a hurry. The best part about this is that you can use your device while it’s charging meaning there will never be an interruption in your oxygen treatment.
The Respironics SimplyGo
The last portable oxygen concentrator we’d like to recommend for power outages is the Respironics SimplyGo. Certain patients are prescribed continuous flow oxygen which is where oxygen is administered irrespective of the user’s breathing rate. When this is the case, the SimplyGo is the lightest and most reliable unit available to you. The SimplyGo has a maximum flow rate of 2 liters per minute (LPM) at it weighs only 10 pounds which is significantly lighter than most continuous flow POCs on the market. Unfortunately, the SimplyGo offers significantly less battery life than the aforementioned POCs, so you may need to keep even more batteries charged.

Create a List of Contacts
Having a convenient list of contacts you can call during a power outage is very important. You don’t want to be searching the internet using what little electricity you have to find out the number of your utility company or your neighbor’s phone number. Take some time right now to write down your contacts so that you don’t have to do it when an emergency occurs.

Firstly, you should write down the numbers of a couple of friends or family members who could come pick you up if your power is out. Secondly, you should have your doctor or pulmonologist’s number as well as the closest medical oxygen company. If you happen to run out of oxygen for one reason or another you can reach out to them and have them deliver some oxygen tanks. Lastly, don’t forget to write down the number of your utility company. Be sure to call them immediately when the power goes out so that you can plan accordingly.
Keep Non-Perishable Food in Your Home
One of the most notorious issues with power outages is that all of the food in your fridge will begin to spoil. This can be absolutely devastating if you like to keep your fridge well-stocked with lots of food and beverages. It’s a good idea to get in the habit of buying healthy non-perishable food at the grocery store that can hold you over if you experience a power outage. Apples are a great source of energy and they will stay fresh for up to a week while sitting on the counter. However, be sure to ask your doctor about non-perishable foods that are healthy for COPD patients.
.jpg)
Speak With Your Doctor
Last but certainly not least, you can and should speak with your doctor about managing your COPD during a power outage. Your doctor might have some helpful information or resources for you to refer to. Most likely, he/she will tell you the minimum flow rate you’re allowed to use on your oxygen tank or concentrator in order to maintain your blood oxygen levels. Also, be sure to ask your doctor if it’s okay to cease your pulmonary rehabilitation routine while the power is out so that you can conserve your oxygen supply.

Conclusion
While it’s rare to experience a power outage that lasts more than a couple of hours, it’s crucial that you are prepared for the worst-case scenario. Studies have shown that power outages are associated with a greater risk of exacerbation and hospitalization in COPD patients. Ensuring that you always have access to a dependable medical oxygen supply will help you to stabilize your respiratory condition.
What’s more, you should work together with your doctor to create a power outage action plan. You may be able to reduce your oxygen flow rate in order to conserve your oxygen concentrator battery life during a prolonged power outage. And ideally, you’ll have some sort of backup generator that you can use to hold you over until the electricity returns to your home.
Here at LPT Medical, we can help you prepare for power outages by providing you with a durable and reliable portable oxygen concentrator like the Caire FreeStyle Comfort or the Inogen One G5. While we can’t guarantee that your battery will last the duration of the outage, we can help you find the best concentrator for your needs. Please don’t hesitate to reach out to us either by email or by phone.

According to a company press release, officials with the Food and Drug Administration (FDA) have approved Trelegy Ellipta, a once-daily, triple therapy, fluticasone furoate/umeclidinum/vilanterol (FF/UMEC/VI) for the long-term maintenance treatment of patients diagnosed with Chronic Obstructive Pulmonary Disease (COPD).
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
It is the first product to have been approved in the United States that has a combination of three active molecules in a single-dose inhaler, and to be taken once every day for the treatment of COPD including chronic bronchitis and emphysema. The press announcement came from GlaxoSmithKline (GSK) and Innoviva Inc. saying that the drugs will be available to patients soon.
The triple therapy manufactured by GSK is approved for COPD patients on a fixed-dose combination of fluticasone furoate and vilanterol for airflow obstruction. It is also approved for patients that are already taking umeclidinum and a fixed-dose combination of vilanterol and fluticasone furoate. GSK and Innoviva noted that it was not indicated for treatment of asthma or the relief of acute bronchospasm.
Trelegy Ellipta consists of a combination of an inhaled corticosteroid (ICS), a long-acting muscarinic antagonist (LAMA), and a long-acting beta2 adrenergic agonist (LABA) to be delivered orally, once-daily, through GSK’s Ellipta dry powder inhaler. The strength which has been approved is FF/UMEC/VI 100/62.5/25 mcg.

GSK estimates that approximately one quarter of patients diagnosed with COPD already use the three drugs in Trelegy Ellipta individually to treat COPD and hopes that this product will prove to be an attractive and simpler alternative regimen for such patients.
A positive opinion recommending the marketing authorization for the medication as a maintenance treatment in appropriate adults with COPD in its moderate to severe stages was issued by the European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CMPH) on the 15th of September, 2017.
The CEO of Innoviva Inc., Mike Aguair, said, “This approval represents a significant therapeutic convenience for those appropriate patients already on Breo Ellipta, that require additional bronchodilation or for those patients already on a combination of Breo Ellipta and Incruse Ellipta. Trelegy Ellipta is the latest development in our collaboration with GSK and is testament to our ongoing efforts to advance respiratory medicine.”
Eric Dube, SVP & Head, GSK Global Franchise, said, “COPD is a progressive disease that can worsen over time and represents a significant burden to patients and healthcare systems. The approval of Trelegy Ellipta, and the addition of a once-daily single inhaler triple therapy to our portfolio of respiratory medicines, is an important milestone for the GSK that builds on our long term heritage in this area.”
There has been submission of regulatory applications which are being assessed in a number of other countries including Canada, Australia and the European Union. Trelegy Ellipta will be available very soon in the United States; it is however not licensed as a single inhaler triple therapy anywhere else apart from the United States.
What is COPD?
COPD is a chronic condition in which there is slow, progressive obstruction of airflow into or out of the lungs. It is mainly characterized by shortness of breath. It includes emphysema and chronic bronchitis which can also occur at the same time. It is believed to affect close to 384 million people in the whole world and about 30 million people in the United States alone.
It is a progressive disease which means that it gets worse over time. Life can become very difficult when you are living with COPD due to the worsening of your symptoms and lack of ability to breathe normally. This can devastate your life making simple day to day tasks such as walking up a flight of stairs to your house a daunting task. It ends up affecting your life quality because there are some activities that you may not be able to carry out over time.
Exposure to lung irritants for a long period of time damages your lungs and your airways and may cause COPD. Air pollution, presence of dust in your environment, cigarette smoke as well as second-hand smoking, and chemical fumes can all be contributors to COPD. Most of the people diagnosed with COPD are at least 40 years old when they symptoms start to show.
Symptoms may include having a chronic cough, production of a lot more mucus than usual, having a blue color on your nail beds and lips and wheezing among many others. Seek medical attention should you experience any of these to be checked for COPD.
Important Safety Information for Trelegy Ellipta

The following is based on the highlights section of the United States Prescribing Information for Trelegy Ellipta:
-
It is contraindicated in patients with severe hypersensitivity to milk proteins or any of its ingredients.
-
Its safety and efficacy in patients with asthma has not been established. It is not indicated for the treatment of asthma.
-
Because of risk of overdose, it should not be used in combination with other medicines containing LABA.
-
It should not be initiated in patients experiencing episodes of acutely deteriorating COPD. Do not use to treat acute symptoms.
-
Candida albicans infection of the pharynx and the mouth has occurred in patients treated with fluticasone furoate which is one of the three components contained in Trelegy Ellipta. Patients should be monitored periodically and advised to rinse their mouth with water without swallowing after inhalation to reduce risk.
-
Patients that use corticosteroids are at risk of potentially worsening of infections that they have. For example existing tuberculosis and bacterial, fungal or viral infections and should be used with caution in patients that have such infections.
-
Increased risk of pneumonia in COPD patients taking Trelegy Ellipta. Patients taking it should be monitored for signs and symptoms of pneumonia.
-
Trelegy Ellipta should be used with caution in patients with cardiovascular disorders because of beta-adrenergic stimulation.
- Hypercortism and adrenal suppression may occur with very high dosages. They may also occur at the regular dosage with susceptible individuals. Appropriate therapy should be considered if such changes occur.
The most common adverse reactions reported for Trelegy Ellipta (incidences less than or equal to 1 percent) are; dysgeusia, cough, headache, gastroenteritis, back pains, diarrhea and oropharyngeal pain.

Researchers have found that there is a treatment in existence which could help patients with a particular kind of Chronic Obstructive Pulmonary Disease (COPD). This antibody treatment is said to reduce the rate of flare-ups by close to 20 percent in patients with a sub group of treatment-resistant COPD, according to the results of two large international trials presented at the European Respiratory Society International Congress in Milan, Italy and simultaneously published in the New England Journal of Medicine.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
“The goal of precision medicine is to give the patient the right treatment,” said lead author Frank Sciurba, the director of the Center for COPD and Emphysema and University of Pittsburgh Medical Center’s Pulmonary Function Exercise Physiology Laboratory, and a visiting professor in the Division of Pulmonary, Allergy and Critical Care Medicine at the university’s School of Medicine. “These findings are the first example of a precision therapy that is uniquely effective in a sub group of patients with treatment-resistant COPD.”
COPD is a progressive lung disease that causes breathlessness as a result of airway obstruction and chronic inflammation that is believed to affect 30 million Americans. More than 12 million Americans are believed to have undiagnosed COPD and have no idea that they do. COPD is the third leading cause of death in America claiming approximately 120,000 lives every year.

There are a number of signs you can look out for should you suspect that you have COPD and these include; having a chronic cough, production of a lot of mucus, blueness of your fingernail beds and lips, fatigue, lack of energy and chest tightness among a number of other signs. Should you experience any of these signs while going about your day to day activities, you are advised to visit your health provider so that they can perform a spirometry test to check whether you do have COPD.
“There is significant variation between patients in the cells and other proteins responsible for lung inflammation, so there are actually many different subtypes of COPD”, Sciurba said.
One subgroup called eosinophilic predominant COPD is present in as many as 40 percent of patients and is characterized by elevated levels of a type of white blood cells known as eosinophils, he said.
The new study reports the outcomes of two Phase III clinical trials assessing the effectiveness of mepolizumab, an antibody treatments that brings down the number of eosinophils in the blood, in moderate to severe treatment-resistant eosinophilic COPD by blocking the pro-inflammatory results of interleukin-5. Despite a year of standard treatment known as “triple inhaled therapy” which includes the use of bronchodilators and glucocorticoids, patients included in the trials were still experiencing flare-ups.
Sciurba said that these patients already have been given every treatment that they have to offer them and are still having flare-ups that significantly interfere with their quality of life and can lead to deterioration in lung function and higher mortality. He added that they hoped to be able to offer them an option.

The Food and Drug Administration (FDA) have already approved mepolizumab to help reduce symptom flare-ups and improve life quality in eosinophilic asthma.
The first trial which was conducted from the year 2014 to the year 2017 was conducted at 117 sites in 15 countries and was termed METREX. It involved a total number of 837 patients diagnosed with COPD, who were stratified by blood eosinophil counts and randomized to receive either placebo or 100 milligrams of mepolizumab which was delivered under the skin on a monthly basis for a year.
The patients with high eosinophil counts that were receiving doses of mepolizumab had a statistically significant 18 percent lower rate of moderate or severe flare-ups (1.4 per year compared to 1.7 per year) than those that were in the group receiving doses of placebo. The exacerbation rate of the patients with low eosinophil counts treated with the biologic did not differ from the placebo. The time to the first exacerbation also was lower with placebo than mepolizumab, but only in the group with the high eosinophil count.
In a second trial that was done concurrently, the team made an assessment of the effect of a higher dose of mepolizumab in 675 patients with elevated eosinophil levels. This second trial was termed METREO. Patients were selected at random in the trial to receive 100 to 300 milligrams of mepolizumab or placebo with the same schedule and delivery method as that of METREX.

Similar to the first trial, METREX, the findings of the second trial showed that the rate of the flare-ups was reduced by 20 percent in the group with a high eosinophil count after 100 milligrams of mepolizumab. The METREO outcome narrowly missed statistical significance. There was however no advantage showed of the 300 milligram dose over the lower dose.
Through analyzing data from both the METREO and METREX trials, it was found that as baseline blood eosinophil counts increased, it also had the same effect on mepolizumab’s reduction in the annual exacerbation rate. Sciurba said that these findings indicated that patients with a higher initial eosinophil count benefited more than those with lower eosinophil counts. There was no difference in the safety profile between placebo and mepolizumab in either trial.
“In addition to providing a new treatment option for patients with treatment-resistant moderate to severe COPD, the results are also important because they identify a potential biomarker for the disease and demonstrate that eosinophilic inflammation plays a role in flare-ups in COPD,” Sciurba said.
The division chief of the Division of Pulmonary, Allergy, and Critical Care Medicine Dr. Rama K. Mallampalli said, “The findings in these trials exemplify what we hope to achieve not only in COPD but across all lung diseases with regards to a precision approach to treatment.”
GlaxoSmithKline, a British pharmaceutical company established in 2000 through the merging of two companies, Glaxo Wellcome and Smithkline Beecham provided the funding for both the first and the second trials that were conducted. They plan to seek approval from the FDA for the use of mepolizumab in eosinophilic COPD.
If you have COPD, the first sign that something was not right was likely feeling shortness of breath, to the point that you wanted to see your doctor about it. It also could have been that incessant cough throughout the day and night.
It's easy to blame a cough on allergies or a common cold, but if it persists and becomes a regular thing, you should see your doctor to discuss the possibility of having COPD or another lung ailment. The sooner you find out if it is COPD causing your symptoms the sooner you will be able to treat the chronic illness, thereby slowing down the progression of your COPD.
The first thing that you need to understand is that coughing may seem like a symptom you want to relieve, but in the case of COPD, it actually serves a function.
Continue reading to understand how COPD and coughing are related, what you can do to ease a cough, and when to seek medical attention.
How are COPD and coughing related
If you have COPD you probably experience a persistent cough. This symptom is related to a condition of COPD called chronic bronchitis, which means that your airways are constantly irritated. This irritation is often caused by smoking or second-hand smoke, but it can also be caused by other irritants and biological factors, such as pollution or genetics.
The irritation in your airways causes two problems that prevent enough air from passing through to the lungs:
- The lining of your airways become swollen
- There is too much mucus produced by your lungs
People with chronic bronchitis can have a persistent cough because it is important to regularly clear their swollen airways of this excess mucus, which can sometimes be difficult and require extra attention and treatments, of which, we will discuss in more detail in the What you can do to ease a cough associated with COPD section of this article.
So, coughing caused by COPD is often productive and it is a natural function of your body that plays an important role in your breathing system. Coughing helps to move extra mucus out from your lungs. Coughing is also a reaction that can help remove certain irritants you may inhale into your lungs, like dust, pollution, and other common allergens.
When your cough produces mucus, which is also called sputum or phlegm, that means your body is working correctly to clear the excess mucus up through your swollen airways and into your throat and out of your mouth.
It is normal for the mucus to be clear or white, yellow, or green in color but if the mucus is very mucky, it may be a sign of a respiratory infection. We will go over this in more detail in the When you should see a doctor section
What you can do to ease a cough associated with COPD
To determine whether or not your cough needs to be treated with medication or other remedies, depends on the type of cough you are experiencing and whether or not your cough is actually helping to clear your lungs and airways.
You should consult with your doctor to determine the type of cough you are experiencing and how to deal with it going forward.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
As we discussed in the section above, airway clearing coughs serves a meaningful purpose by clearing out mucus from your airways. In this case, it is best for you to continue coughing in order to avoid mucus building up in your lungs.
.png)
That being said, there are certain medications you can take as well as techniques you can learn how to perform in order to couch more effectively.
COPD and coughing medications
If your cough is due to very thick mucus, first you should try to drink more fluids. This can help make your mucus thinner and easier to clear. If this does not work well enough, then there are medicines called “expectorants” that can help make the mucus easier to cough up.
If your coughing becomes painful or difficult to control. In those cases, your doctor might recommend cough suppressants that keeps your body from coughing. These suppressants might also be used for coughs that do not produce mucus, like a dry smoker’s cough.
If you have COPD, coughing can also cause a “bronchospasm” or “spasm.” This happens when your muscles around your airways suddenly tense up causing your airways to become very narrow, This makes it even hard to breathe. To reduce coughing that causes spasms, healthcare providers might prescribe special types of inhaled medications called “bronchodilators” or inhaled steroids.
.png)
If you are not interested in getting on medication for you coughing, there are also three airways clearing techniques you can do to clear your lungs
Airway clearing techniques for COPD
One of the most effective ways to clear your airways is to use the effective, or controlled, cough technique. This cough comes from deep within your lungs and has just enough force to loosen and carry mucus through your airways without causing them to narrow or collapse. By utilizing the controlled coughing practice, you will save energy and therefore, oxygen.
- Controlled coughing: A type of cough that comes from deep in your lungs. It loosens mucus and moves it though your airways
- Postural drainage: You lie down in different positions to help drain mucus from your lungs
- Chest percussion: You lightly tap your chest and back. The tapping loosens the mucus in your lungs
To cough effectively:
- Sit on a chair or on the edge of your bed, with both feet on the floor. Lean slightly forward. Relax
- Fold your arms across your abdomen and breathe in slowly through your nose. (The power of the cough comes from moving air.)
- To exhale: lean forward, pressing your arms against your abdomen. Cough 2-3* times through a slightly open mouth. Coughs should be short and sharp. The first cough loosens the mucus and moves it through the airways. The second and third cough enables you to cough the mucus up and out.
- Breathe in again by "sniffing" slowly and gently through your nose. This gentle breath helps prevent mucus from moving back down your airways
- Rest
- Perform again if needed
Here is a link to postural drainage and chest percussion treatment and how to perform these mucus clearing techniques.

Natural home remedies for helping reduce COPD induced coughing
Eucalyptus oil
Eucalyptus oil contains a natural compound called eucalyptol. Eucalyptol may have the following benefits for people with COPD and may ease uncomfortable coughing symptoms:
- antioxidant and anti-inflammatory properties
- opens up the airways in the lungs
- reduces mucus production
- helps clear mucus from the lungs
- prevents flare-ups in moderate to severe COPD
One way you can use eucalyptus oil is by adding 12 drops of eucalyptus oil to 150 milliliters of boiling water and inhaling up to three times per day.
This will not work for everyone, and if you experience any side effect of the oil, stop using it immediately.
-1.png)
Quit Smoking to reduce dry coughing
Smoking is the leading cause of COPD in the United States and is responsible for around 90 percent of COPD-related deaths.
Tobacco smoke is known to irritate your airways and your lungs. Smoke causes inflammation and obstruction within your airways causing them to narrow, and making it very difficult for air to pass in and out.
If you smoke, the most important step to reduce COPD related symptoms and slowing down the progression of your COPD is to stop smoking. Quitting will put an end to “smoker’s cough,” the dry, hacking cough common among people who smoke.
A deep, productive cough that clears the airways of mucus may replace this dry cough also benefiting you and your breathing.
-png.png)
When you should seek medical attention
Call your doctor within 24 hours if you notice:
- You’re out of breath or coughing more than usual
- Being out of breath affects your daily routine
- You’re coughing up more gunk that normal
- The mucus you are coughing up is dark yellow, dark green, or rust-colored
- You have a fever over 101 F
- You feel dizzy or lightheaded
If you begin to experience any of these symptoms it could mean that you have a respiratory infection or your COPD is getting worse.
Call 911 or go to the emergency room if you’re still out of breath after using the medicines your doctor has prescribed for your COPD.

Other symptoms associated with COPD
One of the other many symptoms of COPD we mentioned very briefly in this article was shortness of breath. When you have COPD your lungs are no longer able to process oxygen like they once did. This is partly due to the irritation in your airways that also causes coughing.
Both chronic bronchitis and emphysema can cause shortness of breath. This symptom is also called “breathlessness” or “dyspnea".
If you airways are swollen and filled with mucus, not only does this initiated a coughing reaction, but it also inhibits oxygen from flowing through your lungs and into your blood stream and organs.
Not only is this feeling extremely uncomfortable, it is also life threatening, and if it goes untreated for a long period of time, you will inevitably be taking years off of your life.
Here are positive changes you can make to improve breathing with COPD:
Learn pursed-lip breathing This is a breathing exercise designed for people with COPD: Purse your lips and blow as much air out as you can before taking a deep breath in through your pursed lips again. Then slow down your breath so that you’re using as much of your lungs as you can. This technique slows your breathing rate and helps to keep your airways open which can also help to reduced coughing episodes.
Drink plenty of water because water helps thin out mucus so you can clear it better. Some people with COPD have conditions that could be made worse by extra fluid, however some people with COPD may be very dehydrated.Speak with your doctor to find out how much water you can safely drink.
Get informed and continue learning about COPD and how your lungs function. This can help you better understand and manage your condition. Pulmonary rehabilitation programs often offer this type of education.
Exercising regularly can make a big difference in your breathing capabilities and COPD symptoms. A lot of people with COPD get more and more out of breath as their disease progresses, but it’s not due of their lung function — it's because they’re not conditioning enough. Most doctors recommend walking for people with COPD since it’s moderate in intensity and easily accessible.
Know and avoid your triggers. If you have COPD and allergies, take steps to avoid anything you’re allergic to. This may mean putting dust covers on your pillows and mattress or keeping your pets out of the bedroom. High-efficiency particulate air filters can remove dust and other irritants from the air in your home. You may also consider a humidifier if dry air triggers your symptoms.
Get your rest Many people with COPD have an underlying sleep disorder, like sleep apnea, that makes it difficult to get good sleep. When you sleep better, you’ll feel better and breathe better, so if you are not able to fall asleep, or have trouble staying asleep, speak with your doctor to understand the root of this issue so you can solve it.

Stay on a healthy diet full of nutrient-dense foods is needed with COPD to maintain strength and fight off infections. Eating healthy can help you lose weight and breathe easier. If you’re underweight, ask your doctor about the best foods to eat and if nutritional supplements are right for you.
Take your medication COPD medications can help manage symptoms, including shortness of breath so be sure you’re taking the right medications and get evaluated to make sure your lung function is as good as it can be
If you have severely low oxygen levels this is called hypoxemia, your doctor will likely prescribe you medical-grade oxygen, for home oxygen therapy. Long-term oxygen therapy has many benefits if it is used correctly and It can even help you live longer.

- Confusion
- A sense of euphoria
- Restlessness
- Headache
- Shortness of breath
- Rapid breathing
- Dizziness, lightheadedness and/or fainting spells
- Lack of coordination
- Rapid heart rate
- Elevated blood pressure
- Visual disturbances
- A bluish tint to the lips, earlobes, and/or nail beds (cyanosis)
Hypoxemia is the main reason that people with COPD and other lung diseases are prescribed supplemental oxygen. There are a few forms of home oxygen therapy: You can opt for liquid oxygen tanks, gas cylinder tanks, or the most popular, convenient, and cheapest option a portable oxygen concentrator.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you are a good candidate for long-term oxygen therapy, this is a blessing in disguise. While it might seem as if you lung function is declining, once you are able to utilize oxygen, your quality of life will improve drastically. When you have adjusted to the oxygen therapy, you will begin to slow the progression of you COPD as well!
Once you find the right POC for you, your bones and muscles will feel stronger and energized, you will have improved exercise tolerance, your mood and stamina will boost, your quality of sleep may improve, and so much more.

If you feel like you have experienced any of the symptoms of hypoxemia, and are curious how to find the best portable oxygen concentrator to fit you oxygen requirements, fill out the blue box to the right, it is our official guide to portable oxygen concentrators.
Cough with a Purpose
Remember, COPD-related lung damage can’t be reversed, but it can be controlled if treated properly.
We hope you and your caregivers understand more about COPD and coughing, and how avoiding coughing is not always the best option.
Now that you understand that your cough can in fact be beneficial for your health while treating COPD, we hope that you can use the information in this article to cough effectively and efficiently. These coughing techniques, mixed with medication and other home remedies should reduce the dry uncomfortable smokers cough, and influence you to cough with a purpose.
Even though this can be a pain, always feel free to excuse yourself during social gatherings, and other outings to clear mucus from your lungs and airways. This will allow you to go longer without coughing and spend more quality time with the ones you love while enjoying the things you like to do.
The more you practice these coughing techniques the more efficient you will become at clearing your airways, and therefore breathing!
If you have any questions please leave a comment on this blog below, and always feel free to share our blog with your friends and family. By explaining how beneficial your cough is for managing your COPD, they will better understand and be willing to help and encourage coughing rather than trying to help you avoid it.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













