Interstitial lung disease (ILD) is a broad umbrella term that’s used to describe over 100 different chronic lung conditions. Each of these illnesses is characterized by scarring and hardening of lung tissue, a process commonly known as “pulmonary fibrosis.”
The term “interstitial” refers to the space around the blood vessels in the small airways and the walls of the alveoli (the small air sacs in the lungs). ILD results when inflammatory cells accumulate in these areas, causing shortness of breath, chest pain, and a chronic cough.
While all types of ILD are separate and often have different causes and risk factors, they are all considered “restrictive lung diseases.” This means that they all decrease the total volume of air that the lungs can hold or they’re caused by a problem related to the expansion of the chest during inhalation.
If you’re interested in learning more about the different types of ILD, their symptoms, causes, and treatment options, as well as how they compare to other chronic pulmonary diseases such as COPD, read on. The more educated you are about your lung health, the better you will be able to deal with symptoms if they arise.
What are the Different Types of Interstitial Lung Disease?
A lot of the confusion around interstitial lung disease is due to the fact that there are so many conditions listed under this umbrella term. Rather than going through every single disease, it’s more practical to divide them all into subgroups based on how they’re contracted. Once you understand each of the different subsets of ILD, you’ll be able to adjust your lifestyle choices accordingly to reduce your risk of contracting them.
Occupational or Exposure-Related ILD
The first type of ILD, occupational or exposure-related, is also one of the most common. Just like the name suggests, this type of ILD is caused by exposure to harmful substances like smoke, metals, or chemicals, often found in unsafe working environments like factories, mines, or construction sites.

These illnesses can be particularly dangerous because they often develop over many years of exposure with little or no side-effects at first. In the past, business owners were not required to implement safety protocols that would protect their workers from these harmful substances, but this all changed in the late 1900s.
The Occupational Safety and Health Administration (OSHA) was founded in 1971 which is a government organization that oversees many of the work-related safety laws and regulations in the United States. In particular, the OSHA has set their sites on ILD prevention because it’s a problem that’s been overlooked for so long.

If you contracted ILD while working, you may be able to file an occupational disease workers’ compensation claim. These laws typically vary based on the state you’re in, but generally speaking, you can receive monetary compensation as long as your doctor can provide you with a note indicating that your disease was caused by your job.
Below are some of the most common types of occupational ILD:
Asbestosis
For many people, the first thing that comes to mind when they think of occupational disease is asbestosis. This is the condition that results from the inhalation of asbestos particles often used in things like cement, fire-resistant coating, pipe insulation, drywall, and more. Since the 1970s, however, asbestos has become heavily regulated especially concerning its use in home and consumer products.

The reason asbestos poses such a hazard is that the microscopic fibers it releases can become lodged in the lungs causing permanent damage and fibrosis. There is no ‘safe’ amount of asbestos you can inhale before it starts to damage the lungs, so it’s imperative to use a respirator any time you have to handle it. There are six different types of asbestos — actinolite, tremolite, anthophyllite, crocidolite, amosite, and chrysolite — all of which are known to cause asbestosis.

Asbestosis should not be confused with mesothelioma which is a type of cancerous tumor that forms in the lung due to asbestos poisoning. The life expectancy of mesothelioma patients is much shorter than that of an asbestosis patient.
Silicosis
Silicosis is a type of ILD that’s caused by tiny crystals called silica. It’s commonly found in the mining, steel, construction, and roofing industries, and much like asbestos, these particles become deeply embedded in the lungs, leading to permanent and irreversible damage.

According to the OSHA, about two million people are exposed to crystalline silica through construction work across 600,000 workplaces in the country. Employers are required to follow a strict set of regulations that limit workers’ exposure and they’re also required to provide a specific type of respirator that filters out silica crystals.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Treatment-Related ILD
Believe it or not, interstitial lung disease can occur as a side-effect of certain medications or drugs; this is referred to as treatment or drug-related ILD. Some of the most common medications associated with ILD include chemotherapy, antibiotics, anti-inflammatories, and heart medications.
Chemotherapy Medication
Bleomycin is a type of antitumor antibiotic commonly used to treat conditions like Hodgkin lymphoma and germ cell tumors. Approximately 10 percent of patients who receive this drug contract pulmonary fibrosis and it’s associated with a number of other lung injuries including hypersensitivity pneumonitis and pneumonia.
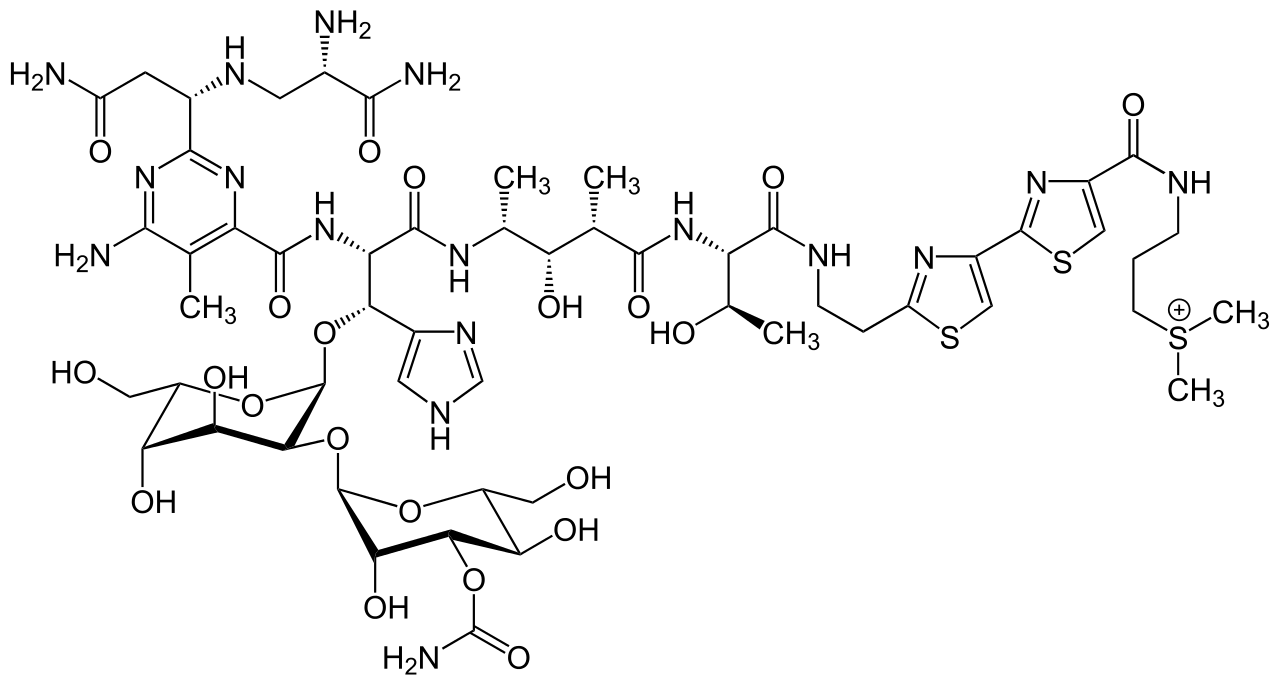
It’s not known exactly why bleomycin can cause lung damage, but research indicates that it may be related to oxidative damage, genetic predisposition, and elaboration of inflammatory cytokines. Other chemotherapy medications that can cause lung damage include carmustine, busulfan, and cyclophosphamide.
Immunosuppressant Drugs
Just like the name suggests, immunosuppressant drugs help to slow or block immune responses in the body. This is important for people with an autoimmune disease where the immune system attacks the patient’s own organs. Some common immunosuppressant drugs include azathioprine, cyclophosphamide, and azathioprine and they all have the potential to cause collateral lung fibrosis.

Heart Medications
A study found that people who use amiodarone to treat abnormal heartbeats had a 5 to 7 percent chance of developing pulmonary fibrosis. Among the patients who develop fibrosis of the lungs, there is a fatality rate of about 10 to 20 percent. Multaq (dronedarone) is often used as an alternative to amiodarone due to its lower risk of lung injury.

Biologic Agents
A biologic agent is a medication that’s made from living organisms. It’s typically used to treat cancer, but it can treat other diseases as well. Biologic agents such as alemtuzumab (Lemtrada), trastuzumab (Herceptin), and bevacizumab (Avastin) are known to cause ILD. However, since these are used to treat serious illness, the benefits may outweigh the risk.
Autoimmune Disease ILD
Your immune system is responsible for protecting your body from foreign substances like bacteria. In a healthy person, immune cells (lymphocytes, neutrophils, and monocytes) prevent infection and keep your body healthy. However, in someone with an autoimmune disease, the immune system mistakenly identifies its own cells as “foreign” and attacks them.
There are many different types of autoimmune diseases. Some of them target a specific organ like the lungs, while others may be systemic meaning they can cause damage to the body as a whole. Autoimmune disorders typically can’t be cured, but they can usually be managed with a precise treatment plan focused on suppressing the immune system and reducing inflammation.
Women are far more likely to develop autoimmune diseases, making up about 78.8 percent of those affected. While there are several reasons why this is the case, it’s mainly due to genetics.
Rheumatoid Arthritis
Rheumatoid arthritis (RA) is a systemic autoimmune disease that affects about 1.3 million Americans. RA primarily attacks cells in the joints such as the hands, feet, wrists, and knees and causes chronic inflammation and swelling. People with RA tend to have difficulty standing, walking, and living an otherwise normal life.
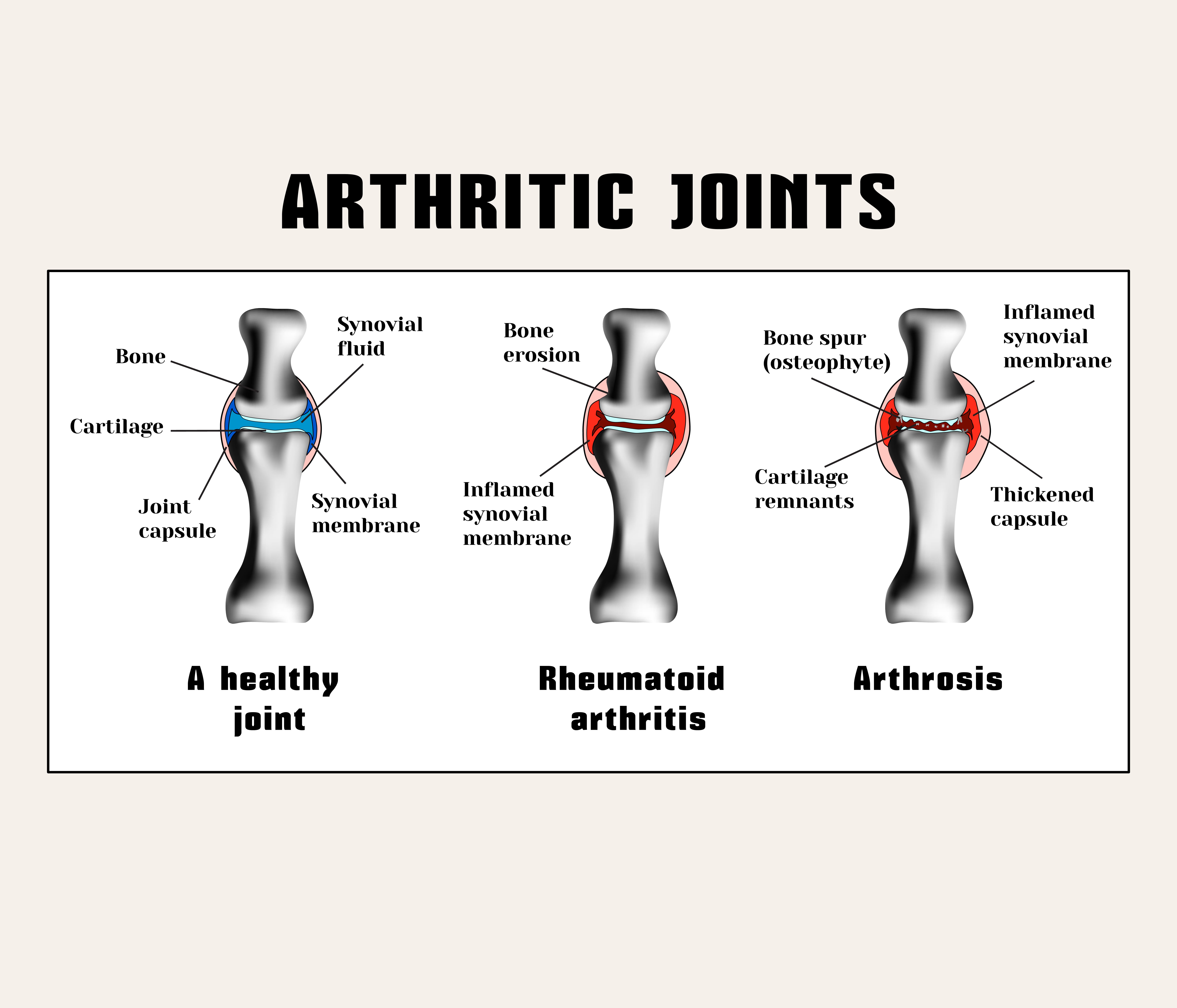
In a number of patients, rheumatoid arthritis has been known to manifest itself in other parts of the body such as the lungs, heart, and eyes. In particular, fibrosis of the lungs and interstitial lung disease have been known to significantly increase the mortality rate of rheumatoid arthritis patients. According to a medical report, the expected survival rate of someone with RA and ILD is about 3 years on average.
Lupus
Lupus shares many of the same symptoms as rheumatoid arthritis, but they are not the same disease. While lupus can lead to inflammation and swelling in the joints just like RA, lupus is more likely to affect the internal organs and skin. The pain caused by RA also tends to increase and then dissipate whereas the pain from lupus usually remains constant. There are four different types of lupus:
Systemic lupus erythematosus (SLE) — the most common type of lupus.
Neonatal lupus — a condition that affects infants
Drug-induced lupus — caused by prescription drugs
Cutaneous lupus — primarily affecting the skin
.jpg)
Just like RA, lupus can affect the lungs. According to the Johns Hopkins Lupus Center, 50 percent of people with SLE will experience lung complications. These complications include the following:
Pleuritis — This is when the pleura (the membrane surrounding the lungs) become inflamed. If fluid begins to form and leaves the membrane, this is known as pleural effusion.
.jpg)
Acute Lupus Pneumonitis — This is a rare condition that can have serious complications for lupus patients. it’s known to cause sharp pain the chest, a dry cough, and shortness of breath. If acute lupus pneumonitis isn’t treated immediately, it could result in permanent lung scarring.
Chronic (fibrotic) Lupus Pneumonitis — This is essentially the same as acute lupus pneumonitis but it occurs over several years rather than abruptly. While both these conditions are interstitial lung diseases, chronic lupus pneumonitis is more comparable to other ILDs like occupational and treatment-related.
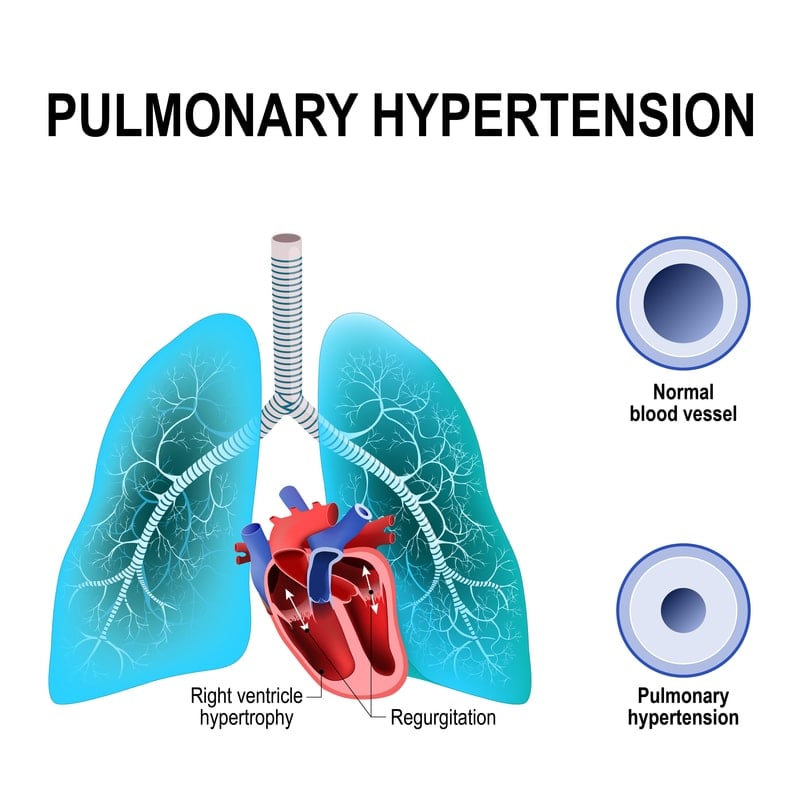
Pulmonary Hypertension — Although this condition is not technically considered an ILD, it’s important to know about if you have lupus. PH is a type of high blood pressure that affects the arteries leaving the heart. This damages the heart because it’s working harder to pump blood and it can damage organs throughout the body if they aren’t getting oxygen.
Scleroderma
Your body is composed of a variety of “connective tissues” like collagen, fibers, and other tissues that give each organ its shape and elasticity. Scleroderma is an autoimmune disease that alters your body’s production of these tissues.
While this may seem harmless at first glance, it’s important to note that most organs, especially the lungs, depend on their shape and consistency in order to function properly. For example, your lungs need to be elastic in order to expand and take in air. And if your skin gets too thick, it can begin to block blood vessels, requiring your heart to work harder to pump blood throughout the body.
.jpg)
The type of ILD caused by scleroderma is called pulmonary arterial hypertension (PAH). This is a result of small blood vessels in the lungs called pulmonary arteries, becoming narrow and constricted. Since PAH is caused by pulmonary fibrosis, it’s considered a progressive lung disease. Symptoms are not likely to improve on their own, so a refined treatment plan is necessary.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Pulmonary Sarcoidosis
Sarcoidosis is a very rare condition characterized by tiny clumps of inflammatory cells called granulomas. Sarcoidosis usually appears on the skin, but pulmonary sarcoidosis forms on the lungs. Usually, the granulomas go away on their own, but if they don’t, they can cause permanent scarring and obstruction in the lungs. It can also result in a condition called bronchiectasis which is when the lungs are frequently infected.
Idiopathic ILD
The term “idiopathic” denotes a disease or condition that has an unknown cause. If your doctor believes you may have idiopathic pulmonary fibrosis (IPF), he/she will perform a number of tests to rule out any potential causes. If no cause is found, you may be prescribed standardized IPF treatments like nintedanib, an anti-fibrotic drug, or pirfenidone, an anti-fibrotic and anti-inflammatory drug. As you can imagine, not knowing the root cause of IPF makes it much more difficult to treat.
What are the Symptoms of Interstitial Lung Disease?
The above list gives examples of just a few of the interstitial lung diseases there are and what causes them. Researchers are constantly working on understanding the prognosis of lung fibrosis and how it can be treated more effectively. But if you want to limit the damage caused by interstitial lung disease, it’s important to recognize the warning signs early on.
As aforementioned, symptoms of ILD can develop over the course of many years so it’s imperative that you take all respiratory symptoms seriously and consult with a doctor as soon as possible. ILD is a chronic disease, so the damage that’s caused by it is irreversible. However, the sooner it’s recognized, the sooner your doctor will be able to provide you with treatments that will prevent it from progressing as quickly.
.jpg)
The two most common symptoms of ILD are shortness of breath and a dry cough. Excess mucus is not usually a symptom of ILD, but it could be a sign of COPD or another chronic lung disease. Other symptoms of ILD include whole-body fatigue, fast breathing, deformity of nails, or rapid weight loss.
How is Interstitial Lung Disease Treated?
Pulmonary Rehabilitation
Many people are surprised to find that exercise is a key part of treating ILD. While heavy exercise can exacerbate respiratory issues, controlled and precise training routines can help improve endurance, strength, and regulate weight. Pulmonary rehabilitation programs are run by health professionals who can educate you about how your lungs work and what steps you can take to improve your quality of life with ILD.

Medications
There are many medications used to treat ILD, so it’s hard to say what your doctor will prescribe. However, some of the most common medications for ILD include corticosteroids, pirfenidone, nintedanib, as well as anti-fibrotic and anti-inflammatory drugs. If your ILD is caused by something like gastroesophageal reflux disease (GERD), you may be prescribed medication that limits this, preventing further damage to the lungs.
Oxygen Therapy
Oxygen therapy is the administration of medical-grade oxygen through a nasal cannula or oxygen mask. Most ILD patients are prescribed periodic or 24/7 oxygen because it helps ensure the lungs are fully saturated with oxygen. There are many different oxygen therapy machines on the market, but most people prefer portable oxygen concentrators like the Inogen One G5 or the Caire FreeStyle Comfort. These units are lightweight, reliable, and allow oxygen patients more freedom in their daily life.

Surgery
Lung biopsy is a fairly common procedure for anyone with ILD. This is when a medical professional surgically removes a part of the affected lung in order to take a sample and study it. This can help your doctor better understand how you contracted ILD, and what medication you can take to reduce your symptoms. In very rare and severe cases, your doctor may recommend a lung transplant surgery which is the full removal and replacement of the lungs.
What’s the Difference Between Interstitial Lung Disease and COPD?
Interstitial lung disease and chronic obstructive pulmonary disease (COPD) are commonly confused, likely due to the fact that they have very similar symptoms. Both are characterized by a chronic cough, fatigue, reduced exercise tolerance, and shortness of breath. However, where these conditions differ is in their causes, risk factors, and the type of damage that is done to the lungs.
Like ILD, COPD is an umbrella term, but instead of 100s of conditions, COPD is made up of just two: emphysema and chronic bronchitis. In emphysema patients, the walls of the alveoli begin to collapse preventing the proper exchange of oxygen and carbon dioxide to and from the blood. Emphysema can also cause air to become trapped in the lungs so that it can’t be expelled correctly. Chronic bronchitis is when the bronchial tubes, the airways that lead to the lungs become damaged and start to swell.

COPD is an “obstructive” lung disease, meaning it prevents the patient from expelling air correctly. ILD is a “restrictive” lung disease, meaning it prevents the patient from inspiring air properly. 85 to 90 percent of COPD cases are caused by smoking while ILD is caused by a whole variety of things. While smoking is a risk factor for ILD, it is not a primary causal factor.
Treatment for COPD and ILD may look similar and it usually starts with eliminating the factor that’s causing the lung damage. Smoking cessation is imperative in both cases but it’s especially important for COPD patients. Oxygen therapy, pulmonary rehabilitation, and lifestyle changes are commonly used to treat both conditions, but COPD patients may need additional medications like bronchodilators to reduce swelling in the airways.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Conclusion
While interstitial lung disease denotes hundreds of different conditions, it is still possible to significantly reduce your risk of contracting it. First and foremost, you should quit smoking and always wear a respirator if you have to work in dangerous industrial environments such as mines, construction sites, or factories. Take care to also follow all OSHA regulations that your company requires.
Secondly, if you have an autoimmune disease like lupus or rheumatoid arthritis, you should visit your doctor frequently in order to keep it under control. Untreated inflammation and immune reactions can lead to damage and scarring of the lungs.
Lastly, if you’re experiencing respiratory symptoms like breathlessness, chest pain, or a chronic cough, you should schedule an appointment with your doctor right away. Respiratory symptoms lasting more than a couple of days are considered “chronic” and might be a sign of a serious underlying condition.

