.png)
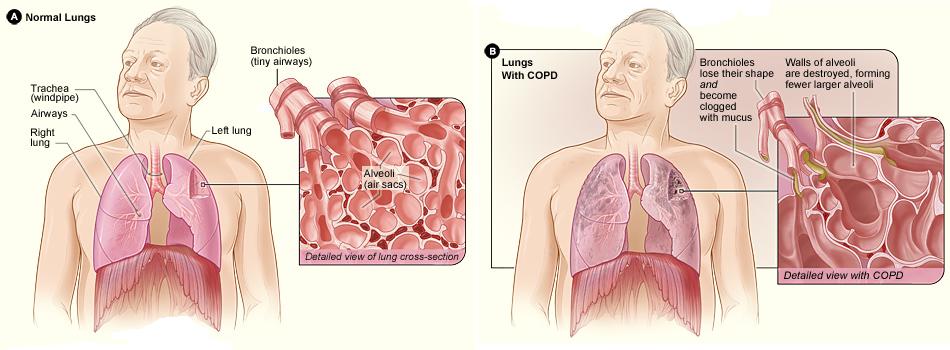
Chronic obstructive pulmonary disease (COPD) is one of the diseases with the greatest financial burdens worldwide and within the United States. Studies have shown that the average annual COPD-related expenditure is around $4,147. And while 51% of these costs are covered by Medicare according to the Centers for Disease Control and Prevention (CDC), that still leaves roughly $2,000 a year that COPD patients need to spend out-of-pocket. Combine this with the cost of aging and limited retirement funds and it’s not hard to see why COPD is such a major financial burden for so many people.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Without a doubt, the later stages of COPD pose the greatest burden for most people. It’s during end-stage COPD that you’re most likely to experience hospitalization due to exacerbation and you’re also more likely to be hospitalized for an extended period of time. Since symptoms tend to develop more quickly during this time, you’re also more likely to schedule more doctor’s appointments, use your medication more frequently, and seek out other treatment options for your disease.
In this post, we’re going to discuss end-stage COPD (also called late-stage or stage 4 COPD). We’ll take a closer look at what exactly this term means, what to expect, and how to prepare for this stage of COPD in order to mitigate some of the physical and financial challenges it poses. If you have any questions, either leave them in the comment section below or reach out to your doctor to schedule an appointment.
What is End-Stage Chronic Obstructive Pulmonary Disease?
Since COPD is a long-term condition that progresses slowly, it’s generally divided into four different stages. These stages help healthcare specialists identify the symptoms of your disease, predict the prognosis of your disease, as well as your life expectancy. And because COPD manifests differently in every patient, that also means the stages are going to look different for everyone. While researchers have a good idea of the average life expectancy of someone with COPD, what ultimately matters is your own health. In this way, it’s often better to think of COPD as a sort of “catalyst” for other health issues.

The best way to know that you’re approaching late-stage COPD is based on your symptoms. Someone with end-stage COPD will likely experience similar symptoms that they’ve experienced for many years such as coughing, breathlessness, fatigue, or chronic pain. In end-stage, however, these symptoms become significantly more debilitating to the point where they may need to rely on caretakers, friends, or loved ones to take care of them. They’ll also experience more frequent trips to the hospital due to flare-ups and exacerbations.
-jpg.jpeg)
The term “end-stage” is controversial in many ways because it can imply that the patient doesn’t have much time left to live, but this isn’t always the case. Even when it’s evident that symptoms are increasing in frequency and severity, that doesn’t mean that won’t outlive them and go on to live many more years. However, using this term can be helpful when it comes to planning and the approach that you use to treat your disease. For example, some people prefer to switch to palliative care which is a type of specialized medical care that’s focused on optimizing a patient’s quality of life and ease discomfort.
How to Recognize End-Stage COPD
As aforementioned, late-stage COPD looks different for everyone. This is why it’s important to maintain open lines of communication with your doctor who can provide you with detailed information about your disease prognosis as well as advice on how to plan. Generally speaking, however, you’ll be able to notice an increase in the frequency and severity of symptoms you’re experiencing. Take a look at some of the symptoms below and see if you notice any similarities to what you’re experiencing.
- You experience heavy coughing or wheezing throughout the day
- You experience shortness of breath even while at rest
- You lack the energy or will to maintain your diet
- You’re becoming more reliant on friends and family for simple tasks
- You experience dizziness, confusion, or trouble sleeping
- You experience more frequent or severe exacerbations that lead to hospitalization
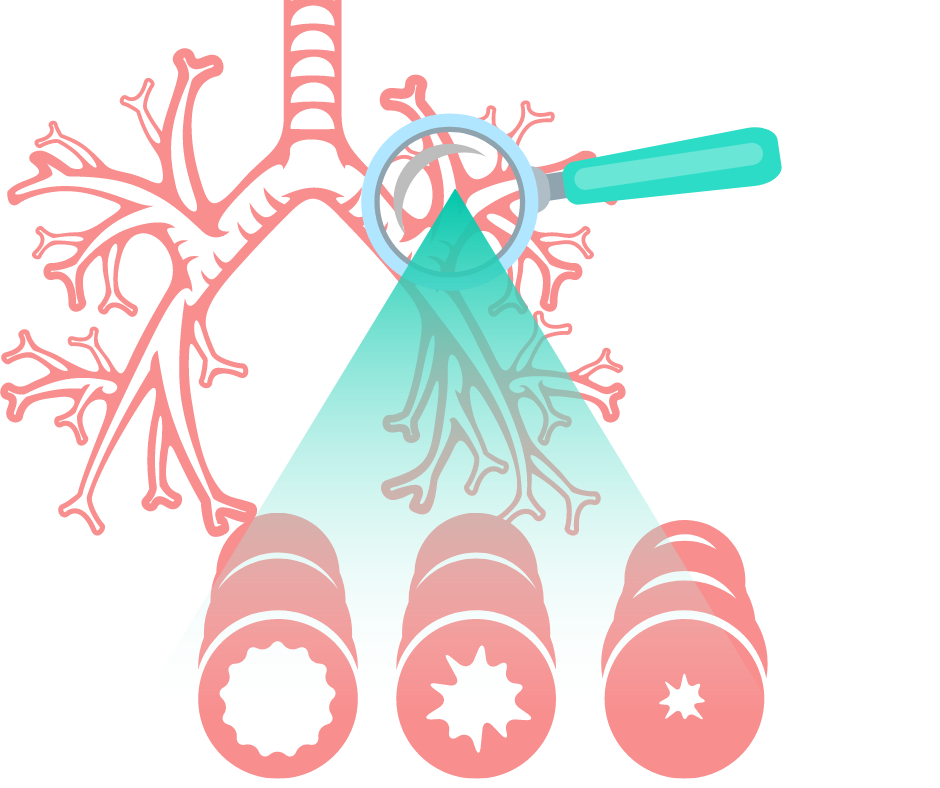
Another way to recognize end-stage COPD is by performing a spirometry test. A spirometer is a simple device used to derive two different results: Forced Expiratory Volume in one second (FEV1) and Forced Vital Capacity (FVC). Combined, these results will tell you how well your lungs are functioning, and if you have spirometry results already, you and your doctor will be able to compare them to determine how quickly your lungs are deteriorating. FEV1 refers to the total amount of air you can force from your lungs in one second and FVC refers to the total amount of air you can expel from the lungs in one breath.

From a diagnostic perspective, stage four COPD is recognized as an FEV1/FVC ratio of less than 70% or an FEV1 less than 30%. Even if your FEV1 is above 30%, however, your doctor may classify you as stage four severe COPD if you have chronic respiratory failure. Several other tests your doctor may use to diagnose stage four COPD include lung volume tests, gas diffusion tests which measure how well oxygen moves from the lungs to the bloodstream, and exercise tests.
How to Ease End-Stage COPD Symptoms
All-in-all, your treatment plan for end-stage COPD shouldn’t look all that different from your treatment plan for any other stage of COPD, but you may need to make adjustments based on your physical, mental, and emotional abilities. What’s more, there are several additional strategies you can add to your routine that can ease some of the pain and increase your comfort.
Supplemental Oxygen Therapy
Oxygen therapy is likely the most consistent treatment you’ve used since being diagnosed with COPD. Since COPD leads to progressive lung obstruction, one of the best ways to remedy this is by helping your lungs out and providing them with a higher concentration of oxygen. By doing so, your body will have the resources it needs in order to stay healthy. Unfortunately, many COPD patients use oxygen incorrectly or they use an oxygen device that doesn’t suit their needs and lifestyle.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
When it comes to oxygen delivery devices, there are several options available to you. Oxygen tanks have been around the longest, followed by liquid oxygen tanks, home oxygen concentrators, and portable oxygen concentrators. While each of these can provide you with the oxygen you need, portable oxygen concentrators tend to offer the most comfort and convenience in end-stage COPD. There are many reasons for this, but above all, they don’t need to be refilled.
.png)
Rather than containing compressed oxygen like oxygen tanks do, portable oxygen concentrators run off of powerful lithium-ion batteries which allows you more freedom to move around on your own time. Instead of having to call an oxygen company to deliver full tanks to you, simply plug your POC into any wall outlet and you’ll be able to recharge your batteries. You’ll even be able to use the device while it’s charging.

There are several different types of POCs you can choose from depending on your wants and needs. Pulse dose portable oxygen concentrators like the Caire FreeStyle Comfort or Inogen One G5 closely monitor your breathing and only deliver oxygen when you inhale. These devices are incredibly efficient, lightweight, and small. On the other hand, you could opt for a continuous flow portable oxygen concentrator like the Respironics SimplyGo which provides the user with a constant stream of oxygen. These machines tend to be slightly bigger and bulkier than their counterparts.
Nutritional Counseling
Like we mentioned before, malnutrition is a significant problem that many stage-four COPD patients face. Symptoms like breathlessness and chronic fatigue can lead to a situation where patients simply don’t have the energy to eat or they don’t get the same satisfaction from it that they used to. Conversely, it could lead to someone choosing foods that are convenient and provide a quick energy boost. Unfortunately, these foods tend to also be filled with sugar and other problematic ingredients that don’t provide your body with the nutrients it needs.
If either of these situations sounds like you, it might be a good idea to consider nutritional counseling. This is a type of therapy that’s focused solely on your eating habits and it attempts to break down any barriers you might be facing that are preventing you from sticking with the diet that your doctor has provided for you. Contrary to popular belief, nutritional counseling isn’t just for people facing weight issues, it’s also extremely beneficial for people with chronic illnesses like COPD who struggle to get the nutrients they need. It’s also useful for anyone who believes that they have “unhealthy” or “unproductive” eating habits.
Complementary Therapies
Complementary therapies are any therapy that can help you ease the burdens associated with late-stage COPD. As you can imagine, this varies greatly depending on the patient because everyone faces different issues with their disease. For some, this might mean attending cognitive behavioral therapy (CBT) sessions in order to prevent anxiety or depression, for others it could mean speaking with a spiritual or religious leader who can help you settle any concerns or fears about living out the later stages of your life.

Cognitive behavioral therapy is a type of psycho-social intervention that’s focused on correcting negative or inaccurate thought processes or actions. It’s a type of therapy that’s become very popular among older adults, especially those with chronic conditions, who want to seek more fulfillment in their daily lives. CBT takes place over the course of several weeks, months, or however long it takes for the patient to feel comfortable on their own.
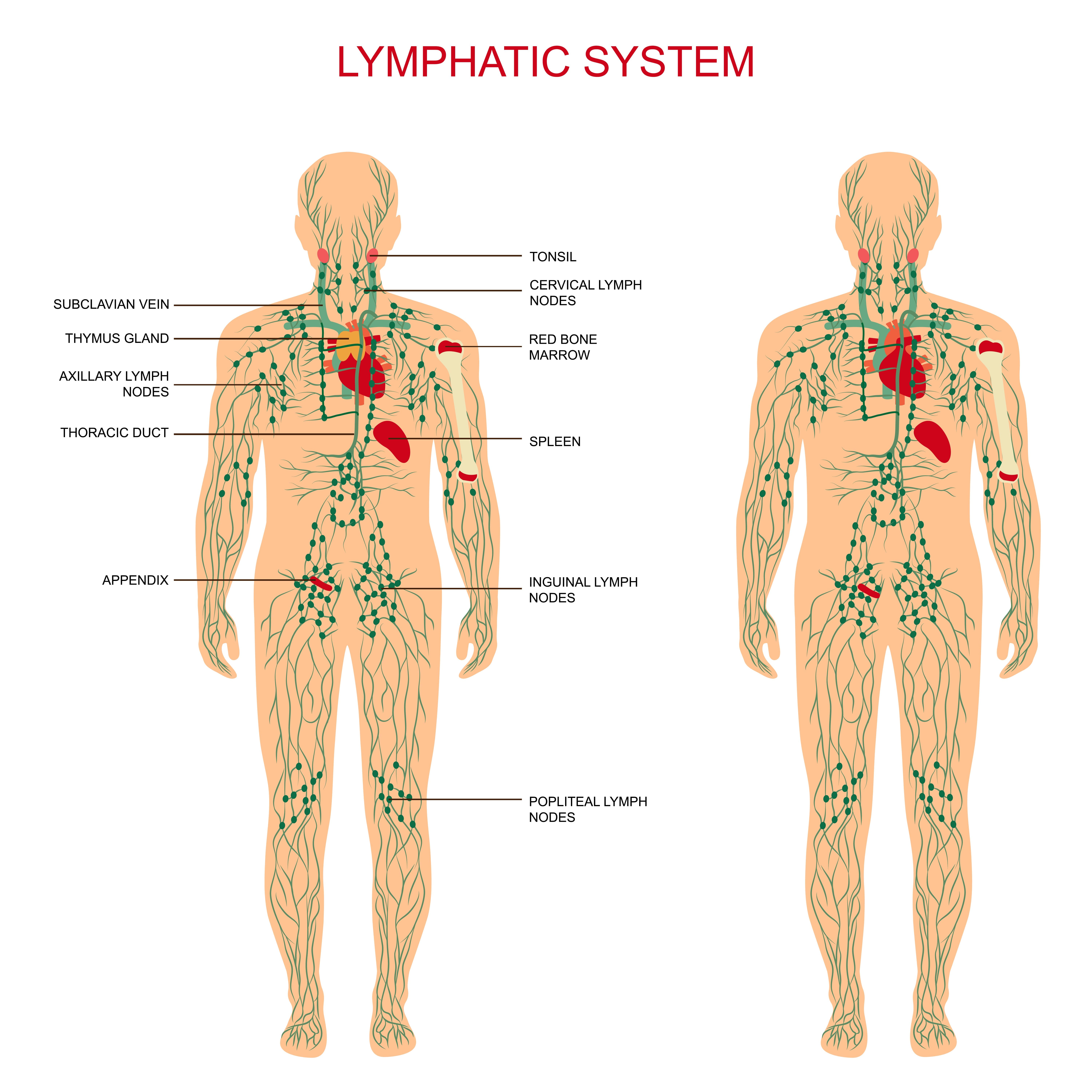
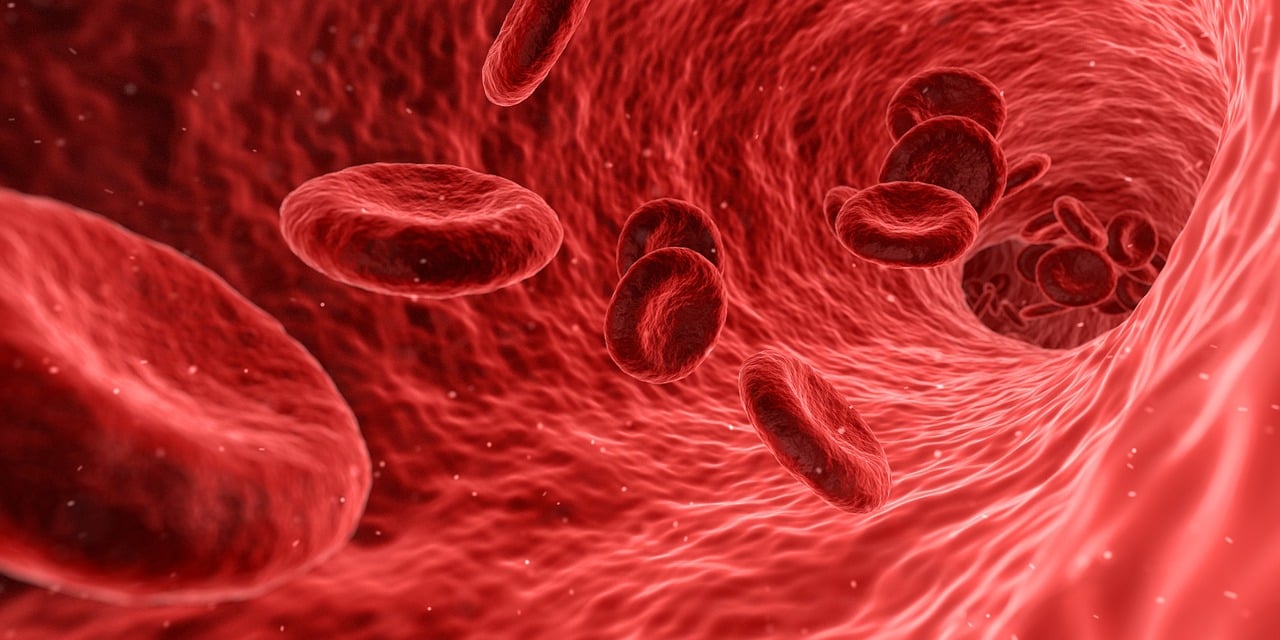
Another type of therapy you might want to consider when it comes time to plan for end-stage COPD is massage therapy. Studies have shown that anxiety can cause a lot of tension to form in our bodies and this tension can lead to more anxiety. Massage therapy is a great way to break this tension causing us to feel better both physically and mentally. According to this medical report, there are two reasons massage therapy is beneficial for COPD patients. Firstly, it causes hyperemia which is the increase of blood flow to different tissues. Secondly, it activates the lymphatic system which is responsible for draining your body of toxins.
A Revised Pulmonary Rehabilitation Routine
Most people are well-aware that with aging comes problems with mobility, endurance, and strength. It’s a natural part of life that we lose a lot of our physical abilities as we get older, but that doesn’t mean you can’t continue to do pulmonary rehabilitation. It simply means that you will need to find new ways to do it. Some people find that the best option for them is to switch to exercises that involve sitting as well as ones that don’t require them to leave the house or meet up with other people.

The important thing to remember is that any form of exercise will benefit your lung health, not just exercises that work your lungs specifically. In many cases, this mindset can even be counterproductive in late-stage COPD because most people don’t have the lung capacity to perform any strenuous endurance exercise that gets your heart rate up. Rather, targeting specific muscle groups in your body will improve your strength and circulation, thus easing some of the burden on your lungs. Studies have shown that muscle requires less oxygen to use and it produces less carbon dioxide as waste, ultimately resulting in less air that your lungs need to take in.

The thing that we would like to stress, like we’ve done many times before, is the importance of consistency when it comes to your pulmonary rehabilitation. Just like maintaining a healthy diet, your exercise routine will be more effective if you are able to do it everyday without letting yourself fall back on your goals. Ideally, you should have someone like a friend or family member who can hold you accountable at least until you are able to do so for yourself.
Address Your Concerns With Your Doctor
Just like with any other stage of COPD, you’re going to want to work closely with your doctor in end-stage COPD. This is because you’ll want to make sure that your goals are in line with or at least not counterproductive towards your treatment goals. Like we mentioned earlier, end-stage COPD should be all about improving your comfort and reducing chronic pain. But this doesn’t mean that you should completely ignore the treatment plan that you’ve followed throughout your whole life with COPD.

Another reason to consult your doctor is because he/she will likely have some helpful resources for you in regards to finding other health specialists such as nutritionists or mental health experts. This will not only save you a lot of time but it will set you off on the right path. You should also make it a priority to visit your doctor more frequently so that you can make healthy choices that fall in line with your COPD treatment plan.
Conclusion
Chronic obstructive pulmonary disease (COPD) is an ailment that develops and progresses over the course of many years — sometimes even decades. This is why it’s important to always be adaptive when it comes to your treatment plan and lifestyle. While during stage one COPD, you were likely very active and took the time to travel as much as possible, stage four COPD treatment should focus more on improving your comfort and ensuring your psychological, physical, and even spiritual needs are met.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
While you should take the initiative to do these things for yourself, it’s also important to consult your doctor to make sure you don’t leave out any aspect of your treatment plan in the process. Even in end-stage COPD, you’ll need to keep up with your oxygen therapy, dietary plan, pulmonary rehabilitation, and avoid environmental triggers such as pollution or airborne allergens.

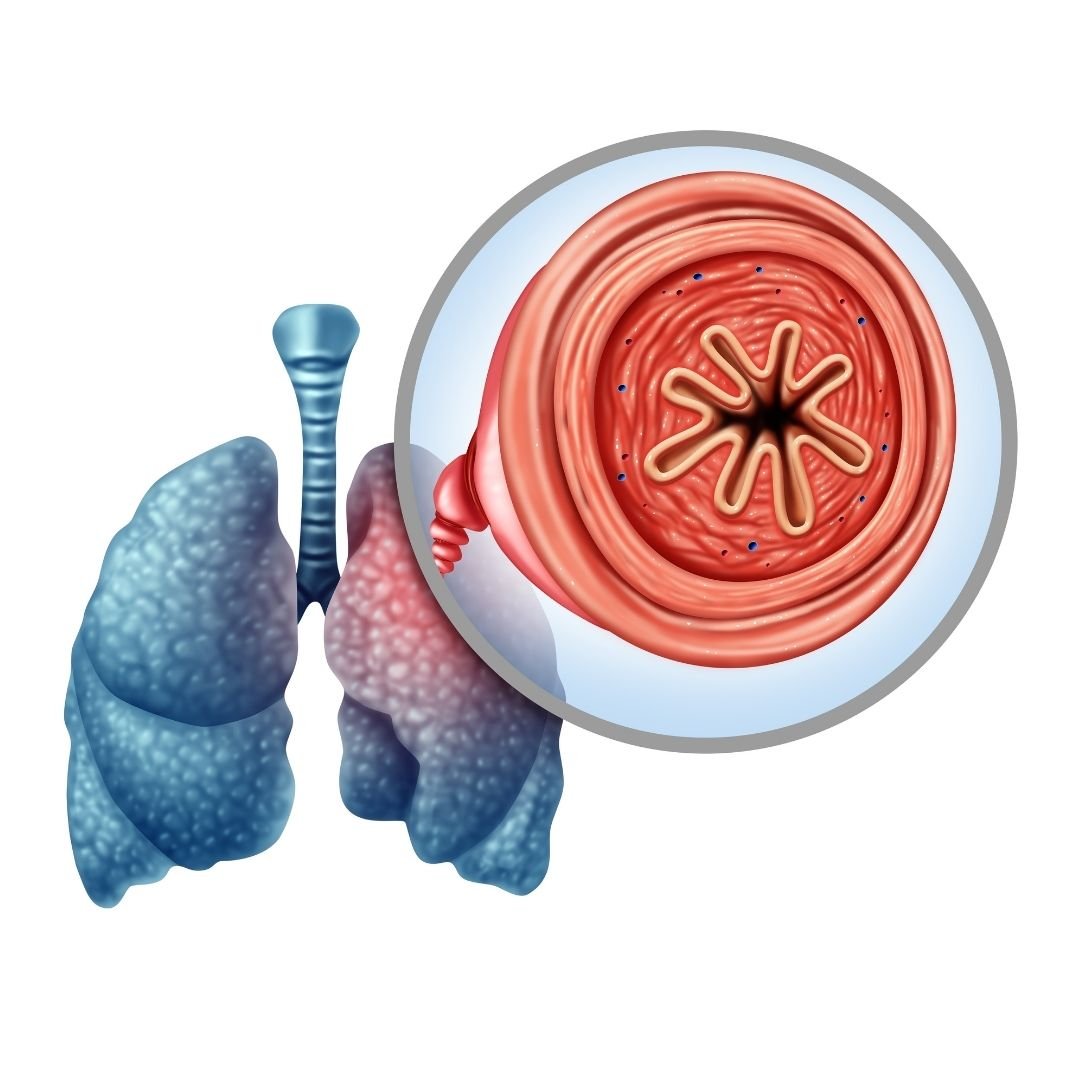
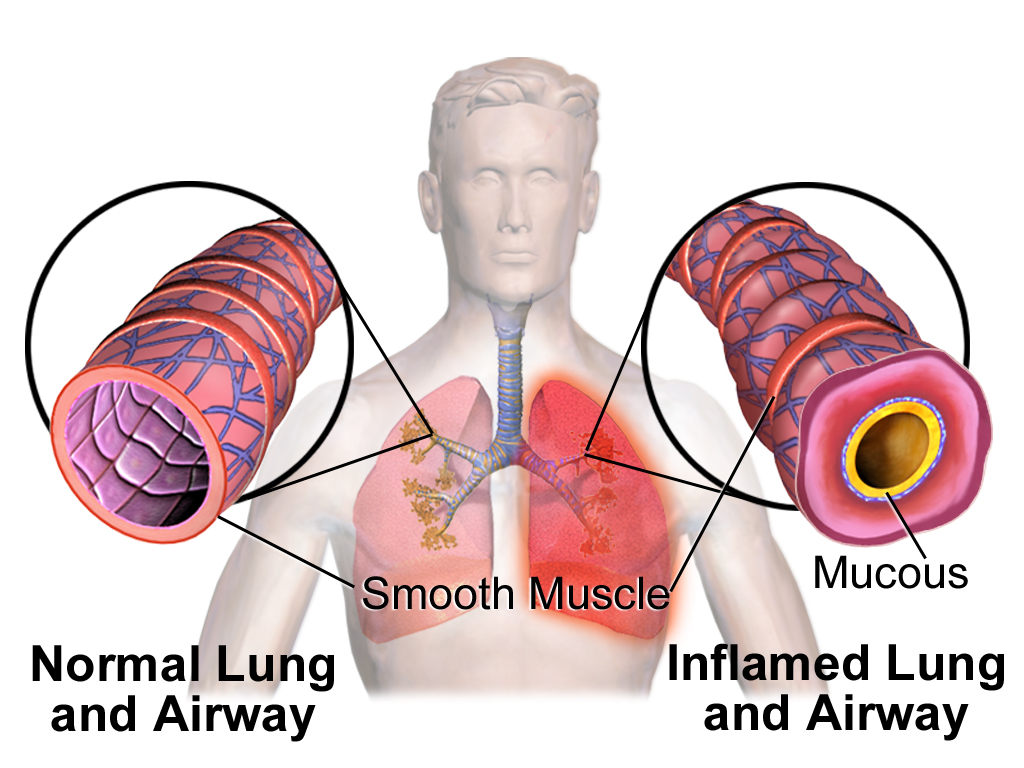
There are five big respiratory diseases that are the most common causes of severe illness and death worldwide- COPD, asthma, acute lower respiratory tract infections, tuberculosis and lung cancer. There are other forms of lung disease that also impact large populations around the world like occupational lung disease, pulmonary hypertension, sleep apnea, pulmonary embolism.
Chronic obstructive pulmonary disease, or COPD affects 16.4 million adults and accounts for two main groups of lung diseases, emphysema and chronic bronchitis, each contributes to the obstruction of air flow that interferes with a patient’s normal breathing.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
If you have been diagnosed with COPD, understand that your condition will worsen over time. However, you can take the necessary treatment that can improve your quality of life and slow down the progression of your disease and you can do so by overcoming hardships and challenges that your disease will inevitably present you. Its called a fight for a reason!
Early and accurate diagnosis of COPD is a huge factor in treating your disease, this may seem obvious, how can you treat a disease if you don’t know that you have it? But it is not that simple, inaccurate diagnosis of COPD happens all of the time, and it is important that you and your doctor are aware of the signs of COPD so you can catch it early on!
Testing for COPD
Doctors should use spirometry for the diagnosis of COPD according to a GOLD report that was released in 2020. This test is helpful in avoiding misdiagnosis and determining the severity or stage of your COPD.
When diagnosing COPD, a doctor is looking at things like:
- Symptoms
- Severity of airflow limitation
- History of exacerbations
- Presence of other health conditions
Looking Out for Early Signs of COPD

Looking out for COPD symptoms is not the easiest way to prevent COPD because oftentimes symptoms don't appear until lung damage has already occurred to the point of no return. The best way to look out for yourself and avoid getting COPD or at least be sure that you are slowing the progression of the disease if you already have it, is to reduce and eliminate your exposure to respiratory irritates, number one being cigarette smoke. Quit smoking!
If you have COPD you’ll start to notices signs and symptoms of COPD like:
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Chronic cough
- Excess production of mucus that may be clear, white, yellow or greenish
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (if your disease has progressed into more severe stages)
- Swelling in areas of your legs
All of these COPD symptoms can inflict pain and suffering on your day to day life, so treating your disease properly can help ease these discomforting symptoms.
Treating COPD Symptoms

COPD affects everyone differently, you might experience more shortness of breath throughout the day and someone else may have a chronic cough, COPD is not a straight laid out treatment plan, it requires you to be flexible and listen to your body.
You also have to listen to your doctor and take the medication and oxygen therapy as prescribed in order to reduce the chances of experiencing an exacerbation and hospitalization, and to slow down the progression of your disease.
Oxygen Therapy

Long term oxygen therapy is one of the most effective treatments for COPD if your blood oxygen levels are low enough, and is the only treatment that will actually add years to your life.
This is because once your COPD has infiltrated your lungs to the point where they can no longer function properly enough to provide your body with the oxygen it needs to survive, supplemental oxygen can oxygenate your blood for you.
If your blood oxygen levels are low enough, and your doctor prescribed you supplemental oxygen therapy, a portable oxygen concentrator is your ticket to a healthier lifestyle. With the help of your oxygen device you should be able to sleep better, exercise more, and breathe easier.

Overcoming Challenges Presented with Supplemental Oxygen Therapy
Overcoming challenges with your oxygen therapy will come with time, patience, and practice. As with anything, it will take time to get used to using your device.
Tubing
Using the tubing during the day and at night while you sleep is a learning process, but eventually it will be second nature.
If you feel like the tubing is rubbing uncomfortably on your ear or your face, try wrapping the tubing in fabric or foam. This is a great solution for irritated skin caused by the friction of a nasal cannula sitting against your face or on top of your ears. Because you have to wear this tubing all day and night, the constant contact can cause soreness and skin irritation over time, which can make oxygen therapy very uncomfortable.
Dryness and irritation
Sometimes, you will notice your supplemental oxygen can cause dryness and irritation, common areas that might be affected are your lips, the skin under the nose, and other areas of the face that are near or in contact with your nasal cannula, oxygen, mask, or tubing.
This can be the result of rubbing, chafing, or the constant flow of air drying out your skin. When you use oxygen continuously, it is common that your skin will dry out in the areas where air escapes the tubing.
A simple solution for dryness and irritation that can help your skin heal and reduce the chances of future inflammation is to start using water-based moisturizers on your face and lips. If that does not help, your skin irritation could be a sign that your oxygen mask or nasal cannula isn't fitting you properly. If it's too tight, too big, or sits too loosely on your face, it can cause unnecessary friction and chaffing.
If you are having chronic problems with soreness or irritation, talk to your doctor or your oxygen supply company about getting a new nasal cannula or oxygen mask. You might need to try a different size, a different design, or a different brand in order to find one that fits your face more comfortably.

For more tips and trick to make you oxygen therapy more comfortable, read this blog:
How to Make Supplemental Oxygen More Comfortable
Medication

Common COPD medication consists of long-acting and short-acting bronchodilators, inhaled steroids, combination inhalers, oral steroids, phosphodiesterase-4 inhibitors, theophylline, and antibiotics.
All of these mediations have some kind of set back or side effect that can disturb your day to day life. Managing your medication and taking it properly is one of the only ways you can combat these issues.

Overcoming Challenges Presented with Medication
First of all, if one of your medications is giving you horrible side effects, talk with your doctor about trying a different medication with the same purpose but perhaps a different medication will not have such great side effects.
There is a lot of research being done surrounding COPD, and new innovative medications become available from time to time, so be sure you stay up to date with COPD news and experiential treatments either by doing your own research online or speaking with your doctor.

There are many efforts to develop new drugs for COPD. A research team from NIH’s National Institute of Environmental Health Sciences (NIEHS) in Rome, Italy, investigated the use of hyaluronan. Hyaluronan is naturally produced by many of the tissues in your body, including your lungs. The idea of utilizing hyaluronan as a new drug for treating COPD wound be for healing and reducing inflammation. In animal studies, inhaled hyaluronan treatment was shown to reverse some types of COPD, so watch this space and others like it for new COPD clinical trials.
Exercise

If you have COPD, you already know that exercise is a huge aspect of your treatment plan, and finding a time to exercise everyday will help you manage your COPD and slow the progression of your disease. But you also must know how hard it is to find the motivation to exercise.
Overcoming Challenges Presented with Exercise
If your disease has progressed, and you are required to be on oxygen therapy, having the right oxygen equipment can help you find motivation to exercise more than any other one thing. A lightweight portable oxygen device will give you the ability to bring your oxygen with you for a long walk or bike ride so you can stay oxygenated during your exercise session.

If you need continuous flow oxygen, the Respironics SimplyGo is the lightest continuous flow device available today, and it is a great option for any oxygen patient that is looking for more range of motion and freedom to exercise.
Of course, even with the help of your oxygen device, exercise can still be challenging.
Here are a few tips for getting in shape with COPD:
- Start with small increments and time, and build from there.
- Write down an attainable goal everyday that involves moving your body or an exercise that you can do. Check off the goal once you’ve accomplished it.
- If you feel tired one day, try to go for a short walk instead of taking the day off
- Drink plenty of water and stay hydrated
- Eat a healthy and balanced diet that give you energy
- Join a pulmonary rehabilitation course to learn new exercise and be around people going through similar trials and tribulations as you

Mental Health and Depression
Dealing with a chronic illness will take its toll on your mental health because you are not always capable of doing the things you once loved. Not to mention that diseases like COPD can be intrusive and uncomfortable to live with.
Emotional health is just as important to take care of on top of your physical health that you treat with medication and oxygen therapy. One of the best ways to treat mental health issues is to seek out meaningful and helpful social interactions.
Try talking to support groups and opening up in your pulmonary rehabilitation courses, it is likely that someone in your COPD community is going through similar issues. If you have trouble opening up about your mental health in person, try joining facebook and online forums and talking to people online. Also don’t forget that confining in friends and loved ones may seem hard at first, but it can really help them understand your mood swings and symptoms that are not always as obvious.
Beyond social interaction, you can also talk to your healthcare team about your mental state. Asking for help is sometimes the only way to get your emotions under control, so ask your health care providers to work with you to understand the cause of your feelings, and to identify coping strategies that will work for you. They may recommend you speak with a mental health professional such as a counselor, psychologist or psychiatrist.
There are also medications available to help with anxiety and depression, but they have not always been found to be effective for people with COPD. Counseling, or talk therapy, can successfully help people living with COPD change patterns of negative thinking and behaviors, improve quality of life and reduce anxiety and depression.
Overview

Dealing with challenges is a guaranteed part of having a chronic illness like COPD, overcoming these challenges is left up to you.
There are active steps you can take to get through the obstacles, and if LPT Medical can help you get the oxygen device you need to combat supplemental oxygen related challenges, just call 1(800)-946-1201.
You can also find a plethora of respiratory disease resources on our website where you can get information about everything and anything you need to learn more about your condition and how to manage it!

If you have COPD it is important to take care of your body and your lungs, people do this by quitting smoking, exercising whenever possible, taking medication, and adhering to a strict treatment plan. Beyond these measures, it is important to also pay mind to your mental health, in doing so people with COPD become more motivated and cultivate a positive mind set.
When people's COPD symptoms begin to worsen is when their mental health also deteriorates and subsequently influences people to pay less attention to their COPD treatment thereby negatively effecting their health and well being. This is whats known as a negative feedback loop, which is a reaction that causes a decrease in function. So, creating a healthy environment to live in, by keeping your home clean and irritate free, is so crucial for these patients in order to find "homeostasis" which is essentially a state of normalcy.
In this article we are going to discuss how you can create a healthy living space mentally while living with COPD, but we are also going to give you ways to make your physical living space inside your home more COPD friendly.
Creating a healthy living space inside your mind

We wrote an entire article about the mental health of COPD patients and how this disease can influence depressive and anxious feelings, you can read that article by clicking here.
Now we are going to go over a few ways you can cultivate a more positive mindset while living with COPD, with a following section about living in a healthy environment physically with COPD.
Social connections
Connection is an important part of dealing with COPD and the mental stress and confusion that often comes with the territory. While it is not something your doctor would prescribe, connecting with others is something you doctor should or likely has already recommended. It is also important to maintain a healthy relationship with the people who were in your life before you were diagnosed. It can be challenging to rely on the people in your everyday life more than you had before, so finding a sense of independence is critical here.

In this section we are going to talk about connecting with new people, fostering relationships with your caregivers, and finding your own independence in order to maintain these healthy relationships with others.
One of the easiest and most beneficial ways to connect with other people who have COPD is to enroll in pulmonary rehabilitation. Your doctor should be able to refer you to a program in your area. For example, if you live in Florida in the Boca Raton area you are assured quality care at their South Miami Hospital Pulmonary Rehabilitation program. They have licensed, certified respiratory and physical therapists trained and certified by the National Board of Respiratory Care.
In a pulmonary rehab course, you will work closely with a team of professionals including:
and sometimes other clinical experts as needed

With the help of all of these experts, you will learn about multiple facets of your life. You will learn about your medical condition, how to exercise properly and within your capabilities, respiratory advice and management, managing eating habits and mental stress, all while connecting with others who are suffering from COPD as well.
While all of these aspects of pulmonary rehab are important, but the social component is so valuable for your mental state of mind. Seeing and hearing other people’s hardships throughout their diagnosis can help you feel less “alone”. Feeling alone is one of the main reasons people with COPD struggle to stay positive, thereby neglecting their treatment regimen and their mental health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
So cultivating relationships with people in your pulmonary rehab program who have similar medical conditions, is a great way to connect and feel less alone.
The other way you can create new relationships within a community that you can relate to on a medical level is joining facebook support groups. This is as simple as searching LPT Medical COPD & Respiratory Support Group on facebook and requesting to be added to the group. Once the admin has accepted you, say hello by posting a comment about something you want to talk about.

Even though you are sharing with others online, these people are real, and connecting via the internet is one of the safest ways to relate to people right now amidst a global pandemic.
When it comes to fostering old relationships with your loved ones through the duration of your disease, we could write an entire blog post, so we did, you can read it by clicking here
The main points of this article are as follows:
- Learn how to communicate effectively
- Learn as much about your disease together as possible, education is key in the management and treatment process, the more you know the more comfortable you will both feel
- Destress in any way you can that works for you, such as , exercise, alone time, breathing exercises, medication, or gardening.
- Find independence where you can get it
Point number 4. brings us into the final part of this section: Finding independence. Your independence is so important for your mental health, the current relationships you have, and future ones as well.
Independence
Before you were diagnosed with COPD, you could shower, walk to get the mail, do yard work, without thinking twice about it. Now, you might have to ask for help more often than you are used to because you are unable to do these chores on your own anymore. Many people find asking for help to be frustrating, and if this is not something you are used to, you must find ways to cope, but also find ways in which you can regain your independence.

If you are an oxygen user, your oxygen device may get in the way of you doing things that you could once do on your own. If your oxygen device is too heavy, not portable, or you do not enjoy using your oxygen device, it may be time for an upgrade.
There are modern forms of oxygen therapy that allow you to get back to doing more things you want to do. By buying a portable oxygen concentrator you will be able to travel alone, carrying your device on your own, and feel more confident managing your oxygen therapy on your own.
Depending on the model of portable oxygen concentrator they range from 4 - 18 pounds based on the flow settings and battery life. Having a device that runs on battery life is essential for independence because you will not have to rely on an oxygen refill company to deliver your oxygen tanks every week. Instead you will be responsible for charging your unit or keeping an extra battery on you.
Depending on your oxygen prescription, the right portable oxygen concentrator should have flow setting well above what your are prescribed. For example, it your Doctor writes you a prescription for 630 ml/min of oxygen, the Inogen One G3 could be the perfect oxygen device for you, because it has the capability to run at 1050 ml/min of oxygen so if you ever need to increase your oxygen output in your oxygen device, you will not have to return the device for a new one, you can simply adjust the setting.

As an established oxygen supply company in Denver, CO we have access to the top tier oxygen equipment on the market, but we also have over 10 years experience working with oxygen patients in all levels of their diagnosis. Of the many things we have learned in our experience, one of the most important is to focus one everyone's individual oxygen requirements but also their lifestyle.
Portability and accessibility are two of the main reason oxygen patients decide to switch from traditional oxygen tanks to portable oxygen concentrators, but there are other factors to think about when deciding on your oxygen equipment.
Click here to read about oxygen therapy equipment and how they all compare.
The next part of encouraging a positive mindset is learning how to enjoy the little things.
The little things
We have all heard the saying “enjoy the little things” and while it sounds like a clique, there are a lot of benefits to finding simple pleasures, especially if you have COPD. As a COPD patient, you are still capable of enjoying life, and similarly to the way you once did before you ever started experiencing symptoms.

But if there are aspects of your life, you won’t get back due to your disease, this is the perfect opportunity to try new things. And if you change your perspective this way, there is nothing that can stop you.
Examples of the little things would include family time, reading, movie marathons, gardening, walking, cooking, or any hobby of your choosing. You can start by setting goals; if you don't have a hobby, make a list of new activities or hobbies you want to try. Then make a list of the tools or motivation you would need to start doing said hobby.
Simply looking forward to something is a form of enjoying the little things. Spending more time in your day being active and having something to do will also give your mind something else to focus on besides your COPD symptoms.
Making you physical living space COPD friendly

When you have a disease like COPD, it's vital to breathe air that is clean and healthy as often as possible. Respiratory diseases cause your lungs and airways to be extra sensitive to irritation and inflammation, and even the smallest amounts of airborne contaminates can worsen COPD symptoms and even cause exacerbations.
Air filters

Many people underestimate the importance of using a high quality air filter and neglect their house's ventilation system. Choosing a quality air filter is just another choice the is over-saturated with brands and models so you may not know what to look for or how to choose a kind that's effective and meets your individual needs.
Additionally, there are many different portable and small-space air purifiers you can find, as well as dedicated whole-house air purification systems that hook up to your HVAC system. However, it can be difficult to understand all of these different options, how they work, and how to know if you need one for your home. SO, we wrote an entire blog post about this!
You can read it by clicking here!
Temperature
The next thing you should try to do in your home, is adjust your heating in order to keep your home at a temperature between 19 and 21°C. Cold temperatures may influence your COPD symptoms making you feel worse.
Home renovations
It is also crucial that you avoid using strong chemical products such as polish and paints when or if you ever do home renovations or basic house work. These products can irritate your airways causing you to experience worse symptoms.
Cleanliness

The cleanliness of your home is one of the major factors in determining the indoor air quality. Therefore, cleaning with the intention to maintain good air quality is crucial to avoid COPD flare-ups.
Dust and dust mites, pets, smoking indoors, cleaning solutions, room fresheners and candles, are a few of the irritates that can spark a COPD exacerbation progressing your COPD faster into a more severe state. This is because when you breathe in irritates, they can cause problems like increased mucus production, making it difficult for you to clear your airways, or your airways begin to spasm, making it very hard for you to catch your breath even doing the most simple tasks.
Neglecting to clean your home of dust, allergens, pet dander, smoke and other respiratory irritates can cause major damage to your lungs, but it can also make your life a lot more chaotic than it needs to be. If your home environment is toxic to your lungs you will find yourself visiting the emergency room all the time, and once you’ve recovered from the exacerbation in the hospital and go home, the cycle will continue.
Cleaning products

So you should keep your house clean, but you also need to be aware of the cleaning product you are using because they can be harmful to inhale, and for someone with COPD, this can cause exasperated symptoms. Having a low or no scent home is a good rule to follow. Fresh lemons (or lemon concentrate), baking soda, water, simple dish washing detergent, vinegar, and rubbing alcohol can be used in various combinations to clean most things.
If you ever need to use bleach, try to leave the house or go into a different room while someone else in your household cleans with bleach.
Smoking
It is exceptionally important to keep your home a smoke free environment, meaning no cigarettes or e-cigarettes, and it is best to avoid vape products as well.
Smoke particles are often microscopic, that are byproducts of burning substances or other chemical processes, which can be inhaled into the lungs and cause irritation.
You should not only quit smoking yourself, you should not allow others to smoke inside you home. There are no good ways of getting rid of smoke entirely, and it’s harmful to have in your home for multiple reasons. It not only creates a lot of these microscopic particles that can live in your walls, carpets, and decor, it makes up gases and toxins that are truly lethal.

Natural gas
You might not realize it at first, but if you have a gas stove, or gas fireplace, you have to be cautious about the exposure to nitrogen dioxide emissions. These emissions can come from natural gas. In order to avoid these irritates, adequate ventilation in your kitchen is the best way to remedy this.
Pets
If you have any pets that shed, pet dander isn’t necessarily an issue for all people living with COPD. If you have even mild allergies this may cause exacerbated COPD symptoms. Regularly vacuuming and wiping surfaces, cleaning furniture, and linens in your home can help reduce pet dander.
Dust and carpets
It is so important to dust often in your home. Dust can be especially irritating to people with COPD who have allergies. In addition to keeping home surfaces free from dust, experts also recommend minimizing carpeting in your home.

If it is possible you should remove carpet from your home because dust mites will get into your carpet and live there, making it difficult to remove. Hardwood floor is much easier to manage, and does not hold pet dander or dust like carpet does, making your living environment more manageable with less irritates in the air. If it’s not possible to get rid of your carpet, use a vacuum cleaner with a built in air filter to bring up the dust mites and other irritants found in carpet.
Bedding
Dust mites are also found in bed linens. So you should try to keep them clean as much as possible. This is as simple as washing your sheets using hot water and replacing pillows more frequently.

Humidity
Depending on your body and your COPD, the humidity level in your home could be another irritant in and of itself. Keeping the humidity at a manageable so it is easier to breathe is great, but also keeping the humidity below 50 percent in your home is a good way of helping to control mold and dust mites. Dust mites grow fast when there is a humid environment. Be sure to always use the exhaust ventilation in your bathroom during and after you shower, provided that the vent sends damp air outside of the home and doesn’t simply recirculate it. If you don’t have ventilation in your bathroom, you may want to consider installing it.
Oxygen
It is so important that you follow your oxygen prescription to a T, so having oxygen equipment that you can carry with your throughout your house with ease is very helpful. Even "heavier" devices compares to the lightweight Caire Freestyle Comfort should still be maneuverable. The Respironics SImplyGo weighs 10 pounds, and stands 10" H x 6" D x 11.5" W meaning your SimplyGo will easily fit underneath the seat in front of you on the airplane, you can store it on the floor of your car or in the passenger seat as you drive,, and while this device may be heavier than other pulse flow devices, the SimplyGo is one of the smallest and lightest continuous flow portables available! You will be able to bring it with you wherever you go and you will have no problem finding a place to store it.

The SimplyGo includes a custom carrying case and a wheeled travel cart so you have the option to carry it over your shoulder or you can pull it behind you on the travel cart and it will make it around the house with you and .
If you need oxygen 24/7 is it helpful to own your own portable oxygen concentrator that is designed to run day and night. The Respironics SimplyGo is CPAP/BiPAP compatible and it even offers sleep mode technology! When you are relaxing in your chair at home, and you feel yourself dozing off, you can turn sleep mode technology on to ensure your oxygen gets delivered while you are sleeping. The sleep mode technology on your SimplyGo increases its sensitivity to detect your breath and it softens the pulse flow delivery so it doesn’t wake you up.
Overview
Living with COPD is all about balance, and creating good habits while overcoming bad ones. The goal is to create positive feedback loops that promote function in your mind and in your body.
Believe it or not, the way your body feels influences the way your mind reacts, feels, and makes decisions, and vise versa. The decisions you make and your emotions will directly effect how you body feels physically.
If you can keep your home clean and free from irritates your COPD are less likely to get worse overtime and your body will feel better allowing your emotions to be more positive and capable of making good decisions. Creating a healthy living space in your home is just one example of the many actions you can take in order to live a longer and healthier life with COPD.
We covered a lot of information in this article, and if you made it this far, leave a comment, let us know how you find inner peace both in your mind and your home!
.png)
In the 21st century, we are highly dependent on energy sources like natural gas and electricity. We use fuel to power our cars, cook and heat our homes, and we use electricity to charge our phones, computers, and more. But what happens when we lose access to these resources due to a natural disaster or some other problem? In some situations, this can be a minor nuisance; but in others, it could be life-threatening.
Fortunately, hospitals and other medical facilities have back-up generators that allow them to use life-saving medical equipment even in the event of a power outage. But what about individuals living at home who are reliant on electronic devices? What safety measures are in place to ensure these people are able to use the medical devices they need to stay healthy?
The truth is that there aren’t many safety nets in place to help people experiencing power outages, so this is why it’s always important to be prepared, especially if you depend on electricity to power your medical equipment. In this post, we are going to highlight all the steps you should take to be prepared for a power outage if you have COPD or any other chronic respiratory disease.
What Causes Power Outages?
Before we can discuss the different ways to plan for power outages, it’s important to understand what actually causes them. According to the U.S. Energy Information Administration, the average household experienced one outage in 2016, accounting for 112 minutes of lost power. Although this is the average, this does not mean that power outages cannot last longer. Depending on what causes the power outage, they could last anywhere between several days and several weeks. So you should always plan for the worst-case scenario.

According to Constellation, the most common cause of power outages are severe weather and natural disasters. High winds, snowstorms, and thunderstorms can all knock power lines over causing entire neighborhoods to lose power. Extreme temperatures can also lead to power outages if it results in people overusing their air conditioners or heaters. There are so many different variables that come into play, so it’s best to always be prepared for an outage, regardless of the time of year and what the weather is like.
Install an Emergency Power System
The first thing you should do to prepare for power outages is to have an emergency power system in your home. There are many different options for powering your home in the event of an emergency, so you will have to do a lot of research to determine which one will best meet your needs. However, a good place to start is by contacting your utility company. Some utility companies provide backup generators for people with medical conditions free-of-charge. Others may add an additional fee to your monthly utility bills. Below are some of the most widely used emergency power supplies:
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Home Backup Generators
A home backup generator, also known as a standby generator, is a permanent power generator that is installed outside of your home. These generators resemble air conditioning units and they run off of your existing natural gas or LP fuel supply. While home backup generators are the most costly option for backup power, they are also the most convenient and reliable. These units are designed to turn on automatically when a power outage is detected, so you won’t have to go outside to turn it on. Since these generators are permanent, they will give your home’s value a nice boost if you ever decide to sell it. As you can imagine, home backup generators are extremely advanced, so you will need to hire a professional to install one for you.

Portable Generators
A portable generator, also known as a recreational generator, is a type of generator that’s commonly used for camping and other outdoor activities. However, they can also be a good way to power your home during a power outage. Unfortunately, these devices don’t start automatically when your power goes out, so you’ll have to go through the hassle of setting it up when your power goes out. What’s more, these units use fossil fuels which can exacerbate your respiratory symptoms, so be sure to never use one inside of your home. The benefit of portable generators is that they are much more affordable than home generators.

Solar Generators
Just like the name suggests, solar generators are powered by the sun. The only scenario where you should purchase a solar generator is if you live in an area that is very sunny to ensure that your generator is fully charged when you need it most. Since these generators don’t burn any fuel, they won’t exacerbate your lung symptoms and they aren’t noisy. Solar generators are fairly expensive but they are worth the price for many people.
Install a Medical Alert System
An emergency alert system is a device designed to alert medical professionals if you experience a medical emergency like a COPD exacerbation or a fall. Each medical alert system comes with a pendant that you wear around your neck and a receiver that plugs into the wall. In the event of an emergency, press the button on the pendant and an ambulance will be dispatched to your home.

What many people don’t know is that many medical alert systems have backup batteries that will kick in if there is a power outage. Generally speaking, most backup batteries will last a day or two, but you should speak with the company that manufactures it to learn the full details. Medical alert systems are an invaluable tool to have when the power goes out so be sure to get one installed as soon as possible.
![]()
Another way to prevent falls when the power goes out is to have a flashlight on hand. Chances are, even if you have a generator in your home, you’re going to want to conserve energy by keeping as many lights off as possible. A flashlight will help you navigate your home safely while doing so.
Keep Backup Batteries or Oxygen Tanks
COPD patients have a variety of options at their disposal when it comes to medical oxygen. Some of the most popular options include oxygen tanks, liquid oxygen tanks, and oxygen concentrators. The one you choose as your “backup” oxygen supply in the event of a power outage will depend on what your needs are.

The most notable benefit of having backup oxygen tanks is that they don’t require electricity in order to operate. Oxygen tanks have compressed oxygen inside them, so all you need to do is connect your nasal cannula and you’ll have access to medical-grade oxygen. However, the downsides of oxygen tanks are that they are very heavy and bulky so you won’t be able to get around your home while you’re using one.
Liquid oxygen tanks work a little differently than normal oxygen tanks. Rather than storing the oxygen as a gas, these tanks store oxygen as a liquid. Since gas is expanded, storing it as a liquid allows you to carry more of it with the same size and weight tank. This will allow you more freedom in the event of a power outage. However, there is one glaring flaw with liquid oxygen tanks which makes them impossible to recommend for this situation. Oxygen needs to be stored at very low temperatures in order to stay as a liquid, so over time liquid oxygen will begin to evaporate, According to the Lung Institute, liquid oxygen will evaporate in a week or two depending on the type of tank you have.
.png)
Last but certainly not least there are oxygen concentrators. Unlike the previous two oxygen devices, concentrators are electronic devices. They work by drawing in ambient air and putting out medical-grade oxygen. It may seem silly to use an electronic oxygen device during a power outage, but you may be surprised to find that they are actually the best backup oxygen device for this situation. Portable oxygen concentrators run off detachable batteries that can be stored for emergencies.

These batteries are also very small and only weigh about a pound so you can store as many as you’d like. One important thing to note is that batteries should be used from time to time in order to help them keep their charge. Be sure to swap out the batteries occasionally so that each one is being used. Let’s take a look at some of the best portable oxygen concentrators to have during a power outage.
Best Oxygen Concentrators for a Power Outage
The Caire FreeStyle Comfort
The FreeStyle Comfort is currently one of the most popular portable oxygen generators on the market. It’s a pulse dose portable oxygen concentrator meaning it has built-in technology that tracks your breathing and only delivers oxygen when you inhale through the nasal cannula. What this means is that it’s able to conserve electricity while still giving you the oxygen you need to stay healthy. With the larger 16-cell battery, the FreeStyle Comfort can run for up to 16 hours on one charge.

The FreeStyle Comfort is one of only a few portable oxygen concentrators that weigh at or under 5 pounds. Additionally, it’s one of the most compact concentrators so you can carry it around on your shoulder with ease. In the event of a power outage, the FreeStyle Comfort will provide you with plenty of battery life, ease-of-use, and mobility. It has a maximum oxygen output of 1,050 milliliters per minute (ml/min).
The Inogen One G5
The Inogen G5 is another pulse dose portable oxygen concentrator under 5 pounds. With the 8-cell battery, the G5 weighs only 4.7 and has a battery duration of 6 ½ hours. The battery life can be doubled with the 16-cell battery affording you up to 13 hours of battery life on one charge. Just like with the FreeStyle Comfort, the batteries are very small and lightweight so you can store as many as you think you’ll need to make it through a power outage.
.png)
One of the great things about the Inogen G5 is the number of accessories there are for it. The G5 external battery charger is very useful if you’re planning for a power outage because it allows you to charge one battery separate from the G5 unit itself. In other words, it allows you to charge your batteries more quickly so that you can always be prepared. Another great accessory to have during a power outage is the DC charging cable. This is a type of cable that allows you to charge your G5 in the car via a cigarette outlet. Keep a DC charging cable in your car so that you’re always prepared if you need to leave the house in a hurry. The best part about this is that you can use your device while it’s charging meaning there will never be an interruption in your oxygen treatment.
The Respironics SimplyGo
The last portable oxygen concentrator we’d like to recommend for power outages is the Respironics SimplyGo. Certain patients are prescribed continuous flow oxygen which is where oxygen is administered irrespective of the user’s breathing rate. When this is the case, the SimplyGo is the lightest and most reliable unit available to you. The SimplyGo has a maximum flow rate of 2 liters per minute (LPM) at it weighs only 10 pounds which is significantly lighter than most continuous flow POCs on the market. Unfortunately, the SimplyGo offers significantly less battery life than the aforementioned POCs, so you may need to keep even more batteries charged.

Create a List of Contacts
Having a convenient list of contacts you can call during a power outage is very important. You don’t want to be searching the internet using what little electricity you have to find out the number of your utility company or your neighbor’s phone number. Take some time right now to write down your contacts so that you don’t have to do it when an emergency occurs.

Firstly, you should write down the numbers of a couple of friends or family members who could come pick you up if your power is out. Secondly, you should have your doctor or pulmonologist’s number as well as the closest medical oxygen company. If you happen to run out of oxygen for one reason or another you can reach out to them and have them deliver some oxygen tanks. Lastly, don’t forget to write down the number of your utility company. Be sure to call them immediately when the power goes out so that you can plan accordingly.
Keep Non-Perishable Food in Your Home
One of the most notorious issues with power outages is that all of the food in your fridge will begin to spoil. This can be absolutely devastating if you like to keep your fridge well-stocked with lots of food and beverages. It’s a good idea to get in the habit of buying healthy non-perishable food at the grocery store that can hold you over if you experience a power outage. Apples are a great source of energy and they will stay fresh for up to a week while sitting on the counter. However, be sure to ask your doctor about non-perishable foods that are healthy for COPD patients.
.jpg)
Speak With Your Doctor
Last but certainly not least, you can and should speak with your doctor about managing your COPD during a power outage. Your doctor might have some helpful information or resources for you to refer to. Most likely, he/she will tell you the minimum flow rate you’re allowed to use on your oxygen tank or concentrator in order to maintain your blood oxygen levels. Also, be sure to ask your doctor if it’s okay to cease your pulmonary rehabilitation routine while the power is out so that you can conserve your oxygen supply.

Conclusion
While it’s rare to experience a power outage that lasts more than a couple of hours, it’s crucial that you are prepared for the worst-case scenario. Studies have shown that power outages are associated with a greater risk of exacerbation and hospitalization in COPD patients. Ensuring that you always have access to a dependable medical oxygen supply will help you to stabilize your respiratory condition.
What’s more, you should work together with your doctor to create a power outage action plan. You may be able to reduce your oxygen flow rate in order to conserve your oxygen concentrator battery life during a prolonged power outage. And ideally, you’ll have some sort of backup generator that you can use to hold you over until the electricity returns to your home.
Here at LPT Medical, we can help you prepare for power outages by providing you with a durable and reliable portable oxygen concentrator like the Caire FreeStyle Comfort or the Inogen One G5. While we can’t guarantee that your battery will last the duration of the outage, we can help you find the best concentrator for your needs. Please don’t hesitate to reach out to us either by email or by phone.

The holidays and shopping for friends or family with COPD can be difficult. But you know what's more difficult? Living with COPD every day of the year, and especially in the cold winter months!
Gifts can bring a lot of joy to the holiday, but special gifts picked out specifically for your loved ones with chronic respiratory diseases can bring joy that lasts throughout the year! Below are 16 practical Christmas gift ideas that COPD patients may find useful!
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
So, while the gifts laid out in this article are practical and very useful for COPD patients, always remember that COPD patients may want something lighthearted, fun, that brings an element of the holiday spirit.
Exercise Bike
Exercise is an essential part of treating COPD. Exercise gives COPD patients hope for rebuilding strength and enjoying a fuller, more active life.

Pulmonary rehabilitation programs typically combine education, exercise training, nutrition advice and counseling, but for some people pulmonary rehab classes are not an option!
An exercise bike is a great option for low impact exercise that you can do from the comfort of your own home.
Nothing is more important to the person who has COPD than exercise. Exercise ultimately makes it easier for those with COPD to breathe by strengthening muscles, bones, and lungs.

An exercise bike is something that will be valued by your loved one for years to come.
A tip for purchasing an exercise bike for a loved one is to choose a model that has several levels of resistance and a smooth magnetic resistance system so it can meet any COPD patient's needs.
Hat, Scarf and Glove Set

The cold winter months are a challenging time of year for COPD patients who already struggle to get around.
Staying warm is especially important for someone with COP. Breathing in cold air can ignite a bronchospasm and shortness of breath, causing a nasty flare up.
![]()
A scarf, hat and glove set will help your loved ones stay warm when they go outside and reduce the likelihood of them experiencing an exacerbation due to the cold air.
There are face masks designed for people with COPD that you can also buy. They are less fashionable, but offer a ventilation system that warms and moisturizes the cold dry air they are breathing in while outside!
Oxygen Therapy Gifts

If you are looking for a gift for a love one who uses oxygen therapy here are some ideas:
A New Pulse Flow or Continuous Flow Portable Oxygen Device

Pulse flow options:
Caire Freestyle Comfort
The Caire Freestyle Comfort is a pulse flow portable oxygen concentrator capable of delivering medical grade oxygen to COPD patients via face or nose cannula.

When you order the Freestyle Comfort from LPT Medical you are not only getting the portable oxygen concentrator, it will come with some additional accessories that will help your loved one make the most out of their oxygen therapy device, as well as a 3-year warranty!
Portable oxygen concentrators run off battery power, and the Caire FreeStyle comes with the 8-cell Lithium-Ion rechargeable battery. If you want a more powerful battery, you have the option to get the large Caire FreeStyle 16-cell battery.

You will also get an AC adapter and the DC car adapter, which allows you to charge your device in a traditional wall outlet, or in the car using the cigarette lighter.
If you want another way to charge your device, you can purchase the Caire Freestyle external battery charger separately. With the external charger, you can keep your batteries charged no matter where you are in the world.

When you buy a Caire FreeStyle Comfort, you will also receive the Caire FreeStyle custom carrying case that comes with a convenient shoulder strap. You can also opt for another carrying method with the Caire Freestyle comfort backpack, this way you have several options to choose from when you carry your device with you.
With the purchase of the Caire FreeStyle Comfort, you will receive:
- 8-Cell Battery
- AC Charging Cable
- DC Charging Cable
- Caire Freestyle Custom Carrying Case
- Tubing
- Filter
- Manual
- 3 year-long warranty
Lifestyle P2
The Lifestyle P2 from Rhythm is one of the smallest and lightest units on the market. At 4.37 pounds, it offers pulse settings 1-5 and gets up to 5 hours of battery life.

Rhythm products, specifically their Lifestyle P2 portable oxygen concentrator, is not only built to keep oxygen users safe, comfortable, and independent, it is also a source of guidance and education.
Lifestyle Mobility Aids exists with a simple mission— to take care of people with medical needs, including those with respiratory issues that need supplemental oxygen to survive.
What Comes With the P2 Rhythm Portable Oxygen Concentrator?
- P2 Rhythm Portable Oxygen Concentrator
- AC Power Supply
- DC Power Supply
- Rechargeable Battery
- Protective Carrying Case
- Shoulder Strap
- Tubing
- Filter
- Manual
- 3 year Warranty
Inogen One G5

Medical oxygen tanks can be restrictive and oftentimes people sacrifice their freedom to hang out with friends or visit with family on your terms due to their oxygen device.
Help your loved one get back to doing what they love, ditch those cumbersome oxygen tanks and order the brand new Inogen One G5 portable oxygen concentrator.
Instead of worrying about refilling your oxygen tanks, the Inogen One G5 restores your mobility thanks to its portable delivery of pulse flow settings of 1-6, which is powered by a rechargeable lithium-ion battery.
Plus, if you’re familiar with the Inogen family of medical oxygen concentrators, the Inogen One G3 offers incredible battery life in combination with a compact and lightweight design. Well, the Inogen One G5 portable oxygen concentrator is lighter and offers a longer battery life than the Inogen One G3.
What Comes With Your Inogen One G5:
- Inogen One G5 Portable Oxygen Concentrator
- Single Battery
- AC Power Supply
- DC Power Supply
- Custom Carrying Case
- Shoulder Strap
- Tubing
- Manual
- 3 Year Warranty
Continuous flow options:
Respironics SimplyGo

Philips Respironics broke the stereotypical design for continuous flow portable oxygen concentrators when they released the Respironics SimplyGo.
Ever since it was released it has been one of the top continuous flow units on the market! However, its small size isn’t the only reason it’s been one of the top units on the market. Backed by one of the biggest names in the respiratory field, the SimplyGo is as reliable as they come!
If you are looking for a lightweight portable continuous follow device to gift your loved one for the holiday call 1+(800)-946-1201!

What Comes With Your SimplyGo?
- Respironics SimplyGo Portable Oxygen Concentrator
- 1x Battery
- AC Power Supply
- DC Power Supply
- Custom Carrying Case
- Padded Shoulder Strap
- Padded Handle Strap
- Travel Cart
- Accessory Bag
- Tubing
- Manual
- 3 Year Warranty
SeQual Eclipse 5

The SeQual Eclipse 5 is the 4th generation model in SeQual’s extremely popular Eclipse line of concentrators.
In fact, the Eclipse 5 is one of the best selling and most reliable continuous flow portable oxygen concentrators on the market. It offers the highest oxygen output on the market, gets good battery life, and it was also designed for the US Military.
What Comes With Your Eclipse 5?
- SeQual Eclipse 5 Portable Oxygen Concentrator
- 1x Battery
- AC Power Supply
- DC Power Supply
- Travel Cart
- Accessory Bag
- Tubing
- Filter
- Manual
- 3 Year Warranty

Other COPD Gift Ideas
FDA Approved Pulse Oximetry Monitor
![]()
Having a FDA approved pulse oximetry monitor indicates whether or not you are getting enough oxygen.The large, easy to read LED display and accommodates fingers of all sizes, and is each to bring anywhere due to its compact size.
Blood Pressure Monitor
A blood pressure monitor is an essential piece of a COPD management kit! Many people with COPD also struggle with other complications and may take a variety of medications. Maintaining healthy blood pressure is an essential part of disease management.
Blood Pressure Monitor can also display an automatic alert if an irregular heartbeat is detected and the ability to remember the last 100 BP readings. All great safety features that help to better understand what the body is doing and how it functions in certain situations.
Nebulizer Compressor Kit
A nebulizer administers medication directly into the COPD patient's airways, helping them breathe easier.
Some COPD patients are lucky enough to have insurance that pays for their nebulizers, but this is not always the case and many are unable to afford one.
If your loved one does not have a nebulizer compressor kit, it is a great gift that keeps on giving.
Custom carrying backpack for the Inogen One G5

A custom carry backpack is just the ticket your loved one needs to live a more active and independent lifestyle.
This backpack is lightweight and durable, this one can be used with almost any compact portable oxygen concentrator but it fits the One G5 perfectly. It is perfect for COPD patients who like to travel and be active.
COPD for Dummies
COPD for Dummies or any other resource that helps explain COPD is a great gift that help educate the family on COPD so everyone is capable of lending a helping hand, but also so that everyone can understand the disease and its toll it take on those diagnosed with it
The book includes the most basic information on COPD symptoms, diagnosis, causes, treatment, and how to cope with COPD.
This may be a nice gift for those who were recently diagnosed with COPD.
Overview
![]()
Make the holidays extra special this season with gifts for people in your life with COPD! Buying them gifts that are practical and useful for disease management can help them all year around become more independent and healthier!
If you are interested in the process of buying a portable oxygen concentrator or accessories to go with their portable oxygen concentrator simply call 1+(800)-946-1201
Try to think back, and remember what your daily routine looked like before you started suffering from symptoms associated with chronic obstructive pulmonary disease (COPD), pneumonia, asthma, heart failure, cystic fibrosis, or sleep apnea…
Were your days filled with long walks outdoors, or restful naps after reading your new favorite novel? Did you spend time gardening and taking care of tasks around the house, or did you dedicate you free time to traveling far and wide to see loved ones meeting new friends along the way?
No matter what your daily life looked like before, you should still be able to experience the joys of life by accomplishing a similar daily routine now, or at least a daily routine that you love.
If you are diagnosed with stage one through four COPD or another type of breathing ailment, (for the sake of this article, we will mostly refer to COPD, however, the information applies to everyone who needs supplemental oxygen therapy despite what disease or chronic illness you may have) it is time to take control of your disease before it takes control of you. There are a lot of different lifestyle choices, treatments, and medications that can help you treat and control COPD.

For example, Several kinds of medications are used to treat the symptoms and complications of COPD. You may take some medications on a regular basis like Bronchodilators which are medications that usually come in inhalers — they relax the muscles around your airways.
Your doctor may recommend you begin a pulmonary rehabilitation program, which is a course for people with chronic lung diseases like COPD, emphysema and chronic bronchitis. It will allow you to be as active as possible while educating you about your disease.
You can also try to limit or stop habits that impact your well-being such as smoking or exposing yourself to harmful populates and allergens.
You can start exercising more and eating lung and heart healthy foods.

However, the most impactful treatment that will allow you to get back to the daily routine which you love and value, is starting oxygen therapy. Now, the only people who can reap the benefits of oxygen therapy are patients who experience low-levels of oxygen, enough so that they require supplemental oxygen to increase their blood-oxygen levels to normal rates.
If you do not have low enough levels of oxygen, taking supplemental oxygen will not benefit you, and instead you should try to increase your exercise tolerance, take you medication prudently, and eat healthy. Inhaling extra oxygen your body does not need, can make you feel nauseous or dizzy from too much oxygen saturation.
If you need oxygen therapy, it will not only increase your blood-oxygen levels. This therapy will help you get back to doing the things you love to do, whether that is sleeping, walking, golfing, traveling, reading, socializing, and so on.
The most obvious thing about supplemental oxygen therapy is that it relieves a lot of the symptoms associated with COPD. Many of the symptoms that come with COPD are debilitating, leaving you at the will of your breathlessness and irritation. Taking away these symptoms gives you the freedom and energy you need to take advantage of all the life you have left!
Oxygen therapy relieves symptoms associate with your chronic illness so you can get back to doing what you love

Your goal when it comes to oxygen therapy should be to continue as many of your usual activities as you can!
You should work with your doctor and oxygen supply company to get oxygen equipment that will allow you to do every activities you still enjoy. Choosing the right type of equipment for you and your lifestyle is crucial — the right portable oxygen equipment can play a major role in improving your quality of life, starting by relieving a lot of your symptoms.

Here are 10 symptoms of COPD that oxygen therapy will work to improve or relieve, and some of the benefits you reap by doing so:
- Combats breathless
- Reduces dry coughing
- Improves stamina and energy
- Increases exercise tolerance
- Strengthens muscles, joints, and bones
- Give you the ability to travel
- Improves sleep
- Increases life expectancy
- Reduces headaches and nausea
- Can improve memory

Combats breathlessness
Oxygen therapy takes away that feeling of breathlessness all times of the day. Whether you are resting or exercising, while you are using your oxygen, you should feel comfortable breathing and capable of doing things that once made you stop to catch your breath.
If you use a portable oxygen concentrator (POC), for example the Inogen One G5, you are able to carry it with you simply by slipping it into your purse, side satchel, or backpack. It only weighs 4.8 pounds, and has a pulse dose rate 1-6. So if your oxygen levels fluctuate throughout the day depending on the activities you are performing, your POC will be able to range between every oxygen source you need.

If you have very low levels of oxygen, and you require a continuous flow of oxygen while you rest or sleep, but during the day a pulse dose setting works for you, the Respironics SimplyGO POC has you covered. This unit weighs in at a mere 10 pounds and the SimplyGo is one of the smallest and lightest continuous flow portables available.

These two POC offer the same quality of life for two people with very different oxygen requirements, so whichever oxygen user you are, you can enjoy your days with little to no breathlessness.
Exacerbations, often referred to as flare ups, are caused when someone with COPD experiences extreme shortness of breath and their medications do not work in time to relieve their breathlessness, to the point where they must seek medical attention.
By using and adjusting to a portable oxygen concentrator or another form of oxygen therapy you will likely experience less flare ups and therefore spend less time in the hospital or seeking emergency medical attention.
This peace of mind alone can serve as many forms of release from COPD’s control over you, to the point where you feel in control of your disease.
Works to alleviate symptoms associated with coughing

If you have COPD, you have definitely experienced a persistent cough, but did you know that a cough that brings up a healthy amount and color of mucus is actually very beneficial for your airways and lungs?
If you are coughing “correctly” you are clearing your airways that are filled with excess mucus and often swollen airways. These two factors make it hard for oxygen to pass through, thereby reducing the function and productivity of your lungs.
Read this article for tips and tricks on how to cough correctly if you have COPD.
.png)
Well, if you have COPD you probably also experience a non-productive cough, often caused by smoking, it's called a dry cough. Other coughs that are common among patients with COPD are associated with anxiety. These coughs can be relieved and treated so that you can avoid coughing at social gatherings and in public spaces where it may make you feel uncomfortable.
You can reduce the dry cough if your doctor prescribes you some prednisone. A Prednisone is an anti-inflammatory drug that helps with inflammation of your airways in your lungs. If your cough is due something else that over-the-counter cough medications are unlikely to help, there are still other things that you can do to quiet a pesky cough.
Drinking water thins out your mucus making it easier to expel, staying hydrated also soothes your dry, irritated throat. You should drink at least 8 ounces of water every two hours, and if you tend to drink caffeine you should drink even more than that!
Lastly, you should try to avoid lung irritates like smoke, allergens, pollution, and other impurities in the air. These ailments can get into your lungs and stay there, making your cough last a lot longer than necessary. You can try using a humidifier in your home if you live in an arid environment to keep your throat and airways moist. Some air filters are also great for home use and can go a long way in filtering out dust and other particles in your home for fresh breathing air.
So, what does oxygen therapy have to do with a pesky cough that makes you want to stay home rather than attending your favorite annual conference or attending a social gathering? Coughing is a natural reaction that your lungs will force you to do when your airways are swollen tight and filled with mucus. Your cough alone will not clear your airways enough so that you can breathe in the amount of oxygen you need to not only be more social, but to survive.
An additional oxygen therapy prescription on top of the correct coughing techniques will get your body the oxygen it craves. You will likely start to enjoy attending more social events like you once did because you are not coughing as often, and when you do cough, you can excuse yourself to clear mucus efficiently, so you are able to get back to the festivities.
Improves stamina and energy

Your lack of energy may not have to do with your age at all. As we age we often find reasons to blame our tiredness on the fact that we are getting older. However, this is not always the case and if you are willing to accept that reality, it's time to take a look at your oxygen levels.
Without the proper exchange of gases, oxygen and carbon dioxide, your body can't get the oxygen it needs. When your body is low on oxygen, you will feel tired and fatigue comes more quickly when your lungs can't properly inhale and exhale air. You'll develop low blood oxygen levels, a condition called hypoxemia, which is one of the main signs associated with COPD that indicates you need oxygen therapy.
Your doctor can perform a series of respiratory tests to see what your breathing capacity is and how well your lungs are functioning. In stages one and two of COPD, your oxygen level may be sufficient enough on their own, and if you stick to a healthy and active lifestyle, you should be able to slow down the progression of your disease from becoming more severe.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Once your lungs require supplemental oxygen therapy, this means that you probably have reduced ability to do daily actives without experiencing severe shortness of breath, your stamina and energy have likely declined to the point where you feel lethargic or even exhausted throughout the day.
While there is no cure for COPD, oxygen therapy is essentially a cure that will boost your stamina and energy levels! Once you get adjusted to the best portable oxygen concentrator designed to fit your needs, you will be able to get back to the sports, hobbies, chores, and other aspects of your life that give you purpose!
Works with you to help improve your exercise tolerance

Exercise is one of the best treatments for slowing down the progression of your COPD. And before you started on oxygen therapy, you probably had no intention of exercising because simple tasks would leave you breathless. Exercise seemed out of the picture.
If you have a lightweight and battery powered portable oxygen concentrator (POC), you can go out for walks and adjust the oxygen level to the appropriate output so that you do not feel as breathless and exhausted while walking.
You can also bring your POC with you to the gym, pulmonary rehabilitation, or anywhere else that you get your daily physical activity in.
And because your blood oxygen levels are more saturated after adjusting to your supplemental oxygen, you will not feel as fatigued and you will be able to build up your exercise tolerance.

This means that you might not be able to walk to the end of the street right now, but if you start walking to and from the kitchen into the living room, and then start down the driveway from your front door, eventually you will have the ability to walk up and down the cul de sac.
By improving your exercise tolerance, you are strengthening your heart, bones, muscle and most importantly your lungs! In order for you muscles to work properly your blood must be capable of delivering oxygen-rich blood to the muscle that you are working out, so in order to do this properly with COPD, supplemental oxygen is a must.
The best portable oxygen concentrators for exercise would be a unit that is lightweight so that you can carry it while you walk, jog, bike, or do aerobics. That being said, one of the lightest portable oxygen concentrator is the Caire Freestyle Comfort, and it only weighs 5 pounds. This POC offers pulse dose oxygen delivery at any rate of 1-5, this means it can deliver anywhere from 210 mil/min (milliliters per minute) to 1050 ml/min of oxygen.
The Freestyle Comfort is a wonderful option for COPD patients that need supplemental oxygen for exercise, and throughout the day and if you do not require more than 1050 ml/min of oxygen.
But many COPD patients require a continuous flow of oxygen to start or continue to exercise, others just require a higher pulse dosage.
In the case of the latter, the Respironic SimplyGO portable oxygen concentrator is an option for people who need a pulse flow settings 1-6 or continuous flow settings 0.5-2.0 LPM. This unit weights almost 10 pounds, which is slightly heavier than the other units we have discussed in this article, but that is nothing to shy away from!
You can use your POC with a portable travel cart, and research has shown the travel cart makes it much easier for a patient to bring their oxygen with them. For example, it can take less energy to pull an 18 pound unit behind you than it takes to carry a 5 pound machine so there's no need to be afraid of the larger machines.
No matter what your oxygen requirements are, a certain amount of exercise is right for you. It is up to you to take the initiatives and start somewhere where you can build up strength and endurance, and with the help of the right oxygen equipment, you can get anywhere!
Strengthens muscles, joints, and bones
Similarly to the section above about exercise, oxygen therapy can help to strengthen your muscles, joints, and bones. Now, it is important to understand that using your portable oxygen concentrator or any form of oxygen therapy will not strength your body on its own, simply by you breathing it in.
However, by adjusting and adapting to your oxygen therapy, this will give you the “tools” you need to be successful in training, exercising, and building strength.
Allows you to travel worry free
While there is no direct “symptom” of COPD that says you cannot travel, the condition does impose a lot of challenges when it comes to travel, whether it's traveling by car, airplane or boat.
The only “cure” for travel with COPD when you need oxygen therapy, is a portable oxygen concentrator. This is because if you have a liquid oxygen tank or a gas cylinder that you rely on most of the day and night, you are not allowed to travel by plane with one of these oxygen tanks.
A portable oxygen concentrator is FAA approved! This means that you can bring your POC on the airplane with you.
The SeQual Eclipse 5 portable oxygen concentrator may be heavier than other POCs like the Inogen One G3, G4, and G5, but this unit is still very easy to travel with and perfect for everyday use. It comes with a wheeled travel cart that makes pulling your concentrator behind you seem effortless.

The travel cart is equipped with oversized wheels, an elevated platform, and a telescopic handle. The oversized wheels and elevated platform make going up curbs and stairs a breeze. They also help protect your concentrator from water when you have to go over puddles or when it’s snowing.
The telescopic handle lets you adjust the travel cart to the height that is most comfortable for you! And if you ever need to store your concentrator the handle slides all the way down and locks. So if you’re traveling you can keep your SeQual on the travel cart and it will still fit underneath the seat in front of you!
If you are eager to get back to traveling, it is time to look into which POC will meet your oxygen requirements.
Helps you sleep more soundly

Oxygen therapy is shown to improve the quality of your sleep. This is because the lack of oxygen can wake you up while you are in the REM cycle of your sleep.
Many people with COPD also have obstructive sleep apnea. Therefore, you probably already use a CPAP or BiPAP machine while you sleep to keep your airways open and keep them from collapsing with every inhale and exhale.
If so it is important to have a POC that is compatible with your CPAP and BiPAP machine.
No matter what your oxygen requirements are at night, LPT medical has the right unit that will work for you, and all of our units can hook up to your CPAP and BiPAP machine. That being said it is very important you talk to your doctor about using oxygen at night, and whether or not this decision is right for you.
Can add years to your life

COPD is a chronic illness, meaning there is no cure, and therefore the disease will progress into a more severe state. Nevertheless, there are plenty of lifestyle changes, treatments, medications, and therapies that will slow down the progression of your disease, thereby adding years to your life.
By far, the most important benefit of long-term oxygen therapy (LTOT) is that it may prolong your life, especially if you have COPD with severe resting hypoxemia (low levels of oxygen in your blood) and/or you use oxygen continuously rather than just at night or sporadically.
A combination of healthy choices and medication will get you very far in slowing down the progression of your COPD.
Life expectancy for people with COPD can be predicted by assessing body mass index (BMI), airway obstruction, dyspnea (Breathlessness), and your exercise capacity. After these value are taken into account, your doctor can give you an average of year you are expected to live
In the end, the average life expectancy for people with COPD is just that—an average estimation. You can exceed expectations by taking control and addressing the factors that you can change.
Relives headaches and nausea
One of the more obvious symptoms oxygen therapy can relieve, is reducing COPD related headaches and nausea.
Headaches and that nauseous feeling are often caused by the lack of oxygen reaching your brain. This goes for everyone and not just people with COPD. Have you hiked a mountain top,or been to a town at high elevation where the air is thinner? At high altitudes there is less oxygen in the air, and therefore less oxygen you can breath in, and in these condition someone might experience “altitude sickness”
Altitude sickness causes someone to feel dizzy, nauseous and will also induce a painful head all, all because your body is not getting the amount of oxygen it is used to when you are at lower elevations. A simple cure is to relax, and drink plenty of water and avoid alcohol.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
But if you have COPD, drinking water may help your headache or other symptoms, but not always and not for long. Eventually your headaches will not feel better after drinking water and oxygen therapy is the best solution.
Once these pesky symptoms of COPD induced dyspnea are relieved, you can get back to doing the things you enjoy, rather than being held back by a bad headache or feeling nauseous.
Can help to improve your memory

Several studies show that using oxygen at home for more than 15 hours a day increases quality of life, oxygen therapy has good short-term and long-term effects in people who have COPD.
Using oxygen may also improve confusion and memory problems.
Getting back to the daily life you are used to



 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













