If you want to lead a healthier life, you need to be more acutely aware of how your lifestyle choices — and the lifestyle choices of others — affect your long-term well-being. For example, you need to research nutrition in order to make sure that your diet is helping you progress towards your health goals, rather than pushing you farther away from them. But nobody ever said this would be easy. With all the information (and misinformation) that’s out there, it can be pretty overwhelming trying to create a health plan and carry it out.
One thing that can really muddle up this issue and make it even more challenging is being diagnosed with a respiratory ailment like chronic obstructive pulmonary disease (COPD). While it may seem like this will only have an effect on your lungs, your respiratory health actually has a significant impact on your systemic health. For example, in one of our more recent posts, we took a look at how COPD can cause heart problems and swelling in the hands and feet.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
A topic that’s hotly debated these days is how vaping and e-cigarettes should be viewed as a COPD patient. Some people believe that vaping is an effective tool to help smokers wean off their bad habit to something that’s “less dangerous” and “less addictive.” However, on the other side, people believe it’s being used to get younger generations involved in smoking and other drugs. No matter where you stand on vaping, this post aims to clarify misconceptions about vaping and e-cigarettes. We’ll also show you why it’s a good idea to reconsider vaping as a COPD patient or someone who’s at risk of contracting COPD.
What are Vape Pens and E-Cigarettes?
The concept of “vaping” has not been around very long. In fact, the first commercially successful e-cigarette was created in 2003, but it wasn’t introduced to the United States until 2006. And despite the fact that the vaping industry was valued at around $14.05 billion in 2018 and is expected to grow to $29.39 billion in 2022, there still seems to be a lot of confusion about what vaping actually is.

Like most products, e-cigarettes have evolved a lot since they were first introduced; but the basic principles remain the same: a battery-powered heating device is activated when the user inhales. This, in turn, vaporizes the e-liquid which is inhaled as an aerosol which is a suspension of fine solid particles and liquid droplets. The smoke that comes from a cigarette is also considered an “aerosol” because it contains water droplets, but vaping advocates claim that cigarettes are far more dangerous because they release more HPHCs due to their high combustion temperature.
Technically speaking, e-cigarettes and vape pens are essentially the same thing. The main difference is that e-cigarettes are designed to look like real cigarettes and once you use them up, they are disposed of. On the contrary, vape pens are much more popular and they can be recharged and refilled rather than being disposed of. We’re going to take a look at some of the risks associated with vaping, as well as some of the perceived benefits so that COPD patients can make more educated decisions about their lung health.
What are the Risks Associated with Vaping?
Chemicals Found in “Vape Juice”
Just like cigarettes, vape juice contains a whole host of chemicals that will harm your long-term health. We know that cigarettes have around 7,000 different toxic chemicals but when it comes to e-cigarettes, the facts are less clear. Since vape juice is being produced by thousands of companies across the country, it’s difficult to track everything that’s being put into them. According to the American Lung Association, however, these are some of the most dangerous components:

- Nicotine
- Carcinogens - including formaldehyde and acetaldehyde
- Volatile organic compounds (VOCs) like Benzene
- Diethylene glycol
- Diacetyl - known to cause bronchiolitis obliterans (popcorn lung)
- Acrolein - commonly used as a herbicide
- Propylene glycol - used to make paint solvent and antifreeze
An Argument From Ignorance
There’s a common logical fallacy that vaping companies often use to prove the safety of their products. This fallacy is called “an argument from ignorance.” Basically what this comes down to is using a lack of evidence in order to prove that something is true. Most people realize that this is not a valid way to argue a point, but it’s easy to get past someone if they aren’t actively looking out for it.

Vaping companies will claim that their products are safer than cigarettes because there is no evidence that they cause COPD or lung cancer. The problem with this argument, however, is that vaping has not been researched long enough for us to know exactly how it contributes to chronic lung conditions. COPD, in particular, takes several decades to develop and severe symptoms don’t usually manifest until later in life.
Another thing that needs to be researched is the effects of vaping on systemic health. We know that cigarette smoking damages your heart and blood vessels, and it’s a risk factor for many chronic systemic diseases, but vaping hasn’t been researched enough to determine if there is a link. Vaping advocates will claim that, since there are no immediate systemic effects, you have nothing to worry about. Be sure to look out for these logical fallacies next time you’re offered an e-cigarette.

It’s hard not to draw connections between what is going on now with vaping and what happened in the 1930s to 1950s with cigarettes. During those times, cigarettes were often advertised as “physician approved” just because they irritated the throat less than other cigarettes. These claims were based on nothing more than a couple of surveys and they were designed to profit off the general public’s lack of understanding concerning the dangers of cigarette smoking.
Vaping is Addictive
No matter how you slice it, nicotine is an addictive chemical regardless of how it’s consumed. Cigarettes, cigars, chewing tobacco, and e-cigarettes all contain high amounts of nicotine. This chemical is referred to as a “neurotoxin” because it alters the structure and function of the nervous system. Nicotine activates nicotinic receptors in the brain which are intended for the neurotransmitter acetylcholine, responsible for cognitive processing, memory, and attention.
There are nicotinic receptors in every part of the brain, so this is why nicotine has such a wide array of effects. And because the vapor is inhaled to the lungs, the effects are nearly instantaneous. One of the most well-known and concerning parts of the brain that nicotine affects is the nucleus accumbens which is often referred to as the “addiction hub” of the brain. Once nicotine enters this area of the brain, it releases dopamine, the neurochemical that’s responsible for feelings of reward.
E-Cigarette or Vaping Product Use-Associated Lung Injury (EVALI)
In 2019, we saw our first major outbreak of lung illness due to vaping. This new lung condition was dubbed “E-cigarette or Vaping Product Use-Associated Lung Injury (EVALI) by the CDC, and it’s currently being heavily researched. EVALI caused sudden and severe respiratory symptoms in otherwise healthy people, but researchers have determined that the one thing these cases had in common was the use of vaping products containing tetrahydrocannabinol (THC).

Another problem safety concern associated with e-cigarettes is the battery. While traditional cigarettes can cause fires, e-cigarette batteries have caused harm to the user by exploding or causing severe burns. According to VapeDanger.com, the batteries that are used in e-cigs are not tested well enough to ensure their safety and they’re typically designed for things like power tools rather than e-cigarettes.
Vaping as a “Gateway” Drug
One of the downsides that’s often under-discussed when it comes to vaping is its potential to be used as a “gateway drug.” A gateway drug is a drug that may not be extremely harmful in and of itself, but it can lead to someone trying other drugs that are far more dangerous. For example, even though vape juice contains less nicotine than cigarettes, it could make it either for someone to get hooked on traditional cigarettes.
Are There Any Benefits of Vaping?
While there are some perceived benefits to vaping like reducing addiction to cigarettes or saving money, you’ll be much better off if you completely eliminate nicotine use in your life. Since we don’t know the long-term effects of vaping, you’re basically just flipping a coin when it comes to your health. It’s best to assume that the only things you should be inhaling into your lungs are fresh air or any medication that your doctor has prescribed you for COPD treatment such as corticosteroids, bronchodilators, or other medication administered through an inhaler or nebulizer. Even then, these drugs should only be used as prescribed by your doctor.
How Should COPD Patients React to Vaping?
Find other Methods to Quit Smoking
Possibly the most common use for e-cigarettes is as a tool for smoking cessation. Proponents of vaping will say that vaping can act like a nicotine patch or other types of nicotine replacement therapy in order to wean people off of cigarettes. Unfortunately, studies have shown that using e-cigarettes in this way is no more or less effective than other smoking cessation tools. What’s more, there’s a chance that you could become addicted to both cigarettes and e-cigarettes. According to the Truth Initiative, 54.6% of e-cigarette users in 2016 also smoked cigarettes. This would suggest that many people are using vaping as a supplement rather than a replacement for traditional smoking.

The Centers for Disease Control and Prevention (CDC) maintains that the most effective cessation tools include counseling, medications, or some combination of the two. There are several different types of cognitive-behavioral therapy (CBT) that can be used to quit smoking, but the most popular include one-on-one counseling and group therapy. FDA-approved smoking cessation medication includes Chantix (varenicline tartrate) and Zyban (buproprion hydrochloride). Before taking these medications, however, you should speak with your doctor to determine if they’re right for you.

Above all, it’s important to try these other methods of smoking cessation before resorting to vaping. While e-cigarettes may be the most accessible option for many people, they are not proven to be effective at helping you kick the habit, and more importantly, we don’t yet know the long-term effects of vaping on the body. If you have COPD or you’re currently at risk of COPD, you should invest time in behavioral therapy, nicotine replacement therapy, or one of the FDA-approved medications before resorting to vaping.
Focus on your COPD Treatment Plan
If you have COPD, you should be focusing on your treatment plan above all else. This includes things like smoking cessation, supplemental oxygen therapy, a refined diet, and pulmonary rehabilitation. If you’ve smoked for years or decades, you may find it tempting to invest in vaping because it’s often advertised as a “healthier alternative” to smoking. But in reality, vaping will put you at a higher risk of contracting pneumonia, one of the primary causes of COPD exacerbations.

If you spend your time and energy focusing on making positive lifestyle changes, you’re likely to see your nicotine dependency dissipate over time. According to Addictions and Recovery, nicotine stays in the body for about 72 hours and nicotine withdrawal is worst 2 to 3 days after quitting. However, it takes around 3 months for your brain chemistry to return back to normal after smoking. Try to focus on your COPD treatment for this duration of time and you’ll find that it becomes much easier to avoid nicotine products.
Get Outside and Exercise
If you’re still struggling with nicotine withdrawal, consider exercising more frequently. According to Medical News Today, exercise is one of the best-known ways to combat nicotine cravings, and the best part is that it doesn’t require you to commit to a high-intensity exercise routine. Even 10 minutes each day of moderate exercise can significantly reduce the chance that you’ll fall back on your smoking cessation plan.
.jpg)
Understand the Financial Burden of Vaping
One of the claims you’ll hear thrown around is that vaping is “95 percent healthier and 40 percent cheaper than smoking.” While this is certainly an interesting statement, it’s not based in reality. First and foremost, very little research has been done on vaping especially when it comes to the long-term effects on the lungs. So, it’s very difficult to prove or disprove that vaping is “95 percent safer.”
Secondly, the cost of smoking or vaping varies greatly. Some people smoke several packs of cigarettes a day while others smoke only once or twice a week. When they say that vaping is “40 percent cheaper,” they are usually comparing the lower estimates of vaping with the upper estimates of smoking. Be careful when you hear claims like this, especially if they’re coming from vaping companies.
Conclusion
Vaping is a trend that’s been increasing in popularity for years. Although it’s mainly used by young adults, many older adults and seniors are embracing it as a “healthier alternative” or “cessation tool” for traditional cigarettes. If you suffer from COPD or another chronic respiratory disease, you should be wary of these claims and focus on healthy lifestyle choices that are backed by many decades of research rather than several years of research.
Here at LPT Medical, we only sell products that are medically proven to help patients with COPD. Most people with COPD will be prescribed supplemental oxygen and we are happy to provide lightweight and durable portable oxygen concentrators that can keep you moving despite your respiratory condition. Whether you’re looking for the Caire FreeStyle Comfort, Inogen One G5, Respironics SImplyGo, or any other affordable portable oxygen device, we are here to help.
Oxygen is one of the most abundant gases in the atmosphere making up around 21 percent of the air that we breathe. All organisms need oxygen to survive because it plays a pivotal role in a process called cellular respiration. During this process, glucose from the food that we eat reacts with oxygen to form adenosine triphosphate (ATP), the primary energy carrier in living organisms.
But it’s not just about getting oxygen in your lungs; it’s also about getting the right amount of oxygen. Everyone should have a blood oxygen level between 75 and 100 millimeters of mercury (mm Hg), so if you have a chronic respiratory illness like COPD or pulmonary fibrosis which reduces the amount of oxygen in your bloodstream, you’ll need to rely on supplemental oxygen therapy.
Despite being necessary for human life, medical oxygen is considered a “controlled substance” by the U.S. Food and Drug Administration because it poses several risks if it is used incorrectly. Getting too much oxygen in your blood can result in a condition called oxygen toxicity (hyperoxia). Most cases of oxygen toxicity lead to headaches, confusion, and sleepiness, but continued exposure to high partial pressures of oxygen can cause permanent damage to your lungs and body.
While it may seem scary being prescribed supplemental oxygen, it’s not all bad! If you use oxygen exactly how it was advised by your doctor you’ll find that supplemental oxygen is very safe. Here at LPT Medical we also strongly recommend using a portable oxygen concentrator which is much safer and more reliable than other oxygen devices such as oxygen tanks, liquid oxygen tanks, and stationary oxygen concentrators.
Stick around if you’re interested in learning more about oxygen concentrator safety and feel free to leave any questions or comments in the section below.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why Are Portable Oxygen Concentrators Safer?
First off, you may be wondering why portable oxygen concentrators are considered “safe” in the first place. After all, they put out medical grade oxygen just like oxygen tanks, liquid oxygen tanks, and stationary oxygen concentrators. So, you might assume that it comes with all the same risks that are associated with these other devices. However, this is not necessarily the case.
.png)
Portable oxygen concentrators are the most advanced oxygen delivery devices ever created. They’re a product of many years of innovation and research, so it goes without saying that their safety features are more advanced as well. One of the main safety features are modern portable oxygen concentrators is something called pulse dose oxygen delivery. This is a technology that closely tracks your breathing rate and only delivers oxygen when it detects an inhalation.
The main purpose of this is to conserve energy and make your batteries last longer, but it has some major safety benefits as well. If you happen to drop your nasal cannula, the tubing that delivers oxygen to your nose, the flow of oxygen will stop. Since oxygen is an oxidizer, meaning it makes everything it comes in contact with more flammable, this is a groundbreaking feature. Unfortunately, with older oxygen delivery systems such as oxygen tanks or liquid oxygen tanks, this is not possible.

Another major safety feature of portable oxygen concentrators is their size and shape. POCs tend to be very small and box-shaped meaning they’re easy to carry under your arm and they’re not likely to hurt anyone if you accidentally bump into them. Since they’re so light, you’ll never have to wheel them around with a carrying cart which can be a huge tripping hazard for you and people around you.
As you can tell, oxygen manufacturers have worked hard to make POCs as safe as possible, but there are still some things you should look out for. Without further ado, let’s take a look at 7 safety tips for using a portable oxygen concentrator.
Avoid Smoking Near Your Concentrator
Despite smoking causing about 80 percent of COPD cases, many people still smoke when they’re diagnosed. Every doctor will recommend that you quit smoking as soon as possible because continuing to inhale smoke and chemicals will lower your immune system and make you more likely to experience symptom flare-ups and life-threatening exacerbations. But these are just a few of the reasons to quit smoking.

Another very important reason to quit smoking is that they are a fire hazard, especially when you’re using supplemental oxygen therapy. According to the National Fire Protection Association, there were about 18,000 home fires started by cigarette smoking between 2012 and 2016 which accounted for about 5 percent of the total fires. And smoking near your concentrator will not only increase the chance that you’ll start a fire, but it could make it burn more.
While you should not be smoking at all, regardless of whether you’re using supplemental oxygen or not, it’s especially dangerous to smoke next to your POC. Smoking can leave behind embers and ashes that can easily start a fire in the wrong circumstances. You should also take the time to speak with anyone else who lives in your home to make sure they don’t smoke around your oxygen concentrator. Some people prefer putting up “no smoking” signs throughout their home in order to remind visitors not to light up a cigarette without going outside.
![]()
Keep Your Concentrator Dry
Portable oxygen concentrators are electronic devices just like your cell phone, computer, or tablet. What this means is that they are extremely susceptible to water damage. There are many sensitive electronic components inside of the concentrator, so if you submerge it in water or water enters through any of the vents, then it could permanently damage your device. There’s also a chance it could harm you if you’re not careful.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The best way to keep your unit dry is to use some type of carrying case. Fortunately, if you are using a popular POC like the Inogen One G5, the Caire FreeStyle Comfort, or the Respironics SimplyGo, there are plenty of options available to you. Even older POCs like the Inogen One G3 have new carrying cases that can keep them dry. The GO2 Carryalls, for example, are made of genuine leather and they fully cover the device preventing it from getting wet. However, there are mesh patches on the side that keep the vents clear of obstruction, so it is possible to let water in if you’re not careful.

Unfortunately, we’re unlikely to see waterproof portable oxygen concentrators anytime in the near future. POCs work by drawing in ambient air and filtering out unnecessary gases like argon and nitrogen so all of these devices are vulnerable to water damage.
Store Your Concentrator in a Secure Place
Another safety consideration to make when purchasing a portable oxygen concentrator is the way you store it. Some people like to have a stationary oxygen concentrator to use in their home and a POC to use when they go out so it’s important to have a plan as to how and where you’re going to store it.

First and foremost, you should store your POC in a well-ventilated area. What this means is that you shouldn’t put it in a confined space because it could damage the unit and create an unnecessary fire risk.
Use the Right Oxygen Tubing
Oxygen tubing is very important when it comes to your safety. Oxygen tubing is what connects to your portable oxygen concentrator and delivers oxygen to your nose. The most common problem people have with oxygen tubing is that it’s too long. If this happens it may drag on the ground and cause a tripping hazard for you and the people around you.

One way to solve this is to invest in tidy tubing. This is a type of oxygen tubing that’s coiled so that the tubing is only as long as you need it to be. Whether you carry your portable oxygen concentrator under your shoulder or you wheel it behind yourself using a rolling cart, the tubing won’t be dragging or dangling in a way that could compromise your safety.
Another safety tip related to oxygen tubing is to check it regularly for signs of damage. If your oxygen tubing is kinked or it has a hole in it, you probably won’t be receiving the right amount of oxygen that you need to stay healthy. If you’re using a pulse dose concentrator which relies on breath detection in order to deliver oxygen at the optimal moment, damaged oxygen tubing could negatively impact this. It’s a good idea to have some backup oxygen tubing and nasal cannulas on hand at all times in the event that something goes wrong.

Another thing you should be doing is cleaning your oxygen tubing regularly. Over time, oxygen tubing can gather bacteria which can lead to you becoming sick if you’re not careful. Since infection is the top cause of COPD exacerbations and we’re in the middle of a pandemic, this should be a top priority for you.
Have Back-Up Batteries on Hand
Although portable oxygen concentrator batteries are extremely reliable, you still shouldn’t go out of the house without at least one backup battery. The reason for this is because you may encounter a situation where you need to stay out of the house longer than you thought and you won’t want to stress about running out of oxygen when you’re not near an outlet. Fortunately, most POC batteries are very lightweight so you won’t be adding a lot of extra weight if you need to carry a couple of extra batteries.
If you are planning on taking a flight, be aware that most airlines will require you to have at least 1.5 times the flight duration in battery life. So, for example, if your flight is 4 hours long, you will need to have at least 6 hours of battery life available to you. This rule is in place to make sure you account for any delays that might occur during your flight. Be sure to contact your airline at least 48 hours before a flight to notify them of your oxygen use and ask about any other safety precautions.
Plan for Power Outages
Power outages are a rare occurrence but they’re still a reality. Since portable oxygen concentrators require electricity to run, you need a power source in order to charge your batteries. One thing many oxygen manufacturers advise is that you contact your utility company and ask about priority service. Some companies have safety measures in place to ensure that people who own oxygen concentrators or other medical devices that rely on electricity can always have access to electricity. Electricity generators are the most common way to do this. For more information, check out this site.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Another thing you should do to plan for power outages is to have an action plan. An action plan, just like the name suggests, will help you be prepared to take action in an urgent moment when you have little time to think about what to do. For example, if your power goes out during a storm, you may need to go without power for several days or upwards of a week. A power generator likely won’t last this long so you’ll need to have an alternative course of action.
Read Your Product’s User Manual
Last but certainly not least, you should have a good grasp on your portable oxygen concentrator’s user manual. The user manual is the paper booklet that is packaged with your device and it describes important information like how to use your device, how to troubleshoot any errors, and most importantly, information about how to use the device safely. Every POC works slightly differently, so even if you have used a POC in the past, it’s a good idea to read through your whole user manual and fully understand it.

Conclusion
All around, portable oxygen concentrators are the safest supplemental oxygen devices on the market. They’re lightweight, have a small form factor, and they’re extremely reliable. But since they deliver medical grade oxygen, there are some inherent precautions you should take before using them.
Above all, your oxygen manufacturer and user manual will be the best resources for you. Every portable oxygen concentrator operates a little differently, so it’s best to fully understand how it works before you begin using it. However, if you have any questions, don’t hesitate to leave a comment or reach out to us.
%20(1).png)
Around 70 million people in the United States suffer from some form of sleep disorder such as narcolepsy, insomnia, or obstructive sleep apnea (OSA). These conditions can appear anytime during our lives and they have a significant impact on our general health and well-being.
Unfortunately, there are many obstacles that prevent people from receiving the treatment they need for sleep disorders. Chief among them is the fact that many people don’t even realize they have a problem in the first place. Symptoms such as daytime sleepiness, restlessness, or difficulty concentrating are often shrugged off as an inevitable part of life.
Another obstacle preventing sleep disorder patients from getting the help they need is confusion about their disease and the treatment options that are available to them. People hear terms like CPAP, BiPAP, EPAP, or APAP, but they never actually receive a simple explanation of what these terms mean and how they relate to each other.
In this post, we’re going to clarify any confusion about these terms as well as how they pertain to other types of respiratory therapy like supplemental oxygen. Remember to check in with your doctor if you have any questions or if you are thinking of making any changes to your treatment plan.
What is Obstructive Sleep Apnea (OSA)?
There are several types of sleep apnea, but one of the most common is obstructive sleep apnea. OSA occurs when the muscles in your throat relax intermittently at night causing you to stop breathing and lose sleep. It’s estimated that about 22 million Americans have some form of sleep apnea.
.jpg)
Obstructive sleep apnea is notoriously difficult to self-diagnose because the patient will likely have no recollection of what caused them to lose sleep or wake up frequently at night. In fact, many undiagnosed OSA patients believe that they get great sleep each night. This is why it’s important to speak with your doctor about having a sleep study done so that a medical specialist can examine your sleep patterns and determine if OSA is present.
A sleep study (polysomnography) is a non-invasive exam where you will stay in a sleep center overnight. During this study, electrodes will be placed on your head that measure brain activity, you will have a pulse oximeter attached to your finger which measures blood oxygen levels, and a belt will be wrapped around your chest to monitor breathing.
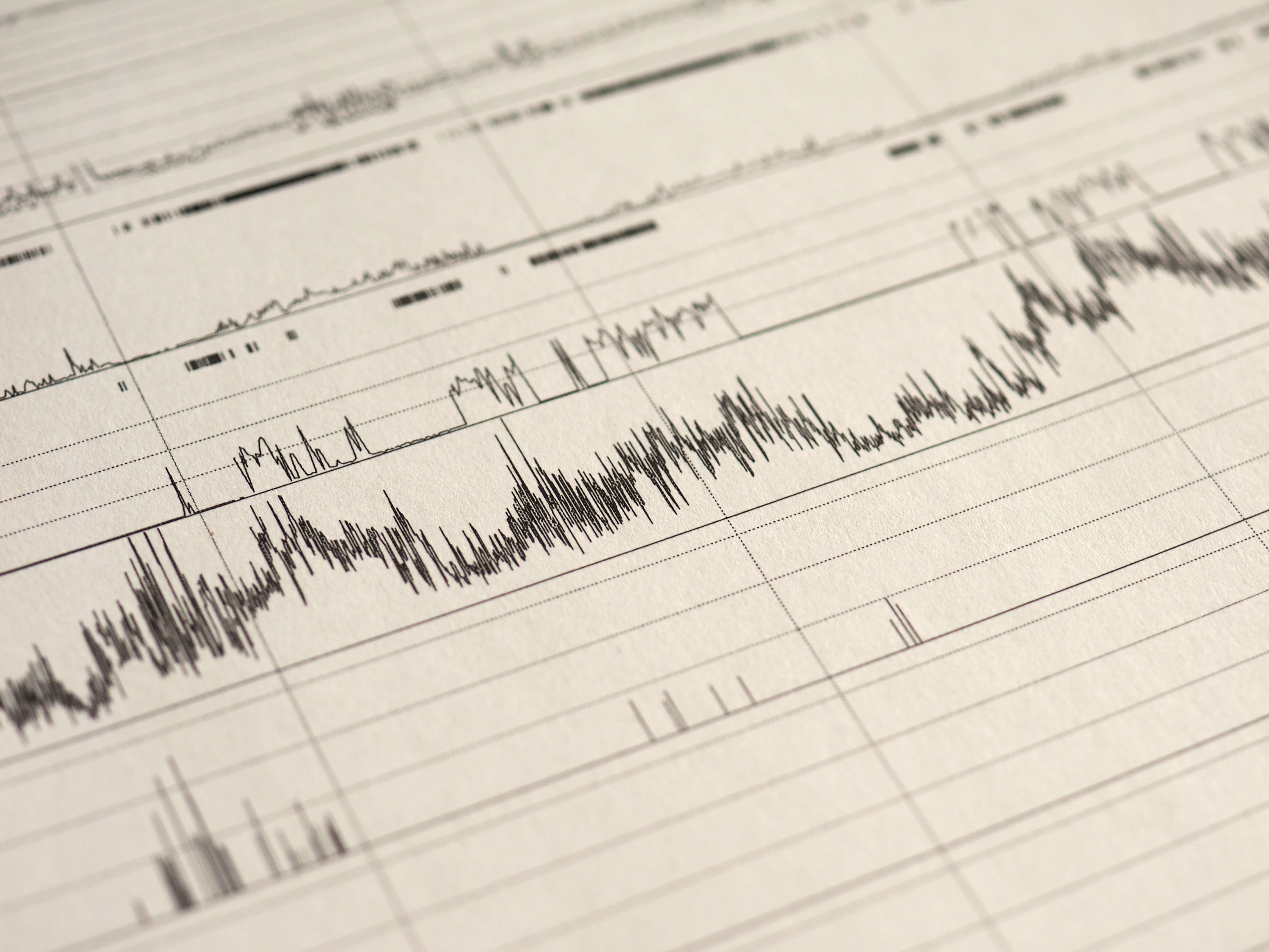
This is one of the most effective ways for a health professional to diagnose OSA because it will show them exactly what’s going on in your body during sleep. For example, if your breathing is interrupted, your blood oxygen levels will likely drop and you’ll wake up. Occasional sleep interruptions are normal, but if it’s happening frequently throughout the night there is a more serious underlying issue at play. According to worldsleepday.org, patients with severe sleep apnea may wake up more than 30 timers each hour.
Why is it Important to Treat Sleep Disorders?
For many people, the term “sleep disorder” doesn’t bring about a huge amount of urgency. You may be thinking that a sleep disorder can be cured with an extra cup of coffee in the morning or an energy drink for lunch, but the issues extend far beyond a little extra drowsiness in your day-to-day life.
Not only can a sleeping disorder sap your energy, but it’s a risk factor for many different life-threatening illnesses as well. According to the Mayo Clinic, complications of obstructive sleep apnea (OSA) include high blood pressure, heart problems, metabolic syndrome, and liver problems.
Furthermore, a medical report published in the Journal of Clinical Sleep Medicine states that sleep apnea increases the risk of heart failure by 140 percent and the risk of stroke by 60 percent. What’s more, it states that obesity is by far the most significant risk factor with about 60 to 90 percent of sleep apnea patients being obese. Other risk factors include cigarette smoking, alcohol consumption, and diabetes mellitus.

Knowing this information, it’s not hard to see how sleep disorders are a much more serious condition than most people realize. While it may only manifest itself with minor symptoms in your daily life, its impact on your long-term health is far worse. It can also contribute to other unhealthy lifestyle choices such as a poor diet or exercise routine, so it’s important to seek out appropriate treatment options.
What is Continuous Positive Airway Pressure (CPAP)?
Continuous positive airway pressure is a therapy that is used to treat obstructive sleep apnea. It’s considered the first non-invasive treatment because, prior to the 1980s, the only effective treatment for OSA was tracheostomy, a surgical procedure that involves making an incision into the trachea in order to bypass an obstructed airway.

The first CPAP machine was invented by Dr. Colin Sullivan in 1981. It works by administering a gentle stream of pressurized air through oxygen tubing that’s connected to the patient’s nose. At night, the patient can breathe freely while the pressurized air prevents the throat from closing up during sleep. Although modern CPAP machines use the same principles as the one created in 1981, they are much quieter and more comfortable, allowing the patient to get a better night’s sleep.
One important thing to note is that CPAP is not the same thing as oxygen therapy. While CPAP does blow air into the nose, it uses ambient air including oxygen, nitrogen, and all the other gases that we normally breathe rather than medical grade oxygen. The sole purpose of CPAP therapy is to keep the airways open while you sleep.

While CPAP machines deliver constant pressure, this pressure can be changed when you aren’t using the device. All CPAP devices use the measurement centimeters of water (cmH20) which is the same unit that lung pressure is measured in. Most patients require between 6 and 14 cmH20 and the average setting is 10 cmH20, however, the setting you use will depend entirely on your condition and the setting that your doctor prescribes. It’s also important to note that every CPAP machine has different capabilities, so you’ll want to make sure it meets your needs before purchasing it.
What is Bilevel Positive Airway Pressure (BiPAP)?
Although CPAP is still the most widely used PAP therapy device to this day, one of the major complaints about it is that it’s difficult to exhale against the air put out by the device. This typically isn’t a problem for someone with healthy lungs, but if you suffer from a low FEV1/FVC ratio, this could be a different story. In simple terms, FEV1/FVC ratio measures your lungs’ ability to exhale effectively. Low FEV1/FVC is often a sign of obstructive lung diseases like chronic bronchitis or emphysema.

BiPAP or Bilevel positive airways pressure is an alternative to CPAP which has two different pressure settings: one for inhalation (inspiratory positive airways pressure) and one for exhalation (expiratory positive airway pressure). The BiPAP machine will automatically detect whether you’re inhaling or exhaling and administer the pressure accordingly. Typically, a higher pressure will be applied when you’re inhaling.
CPAP With C-Flex versus BiPAP
Many people get confused when they hear about C-Flex which is a special feature that comes with some newer CPAP machines. This setting will help decrease the expiratory pressure by up to 3 cmH20. So, in other words, it’s more of a comfort feature that doesn’t completely eliminate the expiratory pressure. On some devices, this feature is called “expiratory pressure relief” or “EPR” for short.
What is Automatic Positive Airway Pressure (APAP)?
APAP is the third and final category of positive airway pressure device. Unlike CPAP and BiPAP, APAP machines automatically adjust airway pressure depending on what is needed at any given time. For example, if the APAP machine detects that your airways have closed, it will increase the pressure to open them up. Similarly, it can detect other episodes like hypopnea (slow and shallow breathing), flow limitation (when an increase in esophageal pressure is not accompanied by a flow increase), or snoring which can also disrupt sleep.
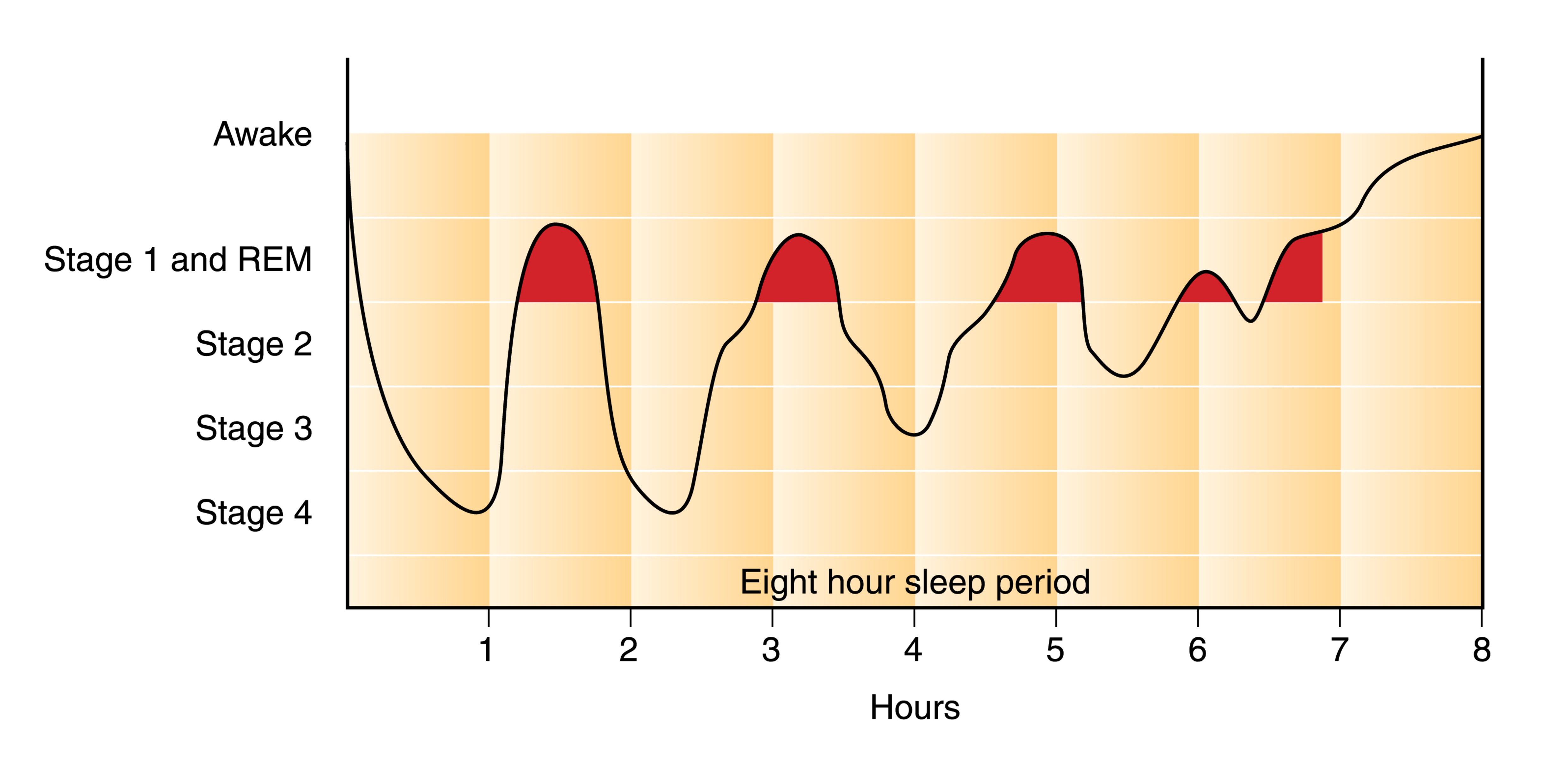
One of the obvious benefits of APAP is that it’s significantly more adaptable than CPAP or BiPAP. It contains a lot more technology and as a result, it’s often better for treating complex sleep apnea conditions. One complex form of apnea, REM-related obstructive sleep apnea occurs specifically during the rapid eye movement (REM) phase of sleep.
Another type of apnea that can be remedied with APAP is positional apnea. This is when your apneic episodes can be attributed to one or more specific sleeping positions. If you tend to move around a lot at night, the APAP machine will recognize this and adjust accordingly.
What is Supplemental Oxygen Therapy?
While supplemental oxygen therapy is often confused with CPAP, BiPAP, and APAP, it is an entirely different therapy that is used to treat respiratory conditions rather than sleep disorders. Oxygen therapy is the administration of medical grade (high purity) oxygen via a nasal cannula. Oxygen therapy ensures the lungs are fully saturated so that a patient can maintain oxygen levels in their blood.

Most commonly, oxygen therapy is used to treat chronic obstructive pulmonary disease (COPD). This is an umbrella term used to describe two different chronic diseases: emphysema and chronic bronchitis. Emphysema is characterized by swollen and damaged alveoli. These are the small air sacs in the lungs that are responsible for the transfer of oxygen and carbon dioxide to and from the blood. Chronic bronchitis is characterized by inflamed and swollen bronchial tubes, the small airways in the lungs.
COPD is one of the most common progressive lung diseases in the world, affecting an estimated 328 million people. Although it’s primarily caused by cigarette smoking, some people contract COPD due to a rare condition called alpha-1 antitrypsin deficiency. COPD is characterized by a chronic cough, chest pain, increased phlegm and sputum production, and exercise intolerance.

Depending on the severity of COPD that a patient has, they will need different flow rates of oxygen. Supplemental oxygen is measured in either liters per minute (LPM) or milliliters per minute (ml/min) depending on the oxygen device that is being used.
What Kind of Oxygen Devices Are There?
There are several different types of oxygen device: oxygen tanks, liquid oxygen tanks, stationary oxygen concentrators, and portable oxygen concentrators. Oxygen tanks are the oldest type of oxygen therapy and they work by storing oxygen at high pressures inside of an aluminum tank. Liquid oxygen tanks are similar to regular oxygen tanks but they’re stored in liquid form meaning they need to be kept at very low temperatures.

Oxygen concentrators are electronic oxygen therapy devices that take in ambient air and remove unnecessary gases like nitrogen and argon, then it puts out medical grade oxygen through a nasal cannula. Stationary oxygen concentrators need to be plugged into a wall outlet at all times but portable oxygen concentrators run off lightweight batteries that can be taken anywhere.
Pulse Dose versus Continuous Flow
There are two different delivery methods for oxygen: continuous flow and pulse flow. The best way to think of these is like the difference between a drinking fountain and a water bottle. Drinking fountains are like continuous flow oxygen concentrators because they put out a constant stream of water irrespective of how much you drink. On the other hand, pulse flow concentrators are like water bottles because you’re drinking all of the water that comes out of the bottle.

Pulse dose oxygen concentrators are more advanced than their continuous flow counterparts because they are able to detect your breathing rate and deliver oxygen at the right moment similar to how an APAP machine changes the pressure in your airways based on your breathing and sleep patterns. However, in certain situations, your doctor may advise you to only use continuous flow oxygen machines. One of the best pulse flow portable oxygen concentrators currently available is the Caire FreeStyle Comfort and one of the best continuous flow portable oxygen concentrators is the Respironics SimplyGo.
How are PAP Therapy and Supplemental Oxygen Therapy Related?
Although PAP therapy and oxygen therapy are used to treat entirely different diseases, that doesn’t mean that they aren’t related. Both therapies are used to improve breathing and to promote lung health as well as general well-being. And in certain situations, you may need to use both CPAP and oxygen therapy at the same time.
What is COPD-OSA Overlap Syndrome?
Just like the name suggests, COPD-OSA overlap syndrome is when symptoms of both COPD and OSA are present. In other words, a patient can have both damaged lungs and airways that collapse during sleep. As you can imagine, this is a pretty bad combination and it can lead to a lot of complications when it comes to getting a good night’s sleep.

There is no evidence to suggest that OSA causes COPD or vice versa, but a COPD patient who is obese or smokes will be at a higher risk of also contracting OSA. It’s important to remember that COPD is an “obstructive” lung disease, not a “restrictive” lung disease. What this means is that it affects the lung’s ability to expel air rather than inspire air. This is why COPD patients with OSA will likely be prescribed an APAP machine rather than a CPAP machine because it doesn’t add any unnecessary strain on their lungs when they expel air.
They Both Require a Prescription
Another similarity between oxygen therapy and PAP therapy is that they both require a prescription. Under the U.S. Food and Drug Administration, CPAP, BiPAP, and APAP machines are considered “Class II Medical Devices.” This means that these devices have potential risks and you’ll need a prescription to purchase one.

Similarly, oxygen is considered a controlled substance by the FDA, and as such, any device that puts out high purity or medical grade oxygen is regulated. If you decide to purchase an oxygen tank, liquid oxygen tank, stationary or portable oxygen concentrator, you will need to provide a prescription from your doctor.
How to Connect an Oxygen Machine to CPAP
If you have COPD-OSA overlap syndrome, you may need to use both oxygen therapy and PAP therapy at the same time. If this is the case, you’ll need to make sure that your PAP device and oxygen device are compatible. Most CPAP machines are compatible with oxygen machines, but you’ll need to make sure you have a continuous flow oxygen concentrator. Pulse dose concentrators like the Inogen One G5 rely on your breathing to deliver oxygen correctly and CPAP will mess with this.

Your oxygen tubing will connect to the CPAP between the mask and the input valve, but if there is no place to connect them, then you will need to purchase an oxygen bleed adapter. Once the devices are connected you should make sure both devices are on before you go to sleep at night. If your nasal passages get dry while using both the CPAP machine and oxygen machine, you can typically purchase a humidifier for either unit that will allow you to sleep more comfortably.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Conclusion
Although CPAP therapy and oxygen therapy are commonly confused, they are not the same thing. CPAP, BiPAP, and APAP are used to treat obstructive sleep apnea, one of the leading sleep disorders in the country. Oxygen therapy, on the other hand, is used to treat COPD and other chronic respiratory diseases.
However, under certain conditions such as COPD-OSA overlap syndrome, your doctor may advise you to use both of these therapies. It can be confusing trying to pick out the right CPAP machine or oxygen concentrator, especially if you want to ensure that they’re compatible with each other. To make this process as easy as possible, reach out to our respiratory specialists here at LPT Medical and we’ll walk you through it and get you the exact device you’re looking for.
.png)
Life is full of obstacles that we need to overcome. Whether it be an obstacle in our career or personal life, success always comes from our ability to adapt to these circumstances and find a way past them. Thankfully, you never have to feel “alone” when it comes to facing these challenges. There’s no shame in relying on friends and family when times get tough, especially if it’s your health that’s at stake.
Chronic obstructive pulmonary disease (COPD) is one life-changing obstacle that millions of Americans are faced with each year. If you’re diagnosed with this common lung disease, you will need to plan your life around your treatment plan which could involve drastic changes to your diet or exercise routine, as well as kicking bad habits like cigarette smoking, a poor sleep schedule, or overeating.
While this may sound like an immense barrier to overcome in your life, by breaking it down and focusing on one thing at a time, you’ll find that it’s much easier than you thought. Aside from relying on friends, family, and healthcare professionals, you should also make it a priority to rely on modern technology. At first, it may seem easier to stick with technology that you know how to use and that you’re comfortable with, however, over time you’ll find that modern technology is not as scary as it seems.
In this post, we’ll take a look at 7 different barriers you’ll be able to overcome with the help of a portable oxygen concentrator. If you have any questions, don’t hesitate to speak with one of our respiratory specialists.
How Portable Oxygen Concentrators are “More Advanced”
If you think about the phone that’s in your pocket or the computer that’s sitting on your desk at home, you might be amazed at how far these devices have progressed in the past decade. These devices have all progressed in a way that allows us to accomplish more with less effort. And in some cases, they can even automate processes that were once tedious chores.

Oxygen delivery devices have progressed in much the same way. Unlike old bulky oxygen tanks, modern portable oxygen concentrators afford COPD patients the opportunity to accomplish more in their day-to-day lives with less hassle. But in order to accomplish that, oxygen manufacturers how to pursue a new type of oxygen delivery that didn’t involve storing oxygen inside a tank.
.png)
Oxygen concentrators work by generating oxygen from ambient air. They use intake vents to draw in surrounding air, then remove impurities like nitrogen and argon. It then puts out medical-grade oxygen that the user inhales through the nasal cannula. While this may sound complicated, the whole process is automated for you and all you need to worry about is learning how to turn the device on or off and adjust the flow setting which determines how much oxygen you receive. Without further ado, let’s take a look at some of the obstacles you’ll overcome with a portable oxygen unit.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Staying Active
Exercise plays a crucial role in weight management, improving mood, boosting energy, promoting better sleep, and reducing your risk of developing diseases like diabetes and arthritis. Unfortunately, many people are under the impression that the need to exercise dissipates as we age or if we develop a chronic condition like COPD. This could not be farther from the truth!

In fact, according to the Centers for Disease Control and Prevention (CDC), regular physical activity in seniors reduces your risk for common conditions like coronary heart disease, high blood pressure, and colon cancer. It’s also one of the best ways to combat feelings of loneliness or helplessness which are common in old age.
The good news is that you don’t need to commit to a rigorous exercise routine in order to benefit. Studies have shown that even a small amount of moderate exercise each day will have immense benefits for our health. What’s more important than the intensity of the exercise is how frequently you do it. Maintaining a sedentary lifestyle for more than a couple of days or weeks on end will inevitably cause your health to decline.

If you have COPD, you know that exercise can be a huge barrier in the way of staying healthy. Even patients with moderate (stage 2) COPD have around 50% to 79% lung function (FEV1), so it’s no surprise that many people with COPD become breathless after a small amount of exercise. This is why it’s absolutely vital that you keep up with your supplemental oxygen needs because it will ensure that your blood oxygen levels remain stable.
.jpg)
According to Healthline.com, a normal blood oxygen level is between 80 and 100 millimeters of mercury (mm HG), but it’s important to first check in with your doctor to make sure this is best for you. Either way, if you want to maintain your oxygen levels, you’re going to need a reliable portable oxygen device that you can take with you whenever you exercise. Since portable oxygen concentrators are much lighter and smaller than their alternatives, most people prefer them if they’re looking to stay active.
Doing Chores Around the House
Doing chores isn’t something that most people look forward to. They can be quite tedious and take time away from things that are much more entertaining. But COPD patients often have a unique perspective when it comes to chores because they can help them feel more in control and independent in their daily lives.

Simple tasks like taking out the trash, washing the dishes, or folding clothes can be very important for COPD patients who may feel anxiety or loneliness. These seemingly menial tasks can help keep your mind occupied in your downtime, keeping your mind off your disease and any other negative thoughts that you might come across. They can also help you keep your living space clean by reducing clutter.
Modern portable oxygen concentrators make it much easier for COPD patients to get around their own homes than old outdated oxygen tanks do. In the past, oxygen patients would need to purchase an extra long nasal cannula that they could drag around from room to room. This can be a pain, not to mention it’s also very dangerous because it can be a tripping hazard.
Traveling Long Distance
Long-distance travel is a huge barrier for many people with COPD. Since oxygen tanks are illegal on commercial flights for safety reasons, those with a respiratory impairment are required to take slower forms of transportation such as driving or riding a train or bus. If your goal is to visit your friends or loved ones across the country, you may be better off letting them come to you.
.jpg)
On the other hand, if you use a portable oxygen concentrator, you’ll be happy to find that no form of transportation is off-limits. Portable oxygen concentrators are approved by the Federal Aviation Administration (FAA) for in-flight use. All that is required is that you bring enough batteries to last you 1.5 times the length of the flight in duration. So, for example, if your flight was two hours long, you need three hours’ worth of battery. This is not a problem, however, considering concentrators like the Caire FreeStyle Comfort and Inogen One G5 can provide you with well over 10 hours of battery life on one charge.
Keeping up With Your Friends
A couple of months ago, we wrote an article titled, “7 Social Benefits of Owning a Portable Oxygen Concentrator.” In this post, we discussed the social stigma that’s often associated with supplemental oxygen therapy. From an outside perspective, oxygen users are often seen as less capable than their counterparts due to the fact that they have to lug around a bulky oxygen tank. But when they switch over to a portable oxygen concentrator, this stigma often goes away.

Not only are oxygen concentrator owners perceived as “more capable,” but they actually are more capable. Portable oxygen concentrators like the Inogen One G3 can easily be slung over your shoulder and carried around all day without you experiencing shoulder or back pain or shortness of breath. What’s more, it offers a variety of carrying options that can help you conceal your device and make it more inconspicuous.

The GO2 Carryall is one such carrying option that any G3 owner can enjoy. This is a leather bag specially designed to fit the Inogen One G3. Instead of simply protecting the G3, however, they also look very stylish and match many different wardrobes. It’s also very easy to access the G3 control panel if you need to adjust your flow setting, check your battery life, or turn the device on or off.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Avoiding Hospital Visits
There’s no doubt about it, being admitted to the hospital constantly due to flare-ups or exacerbations is exhausting, time-consuming, and it can put a huge strain on your financial well-being. According to businessinsider.com, the average stay at a hospital is around $10,700. In other words, you can eat through your savings real fast if you don’t come up with some plan to reduce medical emergencies due to COPD.

Simply put, POCs help you prevent exacerbations and flare-ups because they offer a reliable source of oxygen no matter where you are in the world. Whether you’re sitting at home or you’re exercising at your favorite park, these oxygen machines will keep your lungs fully saturated, which in turn will ensure that every tissue and organ in your body has the oxygen it needs to function properly. This will put you in the best position possible to avoid medical emergencies like a heart attack, stroke, or high blood pressure.
Another way that portable oxygen concentrators prevent exacerbations and flare-ups is because they come equipped with particle filters. These filters remove small particles from the air that you would normally be inhaling before it enters the device. This is mainly done to prevent damage to the POC itself, but it has the added benefit of purifying the air that you inhale through the nasal cannula. However, if you want to breathe the cleanest air possible, you should be sure to remove and clean the particle filter regularly. If you don’t know how to do this, consult your product’s user manual or speak with a respiratory specialist.

Following Your COPD Treatment Plan
A COPD treatment plan is an all-encompassing set of guidelines that your doctor will create for you to help you slow the progression of your disease and reduce symptoms. It usually involves some type of exercise routine like pulmonary rehabilitation, an improved diet, medication, and supplemental oxygen therapy. Like anything in life, the more you work at your treatment plan, the easier it will be to follow.
If you’re struggling to manage all these different things, however, you may benefit from a portable oxygen concentrator. Unlike oxygen tanks, you’ll never have to “refill” your concentrator. Simply plug it into a wall outlet until it’s fully charged or you can keep an extra battery charged so that you have no downtime. This will free up some time for you to work on other areas of your treatment plan such as your diet or exercise routine.
Staying Self-Sufficient
Self-sufficiency is something that can easily be taken for granted if you’re not careful. Chances are, you’ve spent your whole life working and taking care of yourself, but if you’re diagnosed with COPD, you might see this freedom slowly start to disappear. You may find yourself becoming increasingly reliant on friends or loved ones for support.
![]()
One of the reasons COPD patients may find themselves becoming less self-sufficient is because of their oxygen device. Oxygen tanks need to be refilled regularly meaning you’ll either have to go to an oxygen company yourself or have them deliver full oxygen tanks to your home on a regular basis. But if you switch over to a portable oxygen concentrator you’ll find that you never need to rely on others. Simply charge up your batteries and you’ll be able to go wherever you want, whenever you want.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Conclusion
Everyone faces roadblocks in their life that make it more difficult to accomplish everything we’ve set out to do. But being diagnosed with COPD can feel like facing an obstacle that can’t be overcome. Fortunately, by taking things one step at a time and relying on friends, family members, and modern technology, it is possible to make progress and live a happy life.
Most COPD patients prefer using portable oxygen concentrators over other oxygen devices like compressed oxygen, liquid oxygen, or stationary oxygen concentrators because they help them to overcome some of their greatest challenges with less stress and anxiety. They’re also far more reliable and less dangerous to use.
Long term oxygen therapy (LTOT) is a common treatment administered to respiratory patients in the comfort of their home, and depending on their prescription sometimes 24 hours a day. Lung diseases like COPD are chronic, and so LTOT can be life changing and life saving for people who have these low blood oxygen levels, which is also known as hypoxemia.
Oxygen therapy in itself is a simple concept, however there is confusion about where and how a person should buy their oxygen device. Anyone who is administering their own treatments or medication should be aware of every detail when it comes to health and safety, but they should also be informed about their purchasing options. Purchasing an oxygen device can feel as if you are in a maze, at each turn you find a barricade forcing you to start at the beginning again, and the cycle repeats itself. This article guides you through this maze so you know what to look out for, how to make the right choice, and more!
This article will take you through all of the ins and outs of what you should look for when purchasing your oxygen therapy device. This is your all intensive guide into the buying process of a breathing device, what you should look for, and how to make the best choice for you.
What is long-term oxygen therapy

If you have ever experienced a respiratory emergency where you went to the hospital and they put tubes in your nose to help you breath, that is oxygen therapy. This is a necessary treatment if you have ever had trouble breathing on your own and it can be used to save your life.
The difference between this emergency treatment and long-term oxygen therapy is that LTOT is administered while you are at home while going about your daily life, According to International Journal of Chronic Obstructive Pulmonary Disease LTOT should be prescribed for at least 18 hours per day, although some experts suggest that 24 hours would be more beneficial.
Long term oxygen therapy, if done correctly, is proven to improve survival and other qualities of life for COPD patients with chronic respiratory failure.
LTOT doesn’t just help you live a longer life, it helps you to live more active and worthwhile life by:
- Reducing the number of hospitalizations
- Increasing your lung capacity
- Increasing your ability to exercise
- Helping you to get better sleep
- Improving your moods
- Improving your health-related quality of life
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
LTOT would normally be administered in the comfort of your home, by you, therefore the delivery method should meet your oxygen requirements but also be accustomed to your lifestyle.
Most people are prescribed oxygen anywhere from 16-24 hours a day so, this means you should choose a device that fits into your daily routine. You have a few choices when it comes to an oxygen system. These include devices you use only at home and lightweight alternatives you can take with you when you go out.
You’ll choose a oxygen device based on:
- How often you leave the house or travel
- If you need to go up and down stairs
- Your size, endurance, and physical strength
- How much oxygen flow your doctor prescribes
Oxygen devices

Three of the most popular portable devices you can choose from, each have their own pros and cons, and you should pick the best options for you:
- Compressed liquid oxygen tanks
- Oxygen gas tanks
- Portable oxygen concentrators (POC)
This article should give you some insight into what option is best for you.
If you already know that you are interested in buying a portable oxygen concentrator, and you are curious about which brand and model you should get, please read our other blog about the pros and cons of the best portable oxygen concentrators in 2020 by clicking the link here.
Affordability
The upfront costs of portable oxygen concentrators tend to scare off oxygen patients all of the time. This is unfortunate because the prices that are posted online are, for the most part, not the price you would pay for your POC. Due to the manufacturer's advertising policies, oxygen equipment licensed distributors are required to post their prices. Even if the seller has a special, discount codes, or a sale.
So even when you simply search on google “portable oxygen concentrators prices” you will see them ranging from $2,000 to $3,000 depending on the brand, year, and model. To inquire about the real prices, you can call 1-800-946-1021 and speak with a respiratory specialist who knows these devices inside and out.
The other affordable aspect of portable oxygen concentrators is that you never have to refill the device, because it is extracting the air surrounding it, compressing and purifying it into the medical-grade oxygen that you are breathing int. At LPT medical we offer a 3 year long warranty on all our portable oxygen concentrators, so you won’t have to pay for a broken part or a malfunction!
Oxygen devices like the Respironics SimplyGo Portable Oxygen Concentrator have a compressor that is rated to last 20,000 hours. Others like the SeQual Eclipse 5 Portable Oxygen Concentrator were designed for the US Military, and it has the longest-standing track record for being durable and reliable.

All in all, a portable oxygen concentrator is going to last you a very long time, and there are no recurring costs, all you pay for is the device upfront. Also by purchasing a portable oxygen concentrator through LPT Medical you have the option to finance and pay monthly, or buy a used and refurbished device that is less expensive upfront.
For more information about your purchasing options and prices, please read this other blog that we have linked here, or call us at 1-800-946-1201
Portable oxygen canisters must be refilled multiple times per week, each time costing you money. The bigger tanks that you leave in your home to use are even more expensive to refill. While oxygen tanks are the most traditional form of oxygen, it is also the most outdated. Even with the low-initial costs, the recurring costs eventually add up, leading to higher costs over time.
Portability

Unlike portable oxygen concentrators, oxygen tanks are heavy and bulky. Their weight and lack or portability are one of the most commonly noted disadvantages of tanks. While wheel-mounted cart systems can help to make rolling oxygen tanks manageable, the tanks themselves are still rather heavy. Lifting the tank—for example, to put it in a vehicle or carry it up a staircase—can be challenging or even impossible for some simply due to the weight of the device.
Depending on the oxygen flow you need to fill your oxygen prescription, portable oxygen concentrators are very light weight, and small in size. Units like the Inogen One G5, Inogen One G3, and the Caire Freestyle Comfort, all range in weight from 4 pounds to 6. All are small enough to fit inside a purse or backpack, and come with their own carrying case. Having such a lightweight and portable breathing device is great for oxygen patients who want to be more active and do more things, and not to mention travel by plane.
.png)
Having a portable breathing device is essential for keeping up with a consistent exercise regime that is a necessary treatment for all COPD patients. You should be getting the right amount of exercise relative to your health and ability. Having a portable device can make it easier to go for walks, golf, or do any other activities you like to do as your daily physical activity.
Having a breathing device that is designed to be potable is also great for keeping your morale high. It is no secret that having a chronic illness like COPD can be hard for patients mentally. If you have COPD and a portable oxygen concentrator you have the freedom and independence you need to live a normal life without having to adjust your daily routine to fit your oxygen device. Instead your oxygen device fits into your lifestyle.
Battery life vs. tanks

Portable oxygen concentrators generate oxygen using a rechargeable battery, depending on the unit, you can have anywhere from 3-16 hours with oxygen until you must either switch the battery to your backup, or recharge the device. You can recharge any device using an AC or DC power source, meaning you can use a traditional outlet in your home, or the cigarette lighter in your car or boat.
An oxygen tank on the other hand does not need a power source. The tanks or canisters are filled with a finite amount of oxygen that you use up until it is empty and have to get it refilled or replaced. Normally, you pay an oxygen supply company to come to your home and deliver new tanks and take your old ones. The tanks that are heavy and are hard to move around don’t run low as often, probably once a month depending on your oxygen prescription, and the smaller travel canisters run out at least once a week.
Having a battery powered oxygen device versus refilling your oxygen tanks is a personal preference, most people find that charging their portable oxygen concentrators is as simple as charging your cell phone, and having an extra battery to replace one while it charges is the most efficient option.
Insurance
Obviously in a perfect world, insurance would cover all respiratory patients' oxygen devices but this is not the case. There are some very rare situations where Medicare or insurance will cover the purchase or rental of one of our portable oxygen concentrators. In order to qualify, you have to meet strict criteria, and each situation is evaluated on a case-by-case basis.
That being said, You will need to talk to your insurance provider to understand what kinds of oxygen supplies they cover and what requirements you need to meet in order to qualify.
Medical insurance companies have a notorious reputation of denying patients coverage for medical equipment and treatments including portable oxygen concentrators. Unfortunately, Medicare is no exception. They have strict rules that make getting coverage difficult and burdensome, and they often find reasons to deny approval for a treatment even when a doctor says that it's the best option.
If you want the best possible chance of getting insurance or Medicare to pay for your medical equipment, you need to be aware of your provider's criteria on the subject. You must follow their guidelines carefully, to avoid getting rejected on a technicality.
We have a very informative blog about medicare and oxygen equipment that you can find here
In this blog ,we offer a lot of insight into the healthcare system and what it means for oxygen patients like yourself.
One example of Medicare's criteria for covering supplemental oxygen and related equipment:
- You have a serious lung disease (such as COPD, cystic fibrosis, bronchiectasis, etc.), or you have symptoms of low blood oxygen levels (such as pulmonary hypertension, erythrocythemia, congestive heart failure, etc.)
- Your health is likely to improve with supplemental oxygen therapy
- You have medical tests from your doctor to prove that you have low blood oxygen levels (and these tests were taken while your condition was stable, e.g. not during an exacerbation)
- You have tried other medications and treatments, but are still unable to get enough oxygen
- You need oxygen therapy 24/7 (Medicare will not cover supplemental oxygen therapy if you only need to use it at night)
This criteria has to be verified by your doctor in writing before you can receive Medicare benefits for supplemental oxygen. Your doctor will also have to write and submit a detailed report of your oxygen needs, called a Certificate of Medical Necessity.
Which method of oxygen equipment should you choose
.jpg)
While all of this information pertains to the oxygen user, it is important to note, that if you do not need oxygen therapy, meaning your blood oxygen levels are not chronically low enough that your doctor would recommend, let alone, prescribe you oxygen therapy, you should NOT administer oxygen therapy for yourself.
Who needs oxygen therapy
Even though long-term oxygen therapy can be beneficial for many people, not all respiratory patients need it. W
hen considering a lung disease like COPD, According to the American Thoracic Society, appropriate candidates for LTOT include:
- Patients who have an established medical regimen, with a 7.3 KPa (55 mmHg) partial pressure of oxygen measure by looking at arterial blood gases, and an oxygen saturation level of 88% or less.
- Patients who have a partial pressure of oxygen of 7.3–7.8kPa (55-59 mmHg), an oxygen saturation level of 89%, and also shows signs of hypoxemia, pulmonary hypertension, edema from right-sided heart failure, high red blood cell count or impaired mental status.
If you are unable to maintain healthy blood oxygen levels only while you sleep or when you exercise, you may also benefit from using supplemental oxygen specifically under these circumstances.
Moreover, because there are special cases, if you do not fall under these criteria but have severe shortness of breath or limited exercise capacity that may improves with supplemental oxygen you should still talk to your doctors about whether you would qualify for, and more importantly benefit from, long-term oxygen therapy.
Buying from a licensed distributor
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In order to be sure that you are getting an oxygen device, for example, a portable oxygen concentrator, from a licensed distributor, you can simply look on the company’s website and find their certification. At LPT Medical, you will be happy to know that we are a family owned and operated business .
LPT Medical knows what it means to serve the community and treat our customers like family and we are committed to quality and dependability. Our track record shows that we have become one of the most trusted names in the world of oxygen therapy products offering home oxygen concentrators, portable oxygen concentrators, CPAP and BiPAP machines, and all the education you need to make the most of your equipment and subsequently your life.
When you are buying oxygen equipment, something that is so life changing and a reasonably large financial decision, you must be sure that you are buying from a company that you trust. Quality is one of the first words that should come into your head when buying any medical device. If the equipment is designed to make your life easier, it is always important to take into consideration how long your equipment will last and how efficient the machine is.
LPT Medical offers products from the most reputable manufacturers in the industry including but not limited to Inogen, Philips Respironics, Drive Medical, and more. These are innovative companies that are exceeding the limits of what’s possible for patients suffering with a debilitating respiratory condition. By offering these brands, we are here to connect more people around the country with the most state-of-the-art oxygen therapy equipment in the world.

Flow settings
Depending on your oxygen needs, your doctor will either prescribe you pulse flow or continuous flow oxygen or a combination of both and you will be required to buy a device within those boundaries. It is important you do not take more oxygen and it is important that you do not try to go without it, both could do a lot of harm. If you are unsure about your oxygen prescription you should call your doctor and have them go over the process with you until you feel comfortable doing so on your own, and also during an emergency situation.
So the flow settings can be pulse or continuous, pulse gives off a bolus of oxygen every time you inhale and continuous flow settings exert oxygen constantly even when you are not inhaling.
The rate at which oxygen is flowing is known as the oxygen output, and it is most commonly measured in liters per minute. If you require more oxygen your oxygen output will be set to a higher setting and vise versa.

If you only need roughly 210- 630 mil/min of oxygen at a pulse dosage setting, you oxygen device must be able to emit that much oxygen per minute, and if you buy from a qualified company, the seller would advise for you to get a device that is capable of outputting even more oxygen than what is prescribed to you for a number of reasons.
You might be instructed by your doctor to increase your oxygen flow setting in the case of an emergency while you are experiencing an exacerbation or a flare up. In this situation you want to have a device that can increase its oxygen output so that you are able to manage the emergency how your doctor instructs you.
Also, the nature of a chronic progressive respiratory illness is that it gets worse over time. This means, that one day you might need a higher flow of oxygen than what was first prescribed to you in order to meet the demands of your body. In these cases, you want a device that will be able to adjust to your needs and increase its output before you have to buy an entirely new device that is powerful enough.

If you need both pulse and continuous flow oxygen, you can use an oxygen tank because there is a valve you can adjust to have the option to do both. If you still want a more portable option, the Respironics SimplyGo is one of the best portable oxygen concentrators that offers a powerful pulse dose setting, but also gives the user a continuous flow option for when they need to adjust to their prescription.
The most popular pulse dose units are the Caire Freestyle Comfort, the Inogen One G5, and the Inogen One G3, because all of these units are under 6 pounds, and they can produce oxygen 1050 -1260 mil/min, and have a long lasting battery life that can also be replaced with an extra so you never have to go without oxygen.
There are a lot of factors besides your oxygen prescription that go into choosing your oxygen device, but understanding your flow rate and your oxygen prescription is something your respiratory specialist will go over with you first before they ask you any other questions. Your oxygen requirement will weed through and narrow down your search, so be sure you have this information before you call us so we can assist you effectively and efficiently!
Overview

Oxygen therapy is a huge step in your life and it means that your disease has progressed to the point of severity where you can no longer survive without supplemental oxygen. Therefore, it is so crucial for you to take the necessary steps to find that best portable oxygen device that will allow you to continue doing the things you love, comfortably.
Oxygen therapy is not a bed rest sentence, you should still be able to enjoy everyday activities, and once you have adjusted to LTOT you will find that you are more capable of doing more things, even more than before you needed supplemental oxygen.
Every part of your body needs oxygen, every single organ and every single cell. If your lungs are unable to function properly and provide for your body, it will start to deteriorate. You will feel irritated, moody, tired, nauseous, and much more. Oxygen therapy assists your lungs in producing oxygen for your body so you feel better and live longer.
Both oxygen tanks and portable oxygen concentrators will help you get the oxygen you need, but one method will be better for you than the other depending on your lifestyle. For example, if you are an active person, you need a portable oxygen concentrator so that you can bring your oxygen with you wherever you go with ease.

If you need to save money, you can talk to a respiratory specialist about how to purchase a refurbished unit for less, or how you can set up a financial plan to help you pay for your oxygen device over time rather than up font.
You also have to take into consideration how durable your breathing device is, and how long it is rated to last. The longer you can have one machine the more money you can save by not having to get a new one every few years, whether yours breaks or you need to increase your oxygen intake.
There are still some things you need to know about oxygen therapy like, the functionality and tips to get the most out of your oxygen device, so be sure to follow our blog posts as we come out with more information like this is the near future!
For now we hope that this guide has given you some insight into buying your oxygen device whether it is a portable oxygen concentrator or another alternative. If you have any further question please comment on this blog post, or email us at info@lptmedical.com.
Most chronic respiratory conditions are considered “debilitating.” What this means is that they have a tendency to make the patient weak and physically incapable of certain tasks like rigorous exercise. Chronic obstructive pulmonary disease (COPD) is one such condition because it prevents carbon dioxide-rich air from escaping the lungs upon expiration. This results in frequent breathlessness, chest pain, fatigue, and more.
Another reason COPD could be considered a debilitating disease is that it often requires patients to be hooked up to an oxygen machine for a significant portion of the day. People with stage 1 or 2 COPD may only need to use supplemental oxygen for several hours a day, whereas someone with stage 3 or 4 COPD may need to be hooked up to an oxygen device 24/7.
From an outside perspective, this may seem a little daunting. After all, how could you expect to live a normal and full life if you’re expected to be connected to an oxygen device constantly? While this could be the “end of the line” so-to-speak for many other conditions, this is not the case for COPD patients. Fortunately, many years of research have gone into supplemental oxygen therapy and manufacturers are able to offer smaller, lighter, and more portable oxygen delivery machines than ever before.
In 2020, the gold standard in medical oxygen therapy are portable oxygen concentrators. Like the stationary oxygen concentrators which came before them, these are electronic devices. The primary difference, however, is that they run off batteries rather than a wall outlet, meaning you can take them wherever you want. If you’re a COPD patient who’s caught the travel bug, read on as we take a look at the top 5 portable oxygen concentrators for long-distance travel.
If you have any questions at all about any of the units, either follow the link to each product page or reach out to our respiratory specialists who can help you find the concentrator that’s right for you.
The Caire FreeStyle Comfort

There really isn’t a whole lot to say about the Caire FreeStyle Comfort that hasn’t already been said. However, we don’t mind repeating ourselves if it means getting the word out to more people about how great of a device this is. Simply put, the FreeStyle Comfort is one of the best portable oxygen concentrators that money can buy as of 2020 and this rings especially true for people who are interested in long-distance travel.
Outstanding Durability
For many people, the most stressful thing about going on a long-distance trip is the thought of losing or breaking something that’s valuable to them. For example, if you break your phone, you might spend half your vacation getting it fixed rather than enjoying your time away from home. Or worse yet, you may find yourself in a situation where you aren’t able to get it fixed. This is why it’s so important to invest in durable and reliable equipment that won’t stop working when you need it most.

You may be surprised to know that the Caire FreeStyle Comfort is the one and only portable oxygen concentrator that’s used by the United States armed forces; in other words, it’s the only true “military-grade” portable oxygen concentrator. And while we certainly don’t expect you to be going to boot camp anytime soon, this is most definitely a testament to the quality design that Caire uses on their product.
With the FreeStyle Comfort, you’ll never have to worry about damaging your unit if you happen to bump into something or drop it on accident. While there are a lot of delicate electronic components inside the FreeStyle Comfort, they’re all protected by a solid outer shell. Be aware, however, that this portable oxygen concentrator (along with most other POCs) is not waterproof. The carrying case will help protect it from water a little bit, but it is not water-resistant, so be sure to take care when using it outside.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146')}}
The Inogen One G5

Inogen is one of the top companies in the industry when it comes to pulse dose portable oxygen concentrators. Since their inception, they’ve worked tirelessly to make portable oxygen units lighter, smaller, and more powerful than ever before. Releasing just last year, the Inogen One G5 proved that it’s possible to have a high flow of medical-grade oxygen wherever you go.
High Oxygen Output
Oxygen output is a crucial factor to consider when buying a new portable oxygen concentrator. When your doctor or pulmonologist prescribes you oxygen, he/she will give provide you with an exact volume of oxygen that you need per minute. Pulse dose machines like the Inogen One G5 are measured in milliliters per minute (ml/min). And the G5 has the highest oxygen output of any pulse dose concentrator on the market. Its maximum oxygen output is 1,260 ml/min and a pulse flow setting of 6. That’s about 210 ml/min for each flow setting.

Simply put, a high flow of oxygen means that more people will be able to experience the freedom of owning a lightweight portable oxygen concentrator. And if you’re someone who uses a lower flow setting like a 2 or a 3, you’ll be happy to know that you have some breathing room if you should need to move up for one reason or another. For example, if you check your blood oxygen level using a pulse oximeter and it’s lower than expected, you can simply press a button on the G5 and receive an additional 210 ml/min of oxygen.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Possibly the best part about the Inogen One G5’s high oxygen output is that it doesn’t come at the expense of other features. For example, the G5 puts out 1,260 ml/min of oxygen compared to the Caire FreeStyle Comfort’s 1,050 ml/min of oxygen. Despite that fact, the G5 weighs 0.3 pounds less than the FreeStyle Comfort at just 4.7 pounds with the 8-cell battery. It also doesn’t compromise when it comes to battery life. On a pulse flow setting of 2, the G5 offers up to 5 hours of battery life with the 8-cell battery and 10 hours of battery life with the 16-cell battery. Compare this to the FreeStyle Comfort which offers 4 hours with the 8-cell battery and 8 hours with the 16-cell battery.
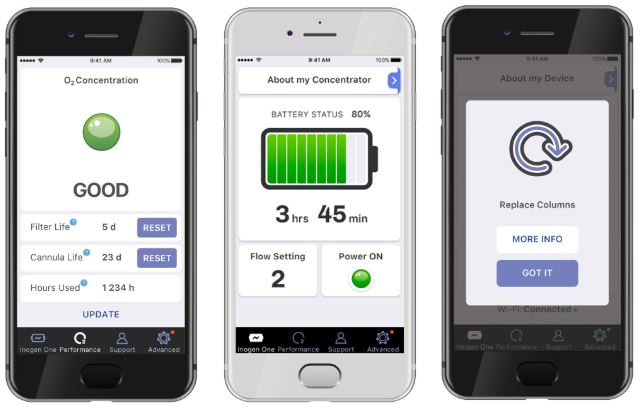
Another great benefit of the G5 is something called the Inogen Connect. This is a smartphone application that connects to your POC through Bluetooth. Once the devices are paired, you’ll be able to view information about your flow setting, remaining battery life, and more. You can even view the device manual if you end up needing to troubleshoot it. This app is especially useful if you’re using the Inogen One G5 backpack and you don’t want to stop constantly to check your G5. Simply pull out your phone and adjust the settings that way.
The Inogen One G3

While the Inogen One G3 came out quite a few years ago, it still holds up in 2020 as one of the top pulse dose portable oxygen devices on the market. The G3 is a slight downgrade from the G5 in terms of size and oxygen output, however, it more than makes up for this with an array of high-quality accessories that allow you to customize your supplemental oxygen therapy.
Options to Suit Your Lifestyle
One of the best things about owning an Inogen One G3 is that you don’t just have to settle with what you get right out of the box. There are plenty of accessories that you can use to make your supplemental oxygen more tailored to your preferences. For example, if you’re getting ready to travel long distance, you might choose to upgrade the carrying case that comes with the G3 to something like the Inogen One G3 backpack which will allow you to carry your G3 on your back instead of at your side. What’s more, you’ll have lots of extra space in the bag for personal belongings like your keys, wallet, or passport.

Another similar option to the G3 backpack is the Inogen One G3 Rolling Backpack. This has shoulder straps just like the other one but it also has wheels and an extendable handle so you can pull it around like a suitcase. This is ideal if you’re going to be traveling by plane and you’re bringing a lot of other accessories such as an additional battery, external battery charger, or additional charging cables.

Last but not least, the GO2 Carryalls are another carrying option available to G3 owners. Unlike the backpacks which are designed to provide users with more convenience and carrying space, the GO2 Carryalls provide a more stylish carrying bag for the G3. At first glance, they look like an ordinary purse or handbag, but upon closer inspection, you’ll notice that they are precisely designed for the G3. The user interface is easily accessible via the top zipper, the sides are made of mesh material so that the devices air intake vents aren’t blocked, and there are several extra pockets where you can store personal items.
The Inogen One G4
If you’re someone with early-stage COPD, you’re likely not going to need a huge amount of oxygen throughout the day. If this is the case, you’re probably not going to want to lug around a large POC if it’s not absolutely needed. If this sounds like you then the Inogen One G4 might be right up your alley.

The Inogen One G4 weighs in at just 2.8 pounds making it the second lightest portable oxygen concentrator ever made, behind the AirSep Focus. The G4 goes up to a flow setting of 3 with a maximum oxygen output of 630 ml/min. This is exactly half of what the Inogen One G5 offers.
The Respironics SimplyGo

The one thing that all of the above machines have in common is that they’re all pulse flow portable oxygen concentrators. These POCs tend to be much smaller and lighter than continuous flow oxygen concentrators, making them ideal for long-distance travel. However, there is one continuous flow portable oxygen concentrator that we’d recommend for travel — the Respironics SimplyGo.
The reason we’d recommend this over other continuous flow units is because it’s far lighter and smaller than other options out there. For example, the SimplyGo weighs only 10 pounds, but other popular continuous flow units like the Oxlife Independence weigh in at 19.4 pounds. This is nearly twice the weight and it doesn’t have much to compensate for it when it comes to oxygen output or battery life either.

The SimplyGo is one of the few continuous flow machines that can be carried on your shoulder and you’ll find it easy and convenient to take on a flight, cruise ship, or whatever mode of transportation you choose. Since the SimplyGo offers both continuous and pulse flow settings, you’ll have more options for how you’d like to receive your supplemental oxygen on the go.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
One more benefit of taking a continuous flow portable oxygen concentrator with you on a long trip is that it’s compatible with CPAP and BiPAP machines. So if you suffer from obstructive sleep apnea (OSA) or any other sleep disorder, you’ll be able to attach your SimplyGo and get a better night’s sleep while you’re away from home.

Are Portable Oxygen Cylinders an Option?
Now that you know about some of the best portable oxygen concentrators for long-distance travel, you might be wondering what’s wrong with portable oxygen cylinders. These are the small oxygen tanks that you’ve likely seen people carrying around on their backs or wheeling around with a carrying cart. While these can be convenient in some cases, they’re a very poor choice for long-distance travel.

Firstly, they are not approved by the Federal Aviation Administration (FAA) for in-flight use. What this means is that — no matter what airline you choose — you will not be able to fly with an oxygen tank. You’ll either have to approve with your doctor first that you’re able to travel without oxygen or find another way to travel which can be difficult and time-consuming.
Tips for Flying with Portable Oxygen
.png)
Conclusion
We live in unprecedented times for oxygen patients. In the past, being diagnosed with COPD, pulmonary fibrosis, or other chronic respiratory conditions meant giving up your basic freedoms. However, in this day and age, it’s possible for oxygen patients to experience significant freedom by investing in a portable oxygen device that matches their lifestyle.
There are plenty of great options available to you, but you may be having trouble narrowing down your choices. When you’re ready, give our respiratory specialists here at LPT Medical a call and we’ll walk you through the whole process.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!













