.png)
From the novel coronavirus to devastating wildfires, 2020 has been a challenging year for us all. But for people with chronic respiratory illnesses like COPD or asthma, this year has been the ultimate test. The good news is that, by following all COVID-19 safety precautions stated by the World Health Organization (WHO) and by checking the air quality index (AQI) before leaving the house, many COPD patients have adjusted nicely to a new way of life.
With the holidays coming up, you may be wondering how you can stay safe while still catching up with friends and loved ones. Whether you’re flying across the country or you’re just going down the street, it’s important to prepare well enough in advance so that you can stay healthy and happy and avoid emergencies like COPD flare-ups and exacerbations. Conversely, if you are having relatives over to your house, you should ensure your home is safe for you and your guests.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In this post, we’ll take a look at several of the most important safety tips you should take into consideration. As always, if you have any questions for us, feel free to leave them in the comment section and we’ll do our best to answer them as soon as possible. What’s more, if you have any questions about your COPD treatment plan or you’re thinking of making changes to your diet, exercise routine, or medication, please consult your doctor beforehand.
Upgrade to a Portable Oxygen Concentrator
Chances are, you know exactly what it’s like to use an oxygen tank during the holiday season. First and foremost, you have to have a plan as to how you will refill your oxygen tank while you’re away from home. This could mean bringing a spare tank or researching oxygen companies in the area that can deliver oxygen to you. Unfortunately, it can be very difficult to find an oxygen company that’s actually open during the holiday season.

The next thing you have to consider is how you will actually transport your oxygen. Oxygen tanks are banned on all airlines, so taking a flight is out of the question. It’s also very dangerous to travel with an oxygen tank in your car, so you will have to take a number of safety precautions in order to ensure that it doesn’t move around while you’re in transit. Last but not least, you’ll have to spend your whole holiday keeping a close eye on your tank, making sure it’s not exposed to any open flames or anything that could damage the fragile components.

Fortunately, using a personal oxygen concentrator is much easier and safer. Travel size oxygen concentrators like the Caire FreeStyle Comfort are lightweight, compact, and most importantly, they’re much safer to use than a standard oxygen tank. Portable oxygen concentrators are electronic devices that draw in ambient air, remove unneeded gases, and then put out medical grade oxygen. As a result, they don’t store oxygen at high pressures like oxygen tanks do.
Another reason they’re safer is that they have an implemented “breath detection technology” which cuts off oxygen flow if no breath is detected. Since oxygen increases the flammability of everything it comes in contact with, you can rest assured you’ll be safe if you accidentally drop your nasal cannula and leave it for an extended period of time.

One final reason that portable oxygen concentrators are safer to use during the holidays is that they don’t create a tripping hazard. If you use an oxygen tank, you will have to wheel it around on a carrying cart meaning your nasal cannula will have to run from the tank to your nose. However, portable oxygen concentrators like the Inogen One G5 can be slung over your shoulder and tucked under your arm so that it’s always accounted for. What’s more, you can keep your oxygen tubing nice and short so that it’s not dragging on the ground.
Have a Plan for Dealing with Exacerbations
According to the American Thoracic Society (ATS), a COPD exacerbation is a period of worsening symptoms, most commonly caused by infection. And unfortunately, being around your family and extended family during the holidays will put you at a higher risk of contracting illnesses like the flu, the common cold, and even the coronavirus. Contrary to popular belief, most medical experts recommend wearing a mask if you have COPD. As long as you’re using supplemental oxygen therapy as prescribed and you’re checking your blood oxygen levels regularly, the mask should not affect your symptoms.

If you’re someone who experiences anxiety or claustrophobia while wearing a mask, there are a number of techniques you can try to alleviate this. Since claustrophobia is closely linked to how you breathe, taking the time to learn breathing techniques like diaphragmatic breathing can help you in the long run. This involves concentrating on using your diaphragmatic muscles to breathe rather than your chest muscles. Another thing you can try is cognitive-behavioral therapy (CBT) which can help you pinpoint the root cause of anxiety and learn ways to cope with it in a manageable way.
Aside from wearing a mask, you should follow all other COVID-19 safety guidelines. This means maintaining 6 feet of distance between other people, washing your hands regularly throughout the day, and making others aware that you’re a high-risk individual. Making others aware of your condition is important because if there was an emergency, they would need to know how to help. If you want, you can even write down an action plan to help you out in a difficult situation. If you’d like to learn more about COPD action plans, read through this post.
Don’t Fall Back on Old Habits
When you were diagnosed with COPD, you likely had some significant obstacles to overcome. Smoking cessation, an improved diet, and a consistent exercise routine are all necessary to get back on track and slow the progression of COPD. Unfortunately, all the bad habits you dropped when you were diagnosed with COPD can come flooding back when you’re around people you haven’t seen in a while.

Before leaving the house for the holidays, it’s important to mentally prepare. While the holiday season is all about relaxing and letting go, you don’t want to be so relaxed that you forget about your COPD treatment plan. One thing most people do on Thanksgiving and Christmas is overeating. This may be relatively harmless for someone who’s healthy, but for someone with COPD, this could mean exacerbating your lung symptoms.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
The main reason you don’t want to overeat during the holidays is that it can lead to bloating. When this happens, you’ll notice that you have a harder time breathing and you’ll be more likely to experience chest pain or a chronic cough. Secondly, COPD patients have a hard time processing a lot of food all at once. This is why doctors recommend eating smaller meals spread throughout the day because it is easier for your body to manage. Eating large meals can also lead to weight gain.

According to U.S. News, being overweight has a number of negative effects when it comes to managing your disease. Overweight individuals will get out of breath faster and excess body weight on the stomach and chest can interfere with breathing. Another problem is that overweight people tend to maintain a diet high in carbohydrates which get converted to carbon dioxide (CO2) during digestion. This means you’ll be struggling to get the oxygen you need to maintain your blood oxygen levels. So, if you want to eat healthy this holiday season be sure to focus on portion control and avoid foods that are high in carbs.

Another habit you may be tempted to fall back on is smoking. Cigarette smoking causes around 85 to 90 percent of all COPD cases and continuing to smoke with COPD will worsen the disease and trigger exacerbations. If you’re spending time with relatives that you used to smoke with or people who currency smoke this holiday season, this could cause you to slip back into an old habit. And even if you don’t smoke with this person, being around them will still expose you to secondhand smoke which can be just as bad.
Take Time Packing Your Medication
If you’re a COPD patient, your medication is paramount to your health. Whether you take orally administered medication, inhaled medication like nebulizer therapy or inhaler therapy, or some combination of the two, you’ll need to ensure that everything is packed and ready to go before you head out the door. If you haven’t done so already, be sure to renew your prescription for all of your medications so that you don’t have to worry about that when the time comes to leave.

Long-acting bronchodilators are designed to relax the airways and help you breathe easier throughout the day. This includes drugs such as tiotropium, salmeterol, indacaterol, formoterol, arformoterol, and aclidinium. Short-acting bronchodilators, on the other hand, are designed to work quickly in the event that you experience a COPD exacerbation. Short-acting bronchodilators include albuterol, ipratropium, ipratropium bromide, and levalbuterol.
Plan a Pulmonary Rehabilitation Schedule
Pulmonary rehabilitation has been one of the most hotly debated aspects of COPD treatment plans. In the past, it was believed that any form of exercise would exacerbate respiratory systems. However, within the past several decades, studies have shown that a carefully planned and consistent exercise routine can improve lung strength and slow the progression of COPD.
While it’s tempting to forget about exercising and practicing breathing exercises while you’re away for the holidays, this will only put you behind on your treatment regime. Rather you should take the time to plan out your day and ensure that you follow all of your doctor's instructions. It may not seem like it, but even a small amount of moderate exercise can go a long way towards improving your long term prognosis and helping you feel better.
Check the Air Quality Index (AQI)
You may believe that, since the temperature is starting to drop, there’s no need to check the air quality index before you go outside. Unfortunately, this is simply not the case. Cold weather actually causes things like car exhaust and other types of air pollution to stick closer to the ground since the air is denser and moves more slowly. This means it’s more important than ever to check the air quality. What’s more, there are a number of wildfires still raging across the country which are filling the air with smoke.

According to this study, the most common types of pollution during winter months are PM10 (particulate matter that is 10 micrometers in diameter or smaller), sulfur dioxide, nitrogen dioxide, and carbon monoxide. Wildfires are a complex mixture of pollutants including fine particles, water vapor, carbon monoxide, carbon dioxide, nitrogen oxides, organic chemicals, and more. When you go to check the AQI in your area, be sure to keep an eye out for these.
.jpg)
COPD patients are considered part of the “sensitive group” when it comes to air quality. Generally speaking, COPD patients should not go outside if the AQI is over 100, but if you have late stage COPD, an AQI under 50 will be ideal. Like we discussed in our last blog post, there is an AQI mobile application that you can download on either your Android or iPhone that makes it simple and easy to check the air quality in your area.
Bring Clothing That’s Appropriate for the Weather
The weather has an immense impact on COPD symptoms. Extreme conditions, typically over 90 degrees Fahrenheit or below freezing can cause flare-ups and lead to unexpected side-effects like increased mucus production. Of course, the best way to cope with these weather conditions is to remain inside with the heater on, however, going outside may be unavoidable if you’re visiting relatives.
![]()
One of the best ways to keep your body temperature high while out in the cold is to wear multiple layers. Unfortunately, simply wearing a heavy jacket won’t do much to keep you warm and it could even restrict your breathing. Rather, you should wear several layers of flexible clothing that don’t add any unnecessary strain to your chest or stomach. Also, be sure to wear gloves, a hat, and a scarf.
For more information on managing COPD in cold weather, read our article titled, “The Complete Guide to Managing Your COPD in the Winter”.
Conclusion
It’s hard to believe that the holidays are just around the corner. In just a few weeks it will be time to pack the bags and head to the relatives’ house. And whether you’re planning on traveling across the country or next door, there’s a lot of planning COPD patients need to do in order to stay safe and healthy during this time. Follow the tips above to get you started and don’t hesitate to leave a comment below if you have any questions for us.
If you’re looking for a lightweight portable oxygen concentrator for your holiday trip, feel free to reach out to our respiratory specialists here at LPT Medical. We are happy to provide COPD patients with plenty of options from the most reputable brands in the industry like Caire Inc., Inogen, and Respironics. Some of our most popular units include the Caire FreeStyle Comfort, Inogen One G5, and the Respironics SimplyGo.
.png)
November is COPD awareness month, a time to come together and educate people of all backgrounds about the global impact of chronic bronchitis and emphysema. COPD awareness month is marked by an orange ribbon and can be observed in a number of different ways. Despite being the third leading cause of death in the United States, COPD suffers from a severe lack of awareness. According to a Health Union survey, only about 38 percent of patients were aware what COPD was or what its risk factors were before being diagnosed.
Believe it or not, November is also lung cancer awareness month. And while these two diseases share many symptoms, causes, and risk factors, they are not the same disease. To put this into perspective, about 16 million people have COPD in the United States, yet only about 541,000 people have lung cancer in the United States. Generally speaking, more people are aware of the impact of lung cancer and they’re more educated about the symptoms than those of COPD.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
No matter whether you’ve just been diagnosed with COPD, you’ve had COPD for years, or you’ve never been diagnosed with COPD, we’re going to take a look at seven of the best ways to celebrate COPD awareness month. If you have any questions about anything you’ve read here, please feel free to leave a comment or reach out to us.
Participate in Local Events
The novel coronavirus has made 2020 a difficult year for in-person events like concerts, fundraisers, and more. In order to prevent the spread of the coronavirus, many of these events have been canceled in order to limit or outright prevent human-to-human contact. But that doesn’t mean that these events have stopped entirely, it just means that people have had to adapt to a new way of doing things. For most people, this has meant relying more on technology than ever before and embracing things like social media and video conferences.

Because COVID-19 specifically targets the respiratory system, it’s more important than ever for COPD patients to be aware of what’s going on in the world of COPD research. According to COPD News Today, although respiratory patients have a high survival rate when contracting COVID-19, they’re still at a much higher risk of experiencing severe symptoms from the virus than the general public. COPD patients are more likely to experience exacerbations such as increased dyspnea, phlegm production in the airways, and chest pain.
Mentor Youth to Prevent Smoking and Vaping
According to the Centers for Disease Control and Prevention (CDC), smoking rates have declined from 20.9 percent in 2005 to 15.5 percent in 2016 among adults 18 years of age and older. While this is certainly great news, there are still many battles to be fought when it comes to smoking prevention, especially among people who are most vulnerable such as the youth. According to Heathline, about 8 percent of teens smoke cigarettes and about 21 percent use e-cigarettes or vape pens.

Vaping has often been touted as the “best option” for weaning people off of cigarettes and onto a substance that’s less harmful for your health. However, vaping has been linked to a number of illnesses commonly called E-cigarette or Vaping product use-Associated Lung Injury (EVALI). What’s more, many people argue that vaping can be used as a “gateway drug” leading to the use of cigarettes and marijuana, especially in younger generations.
If you have COPD, you likely agree that any amount of drug use among American youth is too much. This is why COPD awareness month is the perfect time to mentor kids and teens about the dangers of cigarette smoking. If you know what it’s like to live with COPD and you’ve spent time researching and understanding your disease, this puts you in a great position to mentor younger generations and teach them about a disease they may know little or nothing about.

There are many ways to get involved with youth mentoring. First and foremost, you can simply speak with friends or family members and tell them your story of coping with COPD. Another thing you can do is support tobacco-free schools and programs. While most schools do promote a smoke-free lifestyle, the more engagement there is from parents and previous smokers, the easier it will be to create a truly smoke-free generation. In short, smoking trends have decreased significantly over the decades, and it’s mostly due to people like you who want to make a difference in someone’s life.
Create an Online COPD Group
In this day and age, it’s easier than ever before to stay connected to the outside world. With social media sites like Facebook and online COPD communities like COPD360Social made by the COPD Foundation, you can be connected with thousands of other COPD patients around the world in a matter of minutes. As long as you use discretion when you read something, this can be an incredibly powerful tool for helping you understand your disease and learn about possible treatment options that you may not have heard of otherwise.

If you can’t find the right community for you, however, COPD awareness month may be the perfect time to start your own online COPD community. This is a great idea if you have a close group of friends with COPD who want to stay connected despite the pandemic we’re currently facing. You’ll also have the option of keeping the group closed or open, allowing people all over the world to join in on your conversations about COPD. Keep in mind that your social media group doesn’t have to focus on COPD. You could also discuss things that keep your mind off of your disease and the current state of the world.
Reevaluate Your Short- and Long-Term Goals
Goal planning is extremely important if you live with chronic obstructive pulmonary disease or any other type of respiratory impairment. Long-term goals focus on broad accomplishments such as smoking cessation, exercise goals, and diet goals, whereas short-term goals are like baby steps that you will use to achieve your long-term goals. Being faced with a COPD diagnosis often means drastically altering your goals as well as changing your outlook on life.
![]()
Since COPD awareness month comes around once a year, it’s the perfect time to reevaluate your goals and make sure that you’re on track to meet them. COPD plans are oftentimes confusing and multifaceted, so it’s best to assume that you can always make improvements to it. For example, if you’ve already drastically changed your diet think about other ways to benefit from your diet like eating smaller meals throughout the day, creating a meal plan so that you are more consistent with your diet, or contacting your doctor to see if there are any additional changes you can make. Ultimately, you don’t want to feel overwhelmed by your treatment plan, but you also want to always feel like you have something to work towards.
Participate in a Clinical Trial Program
A clinical trial is a research project aimed at determining the safety and efficacy of a particular medicine or medical procedure. Clinical trials are overseen by the U.S. Food and Drug Administration and they’re divided into four different phases. Phase one clinical trials typically test the safety of a drug or medical procedure and phase two clinical trials are focused on their efficacy. Phase three tests the drug in diverse populations and in different dosages or in combination with other drugs. Last but not least, phase four trials are aimed at monitoring drugs after they’ve already been approved for the market.
![]()
There are many reasons to participate in clinical trials this COPD awareness month, but the main reason is that it helps researchers learn more about the lungs and how to treat chronic illnesses like COPD. In order to learn more about COPD and how to treat it, researchers need people of all backgrounds to test their medication. By doing this, they are able to understand who might benefit from it in the future and who should avoid it due to negative side-effects.

Another reason you may want to participate in a clinical trial is because it affords you the opportunity to use COPD medication that is not available to most people. You’ll also be happy to know that most clinical trials are free to participate in and you may even get paid for the time you put into it. Before offering you any type of medication, clinical trial organizations are required to perform a medical examination to ensure there isn’t a high risk of harm, so you can rest assured that clinical trials are safe. To learn more about clinical trials in your area, visit clinicaltrials.gov.
Take Up a New Hobby
Hobbies are the meaningful tasks that we use to fill our day-to-day life. They’re separate from our life-long goals and aspirations, but they can also be a significant part of who we are and what our purpose is in life. A hobby can be something as simple as doing a crossword puzzle or something more complex and involved like scrapbooking or playing music. Unfortunately, many COPD patients define themselves by their disease rather than by the things that are important to them. This is why COPD awareness month is a great time to pick up a new hobby and discover something that’s important to you.
One of the biggest issues facing the COPD community is anxiety and depression, so it’s best to find a hobby that combats these issues. According to Healthline, one of the best ways to prevent depression is through exercise so if you can find a hobby that gets you up and moving, it’s likely to keep you happy and healthy. Since your COPD treatment plan already requires you to perform pulmonary rehabilitation it might be worth it to find a way to combine your hobbies and your exercise routine. Hobbies like reading or playing games are also great because they keep your mind engaged and prevent your thoughts from wondering.
Raise Awareness for Alpha-1 Antitrypsin Deficiency
It’s so easy to get caught up in conversations about smoking and air pollution and forget about the primary genetic cause of COPD: Alpha-1 Antitrypsin Deficiency (AAT deficiency). Alpha-1 antitrypsin is a type of protein that’s created by the liver. Its job is to protect the lungs from inflammation. When this protein is distributed in low quantities it can make the patient more susceptible to lung damage from smoking, air pollution, and lung infection. Alpha-1 deficiency is known to contribute the pathogenesis of lung disease in people who have never smoked and have lived otherwise healthy lives.

Alpha-1 deficiency is genetic, meaning it’s inherited from the parents and it does not appear in offspring unless both parents have this trait. As a result, alpha-1 deficiency is a fairly rare condition, affecting about 100,000 people in the United States. Alpha-1 deficiency is more common in people of European descent and less common in people of Asian descent. If Alpha-1 deficiency results in the liver retaining this protein, it can also lead to the development of scar tissue in the liver.

While alpha-1 deficiency only causes about 3 percent of COPD cases, it’s still an important risk factor to know about. Many people with alpha-1 deficiency are undiagnosed and resulting lung damage is often misdiagnosed as asthma. So, the more aware the general population is of this rare disease, the more likely it can be treated before doing severe damage to the respiratory system. Read our blog post about alpha-1 antitrypsin deficiency and share it with a friend if they would benefit from it.
Conclusion
Unfortunately, contrary to its prominence in the United States, chronic obstructive pulmonary disease suffers from severe underrepresentation and lack of awareness among the general population. This is due to several reasons. First and foremost, the majority of people who smoke never contract COPD. Rather, smokers are more likely to contract other illnesses such as cancer, heart disease, stroke, and diabetes, all of which can detract from the national conversation about chronic bronchitis and emphysema.
Another reason there is a lack of awareness around COPD is that it shares the same awareness month as lung cancer. While it’s certainly important for COPD patients to understand their high risk of contracting lung cancer, it’s also important to remember that COPD is a silent disease in many ways since it is often underdiagnosed or misdiagnosed. Helping people to understand that COPD and lung cancer are two different diseases may help shed more light on the unique problems associated with each.
Ultimately, COPD awareness month is a month that should be observed by everyone, regardless of whether or not you have COPD or you know someone who has COPD. Take some of the aforementioned tips into consideration as you plan for the weeks ahead and be sure to leave a comment below if you have any questions or concerns.
.png)
Headaches are a problem that we all deal with whether we’re young or old; healthy or not. A mild headache can detract from our daily life causing us to feel distracted, unmotivated, or restless. But at their worst, headaches can leave us completely unable to function in our daily lives. Many COPD patients may find themselves somewhere in between. You might get headaches periodically with varying degrees of severity, and experience periods of relief.
If you’ve noticed that you experience more headaches or more severe headaches since contracting COPD, the two conditions are most likely linked. In other words, focusing on treating your underlying COPD symptoms may help you to manage or completely eliminate your headaches as well.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In the following article, we’ll take a look at some important steps you should take to treat headaches if you have COPD. As usual, if your headaches persist or you believe they may be caused by some other health issue, be sure to schedule an appointment with your doctor to discuss the potential cause.
How COPD Causes Headaches
Chronic obstructive pulmonary disease is a group of lung diseases that cause difficulty breathing. It’s called an “obstructive” disease because it makes it more difficult for a patient to expel air from the lungs. Diseases that make it more difficult for patients to inspire air are called “restrictive” because they’re caused by lungs that are unable to expand completely.
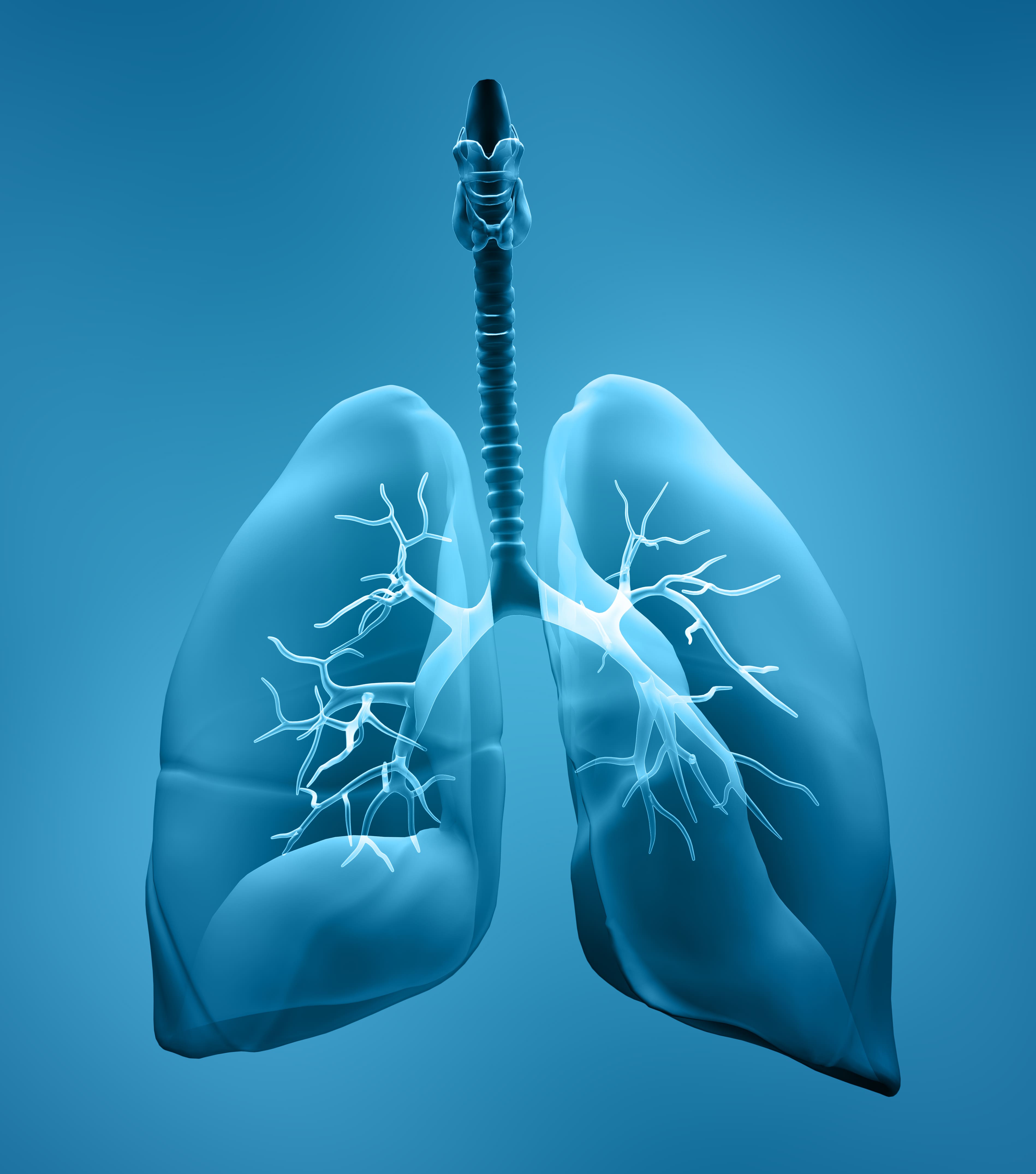
Your lungs have two functions: to bring in oxygen-rich air and to remove carbon dioxide-rich air. If one of these functions is out of balance, it can lead to a lot of problems. For example, hypoxia can occur when your blood has low oxygen levels. Over time, this can lead to severe symptoms, because your tissues are being deprived of a basic component that they need to function.
Another problem that can result from a chronic lung disease like COPD is hypercapnia. This is a condition that happens when you retain too much carbon dioxide. Having too much carbon dioxide in the blood can lead to similar symptoms as hypoxia by damaging organs and slowing the rate at which oxygen gets to your body’s tissues.

The most common cause of headaches in COPD patients is a low blood oxygen level due to either hypoxia or hypercapnia. While the brain only makes up about 2 percent of your body’s weight, it receives 15 to 20 percent of the body’s blood supply. As such, you’re likely to experience a headache due to low blood oxygen levels before any other symptom.
Many COPD patients experience headaches in the morning after waking up and this is likely due to sleeping problems such as sleep apnea which can be exacerbated by a chronic lung condition. When these two conditions occur together simultaneously, it’s called COPD-OSA overlap syndrome. If you have overlap syndrome, your doctor will likely prescribe both supplemental oxygen and CPAP or BiPAP therapy to help you sleep better at night.
Focus on Your COPD Treatment Plan
A COPD treatment plan is a set of steps you take to treat the underlying symptoms of COPD. Most doctors will recommend some combination of supplemental oxygen therapy, pulmonary rehabilitation, an improved diet, and a revised sleep schedule. However, depending on the severity of your COPD and whether or not you have comorbidities may affect how you should be treating your disease.

The reason that you should start with your treatment plan is that it will rule out COPD as the cause of your headaches. If you’re doing everything that you should be doing to manage your respiratory health and you’re still experiencing headaches regularly, it’s safe to say that there is something else causing the issue. On the other hand, if you’re experiencing headaches in the morning, they could be due to a drop in blood oxygen levels at night. In this case, you may need to talk to your doctor about having a sleep test done.
Supplemental Oxygen Therapy
The vast majority of people with COPD are prescribed supplemental oxygen. Some people are only required to use it several hours a day or as needed when blood oxygen levels are low. However, a large number of COPD patients need to use oxygen for 16 hours or more each day. Unfortunately, some people find themselves either falling back on the supplemental oxygen plan their doctor set for them or they are unknowingly using their oxygen device incorrectly.

Oxygen tanks have been the industry standard for oxygen therapy for a long time. But they don’t meet the needs of every oxygen patient because they’re heavy and bulky. As a result, oxygen tank users frequently feel like they aren’t able to get where they need to go without help from a friend or loved one. Carrying around a heavy oxygen tank can also lead to breathlessness, low blood oxygen levels, and thus headaches, so it may be worth it to look for a different oxygen therapy device.

Portable oxygen concentrators offer a much more convenient way to use oxygen. Since they’re both small and lightweight, they help you ensure that your oxygen needs are met wherever you go. POCs are battery-powered, so you’ll never find yourself where you run out of oxygen. Simply plug it into any car or wall outlet and you can continue using it and charging your batteries.
Pulmonary Rehabilitation
Pulmonary rehabilitation is a fancy way of saying exercise that’s focused on your lung health. Pulmonary rehab is a supervised program meaning you will work with a medical expert who will show you the proper way to exercise if you have impaired lung function. However, once you know how to exercise correctly, you can perform pulmonary rehabilitation in the comfort of your own home.

The reason pulmonary rehab is so important in preventing headaches is that a sedentary lifestyle and poor posture can make you more susceptible to headaches. Consistent moderate exercise is one of the best remedies for headaches because it keeps blood flowing to the brain and the rest of the body. Exercise also helps you improve your posture which is another thing that can affect your body’s circulation.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Healthy Diet
Your diet plays an immense role in your body’s ability to ward off headaches. According to migrainetrust.org, skipping meals, dieting, eating high-sugar foods, and fasting can all contribute to or cause headaches. What’s more, according to COPD News Today, studies suggest that inflammation caused by COPD can contribute to the development of type 2 diabetes. This condition is known for causing low blood sugar (hypoglycemia) and as a result, headaches.

As a COPD patient, your diet should be strictly regulated. First and foremost, you should be eating smaller meals throughout the day rather than one or two big meals. Your body may struggle to digest larger meals, so the more you can spread out your meals, the better. Secondly, you need to be eating the right types of foods. COPD patients need food that is high in fiber, protein, and healthy fats, but low in added sugar and salt, as well as highly processed or fried foods. This will ensure that your lungs remain healthy and strong and you don’t have any bouts of hunger or energy loss that could lead to headaches.
Smoking Cessation
Smoking is likely one of the most common causes of headaches in COPD patients. According to the Centers for Disease Control and Prevention (CDC), 38% of COPD patients are current smokers. While smoking temporarily alleviates stress, anxiety, and headaches, the withdrawals you experience after the fact can be particularly painful. According to WebMD, insomnia, cravings, and headaches due to nicotine withdrawal typically begin 3 to 5 days after you last smoked. If you’re trying to quit smoking but keep falling back on your plans, this could be why you’re experiencing headaches.

Avoid COPD Triggers
A COPD trigger is anything that can cause a flareup in your COPD symptoms. Some common COPD triggers include cigarette smoke, car exhaust, indoor cleaners, dust, pollen, and more. COPD triggers can cause your airways to constrict, increase inflammation in the lungs, and increase the production of mucus, all of which make it more difficult to breathe. Additionally, COPD exacerbations can lead to a high degree of stress and anxiety, all of which can contribute to headaches.
![]()
Ideally, you should be conscious of the quality of air that you are breathing throughout the day. When you’re indoors, make sure you are not exposed to dust, mold, or toxic cleaning supplies. And before going outside, be sure to check the air quality index to make sure the air is clean enough for someone with a chronic respiratory illness. Also, be sure to have a plan for dealing with flare-ups and exacerbations.
Drink Lots of Water
According to the H.H. Mitchell, Journal of Biological Chemistry, the heart and brain are composed of 73% water and the lungs are composed of 83 percent water. What this means is that depriving your body of water doesn’t just prevent your brain from getting the water it needs, but it also makes it more difficult for your heart and lungs to bring oxygen-rich blood to your brain. While every tissue in your body needs water, your brain needs it most of all.
.jpg)
COPD Medications
The medications that you take for COPD can be both the cause of, and the cure for your headaches. Generally speaking, taking medication as it’s prescribed by your doctor will help stabilize your blood oxygen level and mitigate the chance that you will experience an exacerbation or other COPD-related complication. However, some COPD medications have “headaches” listed as a side-effect, so this isn’t something you should rule out.

Fast-acting bronchodilators (also known as rescue inhalers) are an important part of any COPD treatment plan. They include drugs like albuterol, albuterol sulfate, and levalbuterol, and they’re responsible for quickly alleviating COPD symptoms like chest tightness and excess mucus production. However, fast-acting bronchodilators are also known for having a lot of side-effects like headaches, dizziness, and nausea.
Be Careful With Pain-Relief Medications
Unfortunately, most discussions around COPD are focused on alleviating the symptoms of the disease and less on alleviating pain that’s associated with those symptoms. While pain medication can be used safely and effectively in COPD patients, it should not be seen as a cure-all or something that’s used on a daily basis. What’s more, you have to be careful about what pain relievers you’re using and how they will interact with your COPD medications.

Consult Your Doctor
While you can continue to research the potential cause of your headaches, the best way to deal with this problem as quickly as possible is to consult your doctor. While it may seem like a hassle to go to the doctor just to ask about your headaches, there could be a very simple solution to your problem or there may be a more serious underlying problem that your doctor needs to know about. Be sure to write down the following information before you schedule an appointment:

- The frequency and severity of your headaches
- What time of day or night your headaches occur
- The location on your head that you feel the most pain
- What foods you’re eating each day
- How much water you’re consuming daily
- What your sleep schedule is like
- Any additional medication you’re taking (that wasn’t prescribed by your doctor)
Conclusion
Headaches are not an uncommon side-effect of chronic obstructive pulmonary disease. Likely one of the first symptoms you will experience if your blood oxygen levels are low is a headache. But there’s also a chance that the pain you’re experiencing is completely unrelated to your respiratory condition.
Start by trying a few of the tips listed above and if they don’t work, be sure to consult your doctor. While there may be a simple solution to your headache problem, they could be a sign of a more serious underlying condition, so it’s best to speak with your doctor sooner rather than later.
In the meantime, if you’re looking for a new mobile oxygen machine to manage your respiratory condition, feel free to browse our portable oxygen concentrators here at LPT Medical. We offer all of the most popular and reliable units including but not limited to the Caire FreeStyle Comfort and the Inogen One G5. Both of which weigh under 5 pounds and offer outstanding battery life to keep you out and about for longer. Speak with one of our respiratory specialists to learn more.
COPD is a life-long, chronic disease that can cause a great deal of stress, anxiety, and physical discomfort. Because of this, people with COPD often have to grapple with depression and other psychological issues as a result of living with this difficult disease.
If you have COPD, you might be wondering what you can do to help yourself cope with the worry, fear, and distress that the disease causes. We've addressed this in previous posts on how to treat COPD-related anxiety and depression, but in this article we're going to introduce you to a specific kind of treatment: pet therapy.
Compared to other types of therapy, which often focus on unpacking difficult feelings and finding effective strategies to cope, pet therapy is much less intense. Pet therapy, also known as animal-assisted therapy, is more like a soothing technique, although it can be surprisingly effective at reducing anxiety and helping depressed patients improve their mood.
If playing with animals sounds like an appealing COPD treatment to you, there are a variety of ways you can reap the emotional and psychological benefits that companion animals have to offer. In this article, we're going to tell you all about animal-assisted therapy and how it can benefit patients with COPD.
We'll also show you the variety of options available for experiencing pet therapy for yourself, including ideas for seeking out more opportunities to interact with companion animals in your community. Continue reading to learn all about animal-assisted therapy and COPD, and how you can experience the extraordinary healing power of pets.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What is Pet Therapy?
 |
| Photo by Airman 1st Class Joshua D. King |
Pet therapy is a type of therapy that uses companion animals to help people with special needs or who suffer from physical diseases, disabilities, or mental illness. Animal-assisted therapy can help people with COPD cope with the difficult emotional and psychological aspects of the disease and help treat other mental conditions, like depression and anxiety, that are caused by COPD.
The idea behind pet therapy is simple: animals make people happy. But studies show that pets can do more than just give you a temporary mood lift; they can be powerful tools for warding off anxiety and depression, and even for physical health.
Pet therapy is a broad term that can include therapy dog programs, animal visits to nursing homes and care centers, owning your own pets, or the therapeutic benefits of interacting with animals in general. Sometimes animal-assisted therapy is facilitated by an individual therapy dog owner, and sometimes it is facilitated by a larger program or organization.
However, you can reap many the same benefits of facilitated pet therapy simply by owning your own pet or interacting with animals in general, both of which can be considered a form of pet therapy.
You are most likely to find facilitated pet therapy programs in hospitals, nursing homes, jails, mental rehabilitation centers, and physical rehabilitation centers. They can sometimes be hard to find outside of these settings, although some do home visits or participate in events that are open to the general public.
If you don't own a pet or have access to facilitated pet therapy, there are several other ways you can find animal companionship in your community. For example, volunteering at an animal shelter or spending time with a neighbor's pet can be a great way to unwind with some relaxing pet therapy.
In these next sections, we'll discuss these options and much more in greater detail. We'll help you understand the benefits and drawbacks of pet therapy and what you can do to access animal-related therapeutic activities and services in your local community.
What are the Benefits of Pet Therapy for People With COPD
 |
| Photo by Sgt. 1st Class Jon Cupp |
While no studies have tested the effects of pet therapy specifically on people with COPD, research has proven the effectiveness of pet therapy for a variety of other chronic diseases and conditions. There is a solid body of research on pet therapy that shows it can be surprisingly effective for helping people cope with a variety of physical, emotional and psychological problems that commonly affect people with COPD, including chronic pain, loneliness, and anxiety.
One of the best-researched areas of pet therapy, and the area in which it seems be most effective, is using pet therapy to treat anxiety and to help people cope with stress. Pet therapy has been shown to reduce anxiety, fear, and distress for many types of patients, including:
- Cancer patients
- Veterans with PTSD
- Patients with mental illnesses
- Patients with dementia
- People with addictions
- People in nursing homes and other long-term care facilities
- Elderly adults, which make up a significant portion of COPD patients.

Pet therapy can also help treat depression, which affects more than one quarter of people with COPD. According to several studies, animal-assisted therapy can cause "significant improvement" in depressive symptoms and in patients suffering from clinical depression.
While you can't expect massive or life-changing improvements from animal-assisted therapy, there is robust research to show that it has noticeable, measurable, and clinically significant effects. Even short periods of pet interaction can measurably improve your mood and stress level; one study, for instance, showed that interacting with a therapy dog for just thirty minutes can lower blood pressure and reduce anxiety.
Pet therapy can also reduce physical ailments like chronic pain, a symptom commonly suffered by people with COPD. For example, one study showed that patients with fibromyalgia experienced significantly decreased pain, decreased emotional distress, decreased fatigue, and improved mood after spending only a short period of time with a therapy dog.
Here is a list of some of the most important benefits you can gain from pet therapy:
- Reduced stress and sensitivity to stressors
- Reduced anxiety
- Enhanced mood
- Increased social interaction
- Reduced loneliness
- Reduced depression
- Decreased blood pressure (in the short term)
- Reduced respiratory rate (in the short term)
- Reduced stress hormones
- Increased quality of life
Facilitated Pet Therapy

|
More hospitals, nursing homes, and other physical care facilities are beginning to use therapy dogs and other forms of animal-assisted therapy to help improve happiness, anxiety, and quality of life for their patients. As someone with COPD, you are most likely to have access to facilitated pet therapy in the hospital.
Many hospitals allow therapy dogs to visit patients, and some even house their own animal-assisted therapy groups. If you have COPD, there's a good chance that you will spend some time in the hospital at some point due to an exacerbation or another COPD complication. If you do, you can ask hospital staff if they offer any kind of animal-assisted therapy that you could take advantage of.
Not everyone is lucky enough to get a visit from a therapy dog while in the hospital, but if you do, it can significantly improve your mood and the quality of your stay. If you ever have the opportunity to participate in animal-assisted therapy, you should take it, as long as your doctor says it won't be too risky.
Most of the time, it is difficult to access facilitated pet therapy unless you are residing in a hospital, nursing home, or another long-term care center. However, you may be able to find therapy animals in your area who do home visits or spend time in places that are open to the public.
You could also ask your doctor if there are any animal-assisted therapy programs or events hosted in or near your hospital or medical practice. If they don't offer any kind of pet therapy, you might be able to encourage them to consider utilizing therapy animals in the future.
Service Dogs
Owning your own service dog can confer many of the same benefits of pet therapy while also providing everyday physical support. Service dogs can help patients with COPD in a variety of ways, especially patients who are disabled or suffer from severe limitations in physical mobility.
For example, service dogs can be trained to open doors, retrieve items from the floor, and notify other people nearby if you need help. Having a therapy dog to help with these small tasks can make a big difference in the life of someone with severe COPD.
Therapy dogs can also carry items for you, which reduces your load while walking and allows you to focus your energy on controlling your balance and breathing. If you use supplemental oxygen, you could even use a service dog to carry spare oxygen tanks for you when you're out and about.
And, of course, interacting with a therapy dog on a regular basis can help improve COPD-related stress, anxiety, and depression. The companionship you get from owning a pet, especially a service dog, can also help you feel more confident, less lonely, and more fulfilled in life.
Should You Own Your Own Pet?

You don't need a trained therapy dog or structured animal-assisted therapy to enjoy these improvements in mood, psychological symptoms, and quality of life. Simply owning a pet can confer many of the same benefits as pet therapy.
If you suffer from COPD-related anxiety, depression, or chronic pain, getting a pet can be a huge help for improving your mood and reducing your psychological symptoms. Caring for an animal can also give you a wonderful sense of purpose and belonging, and interacting with your pet on a regular basis can improve both physical and emotional pain.
Owning a pet can also help you establish a healthier, more regular daily routine. For example, it can be helpful if you suffer from depression to have to get up to feed your pet at the same time every morning, or you could use your pet's schedule to help you remember to exercise and take your medications.
For COPD patients, owning a pet can even improve their symptoms by helping them live a more physically active lifestyle. Most pets require exercise and play time, which are great opportunities for people with COPD to get up and moving.
However, there are many reasons why certain people who have COPD cannot or should not own pets. Pets are a major responsibility, and many patients simply don't have the time or energy to take on the task of caring for and cleaning up after a pet.

Another concern is the fact that pets can expose you to extra amounts of allergens and respiratory irritants that could inflame your lungs and make your COPD symptoms worse. Even indoor pets introduce potentially irritating dust and dander into your home, while pets that spend time outside can track in all kinds of pollen, pollution, and other hazardous particles from the outdoors.
Here are some of the things to consider before owning a pet if you have COPD:
-
Many animals, especially dogs, require a certain amount of physical activity to care for. If you have very limited mobility or have difficulty walking and exercising because of your COPD, you may not be physically able to take care of a pet that requires regular walks and play time.
-
Pet fur can be a problem if your lungs are sensitive to allergens or airborne particulates. Not only do most pets shed--and some shed a lot--but their fur tends to collect pollen, dust, pollution, and other respiratory irritants that could make your COPD worse.
-
Some people with COPD find it difficult enough to take care of everyday cleaning tasks and responsibilities. If you own a cat or dog, those cleaning tasks and responsibilities will only multiply as you care for and clean up after your pet.
- If you struggle with exercise or physical tasks you should look for a pet that doesn't require a lot of energy or clean-up, such as a fish, reptile, or bird. If you must get a dog or cat, consider getting a smaller breed that is low maintenance and allergy-friendly.
Luckily, even if you can't own your own pet, you can find many other opportunities for pet therapy if keep your eyes open. In the next section, we'll give you some ideas for how you can find companion animals to interact with in your community, even if you don't have access to a facilitated animal-assisted therapy program.
Taking Pet Therapy Into Your Own Hands

Unfortunately, facilitated pet therapy services aren't as widespread or easy to find as most patients would like. Many pet therapy programs aren't accessible to the general public and only operate in hospitals, nursing homes, and other care centers.
However, there's no need to worry if you are unable to own your own pet or find a pet therapy center near you. Studies show that you don't need a therapy dog or a full-time pet in order reap the benefits of pet therapy; even brief, occasional interactions with animals can have large effects on mood and well-being.
If you wish to own a pet but can't, or simply want to try pet therapy to help you manage your COPD, you can take matters into your own hands and take advantage of opportunities to interact with pets in your local community. That might mean spending more time with your neighbors' pets, volunteering at an animal shelter, or offering to pet sit for friends and family.
Volunteer at an Animal Shelter
|
|
| Photo by Stacy A. Ouellette |
Volunteering to help out with pets in need is of the most rewarding ways to interact with animals. That's what makes volunteering at an animal shelter or humane society such a great alternative to facilitated pet therapy.
At an animal shelter, you will have the opportunity to provide comfort and companionship to a variety of different cats and dogs. It can be an extremely rewarding experience because, in addition to helping yourself, you will be making a difference in the lives of animals who don't have a home or family of their own.
You might be wondering what volunteering in an animal shelter looks like and what kinds of activities you can do with the cats and dogs. The answer will depend on your local shelter's policies; however, most shelters allow public volunteers to walk the dogs and spend time playing and interacting with the animals indoors.
Even if you don't have the energy to roughhouse with the animals or take the dogs on long walks, you can still offer to provide quiet companionship to the older or more mellow animal residents. Some volunteers even come to sit and read to the animals from a book, which can be heartwarming and beneficial to both you and the lonely cats and dogs at the shelter, even if they can't understand the words.
Another benefit of volunteering in an animal shelter is the opportunity to see a variety of different kinds of dogs and cats in all breeds, shapes, and sizes. However, since pets are constantly being shuffled in and out of shelters, you might not be able to see the same animals every time.
Borrow Fluffy Companions from Friends and Family

Another alternative if you don't have an animal of your own is to spend more time with pets that belong to your neighbors, family, and friends. That way, you can reap the benefits of spending time with animals without having to invest your time and money into a pet of your own.
All you have to do is let your friends and family know that you could use an occasional pet companion, and ask if any of their pets would be well suited for the cause. There's a good chance that at least one person has a friendly animal and won't mind you dropping by to pay regular visits.
Spending more time in the home with a friend or family member's pet is also an opportunity to get out and socialize a bit more. This can be particularly helpful if you suffer from depression, because it gives you something to look forward to and a reason to get out of bed and out of the house.
If you don't mind the extra commitment, you might even ask the pet's owner if you can borrow their pet every so often for a longer period of time. Caring for a pet over an afternoon or weekend isn't nearly as difficult as caring for a pet full-time, and it will provide even more time for bonding and relaxing.
Be the Go-To Pet Sitter

Another way you can spend more time with pets that aren't your own is by offering to pet sit for friends, family, and neighbors. That way you can get some pet therapy time while doing someone a big favor at the same time.
For example, if someone you know has a friendly pet that they have to leave behind for a vacation or business trip, offer to look after their pet while they are away. Most pet owners would be happy to leave their pet with a caring companion and appreciate the opportunity to save money on pet care.
If you are retired or work a schedule where you are home during the day, you could offer to check in on your neighbors' dogs or cats while they are away at work. That way, you can get regular pet therapy time while also providing companionship to an animal that would otherwise be left home alone all day.
Even though pet sitting requires you to take on more responsibility than simply petting a therapy dog, it's a win-win-win situation for both you, the animal, and the pet's owner. You get the opportunity for even more animal interaction while helping out both the pet and the person who owns it.
Other Opportunities for Animal Interaction

If you are willing to get creative, there are even more ways connect with other pets if you can't own one of your own. If you have a computer with a decent internet connection, you can even do it from your own home.
One option is to spend some time watching animals on the internet, and we're not just talking about cat videos on YouTube. You can actually watch live-action streaming video of adorable animals in zoos, shelters, and other places all across the world. You can even find some animal shelters with live-cams featuring toys that you can twirl or jiggle with a press of a button, allowing you to actually interact with the cats and dogs from your computer screen!
Here are some examples:
-
The Houston Zoo has live cameras streaming footage of a variety of animals every day, including gorillas, giraffes, rhinos, elephants, flamingos, and more!
-
This article has a list of interactive webcams that you can use to view and interact with pets at cat and dog shelters and other animal rescue groups. Some have interactive toys, and they're all full of fluffy, adorable pets.
- MangoLink is a website with links to dozens of live animal webcams all across the world. They have streams of every category of animal you can imagine, including birds, farm animals, insects, reptiles, and fish.
Another option, if you are an animal lover and physically able enough, is to volunteer at a zoo or animal rehabilitation center. Some may allow you to participate in some kinds of animal care or feeding, but you may not able to work directly with the animals. However, you may be able to work near them, and you'll have the satisfaction of knowing that you are working to support their care and well-being.

You can also spend time seeking out wild animals in your local area--from a distance, of course. There are many ways you can spot and observe local wildlife, including hiking, bird-watching, and wildlife tracking. Even just putting a bird or squirrel feeder in your yard can provide you with delightful animal sightings from the comfort of your own home.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146')}}
Conclusion

While pet therapy isn't a cure for the emotional hardships that COPD patients face, it can help people with COPD cope with the stress and anxiety of living with a chronic disease. It can also help people who suffer from COPD-related depression, helping them re-connect with the outside world and overcome feelings of loneliness and isolation.
Pet therapy isn't right for everyone, especially those who have allergies to pet dander or who are extremely sensitive to airborne allergens. But if you like animals and don't have
Living with a chronic disease like COPD comes with many challenges, and financial challenges are no exception. Many people who are diagnosed with the disease find themselves blindsided by the high costs of medical equipment, prescription medications, and other necessary treatments.
While Medicare or other insurance providers can cover some of these costs, patients are often still responsible for a large portion of the bill. Many of these costs are rigid and unavoidable, but some can be minimized with a little forethought and research.
Of all of the medical expenses associated with COPD, the cost of medication is one of the most frequent, variable, and burdensome. Fortunately, it's often possible to get discounted prescription medications or payment assistance if you know where to look.
In this article we're going to help you save money by showing you how to find the best prices, discounts, and financial assistance for prescription COPD medications. We know not everyone can afford to pay for their medicine at full-price, and the options on this list can help you reduce the pressure that your disease puts on your budget.
It's difficult enough to handle the emotional and physical hardships of COPD without having to worry about money, too. So if you want to reduce your medical expenses, keep reading to learn about 11 different ways you can save money on prescription medications for COPD.
Go Generic

Many people cannot afford the inflated prices of name-brand medications. Luckily, you can often find off-brand, generic versions of the same medication at a much lower cost.
Although you should always check with your doctor first to be certain, you can rest assured that most generic medications work just as effectively as the more expensive versions. Despite the difference in cost, generic medicines are safe to use and are usually nearly identical to their name-brand counterparts.
All you have to do is talk to your doctor to potentially save a ton of money on your prescription medications. If there is an equivalent generic version of any of your medications available, your doctor will note it on your prescription slip to let the pharmacy know it's okay to use.
Order Your Prescription Online

If you want to save a decent amount of money on your medication, you'll have to look beyond your local pharmacy. Although they might be quick and convenient, brick-and-mortar pharmacies also tend to have the highest prices.
Unfortunately, many people don't realize that they have any other option besides their local pharmacy. In reality, there are dozens or more legitimate online and mail-order retailers that sell prescription medications, too.
However, make sure to research any online pharmacy thoroughly before entrusting it with your prescription. While many are trustworthy, some sites are unreliable, lack quality control, and even sell potentially dangerous counterfeit medications.
Always choose online pharmacies that are based in the United States and look for the “VIPPS” logo. VIPPS stands for “Verified Internet Pharmacy Practice Site,” and it's a good indicator of an online pharmacy's safety and legitimacy.

Also look for seals of approval from third-party organizations like the Internet Mail-Order Pharmacy Accredidation Commission (IMPAC), the Manitoba International Pharmacists Association (MIPA) or the Verified Internet Pharmacy Practice Sites (VIPPS). Accreditation from one of these organizations is another good sign that it's a pharmacy you can trust.
You should also avoid any pharmacy website that prices their drugs significantly cheaper than the typical market price because they might be selling dangerous counterfeit drugs. It's a good rule of thumb to assume that if a price seems too good to be true, then it probably is!
If you ask, your doctor or even your insurance provider might be able to recommend a trusted online pharmacy you can use. As long as you do your due diligence and find a legitimately licensed online pharmacy, you should not have to worry about the quality or safety of your medication.
Get a Prescription Discount Card

Prescription discount cards are another option that can significantly reduce the cost of your COPD medication. You can often get these discount cards from your doctor, local pharmacy, and other organizations like AAA. They are also available from a variety of online websites like WebMD and retail stores like Walgreens.
Many people are skeptical of prescription discount cards because they are free and widely available. However, they aren't a scam. All you have to do is scan your discount card at participating pharmacies to get a reduced price for thousands of different prescription drugs.
You can get a prescription discount card whether or not you have private health insurance, but you can only use one or the other to pay for your medication at any given time. However, prescription discount cards can often get you better prices than you can get through private insurance, especially for generic drugs.
To get the best deal, have the pharmacist run both your insurance and prescription discount card before you pay. That way you can see the price of the medication for both options and figure out whether your insurance company or discount card will give you the better deal.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Apply for a Patient Assistance Program

Did you know that many pharmaceutical companies have their own programs to help patients pay for their medicine? That's right, nearly all of the major drug companies have some sort of financial assistance program for all of their major medications.
These programs are usually called Patient Assistance Programs (PAPs), and they are designed to help low-income patients who cannot afford to pay the full cost of their medication. They offer discounted and sometimes even free medicine to patients who qualify.
Every patient assistance program has its own eligibility requirements that you have to meet in order to get free or discounted medication. While the exact criteria vary from program to program, there are three main requirements that nearly every PAP has:
-
Must Have Low Income: You must not make over a certain amount of income to be eligible. The cutoff is usually about two times the federal poverty income level.
-
Must be a US Resident: Most PAPs require you to live in the United States or be a US citizen to qualify.
- No Outside Prescription Coverage: You usually are not eligible if you are already part of another private or public prescription coverage program. You may not be eligible if you have public or private insurance.
You can usually figure out whether there's a patient assistance program for a drug you take by visiting the pharmaceutical company's website, but the information is sometimes difficult to find. If you need help finding a program that you qualify for, your doctor or pharmacist might be able to help
You can also find online tools that allow you to search through all available patient assistance programs all in one place. These sites make it much easier to find financial assistance programs that you might be eligible for.
All you have to do is search the name of a medication that you've been prescribed, and the site will pull up any and all assistance programs that are available for that drug. Then you will need to fill out an enrollment form, which the pharmaceutical company will then review to determine if you qualify for the program.
Here are a few sites you can visit to search for a patient assistance program that works for you:
- RxAssist
- The Partnership for Prescription Assistance
- RxHope
- NeedyMeds (This site also includes state-sponsored financial assistance programs in their database.)
Participate in a Clinical Trial

There are still many questions to answer about COPD and new treatments that need be studied. Medical research organizations regularly conduct studies on COPD medications and are often looking for participants to participate in clinical trials.
If you have COPD, you can apply to be part of a clinical trial that needs volunteers with the disease to test new treatments and medications for COPD. While all clinical trials have some risks, most are relatively safe and you will always get a full explanation of the study's risks and benefits before you participate.
There are several benefits you can get from volunteering for a clinical trial, the first being that they will pay for any medications or treatments they give you throughout the course of the study. You might even have the opportunity to try a new treatment before it is widely available to the general public.
Another benefit is the knowledge that you are helping to further scientific research on COPD. The study you take part in could end up leading to new medications, treatments, or drug combinations that could help many other people who have the disease. Some clinical trials also pay hundreds or thousands to compensate participants for their time, too!
To learn more about participating in a clinical trial, visit the National Institutes of Health website. To search for a clinical trial in need of participants, visit clinicaltrials.gov or search for COPD studies on healthline's clinical trial search tool.
Comparison Shop
Although you can get your prescription filled at any pharmacy, not all are equal. Many people don't realize that the prices of different drugs can vary widely between pharmacies, even pharmacies in the same city or on the same street corner.
If you want the best deal, you'll have to price shop to find the local pharmacy with the lowest prices for your medication. To make your search easier, you can use online price comparison tools like GoodRx or LowestMed to find the best local prices for a particular medication.
Get Free Samples

Pharmaceutical companies often advertise their medications by providing boxes of free samples directly to medical practitioners. Many doctors are happy to give some free samples to patients who need short-term doses or can't immediately afford the medication.
Some doctors will give you a couple weeks' worth of free samples if you ask, and they might even give you more if they know you are struggling to afford your meedication. While this is not a permanent solution, it might still save you a decent chunk of cash up front.
Free samples can also hold you off in the short term if you find yourself in a situation where you can't afford a new medication right away. Your doctor might be able to give you an immediate supply of medicine via free samples so that you aren't left un-medicated until you come up with a more permanent solution. This is also useful if you have to wait for medicine from a cheaper online pharmacy to arrive in the mail, since it usually takes at least one month.
Get Longer-term Prescriptions

If you have a medication that you know you'll be needing to take long-term, ask your doctor if you can get a larger prescription. Getting more pills per prescription means fewer trips to the pharmacy, and it also means fewer co-pays.
For example, if you can get a 90-day prescription instead of a 30-day prescription, you'll only have to pay one co-pay. So, instead of paying a separate co-pay every thirty days, you'll only have to pay it once every three months.
Ask Your Pharmacist for a Discount

A pharmacy's “list price” for a medication is usually much higher than the price that most people actually pay. In fact, most pharmacies actually expect patients to make use of coupons and other discounts rather than pay full price.
Whenever you go to pick up a prescription, always ask the pharmacist, “Is this the lowest price you can offer?” Many pharmacists have access to a variety of coupons and discount cards, and most will be happy to look for one that they can apply to your medication. It never hurts to ask, and you might be pleasantly surprised!
Tell Your Doctor About Your Financial Concerns
When doctors prescribe medication and other treatments, they don't always think about the financial burden it puts on their patients. That's why you should always speak up if you're on a budget or if you're worried about the cost of anything your doctor recommends.
If you tell your doctor that a treatment or medication is too expensive, there's a good chance your doctor can help you get a discount or find a cheaper alternative. As we mentioned earlier, many doctors also have access to a limited amount of free samples that they can give away, which can help reduce your costs temporarily.
Doctors understand the huge financial burden that medication can put on their patients, and most are willing to help you find more affordable options when they can. However, your doctor probably won't know you need help if you don't ask, so never be afraid to bring up any financial concerns you have about your treatments or medications.
Other Financial Assistance Programs

We've already talked about patient assistance programs and prescription discount cards, but there are a variety of other nonprofits and other patient advocacy organizations out there that might be able to help you.
Here is a list of several organizations and online tools you can use to find a patient financial assistance program that you are eligible for:
-
State Pharmaceutical Assistance Programs: This document lists all of the US states that offer financial assistance for patient prescriptions along with links to each specific program. Some programs only apply to people who meet specific criteria: e.g. patients above a certain age, patients with specific diseases, people with disabilities, patients without insurance, etc.
-
Patient Services, Inc.: This organization is dedicated to helping people who are living with chronic illnesses, including certain types of COPD. They provide financial assistance for qualified patients that can include insurance premiums, co-pays, and travel assistance.
-
PAN Foundation: This nonprofit is dedicated to helping people with certain rare and chronic diseases afford the treatments and medications they need by providing financial assistance for insurance deductibles and co-pays. You must have health insurance and make no more than five times the federal poverty level in order to be eligible.
- The HealthWell Foundation: This is another nonprofit organization that helps under-insured patients with specific chronic and life-altering diseases pay co-pays for the medication and treatments they need. You will need to have health insurance and make no more than five times the federal poverty level in order to be eligible.
Note that many of these are need-based programs or only apply to patients with specific diseases that underlie or co-occur with COPD ( e.g. cystic fibrosis, Alpha-1 Deficiency, or Pulmonary Fibrosis). You might need to have low income or a disability in order to qualify for certain types of assistance.
However, it's worth taking a look and reaching out even if you don't have a disability or can't provide proof of financial need. You'll never know what opportunities are out there for you unless you ask!
Conclusion
Between the cost of hospital visits, medical equipment, and supplemental oxygen rental fees, managing COPD can get very expensive. If you add on to that the price of recurring monthly prescriptions, the cost of treating the disease can get unmanageable fast.
Luckily, with a little research and smart planning, you can usually find a way to get most COPD prescription medications at a discount.
If you are feeling strained under the weight of your medication expenses, don't hesitate to ask your doctor for advice and seek other avenues of support. If you take the time to pursue all the cost-saving opportunities we've discussed in this article, chances are you'll be able to find at least one solution that works for you.
Image attribution: https://traineracademy.org/
Lung function decline is a defining characteristic of COPD, and it gets worse as the disease progresses. Because of this, most COPD patients eventually have to begin using supplemental oxygen to help their lungs once they become too weak to absorb enough oxygen on their own.
The purpose of supplemental oxygen is to deliver extremely oxygen-rich air to your lungs, usually using a pressurized oxygen tank or an oxygen concentrator. This air, generally about 85-95 percent pure oxygen, allows your lungs absorb more oxygen with every breath.
Supplemental oxygen is a very important part of COPD treatment because it helps your lungs take in enough oxygen to supply your organs and tissues with the oxygen they need. Without it, your blood oxygen saturation can fall to unhealthy levels—a condition called hypoxemia—which can lead to serious, life-threatening complications over time.
Supplemental oxygen is also important for treating acute COPD symptoms, and can help you when you feel breathless from exercising or when your symptoms flare up. Many patients also use supplemental oxygen when they sleep to treat low blood oxygen levels during the night.

Despite how often supplemental oxygen is used and prescribed, it can be dangerous if you don't understand the risks. Oxygen is highly flammable, and you have to take special precautions when you use it to reduce the risk of a fire.
Even though they are rare, oxygen leaks and major fires can happen if you don't practice proper oxygen safety. High oxygen levels can make objects that wouldn't usually be a risk highly flammable, such as grease and oily creams. It also causes fires to burn hotter and spread faster than they normally would.
Even small sparks or flames can can cause combustion when there's excess oxygen in the air, which is why it's so important to understand how to use your oxygen safely and minimize the risks.
In this article we're going to show you how to practice proper oxygen safety so you can avoid accidents, injuries, or fires from using supplemental oxygen. We'll explain the benefits and risks of oxygen therapy, how to minimize fire hazards, and tell you how to follow proper safety protocols when using, storing, and transporting your oxygen.
If you or a loved one uses oxygen therapy to treat COPD or another respiratory condition, then it's important for you to know how to use supplemental oxygen as safely as possible. This guide will teach you the basics and provide you with a variety of valuable tips you can use in your everyday life if you are prescribed supplemental oxygen.
The Potential Dangers of Using Supplemental Oxygen

Before we discuss how to use oxygen safely, it's important to understand the potential risks. If you know what to look out for, you're less likely to make a dangerous mistake.
The main immediate danger that supplemental oxygen poses is its flammability. When oxygen leaks out into the air from your tank, nasal cannula, or mask, it can raise oxygen levels in the room or in your immediate area, which significantly increases the flammability of everything nearby.
A certain amount of leakage from your nose and nasal cannula is inevitable, meaning there is a constant flammability risk when you use your supplemental oxygen. That's why you have to take a variety of fire-safe precautions any time oxygen is in use, even if your oxygen tank isn't nearby.
It is also important to make sure that all the oxygen from the tank goes straight into your lungs through your mask or nasal cannula instead of leaking into the air. Leaky tanks, faulty valves, and carelessness when opening and closing the valve can make the surrounding air extremely flammable, putting you, your belongings, and others nearby at risk.

Standard oxygen tanks, the most common type of equipment used to provide supplemental oxygen, pose hazards of their own, as well. The oxygen must be highly pressurized when it's stored in the tank, which means oxygen tanks can explode violently or “take off like a rocket” if the container is somehow damaged and ruptured.
You can avoid this danger by using an oxygen concentrator machine, but they tend to be pricier and harder to come by. Many patients don't have access to anything other than pressurized or liquid oxygen tanks because their budget, insurance, or medicare provider won't cover it.
The Benefits of Using Supplemental Oxygen

Despite the risks, supplemental oxygen is generally very safe to use as long as you use it carefully and as directed. It's also a very important part of treatment for people with COPD and other respiratory conditions who can't get enough oxygen to stay healthy on their own.
By raising your blood oxygen levels and taking some of the strain off your lungs, supplemental oxygen therapy can significantly improve COPD symptoms like breathlessness, coughing, wheezing, and fatigue. It can also help you be more active and participate in more of life's activities by making it easier to walk, exercise, and keep your symptoms under control.
Here are some more of the benefits you can gain from supplemental oxygen therapy:
- Improved mood and mental alertness
- Improved exercise ability and exercise endurance
- Improved energy and reduced fatigue
- Improved cardiovascular function
- Reduced hypoxemia and risk of hypoxia
- Improved sleep
- Reduced breathlessness
- Reduced risk of COPD complications including pulmonary hypertension and heart failure
- Overall improved quality of life
It's hard to overstate the importance of supplemental oxygen for COPD. If you doctor prescribes oxygen to you, it's vital that you use it exactly as directed according to your treatment plan.
Many patients don't follow their supplemental oxygen treatment regimen well enough because of inconvenience, aesthetics, or discomfort, but not using your oxygen as directed can worsen your COPD and lead to life-threatening complications, including heart failure. Talk to your doctor if you are having trouble using your oxygen or sticking to your treatment plan.
Tips for Using Oxygen Safely

Now that you better understand the benefits and potential risks of oxygen therapy, we're going to show you how to practice proper oxygen safety. There are many important precautions that everyone who uses supplemental oxygen must take in order to reduce the likelihood of fires and burns.
In the next sections, we'll give you a variety of tips for preventing oxygen leaks and minimizing fire hazards in your home. We'll explain all the different flammable substances and spark risks that you should look out for and how to safely cook while using oxygen at home.
We'll also give you advice on how to store and transport your oxygen tanks so they won't leak or get damaged. To learn all of this and more, continue reading to learn all about how to practice proper oxygen safety in and outside of your home.
Prevent Oxygen Leaks

One of the most important parts of supplemental oxygen safety is to prevent oxygen from leaking out of your tank or mask. If too much oxygen escapes into the air, it poses a serious fire hazard.
Even a small spark or heat from a stove burner can cause oxygen in the air to ignite and set fire to you or objects nearby. That's why it's important to know how to handle your equipment safely when you use supplemental oxygen.
Here are some tips for preventing oxygen leaks:
-
Always exercise care when turning the valve on your oxygen tank. Turn the valve slowly so you don't release too much pressurized oxygen at once.
-
Do not forget to close the valve on your oxygen tank when you are not using it. Take the time to double check if you aren't sure that it is closed all the way.
-
Visually inspect any oxygen tanks you have, including the valves, regularly. Check the outside of the tank for noticeable wear, tear, or damage, and check for any noticeable leaks.
-
Always store your tanks in a secure place where they won't tip, fall, or get damaged.
-
Liquid oxygen tanks will leak if laid on their sides, so it's particularly important to store liquid tanks upright with a cart or chains.
- Always use clean, undamaged tubing during oxygen therapy. Never use damaged equipment or tubing with holes or tears.
No matter how careful you are to prevent leaks from your tank and tubing, a small amount of oxygen will inevitably leak out near your nose and mouth while you use supplemental oxygen.
That's why it's so important to stay away from heat, sparks, and anything else that could cause the oxygen to combust. We'll go into this in more detail in the following sections.
Keep Heat and Flame Away From Your Oxygen

If you remember nothing else about oxygen safety, you should make sure you remember this: never, ever use your oxygen around an open flame. Doing so could quickly and easily cause a fire, which is why it's so important to keep your oxygen away from flames at all costs.
Open flames aren't the only hazard, however; even everyday heat sources like stoves and space heaters can also be dangerous. Anything with a heating element can pose a fire risk when you are using supplemental oxygen.
Here are some tips for avoiding heat and flame hazards when you use oxygen:
-
Be very cautious when using supplemental oxygen while you cook. Always move at least five feet away from the stove to use your supplemental oxygen, and never wear your nasal cannula near a gas stove or open flame.
-
Your oxygen tank and other equipment should also be kept at least five feet away from the stove and other heat sources at all times.
-
When you are using oxygen, beware of all sources of open flames: this includes lighters, matches, candles, fireplaces, cigarettes, gas burners, etc. Do not use any of these items or allow anyone near you to start a flame while oxygen is in use.
-
Do not smoke or use an electronic cigarette or vaping device while using oxygen. E-cigarettes contain heating elements that could potentially ignite the oxygen that collects around your nasal cannula, causing severe facial burns.
-
Place “oxygen in use” signs in visible places near all of the entrances to your home (these are usually provided by your oxygen supplier). This will ensure that visitors and emergency personnel know to be cautious of the high flammability risk.
-
Make sure to inform people around you of the risks of heat and open flame when you use oxygen. If needed, place a "no smoking, oxygen in use" sign nearby so others remember to be cautious.
- Take the same precautions that you would when using supplemental oxygen when you are near where you store your oxygen and extra tanks. Make sure you and everyone in your home knows where you keep your oxygen tanks and equipment and understand how to exercise proper fire safety.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Keep Your Oxygen Equipment Away from Electronics, Static Electricity, and Flammable Substances
|
|
| . |
While they don't pose as much of a risk as heated appliances and open flames, faulty electronic devices can also pose a fire hazard when you use supplemental oxygen. Some electronics and mechanical toys can also create tiny sparks that can cause fires in the presences of excess oxygen, which is why you shouldn't use them at the same time as you're using supplemental oxygen.
Another risk is static electricity build-up, the kind that happens when you drag your socks across the carpet or rub a balloon on your clothes. The "shock," or spark, that results when the static electricity dissipates can pose a fire risk when you are using supplemental oxygen. While it's impossible to avoid static electricity altogether, especially during the dry, winter months, you can reduce the risk of static sparks by avoiding certain types of clothing and fabrics.
Here are some tips for reducing the risk of fire from electronics and static electricity:
-
Don't use electronic appliances when using oxygen. This includes electric razors, mechanical toys, heating pads, electric blankets, electric toothbrushes, and electronic hair dryers, hair curlers, and hair straighteners.
-
Don't use any electronic device that produces heat when using supplemental oxygen. This includes electronic cigarettes.
-
Avoid static-producing fabrics like wool, nylon, and synthetic fabrics (e.g. polyester). Instead, choose clothing and bedding made of cotton, which is much less likely to produce static electricity.
-
Don't use any flammable products on your skin and hair, including flammable lotions, hair products, and hair sprays that could ignite due to heat or a static spark in the presence of oxygen. Especially watch out for products that contain petroleum and choose water-based ones instead.
-
Avoid using chapstick and oil-based lotions on your body, and especially your face, when using your supplemental oxygen, as they can cause severe burns if they ignite.
-
Avoid other flammable substances when using oxygen, including gasoline, paint thinner, cleaning fluids, aerosols, and sprays that contain alcohol.
-
Never use any aerosol sprays while using supplemental oxygen. This includes air fresheners, spray deodorants, and hairsprays.
-
Don't use alcohol-based hand sanitizers while using supplemental oxygen. If you use hand sanitizer before using oxygen, make sure that it has dried off of your hands completely before starting the oxygen or touching any of your oxygen equipment.
-
Using a humidifier during dry weather can reduce the amount of static build-up that occurs in your home. Keeping your house at an ideal humidity level (usually around 40 percent humidity) may reduce your fire risk when using supplemental oxygen and can also help your COPD symptoms.
- If you use an oxygen concentrator, always plug it into an empty, grounded outlet (an outlet with three holes instead of two). Never plug it into an extension cord, a faulty outlet, or an outlet that has other electronics plugged into it.

Even if you don't want to switch out your wardrobe for cotton-based clothes, consider at least switching to cotton bed sheets and blankets, especially if you use nighttime oxygen.
Static electricity from other types of fabric poses a much greater risk while you are asleep; this is partially because you are more likely to build up a static charge while shifting under your sheets, and partially because you might not be able to respond as quickly if a fire starts while you are asleep.
Use Your Oxygen in a Well-Ventilated Area
Using oxygen in a well-ventilated space is another important precaution that you can take to reduce your flammability risk and avoid fires. That means using your oxygen in an area with plenty of airflow and open space whenever possible.
Proper ventilation ensures that any extra oxygen in the air can quickly dissipate and leave the room before it builds up to the point of posing a significant fire risk. Beware of small, enclosed spaces; you should always try go outside or seek a more open area before beginning supplemental oxygen treatment.
Here are some tips for making sure you use your oxygen in well-ventilated places:
-
Make sure the ventilation system in your home is in good working order.
-
Crack the windows in your car if you are using supplemental oxygen while driving or transporting an oxygen tank.
-
Never place anything on top your oxygen tank. Doing so could cause any oxygen that leaks out to become trapped and build up to extremely flammable levels.
- Keep your oxygen tanks clean and in an open space where air can freely flow around them. Never store your oxygen tanks in an enclosed space or anywhere that doesn't have ventilation.
Prepare Your Home for Fire Emergencies

Even if you are very careful when using your supplemental oxygen, accidents can still happen. That's why, if you use oxygen in your home, you should be extra prepared in case a fire starts.
Here are some tips for home fire preparedness and precautions you should take if you or someone in your home uses supplemental oxygen:
-
Make sure your house has the recommended number of smoke detectors and they are all in good working order. Check the batteries often and replace them promptly when needed.
-
Make sure there is always a smoke detector in or right outside the room whenever you use supplemental oxygen.
-
Always keep a fire extinguisher in your home and within easy reach, especially while you are using oxygen.
-
Make sure your fire extinguisher is in good working order and replace it promptly when it expires.
-
Make sure you and everyone else in your household knows how to operate your fire extinguisher correctly.
- Have an evacuation plan and escape route planned in case of a fire emergency. Make sure everyone in your household knows what to do, where to go, and where to locate any safety equipment such as window escape ladders.
Keep Oxygen Equipment Away from Children

Now that you understand how dangerous supplemental oxygen can be if not properly handled, it should be clear why you should keep children away from your oxygen equipment. Many children are not old enough to understand the dangers of oxygen or to be trusted to treat the equipment gently.
If you have children in your home, you should keep your oxygen equipment secured and out of reach whenever possible. Large oxygen tanks can be particularly tempting for little children to play with and climb on, so it's important to instruct kids that they are off limits and keep a close watch to ensure that they stay away.
Large, heavy oxygen tanks can also be very dangerous to children and cause injuries if they fall. This is yet another reason to store your tanks properly and securely so they can't be tipped or knocked over.
Always Store and Transport Tanks Securely
 |
It's very important to make sure that you keep your oxygen tanks stored safely in a place where they won't be bumped or disturbed. You should keep any extra tanks in a stand or cart to ensure that they do not fall or get knocked over.
This is especially important when you are traveling with oxygen tanks, as there is a higher risk of the tanks getting jostled and tipped. Always keep your equipment carefully secured and protected any time you transport them from place to place.
Here are some tips for storing and transporting your oxygen:
-
Use an oxygen cart, stand, or chains to secure any extra oxygen tanks that you are not using. Never store them loose or unsupported.
-
Make sure all tanks are stored flat on the ground. Do not put them up on shelves or in any elevated place.
-
Transport oxygen tanks in your car by securing them in the main cabin of your car, not in the trunk. Open your car windows slightly to ensure that you have adequate airflow and ventilation.
- Keep your tanks in a moderately temperature-controlled space, like an air conditioned room. Do not leave your equipment in the sun, in a hot car, or allow them to be exposed to temperature extremes.
Exercise Care When Handling Your Equipment

Overall, it's important to always handle your equipment gently and with care. It's important to protect your tanks from damage to prevent leaks and dangerous explosions.
Here are some tips for handling and using your oxygen equipment with care:
-
Be careful not to drop your oxygen tanks. Use a stand, cart, or another safe container to secure your tanks when you move them from place to place.
-
Never handle your tanks roughly or carelessly.
-
Never drag or roll your tanks across the floor, set them down too hard, or let them bang against walls or other objects.
-
Always lift your oxygen tanks by holding the bottom or sides of the tank; do not lift or carry your tanks by holding the cap or valve.
-
Never cover your oxygen equipment, including tanks, tubing, and electrical cords. Do not put them underneath fabric, furniture or bedding.
-
Do not use an oxygen tank that has been dropped or damaged.
Conclusion
Knowing how to use oxygen safely is extremely important for anyone with COPD. Most patients end up using supplemental oxygen at some point over the course of their life, and knowing what precautions to take can prevent devastating fires and injuries.
Even though most people who use supplemental oxygen don't have any problems, all it takes is one poorly-timed mistake or a stroke of bad luck to cau


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!















