.png)
No matter where you are or what you’re doing, you’re always being exposed to disease-causing pathogens. And while this may seem like a scary concept, you'll be happy to know that your immune system is working around the clock to fight off this bacteria and keep your body healthy. At least, that’s what it’s supposed to do…
Immunodeficiency, also called immune deficiency, is a state in which the body’s ability to fight infectious disease is compromised. Primary immune deficiency is one that’s inherited through genetic mutations while secondary, or acquired immune deficiency is one that’s caused by environmental factors, i.e., bacteria, viruses, or immunosuppressive drugs like cigarettes.
Recently, researchers have focused their sights on understanding the effect of chronic obstructive pulmonary disease (COPD) and other respiratory conditions on the immune system and what role the immune system plays in causing COPD. While COPD is not classified as an autoimmune disease (a disease that causes the immune system to attack the body), it’s still linked to the immune system in a number of ways. According to a study published in the American Thoracic Journal, COPD patients are more prone to respiratory infection and they’re less likely to recover from it than those without the disease.
While the correlation between immune deficiency and COPD is complex, it’s important for you to understand because it has a profound effect on your health and wellbeing. For most people, getting sick is just a part of life. However, for someone with COPD, getting sick could mean being at a higher risk for life-threatening exacerbations.
In the following sections, we’ll discuss how the immune system works, the various types of immune disorders, and most importantly, where COPD fits into all of this. Your pulmonologist and primary physician should be your first line of contact when it comes to improving and maintaining your immune system, so be sure to reach out to him/her if you have any questions or concerns.
How Does the Immune System Work?
Just like the name suggests, the ‘immune system’ isn’t one specific entity; it’s a whole host of processes that occur throughout the body that work in tandem to protect you from disease-causing microorganisms. In a healthy person, these processes are all running at full force and working together effectively as the body’s first line of defense.
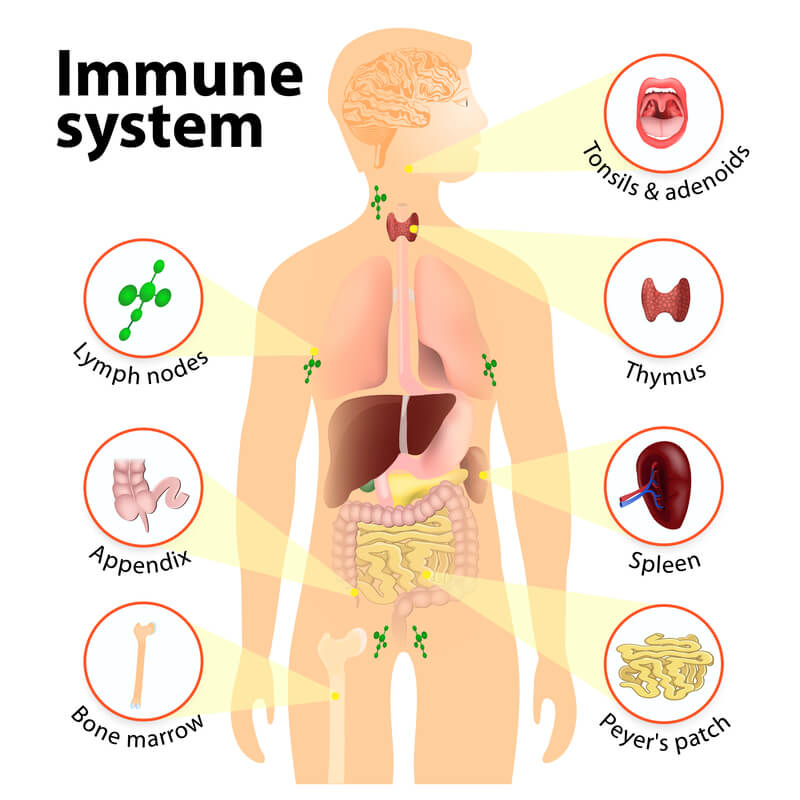
The immune system is one of the most complex parts of the body because it’s made up of a variety of different organs, cells, and proteins. There are three main tasks that the immune system is responsible for in the body:
-
Recognizing harmful substances in your environment and keeping them out of the body.
-
Neutralizing harmful pathogens inside the body such as parasites, fungi, viruses, and bacteria, then removing them.
- Fighting cancerous cells in the body.
Innate Immune System
All immune responses in the body can be divided into one of two different categories: innate or adaptive. The first of which, innate, is characterized by the body’s natural ability to fight harmful substances. Most of the components that make up you innate immune system are present at birth, but they can still develop and adapt over time.
Physical Barriers
While you may not think of your skin, eye lashes, and nose hair as part of the immune system, all of these are considered “physical barriers” and keep harmful substances from entering the body. The skin, for example, has a very low permeability, meaning it’s difficult for foreign substances to enter the body through it. However, other parts of the body like the mouth, nose, ears and eyes are open entry points to the rest of the body, this is why they need extra layers of immune protection.
Defense Mechanisms
Other innate immune responses in the body include things like saliva, mucous, tears, sweat, and secretions. Saliva, for example, plays an important role in managing bacteria in the mouth that causes gum disease. You may simply think of saliva as “water,” which is mostly what it is. However, saliva also contains a number of other substances like electrolytes, mucus, antibacterial compounds and various enzymes, all of which play a number of roles in protecting your oral health.

One important thing to note about your body’s natural defense mechanisms is that there’s a balance to all of it. When your body produces the ideal amount of saliva, mucous, tears, and sweat, you feel good. However, if something alters these processes, the defense mechanisms may be working against you. For example, smoking cigarettes results in high mucus production in the body. While mucus typically helps the body, too much of it can lead to airway obstruction and difficulty breathing.
Another way smoking affects the innate immune system is through the destruction of cilia. Cilia are tiny hair-like protuberances found in the lungs and wave back and forth to keep mucus and other substances out of the lungs. Smoking temporarily disables cilia, and long-term smoking can damage them meaning you’ll be more likely to get sick or experience difficulty breathing.
Inflammation
Inflammation is another key component of the innate immune response. Think of inflammation as a sort of signal that something is wrong. If you get an injury or an infection, inflammation occurs and white blood cells are sent to deal with the issue. Inflammation is a normal reactionary process for your body, but when it goes on for too long it may result in a chronic illness. What’s more, if inflammation never occurs, a seemingly harmless infection could become much more serious.
Adaptive Immune System
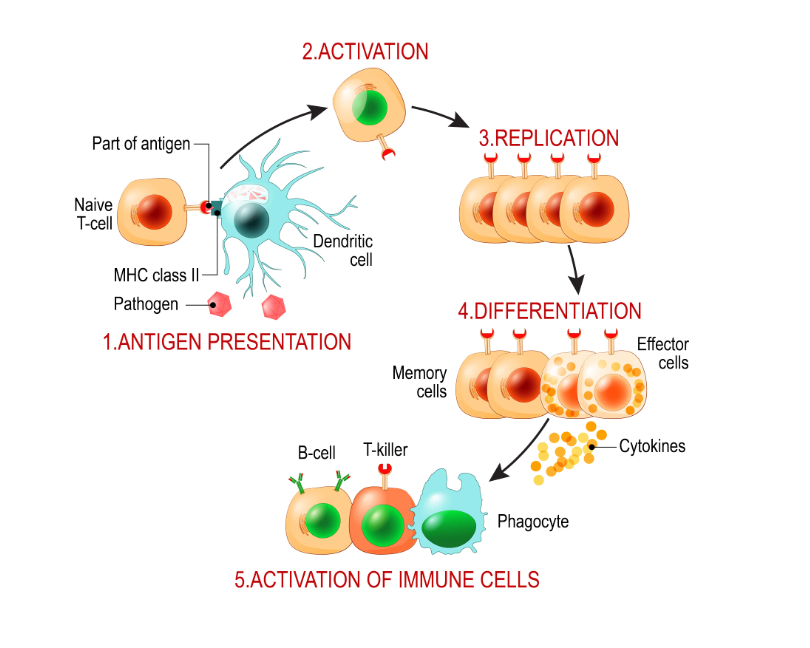
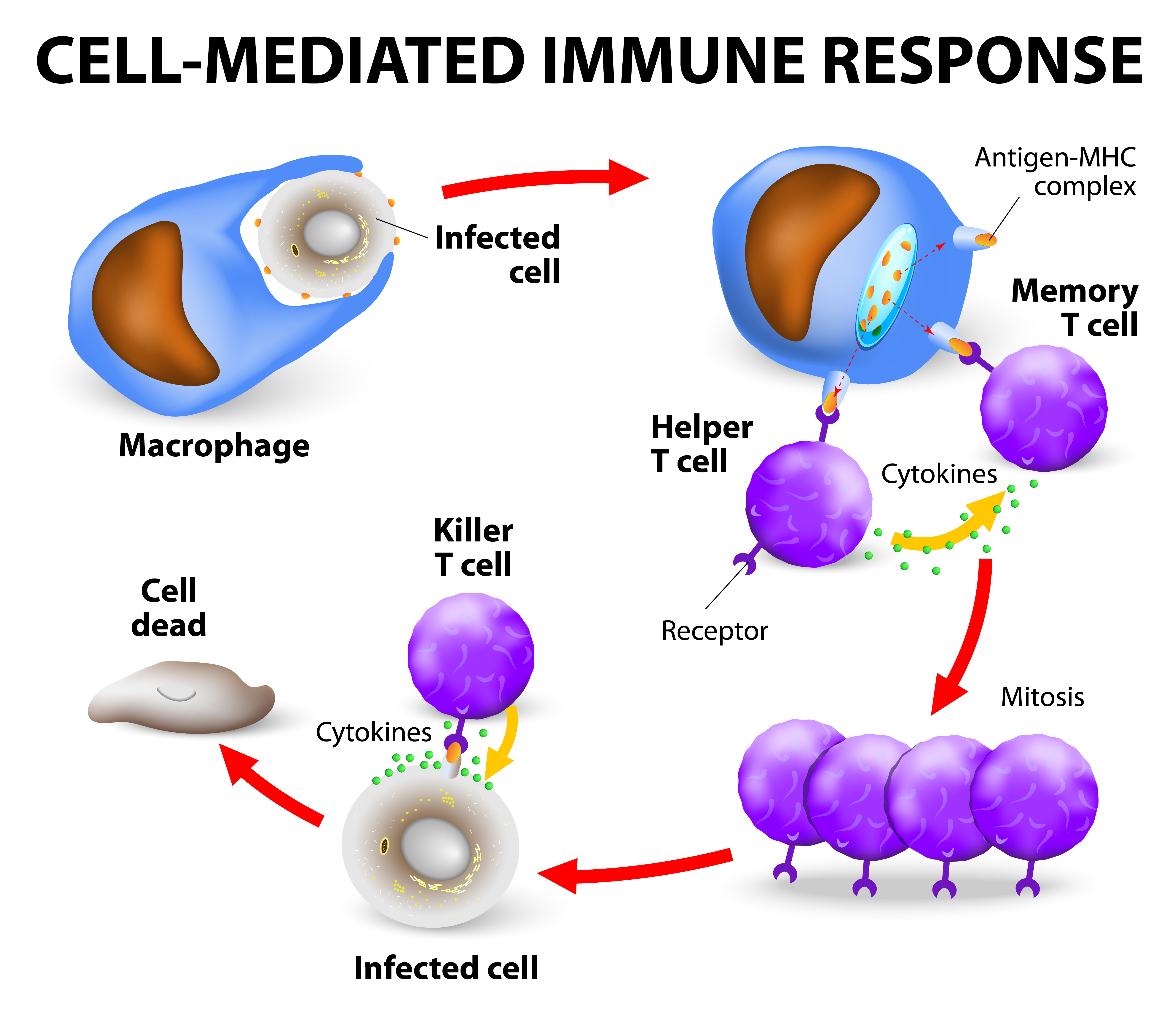
The adaptive immune system is your body’s ability to evolve and adjust based on its circumstances. Whenever you contract a disease, your adaptive immune system “remembers” it, making it much easier to fight off the next time it’s exposed to it. Unlike the innate immune system which reacts to general threats in the body, the adaptive immune system is activated when it’s exposed to pathogens. The adaptive immune system is also a lot slower to react than the innate immune system.
Self vs Non-Self Antigens
In order for the immune system to work effectively, it first needs to be able to differentiate between self and non-self substances, organs, and cells. Self-antigens are ones that originate in the body and should not be attacked while non-self antigens are foreign and can often cause harm to the body if they aren’t neutralized.
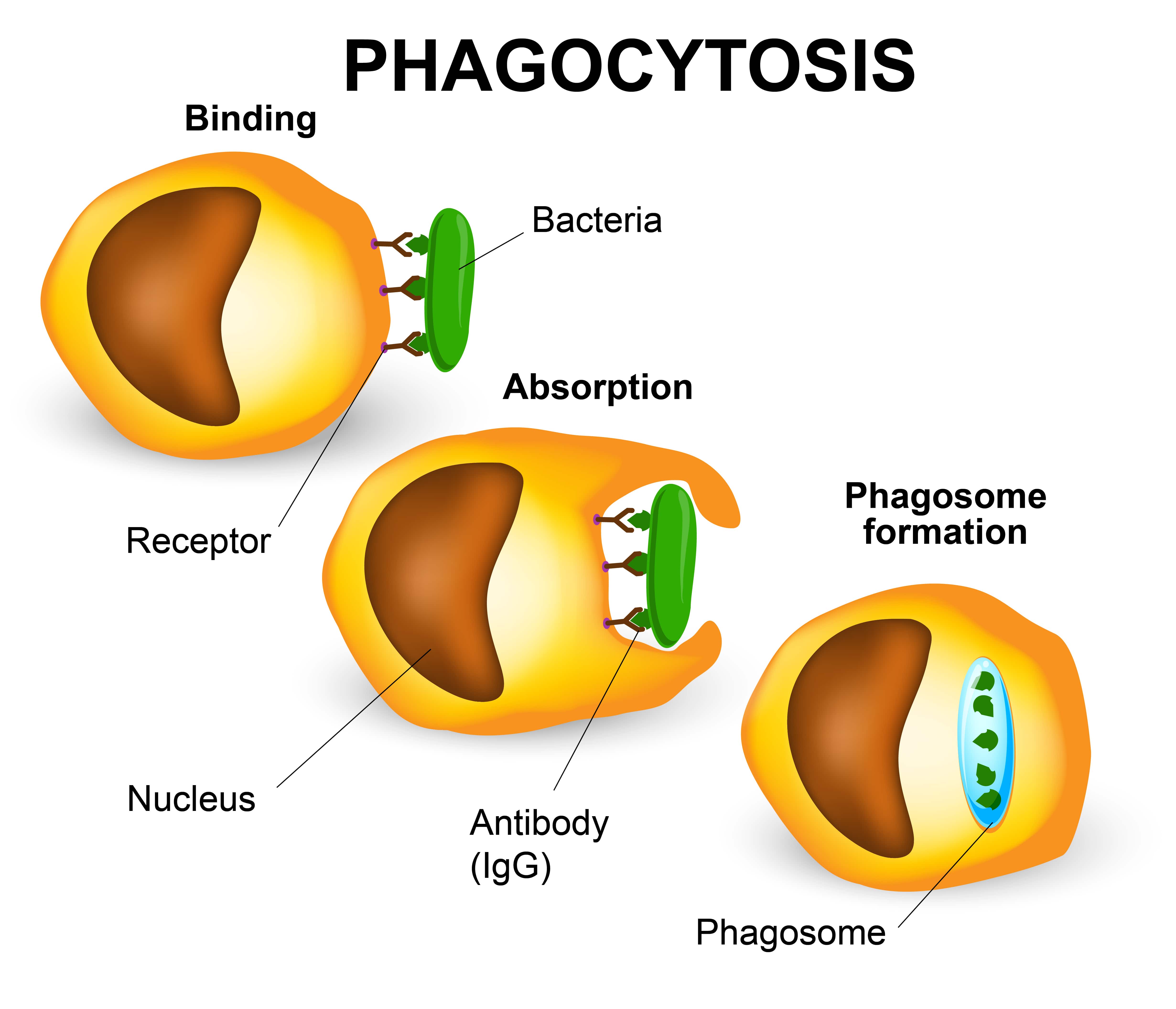
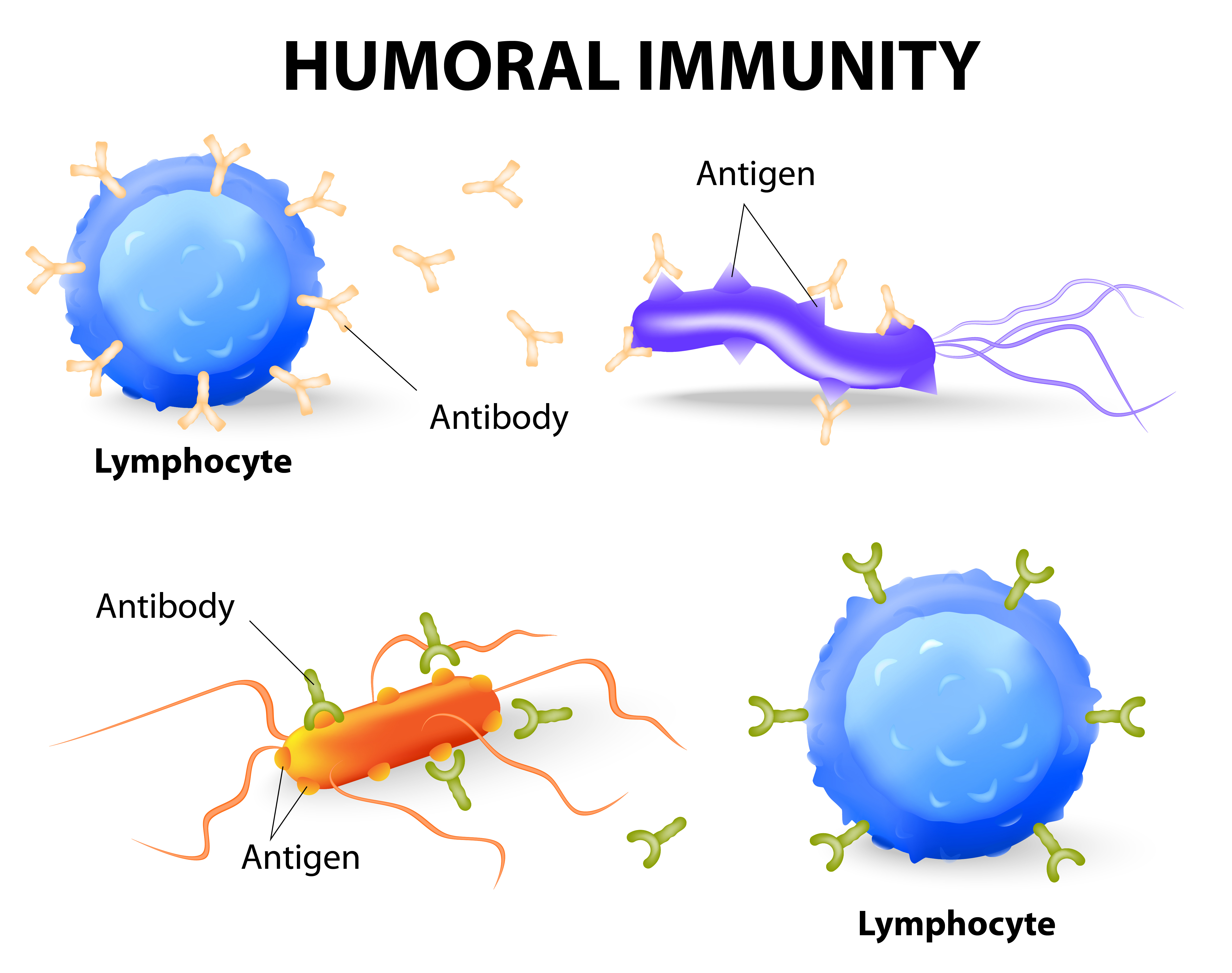
Your immune system is largely coordinated by white blood cells called lymphocytes. When these cells come across a non-self antigen in the blood, they produce something called an antibody that allows them to detect and bind to the antigen. After binding to the antigen, the antibody engulfs and digests it with macrophages through a process called phagocytosis.
If the body has encountered a substance before, it may have stored “memory” cells that remember the microbe, allowing it to create an antibody more quickly. This is why people are less likely to contract a disease if they’ve already had it, because their immune system is better equipped to fight it off before it becomes a problem. However, an antibody that recognizes one antigen will not be able to recognize another.
 Types of White Blood Cells
Types of White Blood Cells
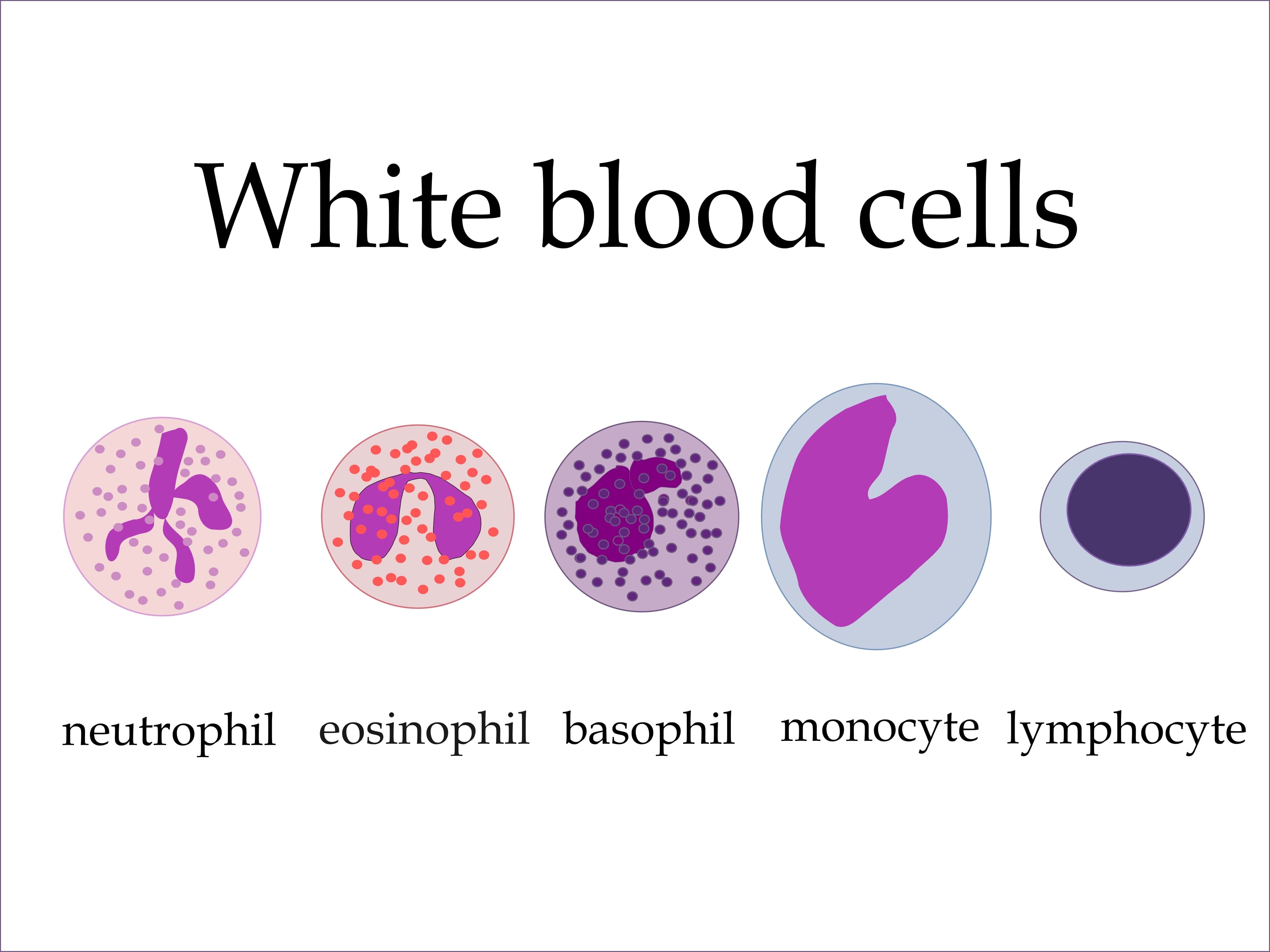
Lymphocytes
There are three different types of lymphocytes: T cells, B cells, and natural killer cells. T cells got their name because they’re produced in the thymus gland, a pinkish-gray organ in between the lungs. T cells are able to recognize foreign bodies and attach to them while ignoring self antigens.
B cells, produced in bone marrow, are another important type of lymphocyte. These cells have a protein on them called the B-cell receptor which generates the antibodies necessary to neutralize an antigen. B cells are part of the adaptive immune system because they develop when they’re introduced to a foreign substance.
NK cells, or natural killer cells, are the third type of lymphocyte. They got the name “natural” killers because they are part of the innate immune system. While T and B cells need to be primed by antigen presenting cells, NK cells have natural immune capabilities. NK cells are known for fighting cells that show early signs of cancer as well as virally infected cells.
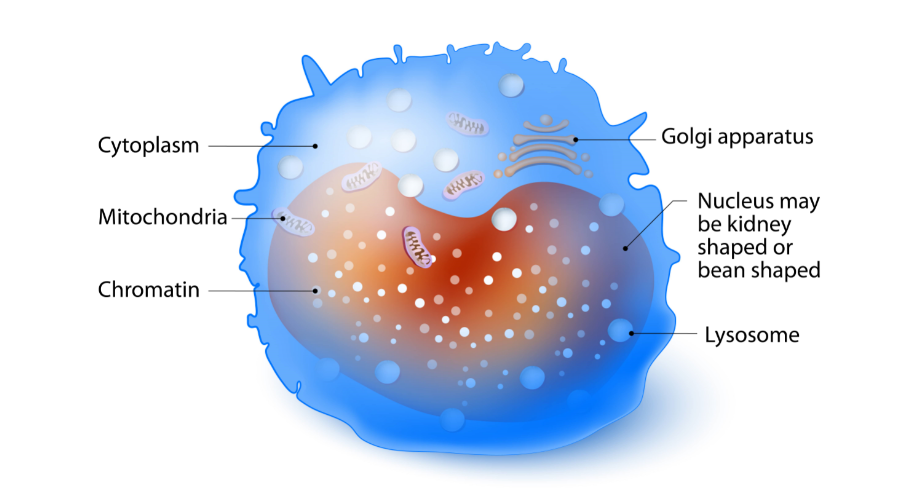
Monocytes
Monocytes are the largest type of white blood cell. They’re produced in bone marrow like many leukocytes and become a macrophage when it travels to different tissues of the body via the bloodstream. These cells ingest foreign material, kill microorganisms, and remove dead cells.
Granulocytes
Basophils
Basophils are a type of white blood cell referred to as granulocytes. A granulocyte white blood cell secretes substances called granules that play an important role in the immune system. When basophils are exposed to an allergen, they release a compound called histamine that causes dilation of capillaries and the contraction of smooth muscles.
Neutrophils
Neutrophils are usually the first white blood cells to arrive at the sight of infection because there are more of them than any other type of immune cell. Neutrophils neutralize bacterial infections through either phagocytosis or endocytosis.
Eosinophils
These are proinflammatory cells that contain two different lobes and a cytoplasm that contains up to 200 granules. These granules contain proteins and enzymes that are needed to destroy foreign substances. While eosinophils play similar roles to other white blood cells, they also have a physiological role in the formation of organs such as the postgestational mammary gland.
Humoral vs. Cellular Immunity
Humoral and cellular immunity are the two main mechanisms within adaptive immunity. Humoral comes from the Latin word “humor” meaning “fluid” or “moisture.” So, humoral immunity refers to immune responses occurring within the body’s fluids, especially the blood. In humoral immunity, the antibody will destroy viruses through either immune cytolysis or phagocytosis.
Unlike humoral immunity, cellular immunity does not use antibodies. Instead, phagocytes, antigen-specific cytotoxic T-lymphocytes, and cytokines are released in response to antigens. When there is a viral infection, cell-mediated immunity can help prevent it from spreading but also results in an inflammatory response which can damage vital tissues surrounding the virus, resulting in chronic disease.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Autoimmune Disease
An autoimmune disease is one that causes the immune system to be overactive and attack the body's tissues rather than pathogens or cancerous cells. Some autoimmune disease you may recognize include rheumatoid arthritis, multiple sclerosis, psoriasis, and vasculitis. There are more than 80 types of autoimmune disease, so it can be difficult to diagnose and differentiate each one.
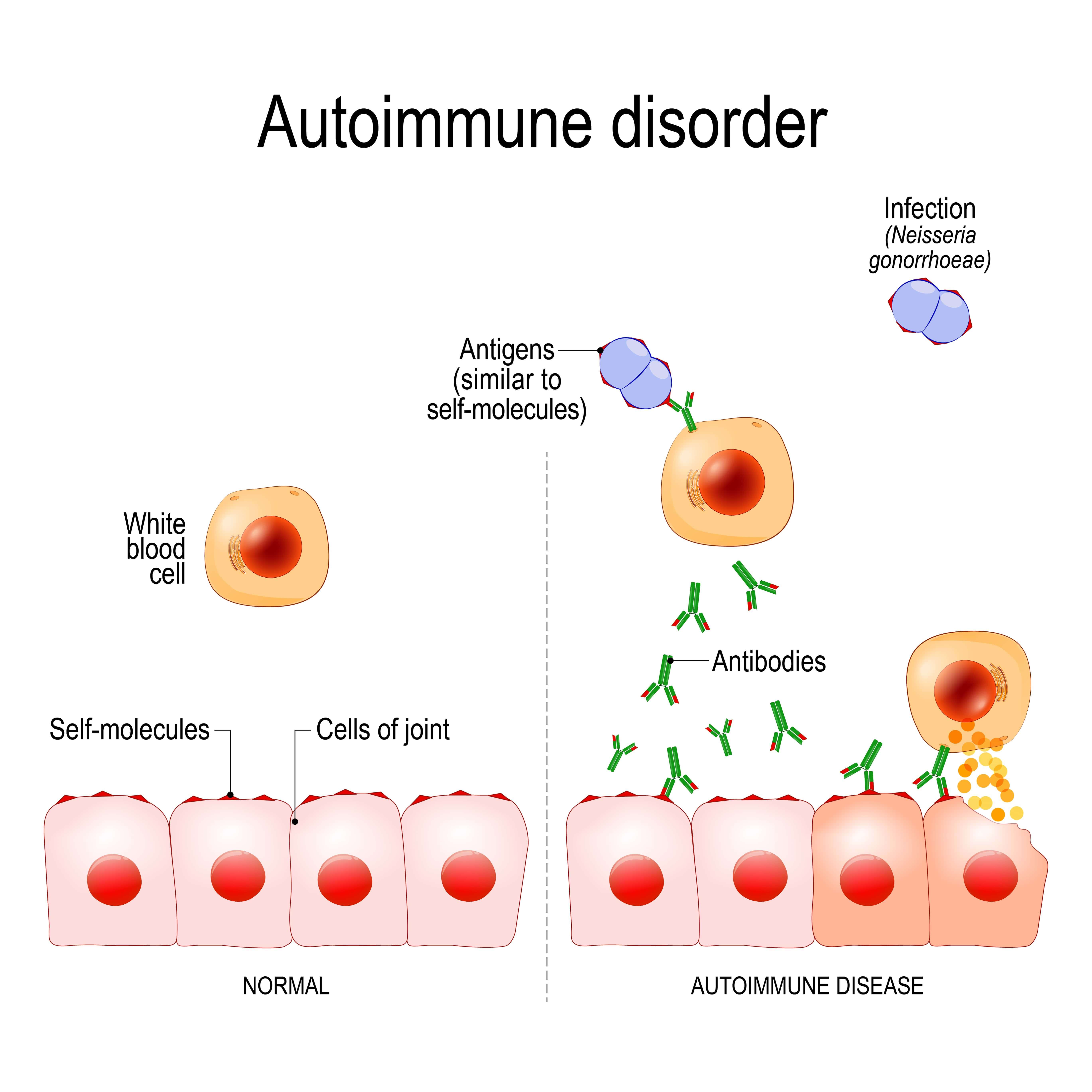
Because autoimmune diseases cause increased immune system activity, they're often characterized by inflammation in the body. When treating these diseases, the goal is usually to reduce inflammation and reduce immune system activity. Your doctor may prescribe corticosteroids or other steroids that can help with this.
COPD and The Immune System
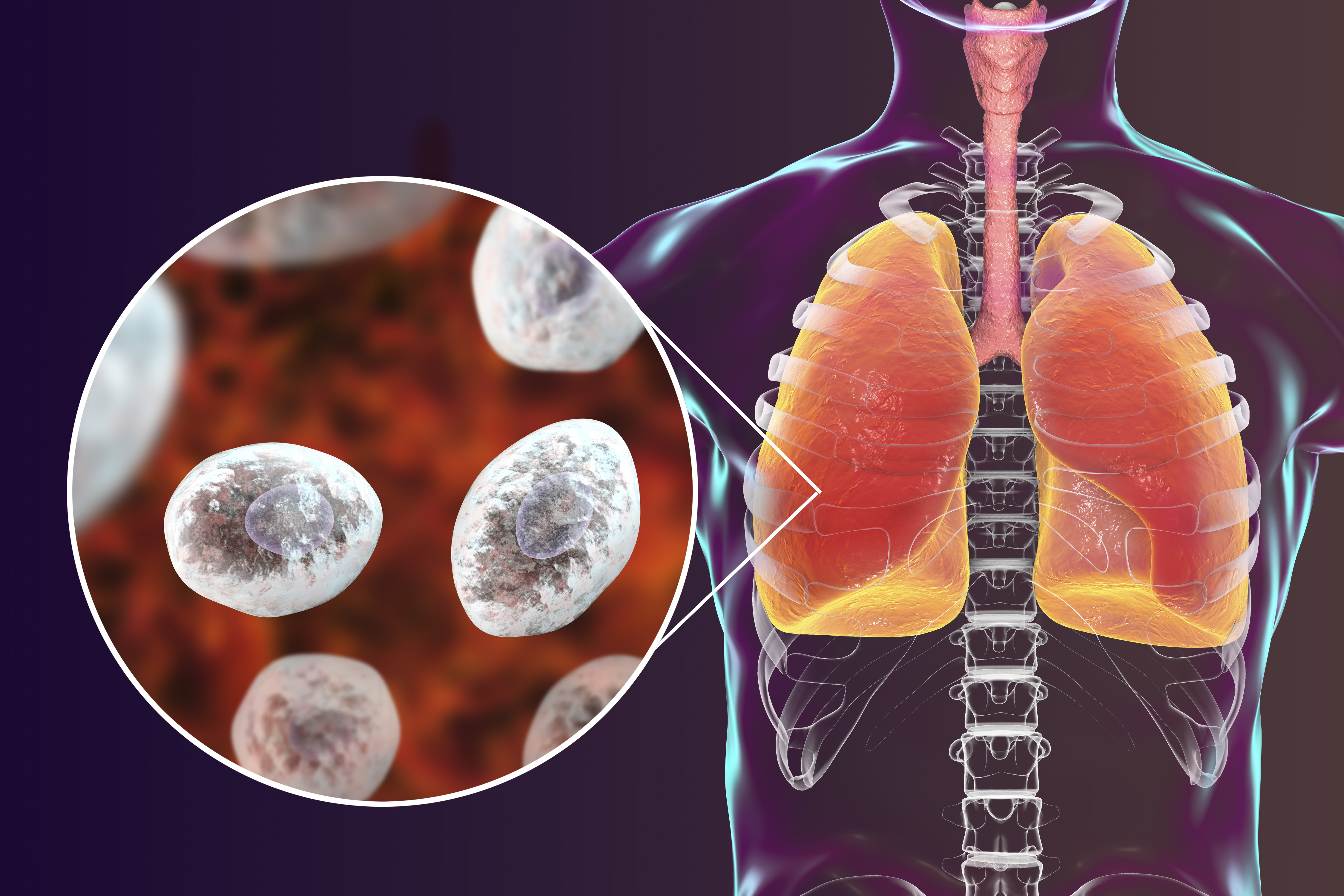
You may recall from earlier that inflammation is one of the key functions of the innate immune system. When cigarette smoke or other airborne irritants enter the lungs, structural and inflammatory cells in the lung begin to release proinflammatory mediators. These mediators create an inflammatory microenvironment that damages the lungs and leaves the immune system in a state of disrepair. Many researchers have found that this lung state leads to more frequent and severe respiratory infection as well as a host of problems throughout the body.
While most medical professionals don’t label COPD as an autoimmune disease, most acknowledge that it has autoimmune components. Think of inflammation as a catalyst for adverse side-effects throughout the body. Because your immune system is preoccupied with chronic inflammation in the lungs, it has fewer resources to use in other areas of the body that may need it.
Immune Dysfunction and COPD are a Two-Way Street
Another important thing to note about COPD and the immune system is that they’re a two-way street. In other words, a compromised immune system will lead to increased COPD symptoms, and COPD symptoms will lead to a compromised immune system. Like we mentioned before, smoking is the primary cause of COPD making up about 90 percent of COPD patients. Continuing to smoke with COPD will not only increase inflammation in the lungs, it will also weaken both your innate and adaptive immune system.
On the other hand, you should remember that only a small percentage of people who smoke actually develop emphysema or chronic bronchitis. This means that there are other factors at play in determining whether a smoker or someone exposed to lung irritants develops COPD. Researchers have found that both genetic makeup and the immune system play a role in determining whether someone develops the disease.
Mucus Hypersecretion
Mucus is a substance created by mucosal glands lining the nasal passages. Its function is to lubricate, moisten, and filter debris that enters the airway, preventing it from reaching the lungs. But mucus isn’t the only substance secreted in the upper body. There are also fluids created by cell membranes in the nose and sinuses. When you get sick or your immune system is compromised by something like smoking or seasonal allergies, these substances are thrown off balance. This means you may experience thicker mucus in the airways making it much more difficult to breathe.
Damaged Cilia
Unfortunately, many of the same things that cause COPD simultaneously damage your immune system. Cilia, tiny hair-like protrusions in the airways are one of the innate immune functions of the body that’s affected by cigarette smoking and air pollution. Much like mucus, cilia are part of a large ecosystem in your body that’s designed to prevent infection. While people who have never smoked or been exposed to a significant amount of pollution may have healthy cilia, most people who have COPD already have damaged cilia.
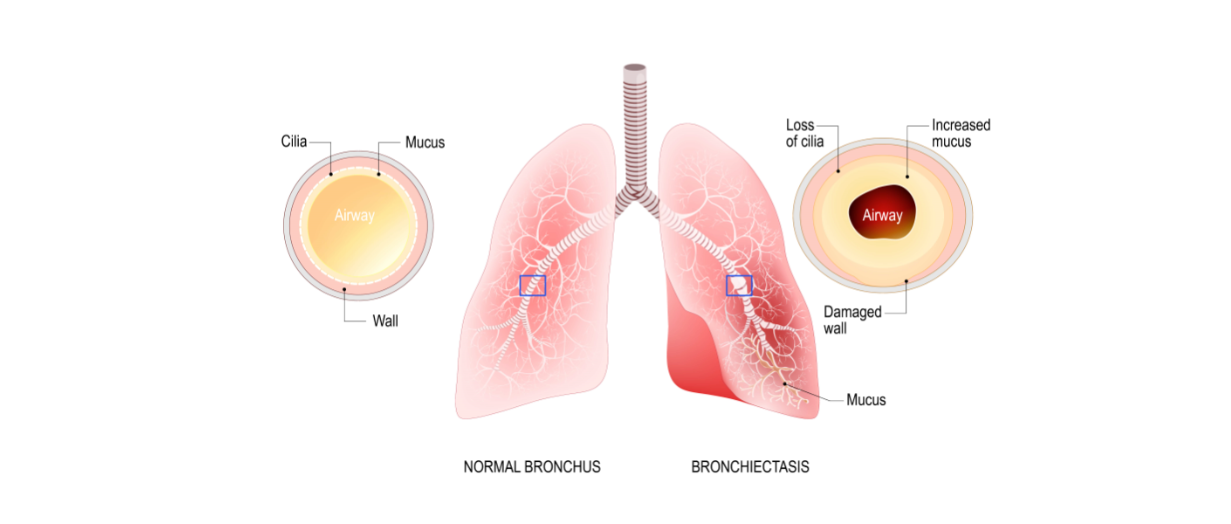
Another function of the cilia is to remove mucus and other substances from the airways. So, when the airways are inflamed due to bronchitis or the cilia are damaged and aren’t able to flow freely, congestion symptoms are likely going to stick around longer in someone with COPD and they may be more severe. This is one of the things that trigger a seemingly never ending cycle of sickness in people with chronic bronchitis and emphysema.
Overactive Immune System
If you’ve ever heard the term “progressive disease,” you may have wondered exactly what that means. What this means is that the disease can’t be cured or reversed. While COPD is a progressive disease, it is still very treatable, meaning symptoms can be reduced and you are able to slow the progression of inflammation in the lungs.
Normally, you think of the immune system as something that protects your body from infection and harm. However, when you have COPD, your immune system is overactive. Something that may cause temporary airway inflammation in a healthy person may cause permanent and irreversible damage to a COPD patient’s lungs because the slightest irritant may result in prolonged inflammation.
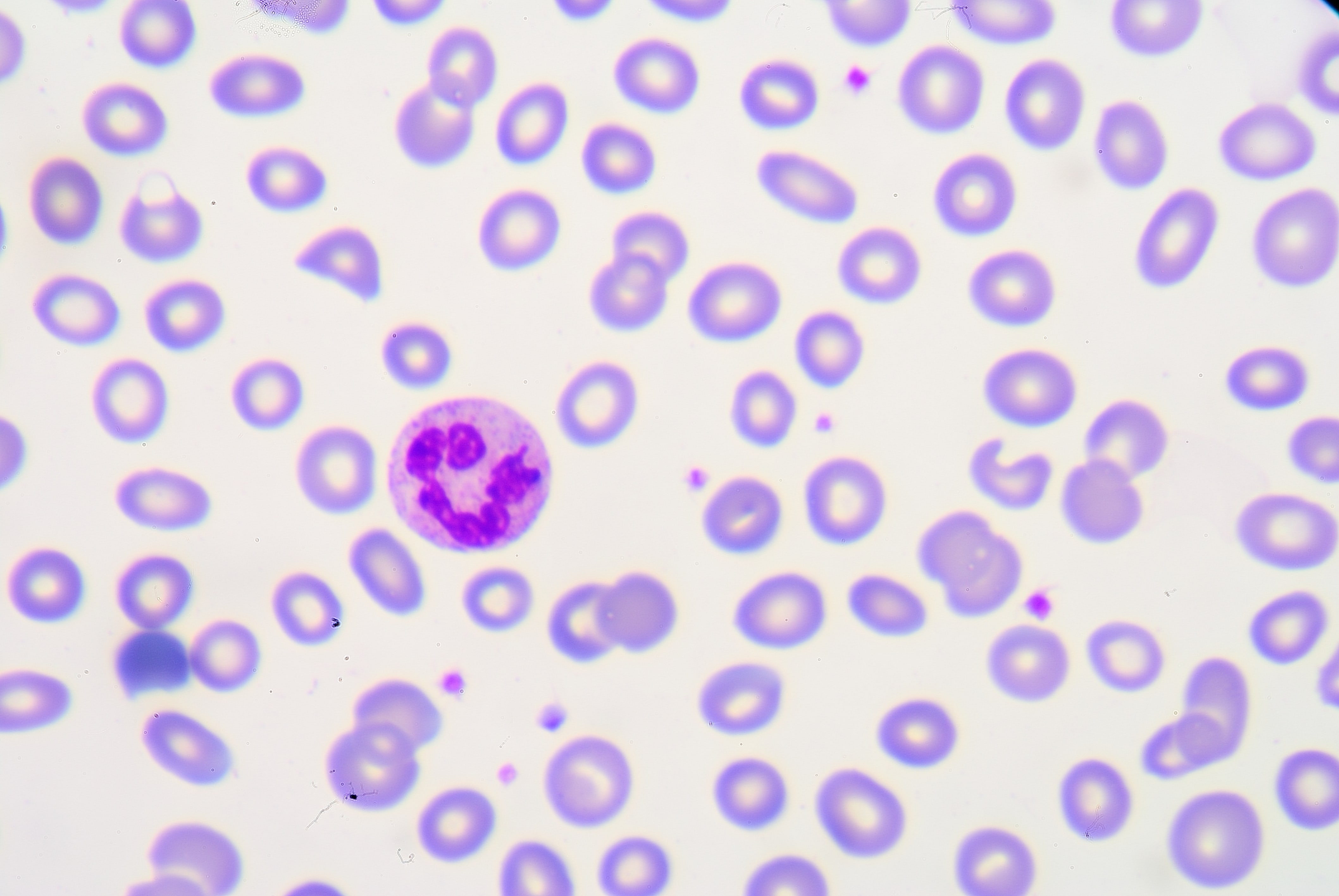
High White Blood Cell Count
While a high white blood cell count in and of itself is not harmful, it is a sign of inflammation, chronic disease, and other symptoms. Since white blood cells are what combat infections, cancerous cells, and viruses in the body, a high WBC count is an indication that your body perceives a threat and is trying to eliminate it.
A study published in the National Center for Biotechnical Information looked at WBC counts between 1,227 COPD patients and 8,679 non-COPD adults over the age of 40. It concluded that high WBC counts were negatively associated with forced vital capacity (FVC) and forced expired volume in one second (FEV1), both of which are crucial for quality of life in COPD patients.
When an inflammatory response is triggered, phagocytes are what accelerate the amount of inflammation needed to treat the infection. They recruit alveolar macrophages that combat and control the inflammation. While alveolar macrophages are increased in patients with COPD, their ability to fight infection is impaired. This, along with a high survival rate of neutrophils leads to a high neutrophil load in the airway and a higher white blood cell count.
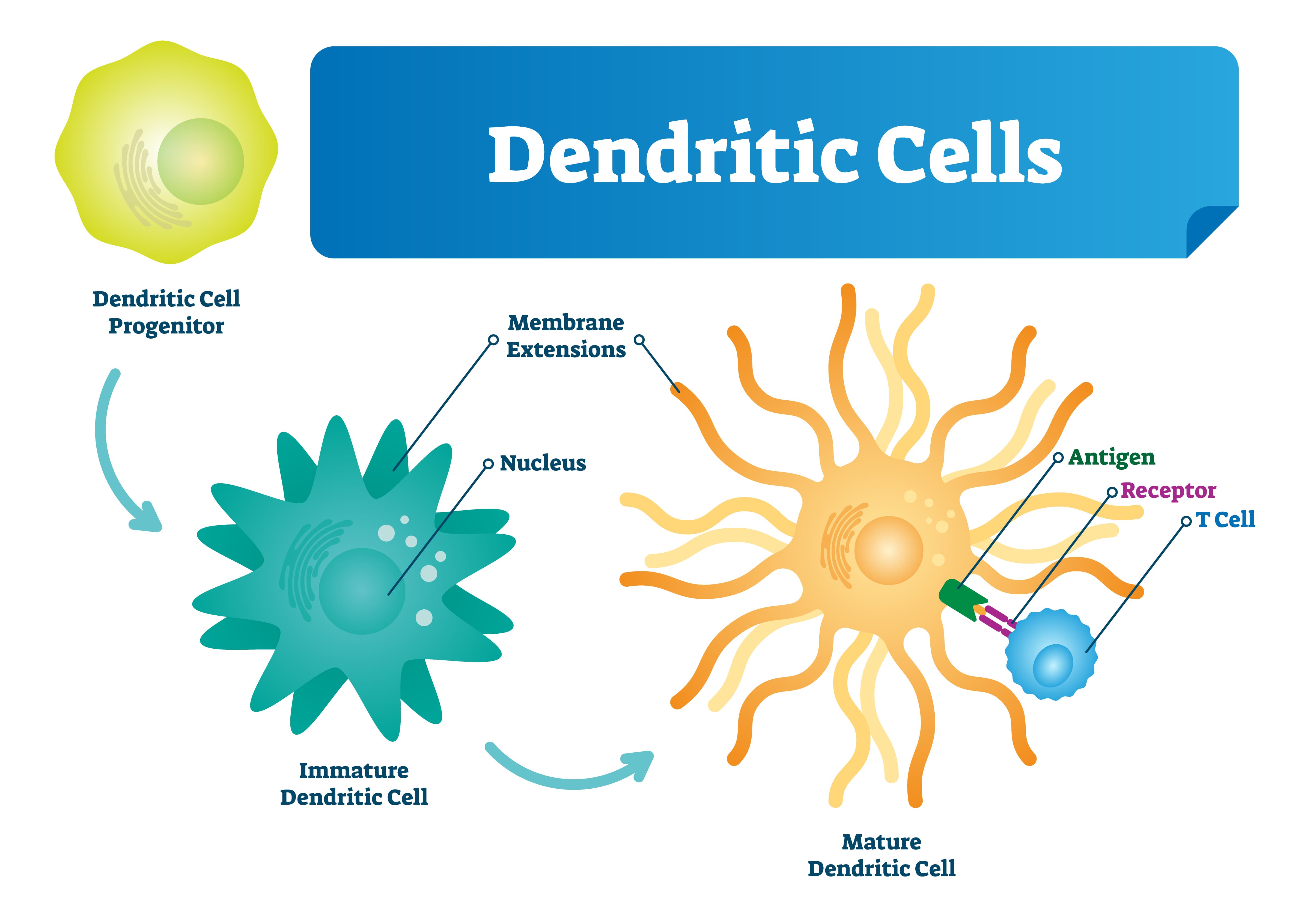
Reduced Number of Dendritic Cells
Dendritic cells are responsible for processing antigens and presenting it to the T cells. They are also the primary line of communication between the adaptive and innate immune system. While researchers have yet to determine exactly how dendritic cells are affected by COPD, some studies have shown that nicotine exposure can reduce the number of dendritic cells in the body while reducing their functionality, thus compromising both the innate and adaptive immune systems and their ability to work together effectively.
The Immune System and Acute Exacerbations
An acute exacerbation of COPD is a sudden worsening of respiratory symptoms and can last as short as two days or as long as a week. Acute exacerbations are more common in later stages of the disease and exhibit signs such as increased sputum (a mixture of saliva and mucus), breathlessness, coughing, wheezing, and more. Acute exacerbations are typically triggered by environmental factors such as air pollution, dirt, dust, or pollen, and infectious disease
Studies have shown that the majority of exacerbations are caused by respiratory illness like the human rhinovirus, influenza, and respiratory syncytial virus. More specifically, around half of the infective exacerbations caused by bacteria are the result of Haemophilus influenzae (NTHi) which, despite its name, is not the same thing as influenza (the flu). Due to a changing lung microbiome, impaired airway system, and unusual inflammatory response, this provides an ideal environment for it to survive in the lower respiratory area.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
How To Avoid Getting Sick
Now that you know a little bit about how the immune system works and how COPD impairs your immune system, you need to know what you can do about it. No matter what stage of COPD you are in, your age, or your overall health, you should adhere to a strict routine that will keep you from getting sick and keep you breathing freely and effortlessly. While you should be doing everything you can to prevent respiratory infection, you’ll need to know how to react if you do get sick.
Quit Smoking
Smoking cessation should always be your first step in getting healthy and preventing respiratory infection. Cigarettes are what’s called an “immunosuppressive drug.” What this means is that when you smoke cigarettes, your immune system is weakened, and your body will be less prepared to fight off harmful viruses and bacteria.
 According to a study published in the Oncotarget Open Access Journal, cigarette smoke damages adaptive immune cells like regulatory T cells, B cells, and memory T/B lymphocytes while damaging innate immune cells such as natural killer cells, macrophages, and dendritic cells. What’s more, smoking increases mucus production and makes it more difficult to clear meaning harmful pathogens are more likely to build up in the lungs.
According to a study published in the Oncotarget Open Access Journal, cigarette smoke damages adaptive immune cells like regulatory T cells, B cells, and memory T/B lymphocytes while damaging innate immune cells such as natural killer cells, macrophages, and dendritic cells. What’s more, smoking increases mucus production and makes it more difficult to clear meaning harmful pathogens are more likely to build up in the lungs.
Get Plenty of Sleep
A great night’s sleep every night helps ensure your immune system is working its best. According to the National Sleep Foundation, sleep deprivation mainly affects one protein in the body: cytokines. This protein targets and prevents infection and inflammation in the body and they’re mainly produced and released while you’re sleeping.
If that’s not enough, when you slack on sleep, you’ll be more sleepy and less prepared to handle any symptoms of breathlessness or fatigue related to COPD. Getting enough sleep will give you the energy you need to follow your treatment plan to a T without making any mistakes.
Stay Hydrated
There’s no understating the importance of hydration for COPD patients. Although everyone, regardless of whether they’re healthy or sick should be getting enough water, it’s especially important for anyone with a respiratory condition. Every cell in the body needs water in order to function, including all of the immune cells that we discussed above. The human body is made of more than
Long term oxygen therapy (LTOT) is a common treatment administered to respiratory patients in the comfort of their home, and depending on their prescription sometimes 24 hours a day. Lung diseases like COPD are chronic, and so LTOT can be life changing and life saving for people who have these low blood oxygen levels, which is also known as hypoxemia.
Oxygen therapy in itself is a simple concept, however there is confusion about where and how a person should buy their oxygen device. Anyone who is administering their own treatments or medication should be aware of every detail when it comes to health and safety, but they should also be informed about their purchasing options. Purchasing an oxygen device can feel as if you are in a maze, at each turn you find a barricade forcing you to start at the beginning again, and the cycle repeats itself. This article guides you through this maze so you know what to look out for, how to make the right choice, and more!
This article will take you through all of the ins and outs of what you should look for when purchasing your oxygen therapy device. This is your all intensive guide into the buying process of a breathing device, what you should look for, and how to make the best choice for you.
What is long-term oxygen therapy

If you have ever experienced a respiratory emergency where you went to the hospital and they put tubes in your nose to help you breath, that is oxygen therapy. This is a necessary treatment if you have ever had trouble breathing on your own and it can be used to save your life.
The difference between this emergency treatment and long-term oxygen therapy is that LTOT is administered while you are at home while going about your daily life, According to International Journal of Chronic Obstructive Pulmonary Disease LTOT should be prescribed for at least 18 hours per day, although some experts suggest that 24 hours would be more beneficial.
Long term oxygen therapy, if done correctly, is proven to improve survival and other qualities of life for COPD patients with chronic respiratory failure.
LTOT doesn’t just help you live a longer life, it helps you to live more active and worthwhile life by:
- Reducing the number of hospitalizations
- Increasing your lung capacity
- Increasing your ability to exercise
- Helping you to get better sleep
- Improving your moods
- Improving your health-related quality of life
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
LTOT would normally be administered in the comfort of your home, by you, therefore the delivery method should meet your oxygen requirements but also be accustomed to your lifestyle.
Most people are prescribed oxygen anywhere from 16-24 hours a day so, this means you should choose a device that fits into your daily routine. You have a few choices when it comes to an oxygen system. These include devices you use only at home and lightweight alternatives you can take with you when you go out.
You’ll choose a oxygen device based on:
- How often you leave the house or travel
- If you need to go up and down stairs
- Your size, endurance, and physical strength
- How much oxygen flow your doctor prescribes
Oxygen devices

Three of the most popular portable devices you can choose from, each have their own pros and cons, and you should pick the best options for you:
- Compressed liquid oxygen tanks
- Oxygen gas tanks
- Portable oxygen concentrators (POC)
This article should give you some insight into what option is best for you.
If you already know that you are interested in buying a portable oxygen concentrator, and you are curious about which brand and model you should get, please read our other blog about the pros and cons of the best portable oxygen concentrators in 2020 by clicking the link here.
Affordability
The upfront costs of portable oxygen concentrators tend to scare off oxygen patients all of the time. This is unfortunate because the prices that are posted online are, for the most part, not the price you would pay for your POC. Due to the manufacturer's advertising policies, oxygen equipment licensed distributors are required to post their prices. Even if the seller has a special, discount codes, or a sale.
So even when you simply search on google “portable oxygen concentrators prices” you will see them ranging from $2,000 to $3,000 depending on the brand, year, and model. To inquire about the real prices, you can call 1-800-946-1021 and speak with a respiratory specialist who knows these devices inside and out.
The other affordable aspect of portable oxygen concentrators is that you never have to refill the device, because it is extracting the air surrounding it, compressing and purifying it into the medical-grade oxygen that you are breathing int. At LPT medical we offer a 3 year long warranty on all our portable oxygen concentrators, so you won’t have to pay for a broken part or a malfunction!
Oxygen devices like the Respironics SimplyGo Portable Oxygen Concentrator have a compressor that is rated to last 20,000 hours. Others like the SeQual Eclipse 5 Portable Oxygen Concentrator were designed for the US Military, and it has the longest-standing track record for being durable and reliable.

All in all, a portable oxygen concentrator is going to last you a very long time, and there are no recurring costs, all you pay for is the device upfront. Also by purchasing a portable oxygen concentrator through LPT Medical you have the option to finance and pay monthly, or buy a used and refurbished device that is less expensive upfront.
For more information about your purchasing options and prices, please read this other blog that we have linked here, or call us at 1-800-946-1201
Portable oxygen canisters must be refilled multiple times per week, each time costing you money. The bigger tanks that you leave in your home to use are even more expensive to refill. While oxygen tanks are the most traditional form of oxygen, it is also the most outdated. Even with the low-initial costs, the recurring costs eventually add up, leading to higher costs over time.
Portability

Unlike portable oxygen concentrators, oxygen tanks are heavy and bulky. Their weight and lack or portability are one of the most commonly noted disadvantages of tanks. While wheel-mounted cart systems can help to make rolling oxygen tanks manageable, the tanks themselves are still rather heavy. Lifting the tank—for example, to put it in a vehicle or carry it up a staircase—can be challenging or even impossible for some simply due to the weight of the device.
Depending on the oxygen flow you need to fill your oxygen prescription, portable oxygen concentrators are very light weight, and small in size. Units like the Inogen One G5, Inogen One G3, and the Caire Freestyle Comfort, all range in weight from 4 pounds to 6. All are small enough to fit inside a purse or backpack, and come with their own carrying case. Having such a lightweight and portable breathing device is great for oxygen patients who want to be more active and do more things, and not to mention travel by plane.
.png)
Having a portable breathing device is essential for keeping up with a consistent exercise regime that is a necessary treatment for all COPD patients. You should be getting the right amount of exercise relative to your health and ability. Having a portable device can make it easier to go for walks, golf, or do any other activities you like to do as your daily physical activity.
Having a breathing device that is designed to be potable is also great for keeping your morale high. It is no secret that having a chronic illness like COPD can be hard for patients mentally. If you have COPD and a portable oxygen concentrator you have the freedom and independence you need to live a normal life without having to adjust your daily routine to fit your oxygen device. Instead your oxygen device fits into your lifestyle.
Battery life vs. tanks

Portable oxygen concentrators generate oxygen using a rechargeable battery, depending on the unit, you can have anywhere from 3-16 hours with oxygen until you must either switch the battery to your backup, or recharge the device. You can recharge any device using an AC or DC power source, meaning you can use a traditional outlet in your home, or the cigarette lighter in your car or boat.
An oxygen tank on the other hand does not need a power source. The tanks or canisters are filled with a finite amount of oxygen that you use up until it is empty and have to get it refilled or replaced. Normally, you pay an oxygen supply company to come to your home and deliver new tanks and take your old ones. The tanks that are heavy and are hard to move around don’t run low as often, probably once a month depending on your oxygen prescription, and the smaller travel canisters run out at least once a week.
Having a battery powered oxygen device versus refilling your oxygen tanks is a personal preference, most people find that charging their portable oxygen concentrators is as simple as charging your cell phone, and having an extra battery to replace one while it charges is the most efficient option.
Insurance
Obviously in a perfect world, insurance would cover all respiratory patients' oxygen devices but this is not the case. There are some very rare situations where Medicare or insurance will cover the purchase or rental of one of our portable oxygen concentrators. In order to qualify, you have to meet strict criteria, and each situation is evaluated on a case-by-case basis.
That being said, You will need to talk to your insurance provider to understand what kinds of oxygen supplies they cover and what requirements you need to meet in order to qualify.
Medical insurance companies have a notorious reputation of denying patients coverage for medical equipment and treatments including portable oxygen concentrators. Unfortunately, Medicare is no exception. They have strict rules that make getting coverage difficult and burdensome, and they often find reasons to deny approval for a treatment even when a doctor says that it's the best option.
If you want the best possible chance of getting insurance or Medicare to pay for your medical equipment, you need to be aware of your provider's criteria on the subject. You must follow their guidelines carefully, to avoid getting rejected on a technicality.
We have a very informative blog about medicare and oxygen equipment that you can find here
In this blog ,we offer a lot of insight into the healthcare system and what it means for oxygen patients like yourself.
One example of Medicare's criteria for covering supplemental oxygen and related equipment:
- You have a serious lung disease (such as COPD, cystic fibrosis, bronchiectasis, etc.), or you have symptoms of low blood oxygen levels (such as pulmonary hypertension, erythrocythemia, congestive heart failure, etc.)
- Your health is likely to improve with supplemental oxygen therapy
- You have medical tests from your doctor to prove that you have low blood oxygen levels (and these tests were taken while your condition was stable, e.g. not during an exacerbation)
- You have tried other medications and treatments, but are still unable to get enough oxygen
- You need oxygen therapy 24/7 (Medicare will not cover supplemental oxygen therapy if you only need to use it at night)
This criteria has to be verified by your doctor in writing before you can receive Medicare benefits for supplemental oxygen. Your doctor will also have to write and submit a detailed report of your oxygen needs, called a Certificate of Medical Necessity.
Which method of oxygen equipment should you choose
.jpg)
While all of this information pertains to the oxygen user, it is important to note, that if you do not need oxygen therapy, meaning your blood oxygen levels are not chronically low enough that your doctor would recommend, let alone, prescribe you oxygen therapy, you should NOT administer oxygen therapy for yourself.
Who needs oxygen therapy
Even though long-term oxygen therapy can be beneficial for many people, not all respiratory patients need it. W
hen considering a lung disease like COPD, According to the American Thoracic Society, appropriate candidates for LTOT include:
- Patients who have an established medical regimen, with a 7.3 KPa (55 mmHg) partial pressure of oxygen measure by looking at arterial blood gases, and an oxygen saturation level of 88% or less.
- Patients who have a partial pressure of oxygen of 7.3–7.8kPa (55-59 mmHg), an oxygen saturation level of 89%, and also shows signs of hypoxemia, pulmonary hypertension, edema from right-sided heart failure, high red blood cell count or impaired mental status.
If you are unable to maintain healthy blood oxygen levels only while you sleep or when you exercise, you may also benefit from using supplemental oxygen specifically under these circumstances.
Moreover, because there are special cases, if you do not fall under these criteria but have severe shortness of breath or limited exercise capacity that may improves with supplemental oxygen you should still talk to your doctors about whether you would qualify for, and more importantly benefit from, long-term oxygen therapy.
Buying from a licensed distributor
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
In order to be sure that you are getting an oxygen device, for example, a portable oxygen concentrator, from a licensed distributor, you can simply look on the company’s website and find their certification. At LPT Medical, you will be happy to know that we are a family owned and operated business .
LPT Medical knows what it means to serve the community and treat our customers like family and we are committed to quality and dependability. Our track record shows that we have become one of the most trusted names in the world of oxygen therapy products offering home oxygen concentrators, portable oxygen concentrators, CPAP and BiPAP machines, and all the education you need to make the most of your equipment and subsequently your life.
When you are buying oxygen equipment, something that is so life changing and a reasonably large financial decision, you must be sure that you are buying from a company that you trust. Quality is one of the first words that should come into your head when buying any medical device. If the equipment is designed to make your life easier, it is always important to take into consideration how long your equipment will last and how efficient the machine is.
LPT Medical offers products from the most reputable manufacturers in the industry including but not limited to Inogen, Philips Respironics, Drive Medical, and more. These are innovative companies that are exceeding the limits of what’s possible for patients suffering with a debilitating respiratory condition. By offering these brands, we are here to connect more people around the country with the most state-of-the-art oxygen therapy equipment in the world.

Flow settings
Depending on your oxygen needs, your doctor will either prescribe you pulse flow or continuous flow oxygen or a combination of both and you will be required to buy a device within those boundaries. It is important you do not take more oxygen and it is important that you do not try to go without it, both could do a lot of harm. If you are unsure about your oxygen prescription you should call your doctor and have them go over the process with you until you feel comfortable doing so on your own, and also during an emergency situation.
So the flow settings can be pulse or continuous, pulse gives off a bolus of oxygen every time you inhale and continuous flow settings exert oxygen constantly even when you are not inhaling.
The rate at which oxygen is flowing is known as the oxygen output, and it is most commonly measured in liters per minute. If you require more oxygen your oxygen output will be set to a higher setting and vise versa.

If you only need roughly 210- 630 mil/min of oxygen at a pulse dosage setting, you oxygen device must be able to emit that much oxygen per minute, and if you buy from a qualified company, the seller would advise for you to get a device that is capable of outputting even more oxygen than what is prescribed to you for a number of reasons.
You might be instructed by your doctor to increase your oxygen flow setting in the case of an emergency while you are experiencing an exacerbation or a flare up. In this situation you want to have a device that can increase its oxygen output so that you are able to manage the emergency how your doctor instructs you.
Also, the nature of a chronic progressive respiratory illness is that it gets worse over time. This means, that one day you might need a higher flow of oxygen than what was first prescribed to you in order to meet the demands of your body. In these cases, you want a device that will be able to adjust to your needs and increase its output before you have to buy an entirely new device that is powerful enough.

If you need both pulse and continuous flow oxygen, you can use an oxygen tank because there is a valve you can adjust to have the option to do both. If you still want a more portable option, the Respironics SimplyGo is one of the best portable oxygen concentrators that offers a powerful pulse dose setting, but also gives the user a continuous flow option for when they need to adjust to their prescription.
The most popular pulse dose units are the Caire Freestyle Comfort, the Inogen One G5, and the Inogen One G3, because all of these units are under 6 pounds, and they can produce oxygen 1050 -1260 mil/min, and have a long lasting battery life that can also be replaced with an extra so you never have to go without oxygen.
There are a lot of factors besides your oxygen prescription that go into choosing your oxygen device, but understanding your flow rate and your oxygen prescription is something your respiratory specialist will go over with you first before they ask you any other questions. Your oxygen requirement will weed through and narrow down your search, so be sure you have this information before you call us so we can assist you effectively and efficiently!
Overview

Oxygen therapy is a huge step in your life and it means that your disease has progressed to the point of severity where you can no longer survive without supplemental oxygen. Therefore, it is so crucial for you to take the necessary steps to find that best portable oxygen device that will allow you to continue doing the things you love, comfortably.
Oxygen therapy is not a bed rest sentence, you should still be able to enjoy everyday activities, and once you have adjusted to LTOT you will find that you are more capable of doing more things, even more than before you needed supplemental oxygen.
Every part of your body needs oxygen, every single organ and every single cell. If your lungs are unable to function properly and provide for your body, it will start to deteriorate. You will feel irritated, moody, tired, nauseous, and much more. Oxygen therapy assists your lungs in producing oxygen for your body so you feel better and live longer.
Both oxygen tanks and portable oxygen concentrators will help you get the oxygen you need, but one method will be better for you than the other depending on your lifestyle. For example, if you are an active person, you need a portable oxygen concentrator so that you can bring your oxygen with you wherever you go with ease.

If you need to save money, you can talk to a respiratory specialist about how to purchase a refurbished unit for less, or how you can set up a financial plan to help you pay for your oxygen device over time rather than up font.
You also have to take into consideration how durable your breathing device is, and how long it is rated to last. The longer you can have one machine the more money you can save by not having to get a new one every few years, whether yours breaks or you need to increase your oxygen intake.
There are still some things you need to know about oxygen therapy like, the functionality and tips to get the most out of your oxygen device, so be sure to follow our blog posts as we come out with more information like this is the near future!
For now we hope that this guide has given you some insight into buying your oxygen device whether it is a portable oxygen concentrator or another alternative. If you have any further question please comment on this blog post, or email us at info@lptmedical.com.

Supplemental oxygen therapy is an amazing, enabling, and life-saving tool that many people with COPD use every day. However, while it can significantly improve how you feel and help you live a better quality of life, supplemental oxygen often comes with its own uncomfortable side-effects and inconveniences.
For example, most patients at some point have problems with ear pain from the ear loops of their nasal cannula. Many patients also struggle to manage their oxygen therapy when they're out of the house, struggling to tote around their equipment and worrying about running out of oxygen before they get home.
Some other common problems that oxygen patients have include dryness and inflammation, which often happens when the constant stream of air through your oxygen delivery device dries out your throat and nasal passages. Another uncomfortable side-effect is skin irritation, which is common on areas of the the face where equipment and tubing touches the skin.
For many reasons, oxygen therapy can be a difficult thing to integrate into your everyday life, especially in the beginning. However, once you work out all the kinks and learn all the little tips and tricks that other oxygen patients have figured out along the way, you'll realize that there are plenty of ways to improve your oxygen therapy experience.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
In this article, we're going to help you solve these common problems by showing you how to make your oxygen therapy more comfortable in every way possible. We'll show you how to reduce the overall hassle of using supplemental oxygen and get rid of ailments like ear pain, nasal dryness, and skin irritation that many oxygen patients struggle with every day.
Although you can use ear protectors for oxygen tubing or ear pads for oxygen tubing, there is a lot more you can do to make your oxygen therapy experience more comfortable. We'll discuss a variety of simple, practical solutions ranging from recommendations for over-the-counter moisturizing products to tips for keeping your extension tubing out of the way. We'll also show you how to reduce the hassle of lugging portable oxygen tanks around with you everywhere you go, and how to make using oxygen outside your home more convenient and comfortable than ever.
Tips and Tricks to Make Your Nasal Cannula or Oxygen Mask More Comfortable
One of the most common sources of discomfort for people who use supplemental oxygen are oxygen masks and nasal cannulae. You have to wear both of these oxygen delivery devices on your face, which can sometimes be uncomfortable and get in the way of daily living.
Here are some of the most common problems that oxygen patients have with nasal cannulae and oxygen masks:
- Nasal dryness and nosebleeds
- Ear pressure and pain
- Skin irritation
- Soreness
- Tubing getting snagged, twisted, and pulled
- Excess moisture and condensation
Chances are, if you are on oxygen, you've experienced at least a few of these issues on occasion. If you use oxygen continuously, you might struggle with these problems a lot, which can take a significant toll on how you feel and how you live.
However, with the right equipment and accessories, and a bit of creative problem solving, you can significantly reduce or eliminate the frustration and discomfort of using oxygen with a nasal cannula or oxygen mask. In the next sections, we're going to address each of these ailments and show you a variety of tricks and simple solutions you can use today to make your oxygen therapy more comfortable and learn how to prevent cannula marks on the face.
Nasal Dryness and Nosebleeds

Many people struggle with dry nasal passages or get nosebleeds from using oxygen, especially those who use oxygen continuously or use a high oxygen flow rate. There multiple ways to address this symptom, and most patients are able to find significant relief with a combination of just a few simple techniques.
Besides feeling dry, other symptoms of nasal dryness include increased mucus production, thick or crusty mucus, or mucus that's streaked with red when you blow your nose. These are very common side-effects of oxygen therapy, but you can manage and minimize them using the tools and techniques we discuss in the following sections.
Most oxygen patients experience nasal dryness occasionally, but you should talk to your doctor if it is very severe or if you are unable to manage it on your own. Left untreated, nasal dryness can worsen COPD symptoms and make you more susceptible to getting sick.
Get an Oxygen Humidifier
If you struggle with nasal dryness or experience nosebleeds as a result of your oxygen therapy, talk to your doctor about getting a humidifier bottle with your oxygen delivery device. All you have to do is fill the bottle up with distilled water (not from the tap), hook it up to your tubing, and it will add moisture to the air passing through so that it's more humid by the time it makes it up to your nasal cannula or oxygen mask.
This is often a very effective way to reducing nasal dryness and can make the air that comes from your oxygen supply more comfortable to breathe. They are also cheap and simple to take care of; just rinse your bottle out daily daily rinses and give it a weekly wash with warm water, soap, and vinegar, just like you do for your nasal cannula.
Get a Home Humidifier
If it's wintertime or the air in your house is dry, you might also benefit from getting a humidifier for your home. You can use single-room humidifiers to moisturize the air in small spaces, or you can invest house humidifier for your HVAC system if you want to go all in.
Even just putting a small humidifier in your bedroom at night can make a huge difference, reducing how dry your skin and nose feels and even reducing your chance of nosebleeds. Especially if you live in a climate with low humidity, a humidifier can help you feel much more comfortable every day, and especially when you use oxygen.

For most people, a humidity level of around forty percent is considered ideal for breathing and comfort. However, some people prefer more or less humidity, and you can adjust your humidifier at home according to your personal taste.
Lubricating Jelly and Nasal Gel

Even if you use a humidifier for your oxygen delivery system and your home, you may still experience nasal dryness on occasion. When this happens, you can use other moisturizing products, like lubricating gels and jellies, that are available over the counter at most superstores and pharmacies.
Nasal gels and jellies are topical lubricating substances that you can apply to the skin inside and underneath your nose. They help seal in moisture in your nasal passage and can reduce friction and soreness caused by the prongs of your nasal cannula.
All you have to do is wash your hands and use your finger or a cotton swab to apply a thin layer of lubricant to the skin just inside your nostrils. You may need to blow your nose after or use a clean towel to remove excess product afterward.
However, don't forget that you should not use petroleum products on your skin if you're going to be using supplemental oxygen, especially on or near your face. Petroleum is very flammable, and when combined with purified oxygen, it becomes even more flammable, raising the risk of serious burns to your face should a fire ignite. Because of this, you should always look for non-petroleum, water-based lubricants instead.
Popular brands of non-petroleum nasal gels include Nasogel, Ayr, and RoEzIt; some patients find that aloe vera works great as well. If you're having trouble finding a gel or have any questions about what nasal lubricant is safe with oxygen, talk to your doctor and ask what products he recommends for you.
Saline Nasal Sprays
Using a saline nasal spray is another effective over-the-counter solution for nasal dryness and soreness caused by oxygen therapy. These products contain a simple solution of water and salt that can be surprisingly effective at soothing and lubricating dry nasal passages.
Note that you should use a spray with a plain saline solution, not the medicated sprays that are often advertised for stuffy noses and colds. Salt water on its own is plenty effective and can be used several times a day, while medicated sprays must be used sparingly and can cause serious side-effects and dependence.

Along with reducing pain and discomfort, moisturizing your nasal passages with a saline spray can also reduce your risk of illnesses and infections. Nasal dryness makes your mucus thick and sticky, raising the risk of trapping harmful bacteria in your airways.
It can also cause the delicate skin in your nose to get dry and cracked, which can make you more likely to get sick. The cracks act like sanctuaries for bacteria, allowing them to multiply and giving them an opportunity to infect your body.
Reducing Skin Dryness and Irritation
Another common problem that patients have with oxygen therapy is dry and irritated patches of skin. Problem areas tend to be the lips, the skin under the nose, and other areas of the face that are near or in contact with your nasal cannula, oxygen, mask, or tubing.
This can be the result of rubbing, chaffing, or the constant flow of air drying out your skin. When you use oxygen continuously, the dryness and irritation doesn't have time to heal, and it will only get worse and worse with time if you don't do something about it.

Luckily, there are plenty of simple solutions for dryness and irritation that can help your skin heal and reduce the chances of future inflammation. In the following sections, we'll discuss a variety of tried-and-true products and techniques that many oxygen patients use to treat skin irritation and make oxygen therapy much easier to deal with.
Use Water-Based Moisturizers on Your Face & Lips

Many of the same moisturizers that you'd use to treat nasal dryness can be used to reduce irritation and chaffing on your skin. Any kind of moisturizing gel or cream can work as long as it's water-based and doesn't contain oils.
Moisturizer can reduce friction and inflammation on any areas of your skin that your head straps, tubing, or other equipment tends to rub against. It's also great for both treating and preventing dry patches that happen as a result of dry air or skin irritation.
Using oxygen can also cause your lips to get chapped, especially if you use an oxygen mask instead of a nasal cannula. You might think the best fix for this is lip balm, but most lip balm brands, including Vaseline, Chapstick, and Blistex, contain petroleum or other oils which can be dangerous to use with oxygen.
Instead, you can use the same water-based lubricants you'd use elsewhere on your skin, like RoEzIt or Vitamin E. You can also find petroleum-free, water-based lip balms from many online retailers that have skin and beauty products for sale.
Use Padding
Many oxygen patients experience discomfort and soreness from tubing, straps, or the edges of their oxygen mask pressing against their skin. In addition to using moisturizers to lubricate the places where the equipment touches your skin, you can use foam and fabric padding to soften the sore points.
There are a variety of different kinds of soft pads and fabric covers you can get to make oxygen masks and nasal cannulae more comfortable to wear. You can find dozens of different options designed to pad all the different areas of your face and head that are prone to experiencing pressure, friction, and discomfort.

For nasal cannulae, you can get small cheek pads to put under the parts of the tubing that stretch across your cheeks. You can also get padding that reduces pain and pressure on your ears, which bear the weight of holding your cannula in place.
For oxygen masks, you can get rubber pads and soft gel pads to soften the point where the mask rests on the bridge of your nose—a common sore point for patients who use masks. You can also get padding and fabric covers for the forehead strap and for straps that go behind your head.
Another common issue with oxygen masks are the lower straps that stretch across your cheeks, which can leave visible red marks and indentations that last for awhile after you take the mask off. To solve this problem, you can buy padded fabric covers designed to reduce the pressure of the strap on your skin, which helps eliminate red marks on your face.
Adding some padding and strap covers can make your mask much more comfortable to wear, especially if you use oxygen continuously or at night. Just make sure you remember to remove and clean any pads or covers your use often with warm soap and water, and replace the padding regularly as the manufacturer recommends. You can also try investing in an extra soft nasal cannula.
Cover Your Tubing
Wrapping the tubing in fabric or foam is a common and very effective solution for skin troubles caused by the friction of a nasal cannula sitting against your face. The constant contact and occasional rubbing can cause soreness and skin irritation over time, which can make oxygen therapy very uncomfortable.
Some people are able to solve this problem simply by finding an oxygen cannula type made with a softer tubing. However, if it doesn't work or you don't have a softer cannula available, then wrapping the tubing in fabric is often the next best option.

There are many different types of fabric tubing covers that you can buy, or you can even make your own if you're handy with a needle and thread. However, the simplest quick solution is to wrap the tubing yourself with fabric first-aid tape, which is cheap, readily available, and easy to use.
To wrap your tubing yourself, get some rolls of white, fabric, self-sticking first-aid tape from your local department store or pharmacy. Then, carefully wrap it all around both sides of your nasal cannula, completely covering the tubing from the prongs to your ears. You can double-wrap it if a single wrap isn't soft-enough, or to reinforce parts of the tubing that cause the most irritation.
However, it's important to remember to keep your tubing covers clean and replace them on a regular basis. If you use a fabric cover, make sure you remove and clean them often. If you covered your tubing in first-aid tape, you should remove and dispose of the tape at least once a week and replace it with fresh tape.
Check Your Fit
Sometimes, skin irritation is a sign that your oxygen mask or nasal cannula isn't fitting you properly. If it's too tight, too big, or sits too loosely on your face, it can cause unnecessary friction and chaffing.
If you are having chronic problems with soreness or irritation, talk to your doctor or your oxygen supply company about getting a new nasal cannula or oxygen mask. You might need to try a different size, a different design, or a different brand in order to find one that fits your face more comfortably.
If you use a nasal cannula, you may also need to try a mask with softer tubing or different prongs. Different cannulas have prongs with slightly different shapes, lengths, and orientations, and which one feels right to you is a matter of personal comfort. Many oxygen patients find that their oxygen therapy is much easier to tolerate once they find a cannula that's the right shape and softness for their face.
Tips for Managing Moisture & Condensation

Some patients struggle with moisture and condensation collecting inside of their oxygen mask or nasal cannula, which can be uncomfortable and make it more difficult to breathe. Excess moisture can also help breed bacteria, which is why you should always try to keep your mask or nasal cannula as clean and dry as possible.
Whenever you notice moisture on the inside of your mask, take it off for a moment and wipe it down with a clean, dry cloth. You should also wash your mask often with warm water and soap at least once a week to remove any mucus, bacteria, or other foreign substances from your mask (but make sure you check the cleaning instructions for your specific mask, first).
Reducing Moisture and Condensation in Your Tubing
Most oxygen patients at some point experience “rain out,” which happens when a lot of condensation forms and collects in your tubing. This tends to be a problem when the humidity is too high or when the outside air is too cold.
For example, if you're using oxygen with a humidifier in a cold room, the tubing gets cooled down by the cold outside air. This can cause the moisture to condense out of the air flowing through the tube, causing water droplets to form in your nasal cannula, oxygen mask, and extension tubing.
This can make it difficult to breathe or cause you to get water in your nose and mouth when you breathe in. It also creates a moist environment that bacteria and mold could grow in if it stays too damp for too long.
To solve this problem, you can turn your oxygen humidifier down to reduce the amount of moisture in the tubing. You can also get a piece of equipment called an inline water trap, a special piece of tubing that attaches to your extension tubing and is meant to catch condensation before it makes it into your nasal cannula or mask.
You can also turn up the heat on your furnace to raise the temperature in the room, which prevents the tubing from getting too cold and causing the moisture inside to condense. Another way to warm up your tubing is to run it underneath a blanket or wrap it in a fabric cover to keep it warm.
If none of these other solutions work, you may need to turn off your humidifier completely to keep the condensation at bay. Once you're in a better environment that won't cause rain out, you can use your oxygen humidifier again.
Reducing Ear Pain and Pressure

Ear pain and pressure is another extremely common problem that patients have with supplemental oxygen therapy. It happens because nasal cannulae are held up by looping over your ears, and the weight creates pressure that can be extremely uncomfortable. If you have to wear a nasal cannula every day for an extended period of time, it can be especially painful and difficult to manage.
Luckily, since it's such a common issue, there are several effective techniques and products available for reducing ear pain and discomfort with oxygen therapy. There are a variety of different types of padding, connectors, specialized nasal cannulae, and more that can make nasal cannulae much more comfort
.png)
We've long known that the harsh chemicals found in many cleaning products can be dangerous if not handled correctly. However, recent research shows that common household cleaners may be much more dangerous than most people realize.
Studies show that breathing in the fumes from cleaning chemicals can cause both short-term and long-term breathing problems. Even if you don't notice immediate symptoms, years and years of exposure to these fumes can cause permanent lung damage and even life-threatening diseases like COPD.
This means that anyone who uses cleaning chemicals regularly may be putting their lungs at risk. However, the risk is much higher for people who suffer from existing respiratory problems like asthma or COPD.
People with respiratory diseases are particularly sensitive to the damaging effects of respiratory irritants like chemical fumes. That's why it is particularly important to learn how to recognize and avoid hazardous cleaning chemicals if you have a lung condition like COPD.
In this article, we're going to explain everything you need to know about how to protect your lungs from dangerous chemical fumes. We'll tell you which products are dangerous, which products are safe, and how to adjust your cleaning methods to be more lung and COPD-friendly.
We'll also introduce you to a variety of simple, safer cleaning techniques and alternative cleaning products, including lung-healthy cleaning solutions that you can make yourself at home. You will find all kinds of practical tips and tricks in this guide that you can use to significantly reduce your exposure to toxic cleaning fumes.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What Cleaning Fumes Do to Your Lungs
Any time you use a cleaning solution, it emits fumes into the air that you inevitably end up breathing. These fumes are made up of gaseous chemicals and tiny droplets that mist from the solution.
Many chemicals found in cleaning products create fumes that are irritating and toxic to your lungs. As soon as the fumes touch your lung tissue, they can cause inflammation and a variety of respiratory symptoms like coughing, sneezing, and shortness of breath.
These fumes can also inflame your eyes, nose, and upper airways, causing sharp, burning pain when you breathe. If you're exposed to a lot of fumes all at once, you might experience a sore throat, dizziness, headache, nausea, and even stomach pain.
These are the acute, immediate effects, but breathing chemical fumes can cause long-term health problems as well. Breathing in even small amounts of fumes over a long period of time can cause chronic health problems and do permanent damage to your lungs.
This often happens as a result of inflammation in the lungs, which can occur any time you breathe in a respiratory irritant, including chemical fumes. If sustained for too long, the inflammation begins to injure healthy lung tissue.
This kind of lung damage is permanent and cannot be reversed. Over many months or years, as more and more lung tissue gets affected, the damage can add up and cause noticeable lung function decline.
Certain chemicals, such as ammonia, emit fumes that are immediately caustic to your lungs. When these fumes come in contact with the delicate tissue lining the inside of your lungs, they cause immediate cell death, destroying healthy lung tissue and causing inflammation.
Usually, it takes many episodes of chemical exposure and inflammation over the span of many years to cause noticeable long-term damage. Unfortunately, studies show that simply using household cleaning products on a regular basis is enough to cause permanent damage—and even COPD—over time.
That's why you should never assume that your lungs are safe when you clean just because you don't notice any symptoms or the fumes don't burn your nose. You might not realize that cleaning fumes have damaged your lungs until much later in life when it starts to have more obvious effects on your health.
What the Research Says
Researchers have known for some time that exposure to cleaning chemicals can cause asthma and respiratory symptoms, but they had little data on the long-term effects. In the past few years, however, researchers have found strong links between cleaning chemical fumes and chronic respiratory diseases.

This is something scientists have long suspected but, until recently, didn't have the data to prove. Fortunately, two large-scale studies published in the past couple of years have shed more light on the link between cleaning fumes and long-term respiratory problems.
One study from Harvard, published in 2017, found a strong correlation between subjects' use of chemical cleaners and fatal lung diseases like COPD. In a study of more than 55,000 US nurses that spanned thirty years, they found that those who used chemical disinfectants just once per week had a 32 percent higher risk of developing COPD.
A more recent study from the University of Bergen in Norway looked at the effects of cleaning in a typical home environment. After tracking 6,000 subjects for twenty years, they found that women who regularly used chemical cleaning solutions had poorer respiratory function than those who didn't.
In fact, researchers estimated that the amount of lung function these women lost was roughly equivalent to smoking a whole pack of cigarettes every day. Those who were exposed even more often than that experienced more severe lung decline.
Despite including men in the study, they were unable to find any strong evidence of cleaning product-related lung decline in men. However, that doesn't mean that men who get regularly exposed to fumes from cleaning chemicals are any less at risk; the researchers noted that the men in the study just didn't use cleaning products as often as the women subjects, which likely left them with too small a sample to detect such effects among the men.
These studies show that even minimal exposure to chemical fumes can have a significant effect on your lungs over the span of many years. They also indicate that the severity of lung damage is directly related to how frequently you are exposed.
The most important take-away is that you should limit your use of chemical cleaning products as much as possible. And when you must use them, you should be careful to breathe in as little fumes as possible.
How Cleaning Fumes Affect People With COPD

Using household cleaning chemicals puts you at risk whether you're a healthy adult or someone who suffers from a chronic breathing disorder. However, exposure to chemical fumes can be even more dangerous for lungs that are strained due to an existing respiratory problem like asthma or COPD.
People with these conditions have particularly sensitive lung tissue, which means that even small amounts of fumes can trigger inflammation in their lungs. This makes their lungs more vulnerable to permanent damage as a result of exposure to chemical fumes.
Because their lung function is already limited, the damage COPD patients sustain from repeated exposure also has more serious effects. Further damage and inflammation from cleaning chemicals is much more likely to cause noticeable symptoms and measurable lung function decline.
Because of this, repeatedly breathing in respiratory irritants like chemical cleaning fumes can actually cause the disease to progress faster. It can cause quicker lung function decline and cause patients' respiratory symptoms to permanently get worse.
Cleaning fumes are also more likely to trigger immediate respiratory symptoms—like wheezing, coughing fits, and severe shortness of breath—in people with COPD. In some cases, they can even trigger COPD flare-ups that last long after the fumes are gone.
As a result, using household cleaners at all can make your COPD symptoms more difficult to manage on a daily basis. This can be dangerous, since managing your symptoms is a vital part of keeping your lungs healthy, preventing complications, and slowing down the progression of COPD.
In the next sections, we're going to show you a variety of ways you can reduce your exposure to dangerous cleaning chemical fumes. First, we'll take a look at which cleaning products are safe (and not safe) to use, and then we'll show you some specific tips and tricks for keeping your lungs protected every single time you clean.
Which Cleaning Products are the Most Dangerous?
Few commercial cleaning products are completely safe to use, but some seem to be much worse for your lungs than others. Certain harsh cleaning chemicals, like ammonia and bleach, are particularly toxic to breathe.
The 2017 Harvard study, for instance, identified some specific chemical culprits that were most strongly linked to respiratory decline. They found that exposure to cleaning solutions containing bleach and a category of chemicals known as quaternary ammonium compounds (quats) seemed especially likely to cause COPD later in life.
Researchers believe that both types of chemicals can cause significant respiratory problems, even in small amounts, to people who use them regularly. If they are that dangerous even to healthy adults, using these chemicals could have even worse consequences for people with asthma or existing respiratory diseases.
Unfortunately, ammonia and bleach are some of the most common chemicals found in commercial cleaning products. If you don't read the ingredients carefully, you might even use cleaners containing ammonia or bleach without even realizing it.
However, ammonia and bleach are not the only chemicals worth avoiding; most commercial cleaning products contain chemical compounds that can irritate your lungs. A category of chemicals known as volatile organic compounds (VOCs), for instance, are well-known air pollutants and respiratory irritants that are found in all sorts of cleaning solutions.

There are many different types of VOCs, and they are found in a wide array of products, including cleaning solutions, hair spray, and even building materials like plywood and glues. Some VOCs are harmless, while others can hurt your lungs and cause a variety of other health issues, including organ damage and cancer.
In small amounts, VOCs are usually not harmful to healthy adults. However, if you get exposed to too many VOCs over a long period of time, they can cause serious health problems and chronic respiratory symptoms.
VOC's are most likely to cause respiratory symptoms in people with sensitive respiratory tracts, including people with asthma and COPD. Their existing respiratory issues make their lungs more prone to both the short-term and long-term effects of exposure, which is why they should be more careful to avoid VOCs.
If you have asthma or COPD, even mild fragrances in cleaning solutions and air fresheners can irritate your lungs badly enough to cause serious respiratory symptoms. Other VOC-heavy household chemicals, like adhesives, varnishes, and fabric softeners, may also trigger coughing and shortness of breath.
That's why it's important to check the ingredients on any cleaning and chemical products you buy to use in your home. Unless you need them for a very specific purpose, you should always avoid any cleaning solutions that contain ammonia, bleach, VOCs, or other harsh cleaning chemicals.
Sometimes, you can find versions of cleaning products that contain smaller amounts of VOCs and other noxious chemicals. However, it can be difficult to determine whether a product is safe because it's so hard to recognize the names of all the hazardous chemical compounds.
To help you out, we've made a list of some of the most common chemicals in cleaning solutions that can be dangerous to your lungs. We've also included some of their more obscure chemical names so you can more easily pick them out of ingredient lists.

Here are some of the most hazardous chemicals for your lungs and respiratory system:
- Ammonia
- Bleach
- Sodium hypochlorite
- Chemical solvents
- Hydrochloric acid
- Sulfiric acid
- Napthalene
- Propellants
- Formaldehyde (a VOC)
- Hydroxymethylglycinate
- Diazolidinyl urea
- Quaternium-15
- DMDM, aka Glydant
- Bronopol, aka 2-bromo-2-nitropropane-1,3-diol
- Grotan, aka hexahydro-1,3,5-tris(2-hydroxyethyl)-S-triazine
- Quaternary ammonium compounds
- Stearalkonium chloride
- Benzalkonium chloride
- Centrimonium bromide
- Quaternium 1-29
- Didecyl dimethyl ammonium chloride (DDAC)
- “Fragrance” (many products don't list specific chemicals used for fragrance)
- 1,4-dioxane
- Cresol
Here is a list of some specific products that contain hazardous chemicals or emit fumes that can irritate your lungs:
- Drain cleaners
- Disinfectants and sanitizing solutions
- Aerosol sprays (including fragrances and air fresheners)
- Carpet powders
- Dry cleaning powders
- Pain thinners
- Varnishes
- Adhesives
- Paint fumes
- Fabric softeners
If you suffer from chronic respiratory problems, it's worth going well out of your way to protect your lungs from all types of cleaning fumes, not just ammonia and bleach. That's why it's best to avoid commercial cleaning products all-together when possible and make your own lung-healthy cleaning solutions at home.
Which Cleaning Products are Safe?

The vast majority of commercial cleaning solutions are likely to contain noxious chemicals, VOCs, and fragrances that are dangerous to breathe. In order to eliminate the risk of harmful fumes, you will likely have to buy specialized, mild cleaning products or make your own DIY cleaning solutions.
Lung-Safe Commercial Cleaning Products
Unfortunately, products labeled “green” or “environmentally-friendly” may not actually be any safer for your lungs. That's why reading the label is a must; you should always look closely at the ingredients list and warning information before using any commercial chemical.
However, there are some other resources that can help you find safer cleaning products to use in your home. Both the Asthma and Allergy Foundation of America and the EPA have endorsed a multitude of products that are better for your health and the environment.
How to Find Safer Cleaning Products:
- The EPA's search tool for “Safer Choice Standard” products (search by product type to find a variety of products for different cleaning purposes)
- The Asthma and Allergy Foundation of America's list of certified asthma- and allergy-friendly products
DIY Lung-Safe Cleaning Products You Can Make Yourself at Home
 |
| Photo by Abi Porter |
Safe commercial cleaners can be difficult to find and expensive to buy once you do. Luckily, you can make simple and effective cleaning solutions yourself using just a few basic ingredients.
The following DIY recipes for homemade cleaners all use common, mild ingredients like soap, baking soda, vinegar, lemon juice, and borax. If you have asthma or COPD, these solutions won't harm your lungs and shouldn't trigger any respiratory symptoms.
All-purpose Cleaner
Recipe:
- 1 quart warm water
- 4 tablespoons baking soda
Uses: This deodorizing solution is great for cleaning smooth surfaces like appliances, faucets, kitchen counters, door handles, and more.
Instructions: Mix the water and baking soda together in a large container like a bucket, mixing bowl, or a large pot. To use, simply wet a cleaning towel or sponge with the solution and gently wipe down the surface you want to clean. The solution works best while the water is warm, so you should try to use it immediately.
Glass and Window Cleaner

Recipe:
- 2 cups water
- ½ cup white vinegar
Uses: Use to wipe down smooth glass surfaces like windows, glass doors. and glass tabletops.
Instructions: Mix the water and white vinegar together and store the solution in an airtight container or spray bottle. To use, either spray the solution directly on the glass surface and wipe dry, or wipe down the surface with a clean cloth dampened with the solution. You may need to wipe the surface one more time with a dry cloth to remove any moisture and leave the glass streak-free.
Grease-cutting Cleaner
Recipe:
- 1 cup white vinegar
- A few drops of liquid Dawn dish soap
- 1 tablespoon baking soda
- 2-3 cups of water
Uses: This cleaner is great for removing oil and grease from smooth surfaces like your kitchen counters, oven, and sink.
Instructions: Mix the vinegar, dish soap, and baking soda together in a spray bottle or another airtight container. Then add 2-3 cups of water and shake vigorously. Spray the greasy surface directly or dip a sponge in the solution, then wipe the surface clean. You may need to give the surface another wipe with a damp cloth to remove any leftover residue.
Scrubbing Solution

Recipe:
- 2 tablespoons lemon juice
- ½ up borax
Uses: This paste is great for removing rust and stains from porcelain, enamel, or stainless steel surfaces like your bathtub or sink.
Instructions: Mix the lemon juice and borax together to form a gritty paste. Apply the paste to a sponge or scrub brush and scrub the surface you want to clean. Once the stain or rust is removed, wipe the area clean with a damp cloth.
How to Reduce Your Exposure to Cleaning Fumes
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
There are many things you can do when you use cleaning products to reduce your exposure to their fumes. After all, even cleaning products that are safer for your lungs can irritate your respiratory system if it is very sensitive or you suffer from severe COPD.
That's why it's important to learn how to use all cleaning products safely. That includes properly handling chemicals, using noxious cleaners only when necessary, and ensuring that the air is well-ventilated while you clean.
Don't Use Spray Bottles

Spray bottles turn cleaning solutions into a fine mist, much of which ends up in the air rather than on the surface you are spraying. These droplets and fumes mix into the air and get into your lungs when you breathe.
Because of this, any time you use a cleaning spray, you are essentially spraying chemical fumes into the room. It is exposes you to significantly more fumes than plain liquid solutions and can be much more damaging to your lungs.
Instead of using spray bottles, you can simply use a cloth or sponge to absorb the solution and coat the surface you want to clean. Just dip your cloth (or sponge) into the solution, wring it out, and use circular wiping motions to distribute it evenly over the area.
Then, use a clean, damp cloth to wipe off the solution and any residue it loosens up. You may need to do a final wipe with a dry cloth to remove any excess moisture left behind.
Minimize How Often You Use Chemical Cleaners

Having COPD means you are more prone to illnesses and respiratory infections, which means it is very important to keep your environment free of bacteria and other sickness-causing pathogens. However, that doesn't mean that you have to use harsh chemicals and disinfectants every time you clean.
Chances are you don't actually need to use chemical cleaners and sanitizing solutions nearly as often as you think. In fact, the vast majority of cleaning tasks can be completed to satisfaction with nothing more than a clean cloth,
Influenza—also known as the flu—is one of the most common and deadly viruses that spreads throughout the US every year. With the peak of the flu season beginning in January and continuing through March, now is the time to get your flu vaccine if you haven't done so already.
Experts recommend that every person over 6 months old get the flu shot every year, but it is especially important for older adults and people with serious health conditions. This applies particularly to people with chronic respiratory diseases like COPD, who have a much higher risk of experiencing life-threatening complications if they get exposed to the flu.
Unfortunately, most adults fail to get the vaccine, and only about forty percent of American adults get their flu shot in any given year. However, doctors and health experts strongly urge all adults to get vaccine, both for their own health and to protect the health of others.
Still, flu vaccination rates stay low, in part because many people underestimate how serious and deadly the flu can be. This, in turn, causes many people to underestimate the importance of the flu vaccine and assume that skipping the yearly shot is not a big deal.
In this post, we're going to explain why getting your flu shot is vital, whether you are old, young, healthy, sick, or anything in-between. We'll also take a closer look at some of the reasons people decline the flu shot while debunking some of the most common myths and misconceptions.
We'll show you how the flu shot works, why it's recommended, and how it protects the lives of people with COPD and other chronic diseases. With the information in this guide, we hope that you will better understand the flu vaccine and why doctors believe it is so important for public health.
Flu Vaccine Basics: What You Should Know
Who Should Get the Flu Vaccine?

Many people assume that the flu vaccine is meant mainly to protect the young, elderly, and people with serious health conditions. However, this is false; doctors and health experts urge everyone over 6 months of age to get a flu shot every year, with just a few exceptions.
Your doctor will be able to tell you if you should get the flu vaccine and will give you the vaccine that is appropriate for your age. For example, adults over the age of 65 receive a special high-dose flu vaccine that is more effective for older adults.
According to the CDC, the following people should get vaccinated against the flu every year:
- Children 6 months of age and older
- All adults, including pregnant women
- Most adults who have chronic health conditions (talk to your doctor if you are unsure)
However, there are some people who should not get the flu vaccine, including:
- Some people with allergies to eggs or other ingredients in the vaccine (If you are allergic to eggs, you should notify your doctor, but you can most likely still get a flu vaccine.)
- Some people with Gillain-Barre Syndrome
Who Recommends the Flu Vaccine?

Just about every major governmental health organization along with many other expert health organizations recommend routine flu vaccination. They emphasize the importance of vaccination in the young, elderly, and those with chronic health conditions, but also urge healthy children and adults to get the vaccine as well.
Here is a list of some of the major health organizations that endorse the flu vaccine:
- The United States Center for Disease Control and Prevention (CDC)
- The World Health Organization (WHO)
- Canada's National Advisory Committee on Immunizations (NACI)
- The European Center for Disease Prevention and Control
- A large number of leading public health organizations and experts. The following represent just a few:
- American Academy of Family Physicians (AAFP)
- American Academy of Pediatrics (AAP)
- American College of Physicians (ACP)
- American Pharmacists Association (APhA)
- Association of Occupational Health Professionals in Healthcare (AOHP)
- National Foundation for Infectious Diseases (NFID)
- And many more!
Who is Most Vulnerable to Serious Flu Complications?

Certain groups of people are much more susceptible to the flu and flu-related health complications than others. This includes a larger number of people than most tend to realize, including anyone over the age of 65, anyone under the age of 5, and people with common health conditions like heart disease and COPD.
For these people, a flu infection could be deadly or cause serious secondary infections like pneumonia. That's why it's especially important for people who belong to these vulnerable groups to get vaccinated against the flu.
According to the CDC, it is particularly important for people in the following vulnerable groups to get the flu vaccine:
- Children under 5 years old (particularly children under 2)
- Older adults over the age of 65
- Pregnant women
- People in nursing homes and long-term care facilities
- Native Americans and Alaska Natives
- People with chronic respiratory illnesses, including asthma, COPD, and cystic fibrosis
- People with other chronic diseases, including heart disease, kidney disease, liver disease, and metabolic disorders like diabetes
- People with blood disorders (e.g. sickle cell disease)
- People with extreme obesity
- People with neurological and developmental disorders (e.g. cerebral palsy, epilepsy, stroke, and muscular dystrophy)
- People with suppressed immune systems (e.g. people taking steroids, immunosuppresant medications, and people with HIV)
- People receiving long-term aspirin therapy
When Should You Get Your Flu Shot?
The CDC recommends that you get your flu vaccine by the end of October every year. This gives the flu vaccine time to work before flu season begins to pick up in November-December.
In general, you will be protected from getting the flu about two weeks after you get your shot. That's why it's better to get your shot earlier in the season, rather than waiting until the flu has already begun to spread.
However, if you forget to get vaccinated early, you can still get the flu vaccine anytime throughout the winter and early spring. It will still be just as effective later in the season, but it won't be able to protect you from any flu viruses you catch before the vaccine takes effect.
If you are over the age of 65 or suffer from a chronic disease like COPD, then it's especially important for you to be protected from the flu for the entirety of the flu season. You should get your vaccine as early as possible so that your immune system has plenty of time to prepare before the virus begins to spread.
How Much Does the Flu Shot Cost?
If you have health insurance, then it's almost always free to get your yearly flu shot. But even if you don't have insurance, you may still be able to get the shot for free, or at least at a reduced price.
The chances are good that you can find some sort of program or event in your city that offers the flu vaccine for free. At worst, you shouldn't have to pay more than $25-35 out of pocket to get the shot at your local Walmart or CVS.
All Medicare plans also fully cover the flu shot. If you have medicare part B, the deductible doesn't apply to the flu vaccine, so you shouldn't have to pay any out-of-pocket costs.
If you don't have health insurance, click here to see a helpful list of some of the cheapest places you can go to get your flu vaccine.
Where Can You Get Your Flu Shot?

Flu shots are cheap, quick, and readily available all across the United States. You can get the vaccine at a variety of different places, including your doctor and just about any chain-business pharmacy.
Many colleges, employers, and other organizations also give flu shots on-site or offer vouchers to get a flu shot for free. You can also check with local health organizations and city, county, or state health departments to see if they offer flu vaccination programs or incentives.
Here is a list of some of the places you can go to get your flu vaccine:
- Your primary care doctor (you can make a special appointment or get the shot during a routine examination)
- Urgent care centers (these are often more convenient and closer to home than the doctor's office)
- Pharmacies (these are often the cheapest and most convenient option, and it's usually free if you have health insurance)
- Walmart
- Walgreens
- CVS
- Kroger
- Rite Aid
- Target
- Kmart
- Stop & Shop
Why You Should Get the Flu Vaccine: A Matter of Life and Death

The reason you should get your flu shot is twofold: first of all, you want to protect yourself from getting sick with the influenza virus and experiencing potentially life-threatening complications. The second is to prevent you from transmitting the virus to other people around you who could be even more vulnerable to the illness.
Here is a quick summary of the major benefits of getting the flu vaccine before we go into them in more detail.
Benefits of Flu Vaccination:
- Reduces your chances of getting sick with the flu
- Reduces your chances of experiencing a serious health complication (including hospitalization and death) from the flu
- Can reduce the severity of your flu symptoms and your risk of complications even if you end up getting sick with the flu
- Reduces your chances of spreading the flu virus to other people (including infants, who cannot receive the vaccine)
- Reduces the risk of serious complications, hospitalization, and death if you are over 65 or suffer from a serious health condition like COPD
- Protects pregnant women and infants (If a pregnant woman receives the flu vaccine during pregnancy, it can protect their infant child from the flu for several months after giving birth)
Getting the Flu Vaccine Protects Your Own Health

According to the Centers for Disease Control and Prevention (CDC), the flu kills, on average, 12,000 to 56,000 people in the US and puts up to 710,000 people in the hospital every year. The exact number of deaths and hospitalizations can vary significantly from year to year depending on the severity of flu outbreaks.
2017, for instance, was a particularly bad year for the flu in the US. That year, more than 80,000 Americans died from the flu, marking the highest number of flu-related deaths in four decades.
Many of these deaths and hospitalizations could have been prevented if more people had gotten the flu vaccine. Many of those who died were also healthy adults with no other serious medical conditions.
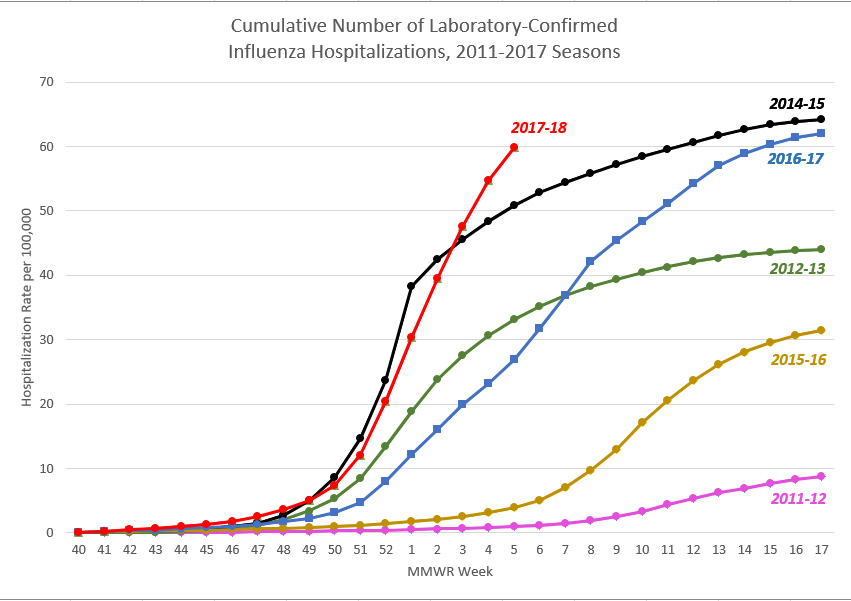 |
| Image created by the CDC |
Just because you've had the flu before and it turned out fine, that doesn't mean you're not at risk in the future. You may have gotten over many flus in your life, but all it takes is one serious infection to put your life and health on the line.
Whether you are 17 or 75, the flu vaccine could save your life and significantly reduce your chances of being hospitalized with the flu. Especially if you have COPD or belong to another high-risk group, there is no reason to take the risk of not getting the shot when the vaccine is so cheap and readily available.
Getting the Flu Vaccine Protects Others Around You and Can Even Save Lives
Even if you are not concerned about getting sick yourself, failing to get your flu vaccine could put the lives of vulnerable people at risk. That's why doctors recommend that everyone, even those with a low risk of flu complications, get the flu vaccine every year.
Chances are, you, a family member, or someone else you know comes into regular contact with someone with a serious health condition who needs extra protection from the flu. More than 11 million people in the US have been diagnosed with COPD alone, and they are certainly not the only ones who are at risk.
Unfortunately, many vaccinations—including the flu vaccine—are not as effective in the elderly and people with compromised immune systems. Even if they get vaccinated, their immune systems may not be able to build up an effective immunity to the virus.
The same applies to infants under the age of 6 months, whose immune systems aren't fully developed. Because of this, infants this young can't generate the immune response necessary to gain immunity from the vaccine.
All of these people who cannot build immunity on their own--from infants to older adults to immuno-compromised individuals--have to rely on the people around them to get vaccinated to protect them from the flu. This relates to a concept known as herd immunity, which we'll discuss more in the sections below.
How Does the Flu Vaccine Work?
Even though the flu vaccine is more effective and more readily available than ever, a large percentage of people in the US still decline this life-saving vaccine. We hope that by learning more about how the vaccine works and the benefits it has to offer, more people—especially at-risk populations like people with COPD—will choose to get their flu vaccine every year.
How Does the Flu Vaccine Protect You From the Flu?

The flu vaccine is essentially a mixture of inactivated flu virus strains. However, instead of getting you sick, the viruses in the vaccine help your immune system prepare to fight similar viruses in the future.
Most simply put, the flu vaccine introduces your immune system to a small sample of the same types of viruses that it might encounter if you get exposed to the flu. Your immune system then “remembers” what those viruses look like by creating an army of tiny molecules—called antibodies—that can recognize what the virus looks like.
That's why, when you get the flu vaccine, it takes a couple of weeks to take full effect. During those two weeks, your immune system is working hard to build up store of antibodies that will lie in wait until you get exposed to the virus again.
The next time one of those viruses (or a similar virus) enters your body, the antibodies will recognize the virus immediately and mark it for destruction. This allows your body to kill the virus so quickly that it never gets the chance to infect you and make you sick.
How Do Researchers Develop the Flu Vaccine Every Year?

The first vaccine able to combat the influenza virus was developed by researchers in the mid 1940's. This first vaccine only worked against one specific strain of the flu virus, but modern flu vaccines offer even greater protection.
The flu vaccine is unique in the sense that it get re-formulated every year. This allows researchers to create a vaccine that targets specific virus strains that are active at the time.
This is necessary because the flu is not just a single virus. There are hundreds of different known flu virus strains, and they evolve and change very quickly.
Right now, it is impossible to develop a vaccine that works against every single flu virus strain. Even if it were, the flu virus changes so quickly that it would evolve to evade the vaccine over time.
That's why researchers work hard every year to predict which strains are the biggest threat. Then, they pick the top 3-4 strains and develop a vaccine that boosts your immunity to those and similar virus strains.

Researchers are pretty good at predicting which strains will be most active, even though their estimations are not always perfect. But even with just 3-4 strains included the vaccine, researchers have been able to develop a vaccine that prevents, on average, up to ninety percent of of targeted flu viruses and about fifty percent of overall flu infections.
However, it's impossible to predict the future with absolute certainty, which means that the flu vaccine might be more or less effective in different years. If the common flu virus strains circulating around don't match well with the strains included in the vaccine, then the vaccine may not be able to prevent as many infections as expected.
How Effective is the Flu Vaccine?
On the surface, a sixty percent overall effectiveness rate might not seem very impressive for a vaccine, but there's a reason that it's endorsed by CDC and leading health organizations. A flu vaccine that prevents more than half of infections is extremely valuable, especially considering how deadly the flu can be.
Consider the fact that, in one of the deadliest flu seasons in America, the flu killed more than 80,000 people and forced Alabama to declare a public health emergency. The flu is no joke, and any vaccine that prevents a noticeable percentage of infections or deaths is absolutely worthwhile to use.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
The flu vaccine doesn't just reduce the number of people who get sick, but also reduces the number of serious flu complications and protects people in vulnerable groups. For example, the vaccine is 30-70% effective at preventing hospitalization with the flu in healthy adults, and 50-60% effective at preventing hospitalization in adults living in long-term care facilities like nursing homes.
The flu vaccine can also dramatically reduce the number of people who die from the flu. For people in long-term care facilities, the flu vaccine reduces death from flu complications by a whopping eighty percent.
The flu shot is also particularly effective at protecting children, which is evidenced by the fact that three out of four children who die from the flu did not receive a flu vaccination. In fact, one study found that getting the flu shot reduced the risk of flu-related death by 65 percent in healthy children and 51 percent in children with high-risk medical conditions.
What is Herd Immunity?

Remember how we mentioned that the flu vaccine not only protects you, but it protects people around you, too? This happens largely because of a nifty phenomenon known as herd immunity.
Simply put, herd immunity is the ability of a large population to resist an illness when a large number of people within that population are immune. It works by “breaking the chain” of infection, because people who are immune to an illness won't pass on that illness to others.
Viruses like the flu cannot spread as quickly when it continually encounters people who are vaccinated and immune. In this way, the flu vaccine can protect even those who are not vaccinated—and are thus not immune—from catching the flu.
Think of it this way: each person who gets the flu is one link in a long, branching chain that represents how the virus spreads from person to person. But if the flu virus reaches someone who is immune, then that particular branch of the chain stops, since the
-png.png)
Being diagnosed with a respiratory illness such as chronic obstructive pulmonary disease (COPD), cystic fibrosis, or pulmonary fibrosis can be life-changing. You’ll have to make adjustments to your daily routine in order to accommodate for doctors visits, pulmonary rehabilitation, supplemental oxygen therapy, and other lifestyle changes.
One hurdle many respiratory patients struggle to overcome after being diagnosed with COPD or similar conditions is maintaining relationships. Whether you like to visit a friend down the street or you have a long-time friend who lives overseas, a respiratory impairment of any kind can make these relationships difficult or impossible to maintain.
The good news, however, is that with enough time and patience, it is possible for respiratory patients to live a normal life. And the more you educate yourself about your condition and the tools at your disposal to help you succeed, the more equipped you will be to deal with problems when they arise.
Possibly the best way for COPD patients to overcome the setbacks of their illness is to invest in a portable oxygen concentrator. Unlike other oxygen delivery devices, portable oxygen concentrators enable patients to regain their freedom and independence while ensuring their oxygen needs are always met. Read on to learn 7 of the most important social benefits of owning a portable oxygen device.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Greater Independence
Independence is something that’s easy to take for granted until it’s gone. Independence is what allows us to get out and do the things we want on our own terms rather than being bound to a person or thing. Unfortunately, many COPD patients lack the independence they need to maintain an active social life.
Traditional oxygen devices like compressed oxygen tanks make it very difficult for respiratory patients to maintain their independence. These tanks can often weigh in excess of 100 pounds and they need to be refilled every time they run out of oxygen. There are portable oxygen tanks available, but they typically only hold a couple of hours worth of oxygen.

Refilling an oxygen tank is a long and tedious process no matter how you do it. If you want a professional to refill your oxygen tanks, you’ll likely need to sign up for an oxygen delivery service which is not only expensive, but it can be very time consuming as well. If you opt to refill your own oxygen tanks, you’ll need to purchase an oxygen refill system. These are very bulky devices that will stay in your home and can take several hours just to refill a small oxygen cylinder.
Aside from being dependent on their oxygen tank, oxygen refill station, or an oxygen provider, many COPD patients are dependent on their friends and loved ones. From making it to monthly doctors appointments or pulmonary rehabilitation appointments, it can be impossible to keep up with all of these things on their own. There’s no understating the work that caretakers put into helping their patients, but the truth is, many COPD patients want to take care of themselves.

This is where portable oxygen concentrators come into play. Unlike with oxygen tanks, you can be entirely self-sufficient when using a portable oxygen concentrator. Since they are electronic devices, all you need is access to a wall outlet in order to charge the batteries. And once they’re charged, you can go wherever you please without having to worry about your oxygen supply.
Ultimately, POCs will give you the independence you need to handle your own life without depending on others. You can make it to doctors appointments, pulmonary rehab, and social gatherings without having to bring a loved one or caretaker along to help out.
Better Health
The goal of supplemental oxygen therapy is to reduce common symptoms associated with COPD. This includes symptoms such as breathlessness, chest pain, coughing, wheezing, and more. Studies have also shown that supplemental oxygen plays a key role in treating COPD exacerbations by preventing hypoxia (deficiency of oxygen in the tissues).
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Whether you’ve been prescribed oxygen for several hours a day or your doctor wants you on oxygen 24/7, your health depends on your ability to receive the right amount of oxygen at the right time. And at the end of the day, portable oxygen concentrators offer much more flexibility when it comes to how your oxygen is administered.
.png)
Portable oxygen concentrators like the Inogen One G5, for example, provides patients with up to 1,260 ml/min of medical grade oxygen. The flow rate can easily be adjusted using the arrow buttons on the top of the unit, allowing you to fine-tune the amount of oxygen you receive. If for some reason a breath isn’t detected and no oxygen is put out of the device, you’ll hear an audible alarm notifying you.

When your health is in check and you’re doing everything you can to prevent COPD exacerbations, you’re likely going to have a much better social life. Whenever you go out with friends or family, you can rest assured that you’re receiving the oxygen you need to stay saturated. Of course, you’ll still want to take precautions such as avoiding polluted or smokey areas that could lead to exacerbations.
Long-Distance Travel is Possible
It’s hard to believe that just several decades ago, it was impossible for oxygen patients to travel long distances safely. Oxygen tanks have never been approved for in-flight use because they’re a fire hazard and they’re highly explosive. However, with the advent of portable oxygen concentrators, oxygen patients can travel freely on most major airlines as instructed by the Federal Aviation Administration (FAA).
.jpg)
The main reason POCs are safe on airplanes is that they contain pressurized oxygen like oxygen tanks do. They simply take ambient air, remove nitrogen, argon, and other impurities, then put out medical-grade oxygen via the nasal cannula. As aforementioned, it will only work when it detects a breath, so if you happen to drop the cannula, it won’t continue to put out oxygen.
Another form of long-distance travel you’ll have available to you are cruise ships. Taking a cruise is one of the best ways to explore an area of the world that you’ve never been to before and it’s also a great way to catch up with friends and family. While oxygen tanks are often permitted on cruise ships, this doesn’t necessarily mean you’ll have a way to refill it. And spending extra time with that means less time that you can spend with your loved ones.

On the other hand, all you’ll need with a POC is a fully charged battery and you’ll be able to stay out all day enjoying your time. Once you settle in for the night, you can charge up all of your batteries and have them ready to go in the morning. With the Inogen One G5, you can even invest in an external battery charger which will allow you to charge a battery separately from your POC.
If flying or taking a cruise isn’t your style, you might want to take a long road trip. Luckily, this is also a breeze when you have a portable oxygen concentrator. Most POCs either come with a DC charging cable or you can purchase one separately which will allow you to charge your device in your car using the cigarette outlet.

All-in-all, owning a portable oxygen concentrator is the best way for respiratory patients to stay connected with their friends and loved ones over long distances. Rather than fussing with an oxygen device that’s difficult to use and could put your health at serious risk, POCs just work, allowing you to spend quality time with your loved ones.
Improved Physical Endurance
Everyone has a friend or two who are constantly on the go. With healthy lungs, this might not be a problem, but if you have a respiratory illness, you may find it difficult to keep up with them. Aside from keeping your COPD symptoms in check, studies have also shown that supplemental oxygen can induce an enhanced physiologic training effect on the muscles which can improve your endurance and strength.

Another way portable oxygen concentrators help with physical activity is that they’re extremely lightweight and easy to carry. The Caire Freestyle Comfort, for example, weighs in at just 5 pounds and it’s still able to put out an outstanding 1,050 ml/min of medical-grade oxygen. Compare this to oxygen tanks or continuous flow portable oxygen concentrators which are too heavy to carry meaning you’ll have to wheel them behind you using a rolling cart.

Ultimately, owning a pulse flow portable oxygen concentrator means you’ll be able to keep up with those active friends in your life. Whether you just want to go for a daily walk in the park or you want to start a new exercise program, you’ll be able to do so without worrying about your ability to keep up.
Reduced Social Stigma
Social stigma is an unfortunate, but very harsh reality that people face on a daily basis. Essentially, a social stigma is a sort of generalized feeling about a certain person or thing. For example, people may see someone in a wheelchair and believe that they’re less capable than someone who can walk.

Similarly, someone who’s carrying or rolling an oxygen tank around with them may be seen as less capable than someone with a portable oxygen concentrator. One of the reasons for this is because most people don’t even know what portable oxygen concentrators are. They also look a lot more high-tech and advanced than oxygen tanks which affect the way people view them.
At the end of the day, we all know that oxygen patients are equally as capable as anyone else. However, owning a portable oxygen concentrator may prevent people from making generalized assumptions about you and your condition. It can also be a great conversation starter because people will be curious about what your POC does and how it works!
Improved Self-Confidence
One thing that’s more important than the way others feel about you is the way you feel about yourself. Confidence is key to maintaining any relationship and portable oxygen concentrators will inevitably make it easier to feel comfortable and confident being yourself.
.jpg)
When it comes to oxygen tanks, there’s very little in the way of customization or personalization. Most oxygen tanks are a drab silver and green color that’s not very appealing to the eye. This can lead to you feeling self-conscious about your oxygen tank, taking your mind off social interactions as a result.
-min.png)
Due to their size and bulkiness, oxygen tanks can also be embarrassing to maneuver in public. Whether you’re walking down a crowded sidewalk or you’re going up a flight of stairs, it’s difficult to be graceful with an oxygen tank.
Portable oxygen concentrators are the polar opposite of this. They’re light enough to carry on your shoulder and small enough to tuck under your arm without bumping into people. You also won’t have to dread taking public transportation or going up a flight of stairs with a portable oxygen concentrator.

When it comes to aesthetics, portable oxygen concentrators are much more stylish than oxygen tanks. While oxygen tanks are very oblong, portable oxygen concentrators are compact and sleek looking. You’ll also have access to more accessories like the Inogen One G5 Custom Carrying Case or the GO2 Carryall for the Inogen One G3 which completely conceals the concentrator.
They’re More Affordable for Long-Term Care
Potentially the most controversial topic surrounding supplemental oxygen is its cost. On one hand, patients need a device that can meet their needs consistently and reliably. On the other hand, they don’t want to break the bank doing it.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
While at first glance, portable oxygen concentrators may seem like they’re the most expensive option, they’re actually far more affordable for long-term oxygen therapy. For example, if you spend $2,000 on an oxygen concentrator that lasts an average of 5 years, that’s just over a dollar a day. What’s more, most POCs come with a 3-year warranty at the very least meaning you’ll have an extra safety net if there happens to be a defect with your unit.

Ultimately, when you invest in a more cost-effective long-term solution for your oxygen needs, you’ll have more money to spend on other things such as a night out with your friends. Since financial struggles are among the top triggers of stress and anxiety, it’s best to always create a long-term financial plan rather than choosing the option that’s the most convenient at the time.
Conclusion
Being diagnosed with COPD or another chronic respiratory illness should not mean sacrificing time spent with friends and loved ones; if anything, the exact opposite is true. COPD patients should be spending more time on their relationships because they’re proven to reduce stress, boost life expectancy, and improve general well-being.
While there are many things you can do to maintain an active social life with COPD, investing in a portable oxygen concentrator is likely one of the most important. With a portable oxygen concentrator, you’ll have the freedom to go where you want, when you want. And you’ll feel significantly more confident and secure with a high-tech medical-oxygen delivery device at your side.
If you have any questions at all about portable oxygen devices for seniors, don’t hesitate to reach out to our respiratory specialists here at LPT Medical. Start by filling out the contact form at the side of the page and we’ll answer any question you may have.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!