COPD affects more than 11 million people in the US, both men and women alike. However, there are some noticeable differences between how men and women are affected by the disease.
For example, in recent years, significantly more women than men have been diagnosed with COPD. Men and women can also have different COPD symptoms, and gender can even affect how quickly the disease progresses and gets worse.
Other differences show up in the doctor's office, when doctors give different care to men and women with early symptoms of the disease. This results in many women having to wait longer to get tested and diagnosed for COPD.
While these differences don't apply to every man and woman, they play a role in many people's experiences with COPD. That's why, in this post, we're going to explain this gendered phenomenon and shed some light on why it matters.
In the following sections, we'll show you how COPD affects people of opposite sexes differently and take a closer look at where these differences come from. We'll also explain what these differences actually mean for men and women who have—or who are at risk for developing—COPD.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Differences Between COPD in Women and Men
It is possible for just about anyone to get COPD, but the disease does not affect all groups of people equally. This is reflected in the fact that people from different regions, nationalities, and sexes tend to get the disease at different rates.
However, this is not because the disease is fundamentally different in different types of people. Rather, it's because COPD is linked to secondary factors that tend to affect people in certain groups more than others.
In other words, when it comes to gender, COPD is associated with traits that tend to differ between men and women. Some of these differences are rooted in biology, but many of them are instead rooted in lifestyle and behavior.
In general, you can divide these differences into three main categories:
- Differences in risk, or how likely men and women are to develop COPD
- Differences in disease, or how COPD affects men's and women's bodies differently
- Differences in psychological symptoms
Differences in Risk
In general, women seem to have a higher risk of developing COPD than men. There are many potential reasons for this, but hormones and physical traits, like smaller airways in women, likely play a role.
This difference seems to be significant, especially among people who smoke tobacco, which is the number one cause of COPD. Research shows that women who smoke less than men actually tend to experience worse lung function decline.
This means that women who smoke are more likely to develop COPD and other lung diseases. Women are also more likely to develop symptoms of COPD at an earlier age.
Statistics show that about 58 percent of people who have COPD are women, and that women make up a slightly higher percentage—53 percent—of those who die from COPD. When you consider that about 15.5 million people in the US have been diagnosed with the disease, that adds up to about 9 million women and 6.5 million men with COPD.
However, this is a relatively recent phenomenon that is strongly tied to an increase in the number of women who smoke. Before the mid-1950's, it was largely men who smoked tobacco and later developed COPD.
Differences in Disease
A person's biological sex plays a role in how COPD affects their lungs. Because of this, men and women sometimes experience different COPD symptoms, and even differences in the overall severity of their disease.
For instance, COPD seems to progress more quickly in general in women than in men. This means that women with COPD often experience earlier and more severe lung function decline.
As a result, women's symptoms tend to be more severe—sometimes significantly more severe—and also tend to show up earlier in the disease. Women tend to experience worse shortness of breath, more frequent exacerbations, and are also more likely to die from COPD.
Men and women with COPD also tend to experience slightly different types of COPD (e.g. emphysema or chronic bronchitis), which can lead to different symptoms.
Men, for example, are more likely to have COPD dominated by emphysema, which tends to cause more fatigue-related symptoms. Women, on the other hand, tend to have worse chronic bronchitis, which causes more coughing and airway obstruction from mucus.
Additionally, while the death rate for men with COPD has fallen in recent years, the death rate for women has remained the same. While researchers aren't exactly sure why this is, declining smoking rates in men and quicker disease progression in women are the most likely culprits.
Women with COPD are also more likely to experience certain COPD complications like osteoporosis. This is partially due to the fact that osteoporosis is more common in women in general, but worse COPD symptoms in women also play a role.
Differences in Psychological Symptoms
Anxiety and depression are extremely common side effects of COPD. In fact, researchers estimate that up to 40 percent of people with COPD suffer from clinical depression while up to 20% suffer from clinical anxiety.
However, studies show that women with COPD are much more susceptible (PDF link) to these psychological disorders than men. This is likely influenced by a combination of several different factors, including the severity of COPD symptoms and high rates of anxiety and depression in women overall.
For instance, the fact that women experience worse symptoms and disease outcomes than men is enough on its own to explain much of this difference. More severe symptoms would naturally lead to more health-related stress, causing a higher incidence of anxiety and depression in women.
It is also worth noting that women, in general, tend to have significantly higher rates of anxiety and depression across the board. It is likely that the same factors that cause this general predisposition also apply to women with COPD.
Why Does Gender Affect COPD?
As you can see, there are a variety of important differences between how men and women are affected by COPD. However, while the facts and statistics are relatively straightforward, they don't exactly explain why these differences exist.
But before you can understand the reasons, you need to know how people develop COPD in the first place. Once you understand that, it's easier to see why certain groups of people (e.g. women) tend get COPD more often—and more severely—than others.
To put it simply, COPD is a breathing disorder caused by lung damage. It causes two main things to happen: it reduces the lungs' ability to absorb oxygen, and it narrows the airways so less air can flow through the lungs at a time.
This lung damage can be caused by many different things, namely diseases or substances that cause repeated irritation and inflammation in the lungs. For example, smoking, noxious chemicals, and other diseases like asthma can all cause COPD.
So, what does all this have to do with differences between the sexes? It's simple: COPD is caused by physical traits and patterns of behavior. Since men and women have different physical traits and different patterns of behavior, this naturally leads to differences in how likely men and women are to develop COPD.
For instance, in a biological sense, women tend to have smaller airways, which makes them more susceptible to damage. From a lifestyle perspective, however, men are more likely to work in occupations that could expose them to dangerous respiratory toxins.
Because of this, the differences between men and women with COPD are not always 100% consistent or clear cut. And, as men and women's habits and lifestyles change, so does their relative likelihood of developing COPD.
It is also important to realize that men and women do not always receive the same kind of medical care. This is another factor that could account for some of the differences we see between men and women with COPD.
Biological Differences

Men and women have different biological traits that affect their experiences with COPD. As we mentioned earlier, these differences can influence how likely someone is to develop COPD, what symptoms they have, and how quickly the disease progresses.
A person's biological sex influences both their physical traits and important hormones that regulate their health. Both of these factors can influence your likelihood of developing COPD as well as how your body responds to the disease.
The Effect of Airway Size
Studies show that women tend to have smaller airways than men, but not smaller lungs. This is a factor that could make some people more likely to develop COPD than others, and could partially explain why women seem to be more prone to COPD.
First of all, smaller airways could make women more sensitive to respiratory toxins like smoke. Because women have less total airway tissue, each bit of tissue gets exposed to proportionally more toxins when they breathe.
Compare a male smoker and a female smoker, for instance, who both have similarly-sized lungs but differently sized airways. When the man inhales smoke, the smoke will come into contact with a larger amount of airway tissue, since he has larger airways than the woman.
On the other hand, when the woman inhales smoke, the smoke comes into contact with a smaller surface area of tissue overall. However, she still inhales the same amount of smoke and toxins, meaning that the woman's airways are exposed to a higher “dose” of toxins per area than the man's airways.
This could explain part of the difference between men's and women's risks for developing COPD. Since women have smaller airways, they could be more prone to the damaging effects of cigarette smoke and other respiratory irritants.
The Influence of Hormones
Some researchers believe hormone activity could play a major role in how COPD progresses differently in women than in men. Having more estrogen, in particular, could make women's lungs more susceptible to damage from things like air pollution and smoke.
Researchers believe that estrogen worsens oxidative stress in the lungs, which could explain why smoking tends to affect women more severely. Oxidative stress occurs anytime the lungs and airways get inflamed by a respiratory irritant or infection.
Too much oxidative stress can damage the delicate tissue in the lungs, causing permanent scarring over time. COPD makes the lungs particularly sensitive, causing them to experience oxidative stress more frequently and severely.

Researchers have long noticed that women with COPD seem to have more lung scarring than men, and that the scarring tends to happen earlier on in the disease. This is true even for men and women with similar smoking histories who have lived with the disease for the same amount of time.
Because of this, women tend to have worse lung function and respiratory symptoms by the time they are diagnosed with COPD. The disease also progresses faster and causes death sooner in women than in men.
More recent studies have revealed that this effect could be caused by estrogen. Research shows that estrogen can significantly increase oxidative stress in the lungs, and experts believe this could make women more prone to both the risk factors and effects of COPD.
Since women produce more estrogen, their lungs and airways get exposed to extra oxidative stress any time they breathe in a respiratory irritant like smoke. This leads to worse and earlier airway tissue scarring in women with COPD compared to men.
This could also explain why women who smoke seem to experience quicker lung function decline than men. Estrogen could make their lungs more sensitive to respiratory irritants in general, putting women smokers at a higher risk for developing COPD and making women's COPD symptoms worse.
Genetic Diseases and Traits
Certain genetic traits might give some people a higher risk of developing COPD than others. However, while researchers know that genetics play some role in COPD, they still are not sure which genes those are or how they work.
It is certainly possible, for instance, that certain genes could predispose either men or women to develop COPD more easily. This is an ongoing area of COPD research, and more answers are likely to come in the future as researchers continue to untangle the genetic complexities of the disease.
Lifestyle Differences
On average, men and women tend to live different lifestyles, with different hobbies, occupations and household roles. While no man or woman is the same, there are, statistically, certain jobs, habits, and activities that either men or women are more likely to do.
These different lifestyles that men and women tend to choose have a significant effect on how likely they are to get exposed to harmful substances. And, as we know, how much someone is exposed to respiratory toxins is directly related to their likelihood of developing COPD.
Smoking

Cigarette smoking is the number one cause of COPD. As such, it is the most important factor in an individual person's risk for developing COPD.
One of the clearest ways to see this effect is to look at the changing rates of COPD among men and women over the years. In the mid-1900's, the vast majority of people with COPD were men; however, this changed in the late 1900's, as more women than men started to get diagnosed with the disease.
This change might seem strange until you realize that it is directly correlated to a major cultural phenomenon: more and more women started to smoke. Before then, a much larger percentage of smokers were men, and COPD was considered a male-dominated disease.
However, once this new generation of women smokers began to age, more and more cases of COPD began to show up in women. In fact, since 1980, the number of women who die from COPD every year has more than quadrupled in size (PDF link).
This made it clear that COPD wasn't a man's disease, but rather a smoker's disease, instead. Today, there is less of a gap between the percentage of men and women who smoke, and about 18 percent of men and 14 percent of women in the US are smokers.
This is the perfect example of how rates of COPD in a group can reflect lifestyles and habits that people in the group tend to share. After all, COPD used to be considered a “man's disease,” but this was almost entirely due to the fact that most cigarette smokers at the time were men, not any biological factor.
The Snowball Effect of Having Worse COPD Symptoms

People who experience worse COPD symptoms also have a reduced ability to exercise and do activities that require physical strength. This makes them less likely to get enough physical activity and more prone to sedentary lifestyle.
This can create a snowball effect that has significant consequences for both mental and physical health. Since women with COPD generally have worse lung function and symptoms, they are also more likely to succumb to this negative cycle.
The consequences can be serious: studies show that not getting enough exercise can significantly worsen both the physical and psychological symptoms of COPD. Studies on the general population also support the idea that physical activity is a powerful tool for combating anxiety and depression.
For both men and women, COPD and depression have a circular, or “bi-directional” relationship. This means that worse COPD symptoms can lead to depression, and that depression can lead to worse COPD symptoms.
This happens for many reasons that have to do with living a healthy lifestyle in general. People who are depressed are more likely to live unhealthy, sedentary lives, and people who live unhealthy, inactive lifestyles are more likely to be depressed.
For instance, studies show a very strong correlation between COPD patients' lung function and their likelihood of being depressed. Worse lung function leads to worse shortness of breath, which in turn leads to higher rates of depression.
As we've discussed already, women with COPD tend to have worse symptoms and worse lung function than men. Thus, it makes sense that women with COPD are also more likely to suffer from depression.
Worse symptoms leads to less physical activity and fewer opportunities to benefit from the protective psychological effects of exercise. This leads to a generally unhealthy and sedentary lifestyle that speeds up psychological, physical, and lung function decline.
Losing strength and endurance also makes it more difficult, or even impossible, to participate in many kinds of normal activities. As a result, many people with severe COPD start to give up on hobbies and other things they enjoy in life, leading to social isolation and depression.
The snowball effect of worse symptoms, less exercise, and worse health also seems to make women more prone to certain COPD complications. It leads to more frequent lung infections, more frequent exacerbations, and puts women even more at risk for other health conditions like osteoporosis.
Occupation

In general, more men than women work jobs that put them at risk for COPD. These jobs include any occupation that exposes workers to dangerous levels of respiratory irritants such as noxious chemicals, smoke, and dust.
Studies show that the jobs that put you most at risk for COPD include coal mining, hard-rock mining, concrete manufacturing, tunnel work, non-mining industrial work, welding, and construction. As it so happens, the vast majority of employees who work in these occupations are men.
Some studies suggest that particular air pollutants, such as chlorine, silica dust, cement dust, and welding fumes pose a greater risk than others. Overall, researchers estimate that occupational exposure causes up to 21 percent of all COPD cases.
Household Tasks

While men tend to dominate many occupations that cause COPD, there are other hazardous jobs and activities that more women than men tend to do. This includes household tasks like cooking and cleaning, which, despite changing gender norms, are still done more often by women than men.
Many studies have shown that both cooking and cleaning expose your lungs to harmful respiratory irritants. Cooking exposes your lungs to aerosolized oils and other toxic chemicals, while common cleaning chemicals emit noxious fumes that can damage your lungs.
This puts men and women who cook and clean frequently for many years at a significantly higher risk of developing COPD. One study, for example,

Pulmonary hypertension is a serious, chronic disease that affects the heart and the blood vessels in the lungs. Although it is somewhat rare, the disease can result from a large number of health conditions, genetics, or even occur spontaneously.
Unfortunately, most cases of pulmonary hypertension are chronic and incurable. But especially with early diagnosis and proper medical treatment, people with the disease are able to manage the symptoms of pulmonary hypertension and maintain a good quality of life.
In the early stages of the disease, people who have pulmonary hypertension tend to experience fatigue and shortness of breath during physical activity. But symptoms worsen and multiply as the disease progresses.
Life expectancy and treatment options depend mostly on how early the disease was caught and what cause, if any, doctors can find for the disease. In this guide, we will help you better understand pulmonary hypertension, what causes it, and what kind of treatments options are out there to help patients manage the disease.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
What is Pulmonary Hypertension?
Most people have heard the term hypertension, which is the name of a common condition where blood pressure is elevated throughout the body. Pulmonary hypertension is a bit different. It occurs when high blood pressure exists specifically in the blood vessels in lungs.
Pulmonary hypertension is somewhat difficult to define, because it can take so many forms and have so many causes. However, all forms of pulmonary hypertension affect the right ventricle of the heart, which is the chamber that pushes used (oxygen-depleted) blood out of the heart and into the lungs.
High blood pressure in the lungs happens when disease, inflammation, or other factors cause detrimental changes to the blood vessels in your lungs. These blood vessels, called pulmonary arteries, become thicker, stiffer, and the openings inside them get smaller.
These structural changes to the pulmonary arteries block blood flow and make it harder for your heart to continue pumping blood through your lungs. Thickened artery walls and inflammation make the inner space where blood flows narrower, causing hypertension and increasing the risk of blood clots.

Also, unlike healthy, flexible blood vessels, the thickened, stiffened artery walls found in people with pulmonary hypertension prevent the arteries from expanding to accommodate increased blood flow when needed. Basically, these changes in the pulmonary arteries work together to make the lungs a choke point for blood flow, raising blood pressure in the area and forcing your heart to work harder to push blood into your lungs.
Pulmonary hypertension is officially diagnosed by measuring blood pressure in the pulmonary arteries. If blood pressure in a lungs is greater than 25mm/Hg while at rest (or greater than 30 mm/Hg when exercising), the patient is said to have pulmonary hypertension. Healthy individuals have a resting pulmonary artery pressure between 8 and 20 mm/Hg.
How Pulmonary Hypertension Affects Your Body
To understand how pulmonary hypertension affects your body, you first have to understand the basics of how blood circulates through the heart and lungs. The following diagram of the heart and pulmonary arteries should help you follow along.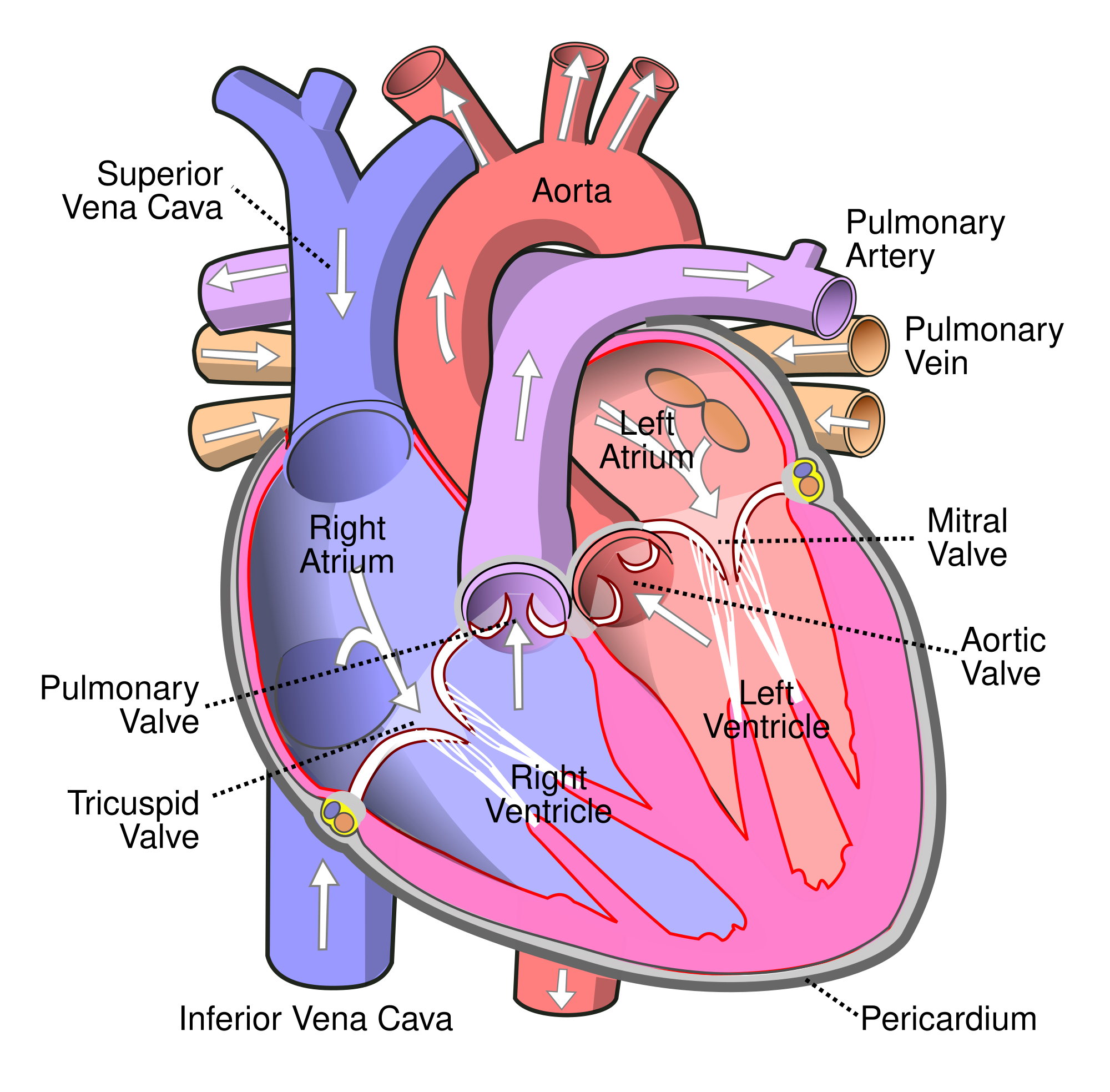
The heart is divided into two main sides: right and left. The heart is further divided from top to bottom, to make four heart chambers total.
The top two heart chambers are called ventricles, and they receive blood from other parts of the body. The bottom chambers are called ventricles, and they pump blood out to the rest of the body.
Pulmonary hypertension mainly effects the right ventricle (bottom right chamber) of the heart, which is responsible for pumping blood out of the heart and into the lungs. When the blood vessels in the lungs become stiff, narrow, or blocked, it creates back-pressure when the right ventricle tries to pump blood into the pulmonary arteries.
As a result, the blood pressure in the lungs goes up and the heart's right ventricle has to work harder and harder to push blood through the constricted arteries. Eventually, the resistance causes the right ventricle to enlarge and become weaker.
Over time, pulmonary hypertension causes the heart to continue to enlarge and get weaker and weaker, until it eventually is unable to pump blood into the lungs at all. The resulting heart failure is a major cause of death for people who are diagnosed with pulmonary hypertension.
This is the general mechanism by which pulmonary hypertension occurs and affects the body, but it is not the only one. There are several other forms of pulmonary hypertension that look slightly different and affect the body in different ways, which we'll discuss later in the section on causes of pulmonary hypertension.
Key Facts about Pulmonary Hypertension
Pulmonary hypertension is a rare and varied disease that has many different causes and can present itself in many different ways. In fact, there are five different groups of pulmonary hypertension, and within each of these groups there are multiple diseases and conditions that can cause a particular type of pulmonary hypertension.
It's estimated that only 15-50 people out of every million adults develops the disease, but the incidence is much higher for people in at-risk groups (including people with associated diseases like HIV or systemic sclerosis).
Idiopathic pulmonary hypertension (disease with no known cause) makes up more than 40% of total cases of pulmonary arterial hypertension. It is also, for unknown reasons, anywhere between 2 and 5 times more common in women than men, and is usually diagnosed around the age of 45 years.
In healthy people, the blood pressure in the lungs is significantly lower than the blood pressure throughout the whole-body, at about 8-20 mm/Hg. Unlike regular blood pressure measurement, testing the blood pressure in the pulmonary arteries requires special, more invasive techniques.
To test pulmonary artery pressure, doctors have to perform a procedure called right heart catheterization. It requires going under anesthesia and having a flexible tube, or catheter, inserted into a major blood vessel in your neck or groin.
The catheter is threaded up through the right side of the heart and into the pulmonary arteries. There it allows doctors to test the blood vessels in the lungs for high blood pressure and learn more about how efficiently your heart is able to circulate blood through your body. This is the most accurate way to test for pulmonary hypertension.
Pulmonary Hypertension Symptoms
In the early stages of the disease, many people who have pulmonary hypertension don't experience any major symptoms. It's one of the things that makes pulmonary hypertension so difficult to spot and diagnose.
When symptoms do show up, they usual begin slowly, starting with shortness of breath during physical activity. You might also notice minor chest pain, a racing pulse, and that you feel easily fatigued from minor physical activities.

Symptoms worsen slowly over time as the disease progresses and your body is unable to keep your blood oxygen levels up. You'll notice that even light activity can make you feel short of breath and experience light-headedness or even fainting. In the later stages, symptoms of severely low blood oxygen, such as a bluish tint to the skin and lips, and ankle or leg swelling (edema) can occur.
Here are some of the most common early symptoms of pulmonary hypertension:
- Shortness of breath (especially after light or moderate physical activity)
- Dizziness
- Racing pulse
- Heart palpitations
- Fatigue
- Reduced appetite
- Chest pain or pressure
- Pain in the upper-right side of the abdomen
Here are some of the most common later-stage symptoms of pulmonary hypertension:
- Feeling light-headed and dizzy
- Fainting
- Weakness
- Distended abdomen
- Bluish tint to skin and lips
- Swelling of the ankles and legs (edema)
Because pulmonary hypertension is a progressive, incurable disease, early detection is key. The longer it takes to get an accurate diagnosis, the worse the disease will become.
Many people, unfortunately, ignore or brush off the mild, early symptoms of pulmonary hypertension. Many others do go to see their doctor but are misdiagnosed with asthma or another type of lung disease.
The earlier you catch pulmonary hypertension, the more likely you are to be able to slow down it's progression with treatment and medication. That's why you should never ignore symptoms like breathlessness and fatigue, especially if you have a family history or other risk factors for pulmonary hypertension.
Causes of Pulmonary Hypertension
Pulmonary hypertension is a complex disease that affects the entire body and has many known causes. In some cases doctors are unable to find a cause, but in many cases pulmonary hypertension results from another known disease or health condition.
Different forms of hypertension affect the body in different ways, and what kind of treatment will be effective largely depends on what is causing the disease. That's why health researchers have divided up pulmonary hypertension into five main categories, each containing similar types of hypertension that are treated in similar ways.
The following sections describe the differences between all five categories of pulmonary hypertension and discusses the most common causes and conditions that lead to them.
Pulmonary Arterial Hypertension
This is a general form of pulmonary hypertension that includes forms caused by genetic mutations, viral infections, drug use, and certain medical conditions like heart and liver disease. It also includes forms of pulmonary hypertension that have no known cause (known as idiopathic pulmonary hypertension).
Pulmonary arterial hypertension occurs when the pulmonary arteries narrow and stiffen, causing high blood pressure in the lungs. This forces the heart's right ventricle to work harder, eventually causing it to enlarge and ultimately results in right-side heart failure.
Causes of Pulmonary Arterial Hypertension
- Heart Disease (including congenital heart diseases)
- Viral Infections
- Genetic Mutations
- Drug Use (especially amphetamines like cocaine or methamphetamine)
- Autoimmune Disease (including lupus, scleroderma, and rheumatoid arthritis)
- Chronic Liver Diseases (such as cirrhosis)
- Chronic lung diseases (such as emphysema, or pulmonary fibrosis)
- Unknown Cause (known as Idiopathic Pulmonary Arterial Hypertension)
Pulmonary Venous Hypertension
Pulmonary venous hypertension is different from pulmonary arterial hypertension in that originates from the left side of the heart. In this form of pulmonary hypertension, the left atrium (the upper-left chamber in the heart) has difficulty taking oxygenated blood out from the lungs.
As a result, excess blood pools up in the lungs because it cannot flow out of them efficiently. This creates back-pressure and makes it more difficult for the right ventricle to pump blood into the lungs, which results in pulmonary hypertension.
Pulmonary venous hypertension is often caused by problems and diseases that affect the left side of the heart, including connective tissue diseases that causes the heart chambers to narrow. It can also be caused by abnormalities in other parts of the heart, including problems that interfere with the ability of the heart valves to open and close correctly.
Causes of Pulmonary Venous Hypertension
- Left-sided Heart Disease (This is the most common cause of pulmonary hypertension)
- Left-ventricle Heart Failure
Hypoxic Pulmonary Hypertension

This category is referred to as hypoxic pulmonary hypertension because all of the diseases in the group share one major characteristic: hypoxia. The term hypoxia refers to lack of oxygen, and the condition occurs when blood oxygen levels are so low that all of the body's tissues are unable to get enough oxygen.
Lung diseases like interstitial lung disease or COPD, as well as sleep-related breathing disorders like sleep apnea, deprive the lungs of oxygen which can lead to hypoxic pulmonary hypertension. In these conditions, the lungs are unable to absorb enough oxygen, causing hypoxia in the lungs. This, in turn, causes many the blood vessels in the lungs to constrict, raising blood pressure in the pulmonary arteries.
Causes of Hypoxic Pulmonary Hypertension
- Chronic Obstructive Pulmonary Disease (COPD)
- Lung Diseases like Pulmonary Fibrosis
- Sleep-related breathing disorders like sleep apnea
- Exposure to high altitudes over long periods combined with other risk factors for pulmonary hypertension
Thromboembolic Pulmonary Hypertension
This type of pulmonary hypertension is caused by repeated instances of blood clots in the pulmonary arteries. It happens when blood clots get stuck in the small arteries in the lungs, restricting or blocking blood from flowing through.
In healthy individuals, blood clots usually don't get stuck in the lungs, or if they do, they resolve themselves without problem. But in rare cases where they don't dissolve or break up on their own, blood clots in the pulmonary arteries can result in pulmonary hypertension and right ventricle heart enlargement and failure.

Causes of Thromboembolic Pulmonary Hypertension
- Pulmonary emboli (chronic blood clots in the lungs)
- Medical conditions and procedures that carry a high risk of causing blood clots (This could include diseases that cause chronic inflammation, having your spleen removed, or having an infected pacemaker wire.)
Miscellaneous Pulmonary Hypertension
Miscellaneous pulmonary hypertension is basically a catch-all category for various forms of hypertension that don't fit into the other four categories. Most of the types of pulmonary hypertension in this category are caused by or related to other diseases and conditions, but the reason for the relationship is not well understood.
For example, certain metabolic disorders, connective tissue diseases, and HIV can lead to pulmonary hypertension, but doctors and researchers don't know exactly why this happens.
Causes of Miscellaneous Pulmonary Hypertension
-
Blood Diseases: Certain blood diseases, such as bone marrow disease, are associated with pulmonary hypertension. Doctors postulate that, because these blood diseases cause the body to produce excess red blood cells, they can contribute to pulmonary hypertension.
-
Systemic Disorders: Some systemic disorders cause a condition called vasculitis, a kind of inflammation that affects blood vessels throughout the body. Over time this can narrow blood vessels and restrict blood flow to vital organs and tissues, including the lungs, which can result in pulmonary hypertension.
-
Tumors: Certain conditions cause tumors to develop in the lungs or chest. These tumors can press against the pulmonary arteries, restricting blood flow and causing pulmonary hypertension.
- Metabolic Disorders: Some metabolic disorders, including thyroid disorders, Gaucher disease, and glycogen storage disease, can result in pulmonary hypertension.
Eisenmenger Syndrome: A Special Case of Pulmonary Hypertension
A type of congenital heart disease, Eisenmenger syndrome occurs most often when you have a large hole in the wall that separates either the two upper chambers in the heart (the left and right atria) or the two lower chambers of the heart (the left and right ventricle). A hole between the lower chambers is called a ventral septal defect.
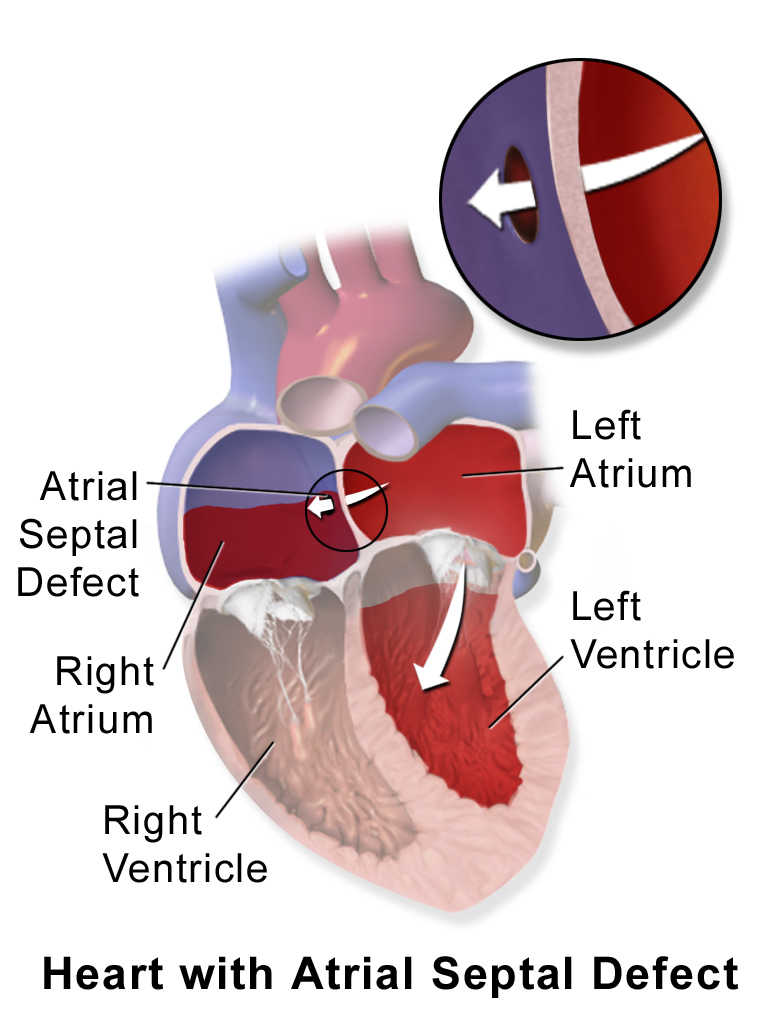
Because of this heart defect, blood cannot circulate normally, and blood in the two heart chambers gets mixed. This is a serious problem because the left ventricle is full of oxygen-rich blood that's ready to be pumped throughout the body, while the right ventricle holds oxygen-depleted blood that needs to be pumped through the lungs to get oxygenated.
This results in oxygen-poor blood being pumped through the body and oxygen-rich blood being needlessly pumped back through the lungs. This increases the volume of blood in the pulmonary arteries, which increases back-pressure, causes pulmonary hypertension, and eventually enlarges the lower heart chambers.
Complications with Pulmonary Hypertension
Pulmonary hypertension can lead to a variety of serious heart and lung conditions. Most of these complications occur later on as the disease progresses and puts increasing pressure on the right side of the heart.
Right-sided Heart Enlargement & Failure

Pulmonary hypertension causes back-pressure in the heart that causes it to have to work harder and harder to pump blood through the constricted pulmonary arteries. In order to compensate for the increased workload, the walls of the heart chamber thicken and the right ventricle expands and thickens (right ventral hypertrophy) so it can hold and pump more blood at a time.
However, these changes are only a temporary fix, and eventually the heart muscles weaken from the strain. Eventually, the right ventricle becomes so enlarged and weak that it fails completely, leading to right-sided heart failure and often death.
Blood Clots
In healthy people, small blood clots are usually able to pass through the lungs without causing any major problems. However, if you have pulmonary hypertension, the pulmonary arteries are narrowed, making blood clots much more likely to get caught and block blood flow in the tiny vessels.
Arrhythmia
Pulmonary hypertension causes your heart to enlarge and disrupts blood flow through the separate chambers. This can lead to irregular heartbeats, or arrhythmias, which can in some cases be fatal.
Arrhythmia can cause other dangerous and uncomfortable symptoms including faintness, dizziness, heart palpitations, and even fainting.
Bleeding
Bleeding into the lungs and coughing up blood is another serious, potentially fatal complication that can occur with pulmonary hypertension.
Risk Factors for Pulmonary Hypertension

Because the disease is so wide in scope, there are many potential risk factors for pulmonary hypertension. Along with the specific factors related to genetics, lifestyle, and medications, having any of the diseases or conditions known to cause pulmonary hypertension is a significant risk factor.
These are some of the risk factors that may increase your chances for developing pulmonary hypertension:
- A family history of pulmonary hypertension
- Being overweight
- Use of appetite-suppressant medications
- Illegal drug use (especially stimulants like cocaine and methamphetamine)
- Prolonged exposure to high altitudes
- Having any of the diseases or conditions that can cause pulmonary hypertension (listed in the section on pulmonary hypertension causes)
Treatments for Pulmonary Hypertension

Because many people with early-stage pulmonary hypertension only have mild symptoms, or even no symptoms at all, many people live with the disease for years before getting diagnosed. That's why it's so important to be able to recognize the early symptoms and get evaluated by a doctor if you notice them, especially if you're at a higher risk of getting the disease.
If the disease is caught early, proper treatment can delay the worsening of pulmonary hypertension and keep more serious symptoms at bay. However, no matter how long your disease has progressed, medication and lifestyle changes can alleviate symptoms and make a huge difference in your overall health and quality of life.
When you're diagnosed with pulmonary hypertension, the first thing your doctor will do is try to determine what caused you to get the disease in the first place. Different causes require different treatments, and you doctor will likely screen you for other diseases associated with pulmonary hypertension while searching for a cause.
If your doctor does find any underlying diseases or conditions that could be the cause of your pulmonary hypertension, your doctor will focus on treating those first. After those other conditions are treated and stabilized, your doctor will focus on medications and interventions to treat the pulmonary hypertension itself.
There are a variety of medicines, surgical procedures, and other treatments like supplemental oxygen therapy to help patients with pulmonary hypertension live longer, healthier, and fuller lives. Your doctor will work with you to create a personalized treatment plan and recommend the best course of action based on your unique case and medical history.
Lifestyle Changes
While lifestyle changes won't necessarily slow down the progression of pulmonary hypertension, they can improve your health and overall quality of life. Healthy habits can help you fight symptoms like breathlessness and fatigue and allow you to stay active in the later stages of the disease.
Stay Well-Rested

Getting enough sleep is an important part of any healthy lifestyle, but it's particularly important if you have pulmonary hypertension. The disease is taxing on your body and can make you feel tired and worn out, so make sure you take time to rest when you feel fatigued.
Quit Smoking
Along with increasing your risk for pulmonary hypertension, smoking causes further damage to your lungs and worsens symptoms of the disease. Quitting can be very hard, but there are many different programs, medications, and hot-lines available to help you if you need it.
Talk to your doctor about smoking cessation resources in your area or to get a prescription for a quit smoking medication. You can also visit the CDC's website for more information and support.
Eat Better
A healthy diet is key for good cardiovascular health
If you have COPD, then you know that getting sick can wreak havoc on your daily life. Even common illnesses like the cold or flu can significantly increase your COPD symptoms and, in serious cases, even land you in the hospital.
That's why many doctors see the prevention of illnesses and infections as a primary treatment goal for COPD. Even the most minor illnesses can lead to exacerbations, which can be life-threatening or cause permanent worsening of lung function and COPD symptoms.
In this article, we'll show you how to avoid illnesses like the flu, pneumonia and the common cold if you have COPD. That way, your body can focus all of its energy and resources on keeping you and your lungs as healthy and strong as possible.
First, we'll explain how common viruses like the flu and common cold spread and how they can affect your COPD. Next, we'll introduce you to a variety of practical tips and techniques you can use to stay healthy and boost your immune system during the cold and flu season this year.
Even though COPD puts you more at risk for getting sick, there are many simple actions you can take in your daily life to stave off illnesses and infections. If you learn how to protect yourself and how to put those steps into action, you can significantly reduce your likelihood of getting sick and making your COPD worse.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Why Common Illnesses Are More Serious for COPD Patients

People with COPD have weakened immune systems, which makes them more likely to get sick if they get exposed to viruses or bacteria. It also makes COPD patients more likely to get secondary illnesses and infections, and more likely to experience serious complications when they get sick.
For instance, if you have COPD, getting a common cold makes you thirty times more likely to experience an exacerbation, which can cause life-threatening symptoms and hospitalization. Even when they don't cause exacerbations, illnesses take precious energy and resources away from your lungs and make it more difficult to breathe.
If you have COPD, any kind of illness or infection can weaken your lungs and cause you to have an acute exacerbation. However, illnesses that affect your respiratory system, like the flu, common cold, and pneumonia, are often the most threatening because of their symptoms and how quickly they can get worse.
Let's go through each of these sicknesses to better understand how they work and how they affect people with COPD.
The Common Cold
The common cold is caused by a virus, or, more precisely, a group of viruses that are constantly changing and adapting. Common cold viruses (known as Rhinoviruses) generally affect your nose and throat, causing a variety of respiratory symptoms like coughing, sneezing, and excess mucus production that make COPD symptoms much worse.
There are more than 200 types of cold viruses and they are all tricky and evasive. Rhinoviruses evolve very quickly, which is one of the reasons why the common cold is so difficult to treat and prevent. By the time researchers can identify and analyze a particular strain of cold virus, there's a completely new set of rhinoviruses getting passed around.
Because of this, there are no targeted vaccines or treatments that are effective for the common cold. Instead, simple prevention through proper hygeine is still the most effective way to protect yourself from contracting a rhinovirus.
Most people start showing cold symptoms 2-3 days after being exposed to a rhinovirus. Most common colds only last about a week to ten days, but they can sometimes last longer or leave lingering symptoms, like a persistent cough.
Symptoms of the Common Cold:
- Coughing
- Sneezing
- Sore throat
- General malaise (not feeling well)
- Runny nose or congestion
- Thickened mucus
- Mild headache
- Mild body aches
- Low-grade fever
If you think that you are coming down with a cold, consult your COPD treatment plan to figure out what to do next. Your doctor might recommend increasing how frequently you take certain medications or starting a course of corticosteroids or antibiotics to prevent secondary infections.
It's a good idea to call your doctor whenever you start to feel sick, and to check back in if your symptoms don't improve in a few days. If your symptoms start to get significantly worse, or you are experiencing an acute exacerbation, don't hesitate to talk to your doctor or seek medical attention.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
The Flu

Influenza (also known as the flu) comes with many of the same symptoms as the common cold. However, unlike the common cold, which is generally very mild, the flu can make you severely sick. It is particularly dangerous for the young, old, and people with chronic diseases to get the flu, as it has the potential to cause serious complications and even death.
The flu is also a common cause of pneumonia and a variety of other secondary infections, including sinus infections and ear infections. People with COPD are particularly likely to develop pneumonia if they get the flu, which is why disease prevention is so important for COPD patients.
Most healthy adults who get the flu are able to recover relatively quickly and don't experience any serious complications. However, the flu can be much more serious and even deadly for people with chronic diseases like COPD, diabetes, and asthma. People over the age of 65 are also at a much higher risk of serious complications from the flu.
Telling the flu apart from the common cold can be tricky, which is why you should always call your doctor if you feel sick during the flu season. Your doctor can give you a test to see if you have the flu and determine how to treat you based on the results.
Common Symptoms of the Flu:
- Fever
- Chills
- Cough
- Runny nose or congestion
- Headaches
- Body aches
- Fatigue
- Sore throat
During flu season, you should take extra precautions and monitor your health more carefully. Take any respiratory or flu-like symptoms very seriously, and call your doctor earlier when you start feeling sick.
If you think you are starting to get the flu, you should follow the appropriate treatment plan recommended by your doctor and talk to your doctor immediately. There are certain medications, like Tamiflu, that can significantly reduce the length and severity of the flu if taken early enough.
Pneumonia
Another particularly dangerous illness for people with COPD is Pneumonia, a type of respiratory infection that causes inflammation in the air sacs in your lungs. Pneumonia happens when the air sacs (or alveoli) in your lungs fill up with fluid, leading to symptoms like coughing, fever, and breathing difficulties.
Pneumonia is more likely than the cold or flu to cause serious complications, especially for people with COPD. In severe cases, pneumonia can cause lung abscesses, fluid build-up in the lungs, respiratory failure, and death.
Pneumonia can be caused by viruses, bacteria, and even fungi, and most commonly occurs as a result of respiratory infections like the flu. Pneumonia is most common in people over the age of 65 and people with chronic respiratory conditions.
When you have COPD and experience respiratory symptoms on a regular basis, it can sometimes be difficult to tell the difference between a minor COPD flare-up and signs that you're getting sick. That's why it's important to remember and recognize the symptoms of the common cold, flu, and pneumonia.
Pneumonia tends to come with symptoms that are similar to the common cold or regular COPD symptoms. It's common to feel chest tightness, shortness of breath, and experience thicker, darker mucus in your airways.
Common Symptoms of Pneumonia:
- High fever
- Chills
- Worsened chest pain and tightness
- Headaches
- Body aches
- Fatigue
- Shaking
- Shortness of breath
- Rapid breathing
- Thick, dark-colored mucus
If you have cold or flu symptoms that last more than a week or if you believe you might have pneumonia, you need to call your doctor immediately. Pneumonia can often be diagnosed through a simple examination, chest x-ray, or by testing sputum that you cough up from your lungs.
If you have pneumonia, your doctor will determine whether it's caused by a virus, bacteria, or fungus, and start you on the appropriate medication. It's important to get proper medical treatment immediately and as early as possible in order to prevent serious and life-threatening complications.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
How to Avoid Getting Sick

Now that you know how dangerous even mild illnesses can be, you're probably eager to know what you can do to protect yourself from getting sick. Fortunately, there's plenty you can do to reduce your chances of catching contagious illnesses, but unfortunately, no matter how careful you are, it's no guarantee.
Most respiratory illnesses, including the common cold and flu, are very contagious and can spread in many ways. You can catch a cold or flu simply by breathing in the virus from the air or from touching a contaminated doorknob.
That's why it's so important to know what to watch out for and how to protect yourself from the viruses and bacteria in your environment. Read ahead to learn how proper hygiene, vaccination, and other precautions you can take in public can reduce your chances of exposure to disease-causing germs lower your chances of getting sick to a minimum.
Wash Your Hands

Most of the things you touch, including food, people, animals, plants, and anything outdoors is a potential source of germs that could make you sick. That doesn't mean you should be afraid of everything, but it highlights why it's so important to wash your hands often.
Hand-washing is probably the most effective way to protect yourself from illnesses and infections. That's why the CDC calls it a “do-it-yourself vaccine” and uses the slogan, “Clean Hands Save Lives.”
Hand washing works because soap and water is generally enough to remove the vast majority of harmful viruses and bacteria that your hands pick up throughout the day. Washing your hands will not only keep you healthy, but it helps protect other people from getting sick as well.
How and When to Wash Your Hands

In general, you should wash your hands anytime they come into contact with anything that could harbor harmful bacteria or viruses. You should scrub your hands immediately after touching anything visibly dirty or unclean, and anytime you arrive home from an outing.
While you should never wash your hands obsessively, you should wash them often, especially when you're out in public. Here is a guide to some situations in which you should always wash your hands:
-
When cooking: It's very important to always wash your hands frequently while prepping and cooking foods, especially after touching raw or cooked meats. Washing your hands in-between handling different ingredients and before you eat will prevent food cross-contamination and exposing yourself to harmful germs.
-
After visiting a public place: Wash your hands whenever you get home from an outing. You risk exposure to harmful bacteria and viruses anytime you go in public or around other people; this includes going to the grocery store, a friend's house, the park, library, movie theater, or a restaurant.
-
After using the bathroom: Always wash your hands thoroughly after using the bathroom, even in your own home. If you're in a public place, use a paper towel instead of your bare hands to touch the doorknob on your way out. You should also always wash your hands after changing a diaper.
-
After touching surfaces in public: Anything that many people use or touch can potentially harbor dangerous viruses and bacteria. You should always wash your hands after touching public doorknobs, pens, counters, sink faucets, credit card machines, and more. You can also bring sanitizing wipes with you to wipe down certain items, like public phones or the handle on your grocery cart, before you use them.
-
After shaking hands: Even if you are careful to wash your hands, the people you meet on a daily basis might not be so hygienic. Always wash your hands after meet-and-greets and anytime you touch another person's hand.
-
After cleaning or handling trash: You're bound to get some nasty dirt and germs on your hands whenever you clean, gather up garbage around the house, or take out the trash. You should wash your hands after anytime you clean your house or touch any trash or garbage receptacles.
-
When visiting a doctor's office or hospital: Contagious illnesses and infections are ever-present in hospitals and doctor's offices, which make them risky places for patients with compromised immune systems. Take care not to touch public handrails, arm rests, counters, and pens if possible, and wash your hands immediately after if you do. Bring your own pen to sign yourself in instead of using the public pen provided at the front desk.
-
Before touching a newborn: Newborn babies don't have fully developed immune systems yet, and are thus especially susceptible to viruses and bacteria that you might have on your hands.
- Before you eat: Whenever you eat, you're using your hands or utensils to put things directly into your mouth. This puts you at risk of transferring germs from your hands or utensils to your food, then putting it into your body where it could make you sick. Whether you have COPD or not, everyone should wash their hands right before eating, without exception. Make it a habit in your household to have everyone wash up before meals.
How to Practice Proper Hand-Washing Technique

While hand-washing is a very effective way to prevent disease, it only works if you do it right. Unfortunately, most people don't know how to wash their hands properly and do a lazy or inadequate job of cleaning their hands.
How to Wash Your Hands Properly
- Wet: Run your hands under clean, running water from a faucet.
- Lather: Turn off the water and put soap on your hands. Then rub your hands together until it forms a frothy lather.
- Scrub: Use the lather to scrub your hands from top to bottom for about twenty seconds. Scrub your hands thoroughly, including your fingers, palms, wrists, and the backs of your hands. Don't forget to scrub between your fingers and under your fingernails. Use a nail brush if your hands are very dirty or there is dirt caught under your nails.
- Rinse: Turn on the tap again and rinse your hands under the clean, running water until all the soap is gone.
- Dry: Use a clean washcloth, towel, or paper towel to pat your hands dry. If you don't have a towel, shake the excess water off your hands and let them air dry.
Stay Away from Anti-Bacterial Soaps At All Costs
 |
| Image courtesy of Mike Mozart. |
As a final piece of hand-washing advice, you should stay away from antibacterial and antimicrobial soaps at all costs. They're not just ineffective, but potentially dangerous for both individual people and the environment.
While the term “anti-bacterial” in the name might make you think they work better, antibacterial soaps are actually less healthy for you than plain soaps that don't contain antibiotics. They don't clean your hands any better than regular soap and water, and they don't make you any less likely to get sick.
In fact, according to the FDA, antibacterial soaps don't offer any extra protection against illnesses and might even “give people a false sense of security.” Antibacterial soaps also encourage the growth of antibiotic-resistant bacteria, a problem that has grown along with popularity of antibacterial soaps.
Because of this, you should always check the label on any soap you buy and reject anything that says “antibacterial,” “antimicrobial,” or has a “drug facts” section on the label. Instead, opt for regular, plain soap and warm water whenever you wash your hands.
Don't Touch Your Face

While it helps to wash your hands every so often while you're out and about in a public place, there's no need to go overboard. You don't want to be a total germaphobe, and it's not possible or practical to wash your hands every single time you touch a doorknob or another potentially-contaminated surface.
Instead, simply keep your hands away from your face in-between hand washings. This will prevent you from accidentally inoculating yourself with whatever viruses and other pathogens your hands have picked up.
Germs on the surface of your skin can't infect you unless they find another way in; your tough skin is an effective barrier for keeping viruses and bacteria out of your body. But if you touch your face, germs on your hands can find their way into your eyes, nose, or mouth, where they can enter and infect your body.
But as long as you keep your hands away from your face, you're not likely to get sick from any pathogens your hands pick up. Just remember not to rub your eyes or nose, chew your nails, or let your fingers touch your tongue or lips.
Face-touching is a common thing that many people do without even realizing it, so it might take some concentrated effort to break the habit. You'll have to keep it in mind when you go out and get used to catching yourself in the act in order to reprogram absent-minded behaviors, like rubbing your face, that put you at risk.

Start the new habit at home and start training yourself to keep your hands at your sides and avoid touching your face unnecessarily. If you need to touch your eyes, blow your nose, or touch your face for any other reason, make sure you remember to wash your hands or use hand sanitizer first.
The other way that germs get into your body is through wounds and broken skin, which is why it's important to wash and cover any scratches, scrapes, burns, or other lesions you have. Otherwise, you could get a serious infection that weakens your immune system and causes you to get sick.
Use Hand Sanitizer
Hand sanitizer is a great option when you need to wash your hands but don't have access to a bathroom or sink. Although not quite as effective as hand-washing, hand sanitizers can kill the vast majority of viruses and bacteria on your skin and can be indispensable in a pinch when you're out in a public place.
But you have to look out for quality if you want a hand sanitizer that's safe and effective. Alcohol is the active ingredient in sanitizers that kills pathogens, but some don't contain a high enough percentage to reliably kill the bulk of the germs on your skin.
Always check the label and make sure that any hand sanitizer you buy contains at least 60 percent alcohol. Any less is hardly better than using plain water, and can even be dangerous for offering false protection.
You can keep a small bottle of hand sanitizer in your purse or pocket for anytime you need a quick, easy way to get rid of germs on your hands. It's useful for when you're out shopping or when you touch surfaces in high-traffic areas like doorknobs, hand rails, and credit card machines.
It is possible to have too much of a good thing, however, and you should only use hand sanitizer when you really need it. Excess hand-washing and hand-sanitizer use is bad for your skin, and using sanitizer too often can even breed super-strong, resistant bacteria. In moderation, hand sanitizer can keep you healthy, but too much can hurt your immune system and actually make you more likely to get sick.
Avoid Large Crowds

Lots of fun events and activities involve being around hundreds or thousands of other people. This includes most public events like parades, conventions, and holiday festivals. Unfortunately, cramming lots of people into small spaces comes with a lot of disease risks, which makes these situations especially dangerous for people with COPD.
While crowded, public events can be fun to attend, patients with compromised immune systems should avoid them during cold and flu season. No matter how many precautions you take, contagious illnesses can spread through crowds like wildfire, and the risk of picking up harmful germs from common areas increases significantly.
Here are some examples of crowded places you should try to stay away from during cold and flu season:
- Large festivals and events
- Sporting events
- Concert halls
- Convention centers and other entertainment venues
- Places with lots of children, including preschools, grade schools, and day cares
- Busy shopping malls
- Busy college campuses

If you can, skip out on busy winter festivals and try to attend public events during other times of the year, when the risk for contagious illnesses is not so high. If you must go to a crowded event, take every precaution you can to reduce your exposure to public surfaces and airborne germs.
Here are some tips for protecting yourself in crowded places:
- Wear a surgical mask or a CDC-certifie
%20(1).png)
Around 70 million people in the United States suffer from some form of sleep disorder such as narcolepsy, insomnia, or obstructive sleep apnea (OSA). These conditions can appear anytime during our lives and they have a significant impact on our general health and well-being.
Unfortunately, there are many obstacles that prevent people from receiving the treatment they need for sleep disorders. Chief among them is the fact that many people don’t even realize they have a problem in the first place. Symptoms such as daytime sleepiness, restlessness, or difficulty concentrating are often shrugged off as an inevitable part of life.
Another obstacle preventing sleep disorder patients from getting the help they need is confusion about their disease and the treatment options that are available to them. People hear terms like CPAP, BiPAP, EPAP, or APAP, but they never actually receive a simple explanation of what these terms mean and how they relate to each other.
In this post, we’re going to clarify any confusion about these terms as well as how they pertain to other types of respiratory therapy like supplemental oxygen. Remember to check in with your doctor if you have any questions or if you are thinking of making any changes to your treatment plan.
What is Obstructive Sleep Apnea (OSA)?
There are several types of sleep apnea, but one of the most common is obstructive sleep apnea. OSA occurs when the muscles in your throat relax intermittently at night causing you to stop breathing and lose sleep. It’s estimated that about 22 million Americans have some form of sleep apnea.
.jpg)
Obstructive sleep apnea is notoriously difficult to self-diagnose because the patient will likely have no recollection of what caused them to lose sleep or wake up frequently at night. In fact, many undiagnosed OSA patients believe that they get great sleep each night. This is why it’s important to speak with your doctor about having a sleep study done so that a medical specialist can examine your sleep patterns and determine if OSA is present.
A sleep study (polysomnography) is a non-invasive exam where you will stay in a sleep center overnight. During this study, electrodes will be placed on your head that measure brain activity, you will have a pulse oximeter attached to your finger which measures blood oxygen levels, and a belt will be wrapped around your chest to monitor breathing.
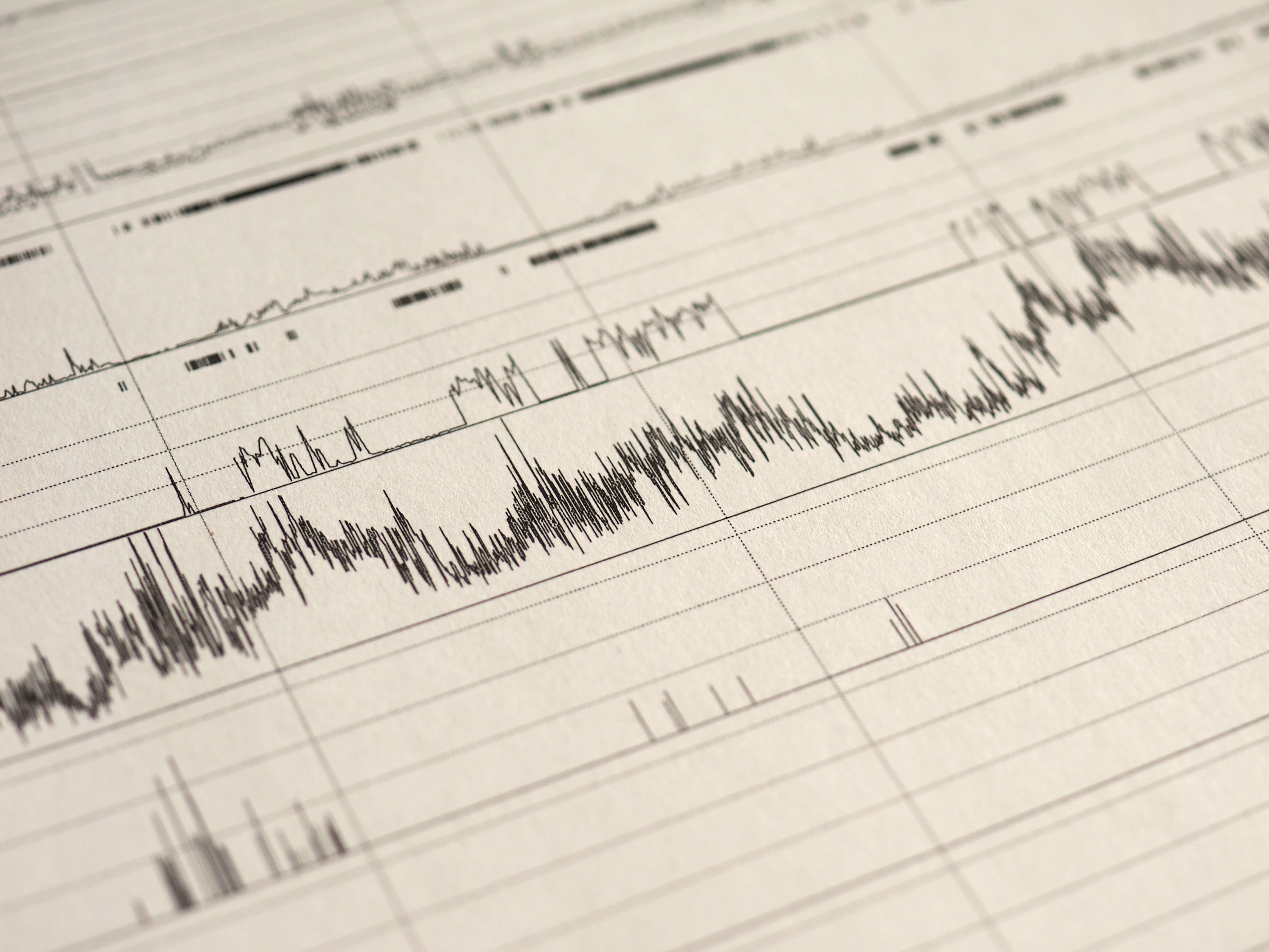
This is one of the most effective ways for a health professional to diagnose OSA because it will show them exactly what’s going on in your body during sleep. For example, if your breathing is interrupted, your blood oxygen levels will likely drop and you’ll wake up. Occasional sleep interruptions are normal, but if it’s happening frequently throughout the night there is a more serious underlying issue at play. According to worldsleepday.org, patients with severe sleep apnea may wake up more than 30 timers each hour.
Why is it Important to Treat Sleep Disorders?
For many people, the term “sleep disorder” doesn’t bring about a huge amount of urgency. You may be thinking that a sleep disorder can be cured with an extra cup of coffee in the morning or an energy drink for lunch, but the issues extend far beyond a little extra drowsiness in your day-to-day life.
Not only can a sleeping disorder sap your energy, but it’s a risk factor for many different life-threatening illnesses as well. According to the Mayo Clinic, complications of obstructive sleep apnea (OSA) include high blood pressure, heart problems, metabolic syndrome, and liver problems.
Furthermore, a medical report published in the Journal of Clinical Sleep Medicine states that sleep apnea increases the risk of heart failure by 140 percent and the risk of stroke by 60 percent. What’s more, it states that obesity is by far the most significant risk factor with about 60 to 90 percent of sleep apnea patients being obese. Other risk factors include cigarette smoking, alcohol consumption, and diabetes mellitus.

Knowing this information, it’s not hard to see how sleep disorders are a much more serious condition than most people realize. While it may only manifest itself with minor symptoms in your daily life, its impact on your long-term health is far worse. It can also contribute to other unhealthy lifestyle choices such as a poor diet or exercise routine, so it’s important to seek out appropriate treatment options.
What is Continuous Positive Airway Pressure (CPAP)?
Continuous positive airway pressure is a therapy that is used to treat obstructive sleep apnea. It’s considered the first non-invasive treatment because, prior to the 1980s, the only effective treatment for OSA was tracheostomy, a surgical procedure that involves making an incision into the trachea in order to bypass an obstructed airway.

The first CPAP machine was invented by Dr. Colin Sullivan in 1981. It works by administering a gentle stream of pressurized air through oxygen tubing that’s connected to the patient’s nose. At night, the patient can breathe freely while the pressurized air prevents the throat from closing up during sleep. Although modern CPAP machines use the same principles as the one created in 1981, they are much quieter and more comfortable, allowing the patient to get a better night’s sleep.
One important thing to note is that CPAP is not the same thing as oxygen therapy. While CPAP does blow air into the nose, it uses ambient air including oxygen, nitrogen, and all the other gases that we normally breathe rather than medical grade oxygen. The sole purpose of CPAP therapy is to keep the airways open while you sleep.

While CPAP machines deliver constant pressure, this pressure can be changed when you aren’t using the device. All CPAP devices use the measurement centimeters of water (cmH20) which is the same unit that lung pressure is measured in. Most patients require between 6 and 14 cmH20 and the average setting is 10 cmH20, however, the setting you use will depend entirely on your condition and the setting that your doctor prescribes. It’s also important to note that every CPAP machine has different capabilities, so you’ll want to make sure it meets your needs before purchasing it.
What is Bilevel Positive Airway Pressure (BiPAP)?
Although CPAP is still the most widely used PAP therapy device to this day, one of the major complaints about it is that it’s difficult to exhale against the air put out by the device. This typically isn’t a problem for someone with healthy lungs, but if you suffer from a low FEV1/FVC ratio, this could be a different story. In simple terms, FEV1/FVC ratio measures your lungs’ ability to exhale effectively. Low FEV1/FVC is often a sign of obstructive lung diseases like chronic bronchitis or emphysema.

BiPAP or Bilevel positive airways pressure is an alternative to CPAP which has two different pressure settings: one for inhalation (inspiratory positive airways pressure) and one for exhalation (expiratory positive airway pressure). The BiPAP machine will automatically detect whether you’re inhaling or exhaling and administer the pressure accordingly. Typically, a higher pressure will be applied when you’re inhaling.
CPAP With C-Flex versus BiPAP
Many people get confused when they hear about C-Flex which is a special feature that comes with some newer CPAP machines. This setting will help decrease the expiratory pressure by up to 3 cmH20. So, in other words, it’s more of a comfort feature that doesn’t completely eliminate the expiratory pressure. On some devices, this feature is called “expiratory pressure relief” or “EPR” for short.
What is Automatic Positive Airway Pressure (APAP)?
APAP is the third and final category of positive airway pressure device. Unlike CPAP and BiPAP, APAP machines automatically adjust airway pressure depending on what is needed at any given time. For example, if the APAP machine detects that your airways have closed, it will increase the pressure to open them up. Similarly, it can detect other episodes like hypopnea (slow and shallow breathing), flow limitation (when an increase in esophageal pressure is not accompanied by a flow increase), or snoring which can also disrupt sleep.
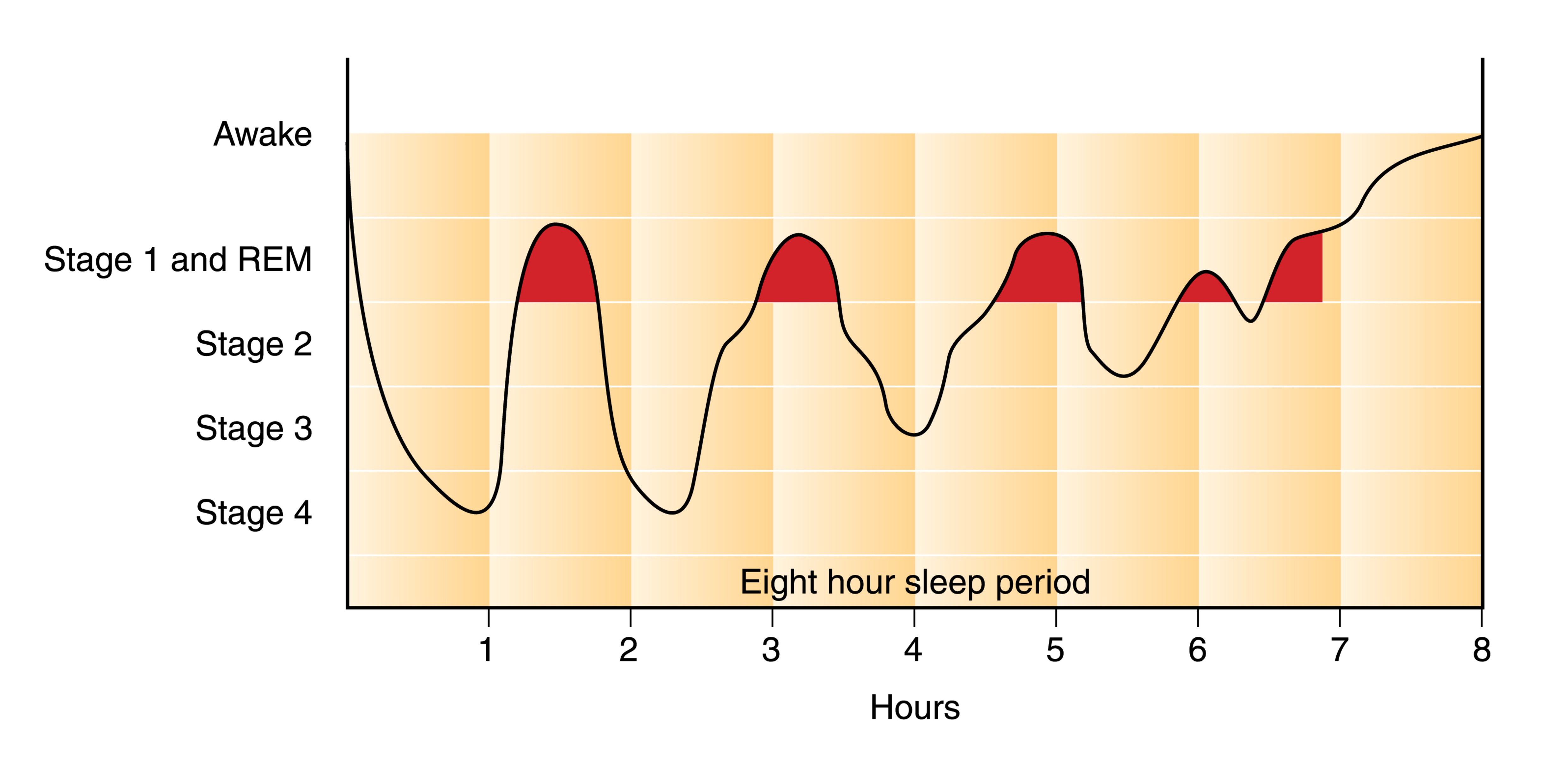
One of the obvious benefits of APAP is that it’s significantly more adaptable than CPAP or BiPAP. It contains a lot more technology and as a result, it’s often better for treating complex sleep apnea conditions. One complex form of apnea, REM-related obstructive sleep apnea occurs specifically during the rapid eye movement (REM) phase of sleep.
Another type of apnea that can be remedied with APAP is positional apnea. This is when your apneic episodes can be attributed to one or more specific sleeping positions. If you tend to move around a lot at night, the APAP machine will recognize this and adjust accordingly.
What is Supplemental Oxygen Therapy?
While supplemental oxygen therapy is often confused with CPAP, BiPAP, and APAP, it is an entirely different therapy that is used to treat respiratory conditions rather than sleep disorders. Oxygen therapy is the administration of medical grade (high purity) oxygen via a nasal cannula. Oxygen therapy ensures the lungs are fully saturated so that a patient can maintain oxygen levels in their blood.

Most commonly, oxygen therapy is used to treat chronic obstructive pulmonary disease (COPD). This is an umbrella term used to describe two different chronic diseases: emphysema and chronic bronchitis. Emphysema is characterized by swollen and damaged alveoli. These are the small air sacs in the lungs that are responsible for the transfer of oxygen and carbon dioxide to and from the blood. Chronic bronchitis is characterized by inflamed and swollen bronchial tubes, the small airways in the lungs.
COPD is one of the most common progressive lung diseases in the world, affecting an estimated 328 million people. Although it’s primarily caused by cigarette smoking, some people contract COPD due to a rare condition called alpha-1 antitrypsin deficiency. COPD is characterized by a chronic cough, chest pain, increased phlegm and sputum production, and exercise intolerance.

Depending on the severity of COPD that a patient has, they will need different flow rates of oxygen. Supplemental oxygen is measured in either liters per minute (LPM) or milliliters per minute (ml/min) depending on the oxygen device that is being used.
What Kind of Oxygen Devices Are There?
There are several different types of oxygen device: oxygen tanks, liquid oxygen tanks, stationary oxygen concentrators, and portable oxygen concentrators. Oxygen tanks are the oldest type of oxygen therapy and they work by storing oxygen at high pressures inside of an aluminum tank. Liquid oxygen tanks are similar to regular oxygen tanks but they’re stored in liquid form meaning they need to be kept at very low temperatures.

Oxygen concentrators are electronic oxygen therapy devices that take in ambient air and remove unnecessary gases like nitrogen and argon, then it puts out medical grade oxygen through a nasal cannula. Stationary oxygen concentrators need to be plugged into a wall outlet at all times but portable oxygen concentrators run off lightweight batteries that can be taken anywhere.
Pulse Dose versus Continuous Flow
There are two different delivery methods for oxygen: continuous flow and pulse flow. The best way to think of these is like the difference between a drinking fountain and a water bottle. Drinking fountains are like continuous flow oxygen concentrators because they put out a constant stream of water irrespective of how much you drink. On the other hand, pulse flow concentrators are like water bottles because you’re drinking all of the water that comes out of the bottle.

Pulse dose oxygen concentrators are more advanced than their continuous flow counterparts because they are able to detect your breathing rate and deliver oxygen at the right moment similar to how an APAP machine changes the pressure in your airways based on your breathing and sleep patterns. However, in certain situations, your doctor may advise you to only use continuous flow oxygen machines. One of the best pulse flow portable oxygen concentrators currently available is the Caire FreeStyle Comfort and one of the best continuous flow portable oxygen concentrators is the Respironics SimplyGo.
How are PAP Therapy and Supplemental Oxygen Therapy Related?
Although PAP therapy and oxygen therapy are used to treat entirely different diseases, that doesn’t mean that they aren’t related. Both therapies are used to improve breathing and to promote lung health as well as general well-being. And in certain situations, you may need to use both CPAP and oxygen therapy at the same time.
What is COPD-OSA Overlap Syndrome?
Just like the name suggests, COPD-OSA overlap syndrome is when symptoms of both COPD and OSA are present. In other words, a patient can have both damaged lungs and airways that collapse during sleep. As you can imagine, this is a pretty bad combination and it can lead to a lot of complications when it comes to getting a good night’s sleep.

There is no evidence to suggest that OSA causes COPD or vice versa, but a COPD patient who is obese or smokes will be at a higher risk of also contracting OSA. It’s important to remember that COPD is an “obstructive” lung disease, not a “restrictive” lung disease. What this means is that it affects the lung’s ability to expel air rather than inspire air. This is why COPD patients with OSA will likely be prescribed an APAP machine rather than a CPAP machine because it doesn’t add any unnecessary strain on their lungs when they expel air.
They Both Require a Prescription
Another similarity between oxygen therapy and PAP therapy is that they both require a prescription. Under the U.S. Food and Drug Administration, CPAP, BiPAP, and APAP machines are considered “Class II Medical Devices.” This means that these devices have potential risks and you’ll need a prescription to purchase one.

Similarly, oxygen is considered a controlled substance by the FDA, and as such, any device that puts out high purity or medical grade oxygen is regulated. If you decide to purchase an oxygen tank, liquid oxygen tank, stationary or portable oxygen concentrator, you will need to provide a prescription from your doctor.
How to Connect an Oxygen Machine to CPAP
If you have COPD-OSA overlap syndrome, you may need to use both oxygen therapy and PAP therapy at the same time. If this is the case, you’ll need to make sure that your PAP device and oxygen device are compatible. Most CPAP machines are compatible with oxygen machines, but you’ll need to make sure you have a continuous flow oxygen concentrator. Pulse dose concentrators like the Inogen One G5 rely on your breathing to deliver oxygen correctly and CPAP will mess with this.

Your oxygen tubing will connect to the CPAP between the mask and the input valve, but if there is no place to connect them, then you will need to purchase an oxygen bleed adapter. Once the devices are connected you should make sure both devices are on before you go to sleep at night. If your nasal passages get dry while using both the CPAP machine and oxygen machine, you can typically purchase a humidifier for either unit that will allow you to sleep more comfortably.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Conclusion
Although CPAP therapy and oxygen therapy are commonly confused, they are not the same thing. CPAP, BiPAP, and APAP are used to treat obstructive sleep apnea, one of the leading sleep disorders in the country. Oxygen therapy, on the other hand, is used to treat COPD and other chronic respiratory diseases.
However, under certain conditions such as COPD-OSA overlap syndrome, your doctor may advise you to use both of these therapies. It can be confusing trying to pick out the right CPAP machine or oxygen concentrator, especially if you want to ensure that they’re compatible with each other. To make this process as easy as possible, reach out to our respiratory specialists here at LPT Medical and we’ll walk you through it and get you the exact device you’re looking for.
Even though COPD is a chronic respiratory disease, its effects aren't limited to your lungs and airways. COPD can affect many parts of the body over time and lead to a variety of complications.
If you have COPD, then you are probably concerned about what kinds of health problems the disease can cause and how you can protect yourself from them. The good news is that, by effectively managing your symptoms and living a healthy lifestyle, you can significantly reduce your risk for a variety of COPD complications.
While you cannot stop COPD from progressing altogether, you can make choices that slow the rate at which your symptoms become more serious. By doing so, you reduce your likelihood of developing more serious health complications that result from reduced lung function and the other effects of COPD.
In this article we're going to give you a thorough overview of some of the most common COPD complications and show you how you can prevent them. We'll also explain how each of these complications is treated so you will know what your options are if you happen to develop any of these conditions.
Here are some of the most common complications of COPD:
- Exacerbations
- Pneumonia
- Collapsed Lung (Pneumothorax)
- Osteoporosis
- Hypoxemia & Hypoxia
- Sleep Apnea
- Heart Complications
Most of these conditions are serious and can lead to more health problems, a severely reduced quality of life, or even death over time. By learning the risk factors and causes of potential COPD complications, you can make better decisions about your health and lifestyle that can protect you from these unpleasant and potentially life-threatening conditions.
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
Exacerbations

Perhaps the most common complication that COPD patients experience is a COPD exacerbation. Exacerbations happen when your COPD symptoms get noticeably worse than normal for an extended period of time.
More serious than a minor flare-up, an exacerbation can cause worsened symptoms that last for days or even weeks. Some exacerbations can be treated at home, while more serious exacerbations require medical attention or even extended hospitalization.
COPD exacerbations are most often caused by illnesses and infections, but they can also be caused by asthma, allergies, or exposure to respiratory irritants. Even a minor sickness, like a cold, can cause someone with COPD to end up with a nasty, prolonged exacerbation.
Unfortunately, one side effect of COPD is that it depresses your immune system and makes it more difficult for your lungs to fight off viruses and bacteria. That means COPD patients are especially prone to getting sick, especially with respiratory illnesses, and have a constant risk of experiencing an exacerbation.
The first sign of an exacerbation is a minor up-tick in symptoms like coughing, wheezing, breathlessness, and fatigue. If these symptoms don't quickly get better on their own, then you are likely experiencing an exacerbation.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Common Symptoms of a COPD Exacerbation:
- Irregular breathing
- Worsened coughing
- Worsened breathlessness
- Noisy breathing (wheezing or rattling may indicate fluid in your lungs)
- Increased mucus in your airways and coughing up phlegm
- Reduced appetite
- Fatigue
- Fever
- Increased difficulty sleeping
- Signs of low blood oxygen levels, including: morning headaches, swollen ankles or legs, a bluish tint to your skin or nails, or an inability to speak or catch your breath
How to Prevent a COPD Exacerbation

The best way to prevent an exacerbation is to avoid getting sick and protect your lungs from respiratory irritants like allergens and pollution. That's why it's so important for people with COPD to wash their hands, keep up with vaccinations, and avoid exposure to germs and sick people, especially during cold and flu season.
Here are some of the best ways to prevent a COPD exacerbation:
-
Stop smoking.
-
Drink plenty of fluids. This helps thin your mucus, preventing it from building up in your airways and harboring viruses and bacteria.
-
Avoid large crowds and busy public spaces during cold and flu season.
-
Wash your hands often and use hand sanitizer when you don't have access to a sink.
-
Always follow your COPD treatment plan carefully, especially when your symptoms flare up.
-
Don't skip or miss any doses of your prescribed medications.
-
Make sure you've received all your recommended vaccinations, including the pneumococcal vaccine and a yearly flu shot.
-
Eat a healthy diet and get plenty of sleep to keep your body and immune system in top shape.
- If you are prescribed supplemental oxygen, always use it as directed.
The next best thing from prevention is early treatment and management to prevent illnesses and exacerbations from getting worse. Because of this, learning to recognize the early warning signs of an exacerbation is a vital skill for anyone who has COPD.
If an exacerbation isn't quickly managed and kept under control, it can cause a permanent damage to your lungs and a permanent worsening of COPD symptoms. However, exacerbations are sometimes difficult to detect when you experience COPD symptoms daily.
This is why it's so important to pay careful attention to your body and look out for times that your symptoms get worse or more frequent than they are on a normal day.
When you notice your symptoms become elevated above your usual baseline for more than a short period of time, you should consult your doctor and your treatment plan for what to do next.
In the most serious cases, severe exacerbations can cause life-threatening complications, like pneumonia, a collapsed lung, or even respiratory failure and death. Because of this, preventing COPD exacerbations is one of the primary goals of COPD treatment.
How to Treat a COPD Exacerbation
How you treat an exacerbation depends on its severity and your unique medical condition. If you have COPD, you should already have a detailed treatment plan from your doctor that includes what medications to take when your symptoms flare up and when to call your doctor.
As soon as you notice the signs or symptoms of a COPD exacerbation, you should immediately consult the instructions laid out in your COPD treatment plan. You may need to use your inhaler more often, reduce your activity levels, or start taking a course of steroids or antibiotics.
One of the most important things to note in your COPD treatment plan is how long you should wait before consulting your doctor or seeking medical attention. The guidelines outlined in your plan should tell you when your symptoms are bad enough to warrant medical attention and how to recognize an emergency.
Here are some general guidelines for managing a COPD exacerbation:
-
Use airway clearance techniques (like huff coughing and chest percussion) to clear excess mucus out of your lungs and airways.
-
Your may need to increase how often you use your short-acting bronchodilators to manage your symptoms effectively.
-
Your doctor may put you on a short course of corticosteroid medications to help decrease inflammation and reduce the chances of more serious complications.
-
Your doctor may prescribe you antibiotics to help you recover and reduce the chances of a secondary infection and further complications.
- Get plenty of rest and drink plenty of fluids.
As we've discussed, early detection and treatment for exacerbations is key for maintaining your health and quality of life with COPD. That's why you should always be monitoring your symptoms and paying special attention to how you feel. Then, when something goes wrong, you will notice right away and be able to begin treatment as early as possible.
Pneumonia

Another common COPD complication is pneumonia, a respiratory infection that causes severe inflammation in the lungs. Pneumonia can be caused by a variety of things, including bacteria, viruses, and fungi, and is particularly dangerous for people with COPD.
Pneumonia often occurs as a secondary infection that happens as a result of another illness, like a cold or (most often) the flu. The symptoms of COPD put patients with the disease at a higher risk for pneumonia because of symptoms like thick, excess mucus, a weakened immune system, and frequent upper respiratory infections.
Pneumonia occurs when the lungs become so inflamed that fluid and pus collect in the lungs. This fluid fills up many of the lung's air sacs, preventing them from absorbing oxygen and transferring it to your blood.
With many alveoli incapacitated, your lungs' have difficulty absorbing enough oxygen with its remaining functional alveoli. For people with COPD, whose lungs have already sustained damage and struggle to absorb enough oxygen, this can severely limit airflow and cause permanent damage to their lungs.
Pneumonia is most commonly diagnosed with a physical exam and chest x-ray. Your doctor may also test a sample of fluid or mucus from your lungs to determine exactly what kind of bacteria, fungus, or virus is causing your illness.
Here are some of the most common symptoms of pneumonia:
- High fever
- Shaking
- Chills
- Fatigue
- Worsened chest pain
- Worsened shortness of breath
- Worsened cough
- Headache and body aches
Although relatively common, pneumonia is not a disease to take lightly; it normally takes up to three weeks to recover and as many as twenty percent of pneumonia cases (about 1 million people each year) require hospitalization. Also, people with COPD who contract pneumonia are at a much higher risk for life-threatening respiratory symptoms such as hypoxia and potentially fatal respiratory failure.
Pneumonia can also lead to other complications, including hypoxemia, sepsis, pleural effusion (fluid in the chest or lungs), respiratory failure, and death. Older adults above the age of 65 and people who have lung diseases like COPD are more prone to contracting and experiencing serious complications from pneumonia.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
How to Prevent Pneumonia
You can lower your risk of contracting pneumonia by avoiding getting sick and treating respiratory illnesses promptly and aggressively. However, the best first line of defense against pneumonia is vaccination.
While not 100% effective, the pneumococcal vaccine protects at least 45 out of 100 older adults from pneumococcal pneumonia. Most people in the US receive the pneumococcal vaccine as children. However, a second dose is usually recommended for people who smoke or who are over the age of 64.
How to Treat Pneumonia

Treatment for pneumonia depends on its cause and how serious the symptoms are. Viral pneumonia can sometimes be treated with antiviral medicine, while fungal and bacterial pneumonia are treated with anti-fungal and antibiotic medications, respectively.
Along with antibiotics, anti-viral, and anti-fungal drugs, rest and home care is often enough to support recovery from pneumonia. Recovery can take time, and until you feel better you should take a break from daily chores and responsibilities and give yourself plenty of time to rest.
Drinking plenty of fluids is also important, because it helps thin and loosen up the mucus so it's easier to cough phlegm up and out of your lungs. It's usually fine to take asprin or NSAIDs for a fever, but you should avoid cough suppressants since coughing to clear the phlegm from your lungs is important for recovery.
If your symptoms are severe, you may need to receive treatment in a hospital until you recover. There, you may receive more targeted antibiotic treatments, supplemental oxygen, intravenous fluids, and general medical support. If your condition is very severe, you may need more intensive treatments in an intensive care unit and breathing support through a ventilator.
You are more likely to require hospitalization if you have one or more of the following conditions:
- You are over the age of 65.
- You have other health problems or chronic diseases like asthma, diabetes, or COPD.
- Your blood oxygen levels drop too low.
- You are so ill that you cannot eat or care for yourself.
- You have severe chest pain.
- You are unable to cough up mucus and clear your lungs on your own.
- You are unable to eat or keep food or fluids down.
- Your pneumonia is not getting better with normal treatment at home.
Collapsed Lung (Pneumothorax)
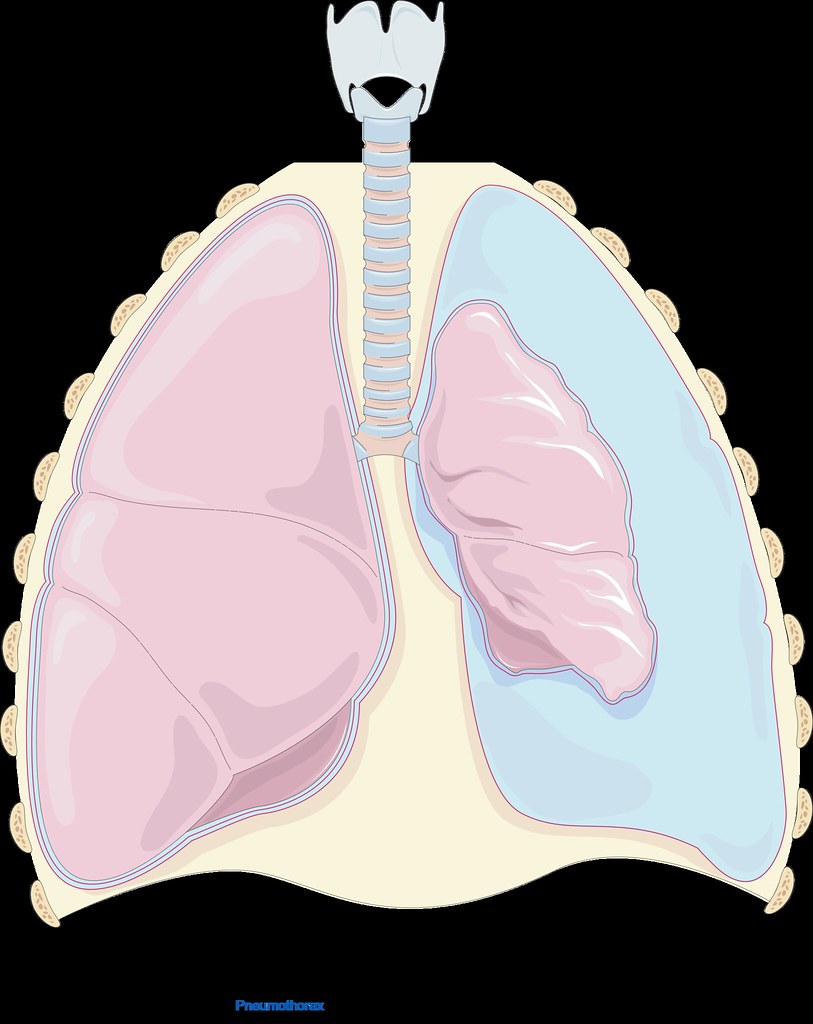
Lungs damaged by COPD are more prone to collapsing because the damaged tissue can leak air into the open space in between your lungs and your chest wall (your chest cavity). The pressure that the trapped air puts on your lung can cause your lung to collapse (also known as pneumothorax).
A collapsed lung can happen suddenly and spontaneously, without any warning. It is usually accompanied by sudden, sharp pain in the chest and worsened shortness of breath.
Pneumothorax is more common in patients with COPD because damaged, weakened lung tissue is both more likely to leak air and more likely to collapse under pressure. A collapsed lung is a medical emergency, especially for patients with COPD whose lung function is poor. If one lung collapses, the other lung may be unable to supply the body with enough oxygen, causing severe hypoxemia or hypoxia.
Here are some of the most common symptoms of a collapsed lung:
- Sudden chest pain (often described as sharp or stabbing)
- Shortness of breath
- Difficulty breathing
- Rapid breathing
- Rapid heart rate
- Coughing
- Bluish tint to the skin
How to Prevent a Collapsed Lung
The first step to preventing a collapsed lung is always to quit smoking. Smoking is one of the greatest risk factors for pneumothorax and quitting can significantly decrease your risk.
The more advanced your COPD, the more likely you are to experience a collapsed lung. That means that the next best way to prevent a collapsed lung is to follow your COPD treatment plan.
If you manage your COPD symptoms well and protect your lungs from further damage, your lungs will be less likely to leak air into your chest cavity and cause a collapsed lung. That's why it's so important to get regular check-ups from your doctor and follow the diet, exercise plan, and medication schedule that your doctor recommends.
How to Treat a Collapsed Lung
If you suspect that you might have a collapsed lung, you should go to a hospital immediately. A collapsed lung can sometimes be fatal without immediate medical attention.
At the hospital, you will likely receive treatment to remove the air in your chest cavity. This is usually done by inserting a small tube between the ribs and into the chest cavity to allow the trapped air to escape.
In some cases, if the collapse is minor, your lung may recover and re-inflate on its own. However, this determination must be made by a doctor and you should never try to treat a collapsed lung on your own at home.
Osteoporosis

Another complication that affects a large number of COPD patients is osteoporosis. Osteoporosis occurs when your bones become thin and brittle as a result of bone density loss, which significantly increases the risk of bone breaks and injuries.
Osteoporosis can be caused by a variety of factors related to COPD, including poor nutrition, lack of exercise, and increased inflammation throughout the body. All of these factors can result in a loss of bone density in patients with COPD; in fact, studies show that nearly seventy percent of all people with COPD have osteoporosis or at least some level of bone density loss.
Many people with COPD, for example, struggle to maintain a healthy weight and get enough nutrients from their diet. This is in part because people with COPD need extra calories and nutrients to support their over-strained lungs, and in part because COPD symptoms like breathlessness interfere with their ability to eat.
This causes some patients to lose weight and become malnourished, resulting in dangerous nutrient deficiencies that lead to osteoporosis. If you fail to get enough calcium and vitamin C in your diet, your body can no longer strengthen and maintain your bones, and will even cannibalize your bones to get the calcium it needs for other bodily functions.
Lack of exercise, too, can lead to bone density loss and disfigurement of your skeleton. That's because your bones are living tissue, and your body is constantly breaking down bits of your bones and building them back up.
Your body balances this process based on the amount of activity and strain your bones experience, taking density away from bones that are used less often and adding density to the bones that experience the most wear and tear.
When you stop exercising, your body takes bone density away from important bones in your limbs and other places in your body that you aren't using much. This leads to osteoporosis and changes to your skeletal structure so that it becomes even more difficult to stay active and avoid injury.
Finally, COPD patients have other characteristics that put them at a heightened risk of osteoporosis. People with COPD tend to be older, have a history of smoking, and use corticosteroid medications to treat their disease. All of these characteristics are also risk factors for osteoporosis and contribute the high incidence of bone density loss in patients with COPD.
Osteoporosis can be dangerous, painful, and interfere with your ability to exercise and stay active. It can cause even minor bumps and falls to bruise and fracture your bones, and recovery can take much longer than normal.
Here are some of the most common symptoms of osteoporosis:
- Bones that fracture easily from minor injuries or falls
- Loss of height over time
- Stooped posture
- Back pain (often caused by a fractured or collapsed vertebra)
- Receding gums (from reduced bone density in your jaw)
- Weakened grip strength
- Weak and brittle fingernails
How to Prevent Osteoporosis

Quitting smoking is one of the most important things you can do to prevent your COPD from getting worse, and it can help prevent osteoporosis as well. Getting regular physical exercise is also necessary to keep your bones healthy and strong.
It's also important to maintain a healthy diet full of whole, nutritious foods. It's particularly important to ensure that you eat plenty of foods rich in calcium and vitamin D; this ensures your body has the building blocks it needs to build thick, strong bones.
Even though COPD symptoms like breathlessness and fatigue can make it difficult to live a healthy lifestyle, it's important to follow your diet and exercise treatment plan, even when it's hard. It's not only necessary for healthy bones, but for maintaining your muscle strength, lung function, and physical mobility with COPD.
If you are struggling to get enough physical activity or need some extra help managing you disease, talk to your doctor about joining a pulmonary rehabilitation class, where you can learn all about how to better manage your diet, exercise, medications, and daily life with COPD.
How to Treat Osteoporosis
Unfortunately, once you begin losing bone density, it is usually impossible to get it back. Once you have osteoporosis or the early stages of bone density loss, the only thing you can do is manage it and keep it from getting worse.
The good news is that it usually only takes adjusting your diet and increasing exercise to manage osteoporosis and prevent further damage to your bones. Your doctor might also prescribe you a bisphosphonate medication which reduces the rate at which your body naturally breaks down your bones.
Other things you can do to prevent worsening of osteoporosis is to stop smoking and avoid drinking excessive amount of alcohol, which can impair your body's ability to build and repair your bones. You may also need to take special measures to prevent falls that could result in serious injury, for example, taking a fall prevention class or removing fall hazards in and around your home.
Chronic obstructive pulmonary disease (COPD) is a disease that causes lung irritation and therefore challenges breathing.
According to the Centers for Disease Control and Prevention (CDC) it’s the fourth most common cause of death among people in the United States. Getting treatment and developing healthy lifestyle habits are essential to improving your quality of life with this condition.
In addition to breathing difficulties, coughing, and lack of energy, COPD can also lead to other weird symptoms that are not as commonly talked about. In this article we will talk about some of these symptoms and what you can do to relieve them.
Irritation, mood swings, and depression
It might not be your first connection when it comes to how COPD will affect your life, but your emotions play an important role in your breathing patterns and vice versa.
People with COPD will sometimes experience emotional problems that they previously didn’t have before they were diagnosed with COPD. They also may be found to have started having symptoms of depression not long before the COPD diagnosis that can be attributed to COPD because their diagnosis might be well after they actually started to have COPD. People who have anxiety or depression even before they have COPD are more at risk for having frequent and severe exacerbations. This is simply because emotions have a big impact on your breathing.
{{cta('43b79c5e-6bd6-4f02-ac27-2d038d20c146','justifycenter')}}
Some of the lifestyle changes and hardships that come with COPD can lead to feelings of loss, frustration, or sadness and if you can’t do the things you once did it is easy to get caught up in depression and anxious feelings. You may even experience a mood disorder that causes you to feel irritated and disinterested.
When you’re depressed, you can get stuck mourning life as you knew it before COPD. One study from The National Center for Biotechnology Information estimated that 40 percent of those with COPD suffer from depression.
So what can you do?
While the physical challenges are hard to face, it is the mental challenges of COPD that are hard to portray to caretakers and your loved ones. The best way to get better is to express your feelings and speak with a professional about how you can communicate these feelings better. You can also talk to your doctor about antidepressants and COPD.
If it is fitting, your doctor might want to prescribe a medication to help alleviate your depression. It’s crucial to find the right medication for you because many antidepressants can interfere with medications you may already take for your COPD.
Two medications that doctors prescribe for depression in people with COPD are sertraline (Zoloft) or citalopram (Celexa). Do not be discouraged if the medication does not work right away, It can take up to 8 weeks for an antidepressant to take full effect.

If you are trying to avoid taking additional medication, but are still suffering from depression, you might find relief by seeing a mental health specialist. You can learn from others in group therapy or find individual help with one on one therapy, both of which can help you learn how to cope with your disease and adapt to your life with COPD.
Ask your pulmonologist or primary care doctor for a reference for a well reviewed therapist who helps people in your particular condition or with similar backgrounds.
Support groups may also be beneficial for people with COPD who are experiencing depression. Being in a setting with others who are facing many of the same problems can help you feel less alone. You may discover some real life tips and advice for taking better care of yourself by talking to others. With the right combination of treatments and communication, you’ll be better able to cope with your COPD and your changing lifestyle.
A variety of online support groups are also available for people with COPD. You can simply search on Facebook “LPT Medical COPD & Respiratory Support Group” and find a community of people willing to help others with COPD. There are many other popular sites that have forums or discussion groups where members can share their feelings to an understanding group of peers.
Always remember that you aren’t the first person to feel this way and someone out there might have found a way of handling their emotions effectively. Taking the time to talk with someone from the comfort of your home can be a great first step to reaching out for help with depression.

How to manage showering
Showering with COPD can be very difficult and leave patients feeling exhausted just by simply standing in the water. Usually people use hot water to shower, and that humidity builds up creating a difficult breathing environment for yourself if you have COPD. You can also be exerting a lot of energy just standing for long periods of time in the heat, so your breathing will be affected by that.
So what can you do?
Here are a few suggestions to help conserve your strength and not become so short of breath while you shower.
1. Use a shower chair
If you have COPD it can take a lot of energy just to stand, bathe, and hold your arms above your head when washing your hair.
Using a shower stool can help you avoid exacerbating your condition. Sitting down alleviates the cost of energy you would exert by standing and bending over. By conserving energy, you are lowering the risk of injury from a fall or slip.
2. Keep a fan in the bathroom
Steam from a shower increases the humidity level in the room. This can also exacerbate COPD, triggering coughing and shortness of breath.
To avoid worsening symptoms, only shower in well-ventilated bathrooms either using a fan or keeping the door open or both. If you have a window in your bathroom you can keep that open as well.
You can also place a portable fan in the bathroom with the door open to ventilate the room, and minimize the humidity.
3. Use your portable oxygen concentrator in the shower

It is ok to use your oxygen in the shower, and it might make it so that you are able to handle the energy it takes to do so.
If you use a portable oxygen concentrator, make sure it is not plugged in to charge, and then you can always add an extension to the cannula tubing so that your concentrator does not get wet.
4. Take less hot showers
This one is easier said than done, because most people love a good hot shower, however this might be the reason you don't feel energized enough to take a shower comfortably.
The heat from the water creates steam so not only is the hot air harder to breath in, the humid steam also poses a lot of issues for people with trouble breathing.

Extreme or Sudden Weight Loss
Weight loss is a sign of severe COPD.
When the damage to your lungs becomes so severe your lung volume will expand in size, which leads to flattening your diaphragm, thereby reducing the amount of space between your lungs and stomach.
You might have noticed that before you were diagnosed with COPD, that you had lost a lot of weight without really doing anything. This is because people with COPD use more calories to breathe than people who don’t have the disease.
So, If you don’t know that you have COPD, this can be perplexing, especially if you’ve tried to gain the weight back and nothing works to do so. This can lead to feeling very run down and weak.
So what can you do?
Try not to eat too fast or eat certain foods that may trigger bloating or indigestion. Doing so can make it harder to breathe and being uncomfortable might discourage you from eating regular, healthy meals as well.
Try to avoid these common triggers:
- salty foods
- spicy foods
- fried foods
- high-fiber foods
- carbonated drinks
- caffeine

To increase your body weight while making sure you get the proper nutrients, it may help to:
- Eat small but frequent meals throughout the day
- Find ways to eat higher calorie foods, such as full-fat milk (“whole milk”) products instead of low fat milk products
- Reduce your intake of fluid during meals to allow more space in your stomach for food
- Drink more fluids in between meals
- Avoid foods and drinks that trigger bloating
- Eat while using oxygen treatments
- Rest before you eat
- In some cases, your doctor or dietitian may encourage you to add a nutritional supplement to your diet.
- Simplify your snacks and meals
- Find ways to prepare snacks and meals more easily might also help you meet your nutritional needs.

For example, you can reduce some of the physical work cooking involves by buying:
- Precut produce
- Microwaveable meals
- Other packaged products
- Cut back on sodium
- When you’re shopping for pre prepared or packaged food products, look for low-sodium options. Eating too much sodium causes your body to retain water, which puts more pressure on your lungs.
It is also important to pay attention to your mental health if you notice that you’ve lost weight around the same time that you’ve been experiencing feelings of depression, anxiety, or stress, consider asking your doctor about ways to improve your mental health.
{{cta('fa8abc2a-1e88-4fa3-82fd-1cb5b9ed43b2','justifycenter')}}
Antidepressants and other treatments may help you manage your weight while improving your mood and outlook on life.
For more tips and support, your doctor may refer you to a registered dietitian or other specialist. A registered dietitian can help you develop ways to adjust your diet while coping with COPD.
Feet swelling
If you have COPD, you may develop peripheral edema (fluid retention), This causes swelling of the feet, ankles, and legs. This lower body swelling can limit your activity and can be very uncomfortable. It is also a sign of advancing COPD.
As COPD begins to negatively impact your lungs and heart, your blood circulation is eventually affected as well, which causes edema. There are other causes of edema, so you will need a medical evaluation to determine if it is caused by your COPD.

So what can you do?
Medications and lifestyle changes can help reduce leg edema, both of which we will discuss in detail. The important thing is that since edema is a sign that your COPD may be progressing, you might also need to adjust your COPD treatments, for example, your doctor may increase your oxygen therapy prescription.
If you have a hard time doing physical activity due to COPD, it can be difficult to distinguish edema from weight gain.
If you are experiencing lower body swelling from your COPD, fluid management is an important part of the treatment, and it involves lifestyle strategies as well as medication.
Medications that can help reduce edema include diuretic prescriptions, which trigger the elimination of fluid in the urine.
Other methods you should try to minimizing leg swelling include:

- Rest with your feet up: By lifting your feet up at the same level as your heart (or higher) you are reducing the blood flow into your legs which should bring down the swelling.
- Wear compression stockings: Supportive socks may also help bring down the swelling of blood in your feet and ankles. These can normally be purchased at any drugstore.
- Keep up with hydration: You must closely follow your doctor's instructions when it comes to fluids because your fluid intake can be tricky when you have COPD-associated leg edema. Drinking too much fluid can cause edema if your kidneys can't catch up with urine production and on the other hand not drinking enough water may also cause swelling if your kidneys retain excess fluid to prevent dehydration.
- Reduce salt: Your salt intake can influence the edema in your legs. Salt concentration managed by your kidneys, so too little or too much salt can result in swelling or dehydration.
- Get regular exercise: Staying active can help your lungs and heart function properly even if you have COPD it is important to maintain healthy circulation.
Oxygen therapy as treatment for COPD
When you start to get extra oxygen into your system while taking oxygen therapy it can help you have fewer intense bursts of being breathless.

It can also:
- Helps you to sleep better
- Increases your energy and ability to exercise
- Helps you focus
- Boosts your mood
- Improves sex
- Lowers your chance of heart failure (when your heart doesn’t pump enough blood to your body)
- Even prolongs your life expectancy
If your doctor prescribes you oxygen therapy at any point, it is crucial to work with a oxygen supply company that is a licensed distributer and has a dedicated team of experienced respiratory specialist that can connect you with a portable oxygen concentrator that fits into your life with ease.
Overview
{{cta('b59df0c1-c4de-47a8-8e1c-0d33d4b414aa','justifycenter')}}
There are a lot of other random feelings and discomforts that people can attribute to their COPD, and because this disease effects everyone differently, you might also experience something completely different than someone that is you same age and gender with COPD. Therefore, there is not one single treatment plan that works for everyone.
For the most part, the COPD diagnosis means a few things across the board. It is time to take control of your lifestyle, eat healthy foods and eat consistently to maintain a healthy weight, you should continue or start to exercise as much as possible, and you need to quit smoking if you do.
After you have incorporated these healthier lifestyle choices in your daily life, you might recognize other aspects of your life that you need to work on or you need help to mange. These weird symptoms in this article are just a few of the realities COPD patients face, and you might experience one, some, or none of these, but whatever you do, remember you are not alone and there are almost 30 million people in the United states alone with this incurable disease, however you can choose to live a well-balance life or not.
If your doctor prescribes you oxygen therapy at any point, it is crucial to work with a oxygen supply company that is a licensed distributer and has a dedicated team of experienced respiratory specialist that can connect you with a portable oxygen concentrator that fits into your life with ease.


 So we can find the best portable oxygen concentrator for your needs!
So we can find the best portable oxygen concentrator for your needs!